Abstract
Objective
Clinics have been established to provide preoperative medical consultations, and enable the anaesthetist and surgeon to deliver the best surgical outcome for patients. However, there is uncertainty regarding the effect of such clinics on surgical, in-hospital and long-term outcomes. A systematic review of the literature was conducted to determine the effectiveness of preoperative medical consultations by internal medicine physicians for patients listed for elective surgery.
Design
Systematic searches of MEDLINE, EMBASE, CINAHL, PubMed, Current Contents and the NHS Centre for Reviews and Dissemination were conducted up to 30 April 2017.
Setting
Elective surgery.
Study selection
Randomised controlled trials and non-randomised comparative studies conducted in adults.
Outcome measures
Length of hospital stay, perioperative morbidity and mortality, costs and quality of life.
Results
The one randomised trial reported that preadmission preoperative assessment was more effective than the option of an inpatient medical assessment in reducing the frequency of unnecessary admissions with significantly fewer surgical cancellations following admission for surgery. A small reduction in length of stay in patients was also observed. The three non-randomised studies reported increased lengths of stay, costs and postoperative complications in patients who received preoperative assessment. The timing and delivery of the preoperative medical consultation in the intervention group differed across the included studies.
Conclusion
Further research is required to inform the design and implementation of coordinated involvement of physicians and surgeons in the provision of care for high-risk surgical patients. A standardised approach to perioperative decision-making processes should be developed with a clear protocol or guideline for the assessment and management of surgical patients.
Keywords: preoperative medical consult, internal medicine physicians, elective surgery, systematic review
Strengths and limitations of this study.
The effectiveness of preoperative medical consultation is uncertain due to a lack of high-level comparative evidence.
The design of services applied to date is heterogeneous, but the consolidation of existing evidence has identified potential elements of preoperative assessment that may contribute to better outcomes, such as eligibility criteria for referral, and the timing and process of assessment.
Despite the limited evidence base, the presented review assembles and critically appraises the available evidence and draws some preliminary findings that may inform the design and adaptation of new and existing preoperative clinics.
Introduction
Preoperative medical consultations are an important component in the care of patients undergoing elective surgery. Patients who are at high risk of morbidity and mortality due to pre-existing comorbidities and the severity of surgery1 are targeted for preoperative medical consultations by internal medicine physicians. Such consultations involve optimising pre-existing medical conditions (eg, diabetes mellitus, ischaemic heart disease); assessing and managing risk of morbidity and mortality; initiating interventions intended to decrease perioperative risk (eg, delirium management, pulmonary preoperative evaluation with postoperative recommendations) and where appropriate, recommending the deferment or cancellation of surgery. This differs to but complements the care provided during a preoperative anaesthetic assessment that every patient receives prior to surgery.
With increasing patient age and complexity of medical conditions, there is a need for comprehensive preoperative evaluation and medical optimisation to enable the anaesthetist and surgeon to deliver the best surgical outcome.2 3 The concept of preoperative medical assessment by internal medicine physicians is moving beyond the early adopter stage, with preoperative physician-led clinics being set up across the USA and internationally. In the USA, several dedicated preoperative assessment clinics have been established to address this need and provide high-quality care.4Centres such as the Internal Medicine Perioperative Assessment, Consultation, and Treatment Center have been included as part of the preoperative evaluation model at the Cleveland Clinic Foundation, with the aim to provide thorough, timely and cost-effective assessment of surgical patients.3 In Australia, the Royal Adelaide Hospital and the Queen Elizabeth Hospital have consultant physician-led clinics dedicated to providing medical assessment and management to high-risk patients in elective surgery.
There is a strong rationale for the beneficial effects of preoperative medical consultations by internal medicine physicians in reducing postoperative length of stay and complications, and improving long-term recovery and rehabilitation. However, no systematic review of the literature reporting evaluations of preoperative medical consultation has been reported. Thus, we conducted a systematic review of the published literature reporting on preoperative medical consultations by internal medicine physicians in high-risk surgical patients.
Methods
Data sources and searches
Systematic searches of MEDLINE, EMBASE, CINAHL, PubMed, Current Contents and the NHS Centre for Reviews and Dissemination (including Cochrane Database of Systematic Reviews, Database of Abstracts of Review and Effects, Health Technology Assessment Database and NHS Economic Evaluation Database) were conducted from database inception to 30 April 2017. A full list of search terms used is provided in the online supplementary appendix 1.
bmjopen-2017-018632supp001.pdf (186KB, pdf)
Searches were conducted without language restriction. The reference lists of all included articles were then manually searched for relevant references that may have been missed during the database searches.
