Abstract
Objectives
To conduct a systematic review of interventions used to improve exercise adherence in older people, to assess the effectiveness of these interventions and to evaluate the behavioural change techniques underpinning them using the Behaviour Change Technique Taxonomy (BCTT).
Design
Systematic review.
Methods
A search was conducted on AMED, BNI, CINAHL, EMBASE, MEDLINE and PsychINFO databases. Randomised controlled trials that used an intervention to aid exercise adherence and an exercise adherence outcome for older people were included. Data were extracted with the use of a preprepared standardised form. Risk of bias was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Interventions were classified according to the BCTT.
Results
Eleven studies were included in the review. Risk of bias was moderate to high. Interventions were classified into the following categories: comparison of behaviour, feedback and monitoring, social support, natural consequences, identity and goals and planning. Four studies reported a positive adherence outcome following their intervention. Three of these interventions were categorised in the feedback and monitoring category. Four studies used behavioural approaches within their study. These were social learning theory, socioemotional selectivity theory, cognitive behavioural therapy and self-efficacy. Seven studies did not report a behavioural approach.
Conclusions
Interventions in the feedback and monitoring category showed positive outcomes, although there is insufficient evidence to recommend their use currently. There is need for better reporting, use and the development of theoretically derived interventions in the field of exercise adherence for older people. Robust measures of adherence, in order to adequately test these interventions would also be of use.
PROSPERO registration number
Keywords: exercise, adherence, older people, behaviour change, behaviour change technique taxonomy, compliance
Strengths and limitations of this study.
This systematic review adds to the evidence for exercise adherence interventions specifically for older people.
Uses a predefined behaviour change taxonomy allowing the categorisation and evaluation of interventions.
Studies included were of moderate to high risk of bias.
Introduction
Exercise is an effective treatment option for a variety of conditions1 and in a number of chronic conditions its effectiveness may be comparable to drug interventions.2 This type of therapeutic exercise is defined as a subset of physical activity that is structured and planned, with the aim of maintaining or improving one or more aspects of physical fitness, in this way it differs from physical activity which is defined as any bodily movement generated by skeletal muscle.3 Prescribed exercise is a common treatment option used by health professionals such as physiotherapists.4 No definitive figure exists regarding the number of exercise programmes prescribed in a given year. However to give some indication as to the magnitude of this number, in 2014 there were 23 006 physiotherapists in the UK.5 A UK survey of organisations offering outpatient physiotherapy reported that of the 54% of organisations to respond 1 480 893 new patients were seen in a year.6 It is known from surveys of practice that exercise is a commonly used treatment modality across a range of conditions.7–11 It is therefore reasonable to assume that a significant number of exercise programmes are being prescribed yearly.
Adherence to exercise is known to be variable. In their seminal paper, Sluijs et al 12 reported that 22% of patients were non-compliant, with 41% being partially compliant. Similar figures have been demonstrated subsequently.13 It is known that exercise adherence can affect treatment outcomes, with factors such as pain, physical function, physical performance and self-perceived effect of exercise being higher in those with better adherence.14 15 Therefore, low levels of adherence may limit the effectiveness of prescribed exercise. This makes adherence an important consideration for those who prescribe exercise.