Study selection
Studies were selected for inclusion on the basis of the following criteria:
Type of studies
Randomised controlled trials (RCTs) and non-randomised comparative studies (eg, quasi-RCTs, controlled before and after studies and cohort studies) were considered in the review.
Participants
Humans aged 18 years and over scheduled for elective surgery.
Intervention
Preoperative medical consultations by an internal medicine physician or generalist for elective surgical patients. The assessment may take place in any setting, such as on a ward or in an outpatient clinic.
Comparator
Preoperative assessment by an anaesthetist, other existing preoperative assessment process or no preoperative medical consultation.
Outcomes
Convalescence (length of hospital stay);
Perioperative morbidity and mortality (same-day admissions, surgical cancellations, complications, mortality);
Cost/resource use (cost-effectiveness analyses, cost-savings, resource use);
Quality of life (generic or disease-specific quality-of-life survey instruments, patient satisfaction).
Two reviewers (CP, JK) independently screened all titles and abstracts to determine eligibility. Full texts were retrieved for potentially relevant articles. Disagreements were resolved through discussion.
Data extraction and quality assessment
Data were extracted by one reviewer (CP) and checked by a second (JK) using standardised data extraction tables that were developed a priori.
The evidence presented in the included studies were classified according to the National Health and Medical Research Council (NHMRC) Evidence Hierarchy.5 Study quality was assessed using the Cochrane Collaboration’s tool for assessing risk of bias in RCTs (chapter 8,6 table 8.5a) and in non-randomised studies (chapter 13,6 table 13.2a). All studies were assessed based on the four main sources of systematic bias in studies of the effects of healthcare, namely selection bias, performance bias, detection bias and attrition bias. Discrepancies were resolved through a consensus process.
Data synthesis and analysis
The heterogeneity of the interventions and the variability of outcome measures precluded meta-analysis. The outcome data from the studies were therefore reported narratively. Differences between intervention and control groups for each outcome measure were reported as difference in means, OR or risk ratio.
Results
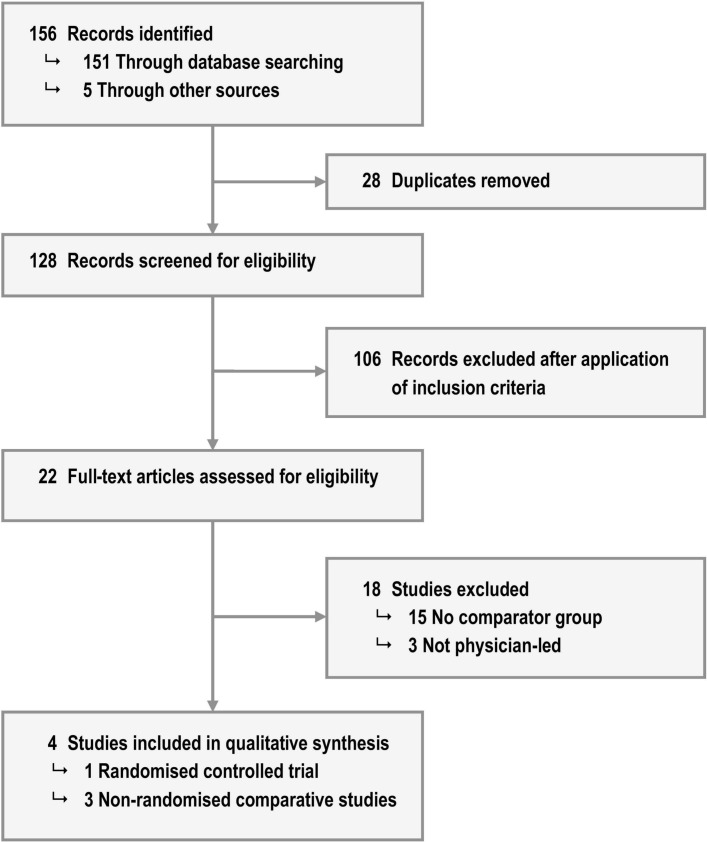
Of the 128 citations screened for eligibility, 4 met the inclusion criteria; 1 RCT and three non-randomised comparative studies (1 prospective and 2 retrospective). Figure 1 provides a summary of the search results and study selection.
Figure 1.
Summary of search results and study selection.
Quality assessment
The quality of the available evidence was poor. Table 1 summarises the risk of bias assessments for the included studies. The one RCT7 described their randomisation process but did not state their method of allocation concealment. Outcome assessments were not blinded but interobserver and intraobserver reliability tests were performed with 100% agreement reported from both tests. Blinding of investigators and patients was not possible due to the nature of the intervention. There were no losses to follow-up. The external validity of this RCT is uncertain as the study setting differed to the non-experimental setting, for example, the time between admission and surgery was more restrictive in the study.