Adherence is defined by WHO as the ‘extent to which a person’s behaviour corresponds with agreed recommendations from a healthcare provider’. 16 Adherence to medical treatments, in particular medication is well reviewed.17–19 Considering exercise adherence, previous literature has focused largely on factors relating to adherence.20–25 A previous review22 reported that adherence to treatment given in physiotherapy including prescribed exercises was influenced by low baseline levels of physical activity, low in-treatment adherence, low self-efficacy, depression, anxiety, helplessness, poor social support, greater number of perceived barriers to exercise and increased pain levels during exercise. Adherence to home-based physical therapies has been linked to several factors including intention to engage in home-based physical therapy, self-motivation, self-efficacy, previous adherence to exercise-related behaviours and also social support.20
Adhering to exercise is important for all populations, however, there are several factors that make it crucial for older people. Exercise adherence in this population is affected by health status,21 and it is known that older people are more likely to have long-term conditions (LTCs) or multiple LTCs,26 for which prescribed exercise is a treatment option.1 Exercise engagement is known to be poor in older people following discharge from hospital,27 or discharge from physiotherapy.28 This is a critical consideration because treatment outcomes in this population are linked to compliance with interventions.29 There are a number of factors that have been identified as affecting exercise adherence in older people, including low self-efficacy, low motivation, depression, lack of interest, fear of falling, health status, physical ability, low expectations, socioeconomic status and exercise programme characteristics.21 27 28 Programme design was also a factor noted by Farrance et al 30 in a mixed-method systematic review of community-based exercise interventions for older people. They also reported six key themes related to adherence, these being social connectedness, participant perceived benefits, programme design, empowering/energising effects, instructor and individual behaviour. While it is important to understand the role of these personal factors and programme characteristics, it is also crucial to establish if there is anything clinicians can do to enhance adherence to prescribed exercise in older people.
Exercise adherence interventions aim to increase the likelihood that people will follow prescribed exercise, in this way they fulfil the definition by the National Institute for Health and Care Excellence31 of a behaviour change intervention, ‘…sets of techniques, used together, which aim to change the health behaviours of individuals, communities or whole populations’. Many previous behavioural interventions have been designed using what Martin Eccles calls the ISLAGIATT principle, ‘it seemed like a good idea at the time’. 32 This lack of theoretical underpinning could potentially limit the effectiveness of interventions. For this reason and so that interventions can be described and categorised, it is important to review the theories or approaches that underpin exercise adherence interventions. One way this can be achieved is through using a method to categorise behavioural approaches, such as the Behaviour Change Technique Taxonomy (BCTT) developed by Michie et al. 33
A Cochrane review exploring interventions to improve exercise adherence in those aged 18 years and over with chronic musculoskeletal pain34 reported that interventions such as self-management techniques and supervised as well as individualised exercise might improve adherence. More recently, Peek et al 35 reviewed adherence to self-management strategies prescribed by physiotherapists. They found that interventions using activity monitoring and feedback systems, written instructions and behavioural exercise programmes with booster sessions may be effective in promoting adherence. Although both these reviews were undertaken on adult populations, they did not breakdown the population further and, there remains a need to consider interventions specific to older populations. Disease-specific reviews that are relevant to older people have taken place, in particular considering arthritis. Ezzat et al 36 reported limited evidence for exercise adherence interventions in an arthritis population. Nicolson et al 37concluded that booster sessions, and behavioural graded exercise could improve adherence for those with osteoarthritis, in addition to motivational approaches for those with chronic low back pain. However, given that exercise is prescribed for a breadth of conditions,1 there is need to consider a broader, non-disease-specific review for older people to draw evidence from a wider population.
Other approaches that have shown potential in adherence include peer delivered programmes and arthritis self-management programmes. Burton et al 38 reviewed the effectiveness of peers delivering programmes, or motivating older people to increase physical activity, finding that involving peers in exercise programmes can promote adherence. Williamson et al 39 reviewed behavioural physical activity interventions in those with lower limb osteoarthritis. They report that self-management programmes for those with osteoarthritis demonstrate a small but significant improvement in short-term physical activity. Although both these examples focus on physical activity, rather than exercise, there may be some crossover, and there remains a need to review interventions in the field of therapeutic exercise. While we know there is no clear guidance regarding approaches for therapists to optimise adherence to prescribed exercise, there are studies that consider older patients and adherence,40–42 but no evidence synthesis as yet. Therefore, the aim of this review is threefold to:
Establish what interventions have been described in the literature to improve adherence to prescribed exercise in older people.
Determine to what extent these interventions are effective at improving exercise adherence.
Describe any underlying behavioural techniques or theory behind these interventions.
Methods
The steps taken in the design and conduct of this review have been done so with consideration of the Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA).43 44 This review has been registered with PROSPERO, registration number CRD42015020884 available at http://www.crd.york.ac.uk/PROSPERO.