Table 1.
Assessment of risk of bias in included studies
| Source of bias | Macpherson and Lofgren7 | Auerbach et al 8 | Katz et al 9 | Vazirani et al 10 |
| Selection bias | ||||
| Randomisation (RCT) | Permuted blocks of size 2 and 4, stratified by quartiles of anticipated LoS | – | – | – |
| Allocation concealment (RCT) | Not reported | – | – | – |
| Control for confounders (NRS) | – | Patients sampled at random; propensity score weighting | Consecutive patients | Regression methods |
| External validity (RCT and NRS) | Uncertain as study setting was more restrictive than a non-experimental setting | Potential unobserved confounding | Potential unobserved confounding | Potential unobserved confounding |
| Performance bias | ||||
| Blinding of participants and/or investigators (RCT) | No | – | – | – |
| Measurement of exposure (NRS) | – | No blinding but 5% of medical record abstractions were reviewed for data validity | No blinding | No blinding |
| Detection bias | ||||
| Blinded outcome assessment (RCT and NRS) | No blinding but 100% interobserver and intraobserver agreement* | Not reported | Not reported | Not reported |
| Attrition bias | ||||
| Completeness of follow-up (RCT and NRS) | Yes | Yes | 35 (8.3%) patients with missing medical records | Yes |
Ellipses indicate not applicable.
*A researcher re-abstracted length of stay data on 10 randomly selected records, and a physician not associated with the study abstracted length of stay from the same 10 records.
LoS, length of stay; NRS, non-randomised studies; RCT, randomised controlled trials.
Two non-randomised studies used concurrent controls, but alternative methods for patient allocation were used. Auerbach et al 8 included patients prospectively via the Center for Medicare and Medicaid Services criteria, randomly selecting medical records of patients for the public reporting of data regarding adherence to surgical site infection processes. Katz et al 9 collected retrospective data on all consecutive patients in their specified study periods. Auerbach et al 8 used propensity scores as weights to control for selection bias but only the discriminative power of the propensity score model was reported and not whether covariate balance was achieved. Katz et al 9 reported significant differences between the medical consultation and no consultation group for age, ASA status, type of surgery and gender, but did not adjust for these differences in their outcome analysis. The remaining non-randomised study used a preintervention/postintervention design and included all retrospective patients in the specified time periods.10 Vazirani et al 10 used regression models with age, gender, time period (pre or post) and the American Society of Anesthesiologists (ASA) classification as covariates to adjust for differences between groups.
Due to the non-randomised comparative study design, outcome assessments were not blinded so there is the potential for error and bias in the collection and interpretation of information. Two studies retained all patients8 10 and the remaining reported losses to follow-up of around 8%.
Description of included studies
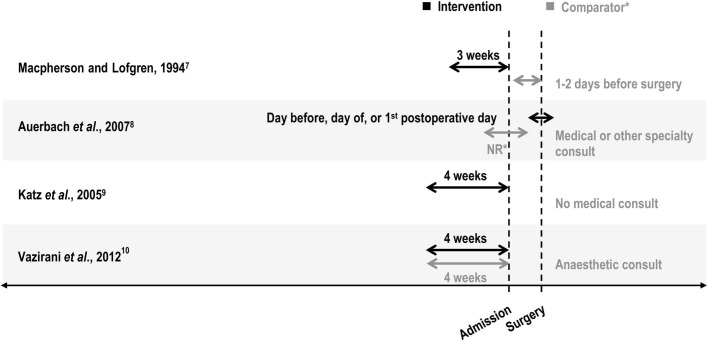
For the RCT, the mean ages of the patients were 65.3 years for the intervention group and 65.7 years for the comparator group. There were no significant differences between groups for number of medications on admission, cardiac risk index category and ASA score. Patients in the comparator group could still receive a preoperative medical consultation, if necessary, but only as an inpatient (ie, only after admission for surgery), compared with the intervention group who attended an outpatient clinic within 3 weeks of surgery (figure 2). A range of surgical procedures across multiple specialties were included, with no significant differences in the proportion of patients in each surgical service.
Figure 2.
The timing of the preoperative medical consultation in each included study. *Macpherson and Lofgren7 compared preadmission medical consultations (outpatient clinic) to postadmission preoperative medical consultations (inpatient) and Auerbach et al 8 compared a medical consultation on the day before, day of or day after surgery with a medical or other specialty consultation on days other than the intervention (ie, two or more days before surgery).
For the non-randomised comparative studies, patients in the comparator group in one study8 received consultation from an internist on days other than the intervention or from another specialty but the actual timing of the consultation was not reported (table 2). Comparator groups in the remaining studies received either preoperative anaesthetic assessment only or did not receive any preoperative medical consultation, although no further details were reported (table 2). The timing of the preoperative medical consultation in the intervention groups differed across the three studies (figure 2). Age ranged from a mean 61.4 years to a mean 70.1 years in the intervention group and a median 58 years to a mean 67.3 years in the comparator group. A range of surgical procedures across multiple specialties were included. Two of the studies focused on clinical outcome measures and the other focused on reviewing the medical consultation process (eg, reason for consultation, consultants’ recommendations).
Table 2.
Characteristics of included studies
| Study and setting | Study type | Population | Intervention | Comparator | n (patients) |
| Macpherson and Lofgren7
Pennsylvania, USA |
Level II, randomised controlled trial | >50 years of age, referred from a surgeon, lived within 100 miles of study hospital The most common procedures included upper airway endoscopy under general anaesthetic for head and neck cancer, hip and knee arthroplasty, cataract extraction, transurethral resection of the prostate, and laminectomy |
Medical preoperative evaluation clinic (outpatient) Consultation provided by internist or third-year internal medicine resident supervised by attending internist |
Internal medicine evaluation, if necessary (inpatient) Consultation provided by internist or third-year internal medicine resident supervised by attending internist |
176 (intervention) 179 (comparator) |
| Auerbach et al
8
California, USA |
Level III 2, prospective observational cohort study with concurrent controls | >18 years of age, underwent one of the following surgeries (emergency or elective): colon surgery, cardiac bypass or valve procedures, hip or knee arthroplasty, hysterectomy, vascular surgery | Medical consultation on day before, day of or first day after surgery Consultation provided by attending physician, and fellow (for subspecialty services, eg, cardiology) or third-year internal medicine resident |
Medical consultation on days other than intervention or from non-internal medicine services Consultation provided by internist or other specialist |
117 (intervention) 1165 (comparator) |
| Katz et al
9
New York, USA |
Level III 2, retrospective observational cohort study with concurrent controls | >50 years of age, underwent elective non-cardiac surgery | Medical consultation (as noted in patients’ medical records) Consultation provided by internist or family practitioner |
No medical consultation noted in patients’ medical records No other comparator details reported |
138* (intervention) 249 (comparator) |
| Vazirani et al
10
California, USA |
Level III 3, pre-post retrospective comparative study | All patients in the Veterans Health Administration database covering the following surgical specialties: ophthalmology, orthopaedics, urology, general surgery | Hospitalist-run preoperative clinic (outpatient) Consultation provided by mid-level providers with hospitalist oversight |
Preoperative anaesthetic clinic (outpatient) Consultation provided by mid-level providers with anaesthesiologist oversight |
2565 (intervention) 2658 (comparator) |
*146 consultations.
Effectiveness of intervention
Table 3 provides a summary of the effectiveness of preoperative medical consultations by an internal medicine physician for a range of outcomes.
Table 3.
Summary of effectiveness of physician-led preoperative assessment by outcome
| Outcome and study | Intervention | Comparator | Difference* |
| Length of stay (days) | |||
| Macpherson and Lofgren7 (mean) | |||
| All patients | |||
| Preadmission for surgery | 1.6 | 2.9 | −1.3 (−0.8 to −1.8) |
| Admission for surgery | 3.6 | 3.0 | 0.6 (−0.6 to 1.8) |
| Total | 5.5 | 6.0 | −0.5 (−2.0 to 1.1) |
| Patients who had surgery | |||
| Preadmission for surgery | 1.9 | 3.0 | −1.1 (-0.5 to −1.6) |
| Admission for surgery | 4.8 | 3.9 | 0.9 (−0.6 to 2.4) |
| Total | 7.1 | 7.0 | 0.1 (−1.7 to 2.0) |
| Auerbach et al 8 (median, IQR) | |||
| Before adjustment | 10 (7–18) | 6 (4–9) | 87% (63% to 115%)† |
| After adjustment | NR | NR | 13% (2% to 26%)† |
| Vazirani et al 10 | |||
| Mean (SD) | 5.28 (9.24) | 9.87 (25.4) | NR |
| ASA classification | |||
| No disturbance | NR | NR | −1.31 (SE 5.90), P=0.82 |
| Mild | NR | NR | −2.52 (SE 1.39), P=0.07 |
| Severe | NR | NR | −4.22 (SE 0.96), P<0.01 |
| Life-threatening | NR | NR | −19.70 (SE 3.81), P<0.01 |
| Costs (USD) | |||
| Auerbach et al 8 (median) | |||
| Before adjustment | 1 55 020 (101 473–292 951) | 74 237 (53 824–126 927) | 116% (88% to 148%)† |
| After adjustment | NR | NR | 24% (14% to 36%)† |
| Postoperative complications | |||
| Auerbach et al 8 (n, %) | |||
| Before adjustment | 60 (51.3) | 322 (27.6) | OR 2.76 (1.88 to 4.04) |
| After adjustment | NR | NR | OR 1.51 (0.98 to 2.32) |
| Mortality | |||
| Katz et al 9 (n, %) | |||
| Unexpected ICU/death | 2 (1.4) | 4 (1.6) | P=0.9046 |
| Vazirani et al 10 (n, %) | 4 (0.4) | 14 (1.3) | OR 0.31 (0.10 to 0.99) |
| Surgical cancellations | |||
| Macpherson and Lofgren7 (n, %) | |||
| During admission | 10 (5.7) | 22 (12.3) | −6.6% (−0.5% to −12.7%) |
| Did not undergo surgery | 43 (24.4) | 42 (23.5) | NR |
| Vazirani et al 10 (n, %) | |||
| Total | 368 (14.3) | 400 (15.0) | NR |
| Medically avoidable‡ | 18 (4.9) | 34 (8.5) | P=0.065 |
| Patient satisfaction | |||
| Macpherson and Lofgren7 | |||
| MOS SF-22 (higher score indicates better health) | |||
| Health perceptions | 38.8 | 33.1 | NS |
| Pain | 55.3 | 59.8 | NS |
| Physical function | 45.7 | 44.1 | NS |
| Social function | 62.3 | 61.2 | NS |
| Mental health | 63.0 | 58.0 | NS |
| Questionnaire adapted from RAND§ (%) | |||
| Satisfaction with care | 73 | 66 | NS |
| Dissatisfaction with care | 39 | 47 | NS |
| Rated care as very good or excellent | 64 | 54 | NS |
| Rated care as better than most or best | 62 | 54 | NS |
| Overall, very or extremely satisfied | 66 | 58 | NS |
*Difference reported as mean difference (95% CI of the difference) unless otherwise specified.
†Cost and length of stay data were log transformed to normalise data with percentage differences attributable to consultation calculated using the following equation: 100x(eβ−1).
‡As opposed to unavoidable, patient-related causes.
§Patient satisfaction questionnaire adapted from RAND.
ASA, American Society of Anesthesiologists; ICU, intensive care unit; MOS SF-22, Medical Outcomes Study Short Form-22; NR, not reported; NS, not significant, actual P value not reported; USD, United States Dollar.
Surgical cancellations
Randomised controlled trial
A similar proportion of patients in each group did not undergo surgery (24.4% for a medical consultation within 3 weeks and 23.5% for a medical consultation after admission but before surgery). Of the surgical cancellations that occurred after the admission for surgery, the patients who received a medical consultation after admission (control group) had a higher proportion of cancellations (6.6% higher, 95% CI 0.5% to 12.7%).
Non-randomised comparative studies
One non-randomised comparative study reported on surgical cancellations.10 There were no significant differences in the number of surgical cancellations between patients who received an anaesthetic consultation and those who received a medical consultation.
Length of hospital stay
Randomised controlled trial
Across all patients, the preoperative length of stay was reduced in the intervention group (1.3-day reduction, 95% CI −1.8 to −0.8), but there was no significant difference between the intervention and control groups for the postoperative and overall length of stay.
Non-randomised comparative studies
Length of stay was reported in two of the non-randomised comparative studies.8 10 After adjustment for observed potential confounding, a medical consultation on or around the day of surgery compared with a medical or other specialty consultation in two or more days before surgery resulted in a 13% increase in length of stay (95% CI 2% to 26%).8 There were no significant differences in overall length of stay between the medical and anaesthetic consultations but patients who were ASA 3 or higher had a significantly shorter length of stay with a medical consultation.10
Costs
Randomised controlled trial
The RCT did not report on costs.
Non-randomised comparative studies
Only one non-randomised comparative study reported on costs.8 There was a 24% increase in costs for patients who received a medical consultation on or around the day of surgery compared with those who received a medical or other specialty consultation in two or more days before surgery, with increases ranging from 14% to 36%.
Postoperative complications
Randomised controlled trial
The RCT did not report on postoperative complications.
Non-randomised comparative studies
The odds of complications after postoperative day 2 for patients receiving a medical consultation on or around the day of surgery was 1.51 times greater than for patients receiving a medical or other specialty consultation in two or more days before surgery (95% CI 0.98 to 2.32).8 Suspected infection, cardiac, pulmonary and other medical complications were the most commonly reported complications.
Mortality
Randomised controlled trial
The RCT did not report on mortality.
Non-randomised comparative studies
The likelihood of death in patients who received a medical consult was significantly lower (69% less likely) than those who received an anaesthetic consult.10
Patient satisfaction
Randomised controlled trial
No significant differences in quality of life and quality of care measures at 2 months postrandomisation were reported between patients who received a medical consultation in the 3 weeks prior to admission, and following admission.
Non-randomised comparative studies
None of the non-randomised comparative studies reported on patient satisfaction.
Review of the medical consultation process
In the non-randomised study of preoperative assessment in the 4 weeks prior to admission,9 medical records were reviewed to determine the characteristics of the medical consultations. The specialty of the requesting physician and the reason for medical consultation could not be determined for the majority of the consultations (51% and 64%, respectively). Of the remaining, requests for a medical consultation were either from surgeons (46%) or other internists or family practitioners (3%), and the main reasons for requesting a medical consultation were for clearance (19%) or evaluation (14%). Other reasons included risk assessment (0.7%) and re-assessment (0.7%). Patients’ diagnoses were listed in 83% of the consultations, with 3% diagnosing a medical condition not previously identified in the admitting history. In terms of recommendations, no recommendations were reported in 43% of the consultations, 34% ‘cleared’ the patient for surgery and 20% provided a risk assessment such as ‘minimal increased risk’ or ‘no increased risk’. Of the 178 preoperative, intraoperative and postoperative recommendations made, documentation in the medical records indicated that 73% were followed, 9% were not followed and in 18% it could not be determined.
Discussion
The effectiveness of preoperative medical consultation is uncertain due to a lack of high-level comparative evidence. The one RCT7 identified reported medical consultations in an outpatient setting were effective in reducing surgical cancellations following admission for surgery compared with medical consultations in an inpatient setting. The RCT also reported a small reduction in length of stay for patients who received preadmission preoperative medical consultations, noting that the active control (inpatient medical consultations) may have reduced the effect size relative to a non-active control. The observational studies reported mixed results regarding length of stay8 10 and mortality,9 10 and increased costs8 and postoperative complications8 in patients who received preoperative medical consultations, but these results must be interpreted with caution due to the potential for bias and confounding.
Design limitations in included studies
As well as differences in the comparator arms, the reviewed studies varied with respect to the timing and delivery of the preoperative medical consultation, which precluded the pooling of results. One study evaluated the effect of medical consultations on the day before or day of surgery,8 while differences in the timing of preadmission consultations may be driven by varying waiting times across forms of elective surgery (eg, cancer vs non-cancer procedures) and geographical locations. In general, it might be hypothesised that consultations undertaken close to the date of surgery provide less time for optimisation. A recent review of guidelines pertaining to preoperative medical management suggested that consultations may be most beneficial when sought at least 4 weeks prior to elective surgery, and when there is a clear understanding of the planned procedure and its associated risks.11
The form of preoperative medical consult also varied across the included studies, with minimal detail from each of the studies on the actual services provided as part of the intervention. It was not clear in any of the included studies if the consultant providing the intervention was also involved in the postoperative care of the patient. A one-off consult with recommendations but no patient follow-up may be less effective than a coordinated approach to shared decision making between specialists and physicians for perioperative management. Katz et al 9 provided some insight into the reasons for requesting a consult, but were limited by the information documented in the medical records.
The comanagement concept of surgeons managing a patient’s surgery and surgery-related issues and the internal medicine physician or geriatrician managing a patient’s medical conditions is rational.12 The results of the review do not confirm nor reject the hypothesis that preoperative medical consultation provides important benefits. The findings suggest that there is significant uncertainty around the overall effect of such services, as well as illustrating the variation in the design and implementation of preoperative assessment.
The role of the general internist compared with other subspecialists
Internationally, the subspecialist providing the preoperative medical consultation will vary. Anaesthetists have a different focus and expertise by providing safe anaesthesia and specific perioperative management,13 14 which complements the role of the general internist who assesses and optimises the patient’s modifiable comorbidities. Despite a great deal of overlap between geriatrics and general internal medicine, the focus of a comprehensive geriatric assessment (CGA) may differ to a preoperative medical consultation in some surgical populations. A CGA intervention that focuses on the assessment component only will differ to the focus of a general internist who will assess the patient and recommend specific management plans to optimise modifiable risk factors for adverse postoperative outcomes.15 For this reason, studies involving a preoperative medical consultation by subspecialists other than the general internist as the intervention were excluded.
Recommendations for improvements in clinical practice and research design
Currently, there are no clear recommendations regarding the selection of patients who require medical consultation.16 Given limited resources, patients at high risk of morbidity and mortality should be prioritised for a medical consultation but substantial practice variation exists.17 The decision to refer a patient for preoperative consultation is at the discretion of the treating surgeon and influenced by the surgeon’s personal preference for the intervention, patient preference, patient characteristics and medical history. Auerbach et al 8 reported increases in postoperative complications with a medical consult but the consultations may have been requested for an impending or suspected complication, which would make it difficult to discern whether a consult reduced the risk of complications. Thus, confounding by indication is a major source of bias in the non-randomised comparative studies.18 Auerbach et al 8 used propensity scores as weights to adjust for confounding but the authors indicated that patterns of consultation and other unmeasured confounding factors in the patient’s medical history or illness may have biased their results. A key potential confounder that may not be adequately represented in the reported studies is frailty, which has been shown to be a predictor of surgical morbidity and mortality, and may also be an important factor in the decision to refer for preoperative medical consultation.19–21
Well-designed and conducted RCTs can remove potential confounding, but issues remain around the feasibility of such trials and the generalisability of the findings. Having a no-consultation arm in the trial for a patient identified as high risk would be a major challenge, and strict trial conditions cannot be easily translated into clinical practice. In the RCT in this review, patients in the comparator group could still receive a preoperative medical consultation as an inpatient, if necessary, and the strict trial conditions on the timing between admission and surgery may not reflect the application of the intervention in routine clinical practice.
Evidence directly linking preoperative interventions with a reduction in perioperative risk are lacking. Given the multidisciplinary care of patients in a hospital setting, it is difficult to assess whether one particular aspect of care provided directly impacts on a particular outcome. The design of services applied to date is heterogeneous, but the consolidation of existing evidence has identified potential elements of preoperative assessment that may contribute to better outcomes, for example, eligibility criteria for referral, and the timing and process of assessment. In the absence of robust evidence, preoperative medical consultations are likely to remain ad hoc in terms of implementation and design. Qualitative data may provide an in-depth understanding of the processes of care and the perceived value of preoperative consultation. Future research should aim to clearly describe the level of involvement of the internal medicine physician in the surgical decision-making process and their relationship with the surgical team. A better understanding of the mechanisms of preoperative medical consultations and the complex decision-making processes involved may help explain the relationship between medical consultations and outcomes. Further research is also required to determine the characteristics of patients who would benefit most from medical consultation.
Conclusion
Preoperative medical consultations for patients with complex care requirements and in poor health is an intuitive health service development. To date, such services appear to have been developed and implemented on a limited and ad hoc basis, resulting in varied service designs and a lack of evidence on the value of preoperative assessment. With an ageing population and increasing rates of chronic disease, the management of high-risk surgical patients is likely to become an increasingly important issue. The available evidence suggests a positive effect of preoperative medical consultation with a general internist compared with standard care, but more conclusive evidence may be needed to persuade hospitals to fund such a service. Alternative forms of preoperative assessment may also need to be considered, such as comprehensive geriatric assessment, and there may be scope to optimise the value of such services by closer consideration of referral criteria and the timing of preoperative assessment. Providing continuity of multidisciplinary care from the decision to operate through to rehabilitation and recovery is certainly logical and intuitive. However, further research is required to inform the value, and the optimal design and implementation of coordinated involvement of physicians and surgeons in the provision of care for high-risk surgical patients. A standardised approach to perioperative decision-making processes should be developed with a clear protocol or guideline for the assessment and management of surgical patients.
Supplementary Material
Footnotes
Contributors: All authors (CP, CG, RF, JK) contributed substantially to the conception and design of the study; and the acquisition, analysis and interpretation of data. CP drafted the work and all authors (CP, CG, RF, JK) provided critical revision for important intellectual content. All authors (CP, CG, RF, JK) approve of the final version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated or resolved.
Funding: This work was supported by funding from the National Health and Medical Research Council Project Grant (APP1025140).
Competing interests: CLG is a consultant physician in the High Risk Clinic at the Royal Adelaide Hospital and Queen Elizabeth Hospital. The remaining authors declare no conflict of interest.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data used in the analysis were extracted from peer-reviewed publications. No additional unpublished data were generated or collected in the study.
References
- 1. Girbes AR. The high-risk surgical patient and the role of preoperative management. Neth J Med 2000;57:98–105. 10.1016/S0300-2977(00)00053-X [DOI] [PubMed] [Google Scholar]
- 2. Michota FA, Frost SD. Perioperative management of the hospitalized patient. Med Clin North Am 2002;86:731–48. 10.1016/S0025-7125(02)00020-2 [DOI] [PubMed] [Google Scholar]
- 3. Parker BM, Tetzlaff JE, Litaker DL, et al. Redefining the preoperative evaluation process and the role of the anesthesiologist. J Clin Anesth 2000;12:350–6. 10.1016/S0952-8180(00)00169-0 [DOI] [PubMed] [Google Scholar]
- 4. Bader AM, Sweitzer B, Kumar A. Nuts and bolts of preoperative clinics: the view from three institutions. Cleve Clin J Med 2009;76:S104–11. 10.3949/ccjm.76.s4.17 [DOI] [PubMed] [Google Scholar]
- 5. NHMRC. NHMRC additional levels of evidence and grades for recommendations for developers of guidelines. Canberra: National Health and Medical Research Council, 2009. [Google Scholar]
- 6. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://handbook.cochrane.org [Google Scholar]
- 7. Macpherson DS, Lofgren RP. Outpatient internal medicine preoperative evaluation: a randomized clinical trial. Med Care 1994;32:498–507. 10.1097/00005650-199405000-00008 [DOI] [PubMed] [Google Scholar]
- 8. Auerbach AD, Rasic MA, Sehgal N, et al. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med 2007;167:2338–44. 10.1001/archinte.167.21.2338 [DOI] [PubMed] [Google Scholar]
- 9. Katz RI, Cimino L, Vitkun SA. Preoperative medical consultations: impact on perioperative management and surgical outcome. Can J Anaesth 2005;52:697–702. 10.1007/BF03016556 [DOI] [PubMed] [Google Scholar]
- 10. Vazirani S, Lankarani-Fard A, Liang LJ, et al. Perioperative processes and outcomes after implementation of a hospitalist-run preoperative clinic. J Hosp Med 2012;7:697–701. 10.1002/jhm.1968 [DOI] [PubMed] [Google Scholar]
- 11. Rivera RA, Nguyen MT, Martinez-Osorio JI, et al. Preoperative medical consultation: maximizing its benefits. Am J Surg 2012;204:787–97. 10.1016/j.amjsurg.2012.02.018 [DOI] [PubMed] [Google Scholar]
- 12. Stefan M, Iglesia Lino L, Fernandez G. Medical consultation and best practices for preoperative evaluation of elderly patients. Hosp Pract 2011;39:41–50. 10.3810/hp.2011.02.373 [DOI] [PubMed] [Google Scholar]
- 13. Blitz JD, Kendale SM, Jain SK, et al. Preoperative evaluation clinic visit Is associated with decreased risk of in-hospital postoperative mortality. Anesthesiology 2016;125:280–94. 10.1097/ALN.0000000000001193 [DOI] [PubMed] [Google Scholar]
- 14. Wijeysundera DN, Austin PC, Beattie WS, et al. A population-based study of anesthesia consultation before major noncardiac surgery. Arch Intern Med 2009;169:595–602. 10.1001/archinternmed.2009.3 [DOI] [PubMed] [Google Scholar]
- 15. Partridge JS, Harari D, Martin FC, et al. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia 2014;69:8–16. 10.1111/anae.12494 [DOI] [PubMed] [Google Scholar]
- 16. Wijeysundera DN, Austin PC, Beattie WS, et al. Variation in the practice of preoperative medical consultation for major elective noncardiac surgery: a population-based study. Anesthesiology 2012;116:25–34. 10.1097/ALN.0b013e31823cfc03 [DOI] [PubMed] [Google Scholar]
- 17. Thilen SR, Bryson CL, Reid RJ, et al. Patterns of preoperative consultation and surgical specialty in an integrated healthcare system. Anesthesiology 2013;118:1028–37. 10.1097/ALN.0b013e31828ea68a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7:1–179. 10.3310/hta7270 [DOI] [PubMed] [Google Scholar]
- 19. Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010;210:901–8. 10.1016/j.jamcollsurg.2010.01.028 [DOI] [PubMed] [Google Scholar]
- 20. Adams P, Ghanem T, Stachler R, et al. Frailty as a predictor of morbidity and mortality in inpatient head and neck surgery. JAMA Otolaryngol Head Neck Surg 2013;139:783–9. 10.1001/jamaoto.2013.3969 [DOI] [PubMed] [Google Scholar]
- 21. Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg 2012;72:1526–31. 10.1097/TA.0b013e3182542fab [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018632supp001.pdf (186KB, pdf)