Data sources and searches
The following electronic databases were searched from inception up to May 2017 AMED, BNI, CINAHL, EMBASE, Medline and PsycINFO. Additionally, the reference lists of papers included in the systematic review were screened.
Search terms
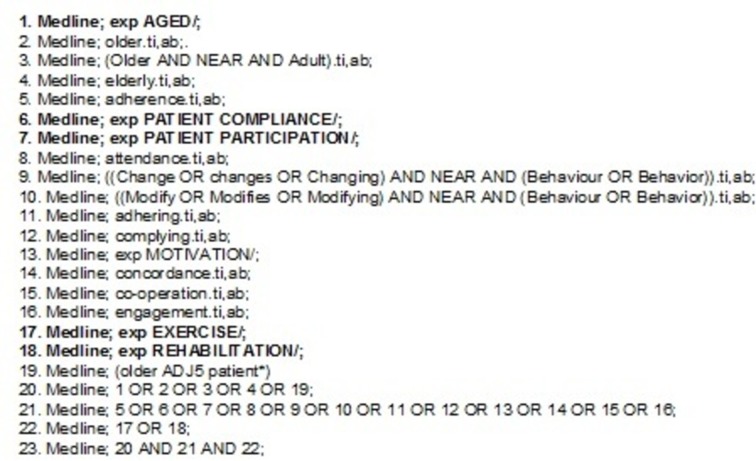
Search terms were developed by JR. The terms were expanded at two consensus meetings attended by healthcare researchers. The list was reviewed by a healthcare librarian and further changes made. The terms make use of both subject headings and free text search terms. Figure 1 is an example of the search from Medline; Medical Subject Headings terms are shown in bold.
Figure 1.
An example of search terms from Medline.
Study selection
All databases were searched by JR, once studies were returned, titles and abstracts were screened and full texts were retrieved if the study was potentially relevant. A second reviewer EH also independently screened the title and abstracts of the studies retrieved by the Embase database. This comprised 1179 hits which was 20.55% of all the studies retrieved. JR and EH compared results, any disagreements were resolved by discussion. A third reviewer KB was available if agreement could not be reached. Once full texts had been retrieved, JR and EH independently assessed the studies against the inclusion criteria. After reviewing all full texts, results were compared. Where disagreement occurred this was resolved through discussion, KB was available if agreement could not be reached.
Eligibility criteria
Studies were included if they met the following inclusion criteria:
Including a population that had a mean age of 65 years or older.
Including a population that is community dwelling.
Randomised controlled trials (RCTs).
Studies including intervention(s) aiming to improve adherence, compliance, concordance to or engagement with exercise, compared with either no adherence, compliance, concordance or engagement intervention; another adherence, compliance, concordance or engagement intervention or an intervention which does not aim to improve adherence, compliance, concordance or engagement.
A comparator group which was also undertaking the exercise programme. Where a no intervention control group occurred, there needed to be a least two active intervention groups to offer a comparison.
Published in English.
Peer reviewed.
Studies were excluded for the following reasons:
Studies including a population with a diagnosis of dementia or cognitive impairment.
Any study design that was not an RCT.
Protocols, feasibility and pilot studies including pilot RCTs.
Data extraction
Two reviewers independently extracted information from the included studies using separate, standardised preprepared forms. Data were extracted about study design, participants, setting, type and dose of intervention, underlying theory behind the intervention, the comparator arm, the method of assessment, outcome measures used and study findings.
Quality assessment
Two reviewers assessed study quality independently. One reviewer was blinded to author, journal, publication date and affiliations. The Cochrane Collaboration’s tool for assessing risk of bias was used.45 Each study was reviewed for the following items: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete data, selective outcome reporting and other sources of bias. Each item was graded as low risk of bias, high risk of bias or uncertain risk. For sequence generation, if an appropriate method of randomly generating group allocation, to allow for comparable groups was described, this was scored as low risk of bias. If a non-random method was described and/or groups were significantly different in baseline characteristics, it was scored as high risk. If the description was not clear, it was marked as uncertain risk. For allocation concealment, where a method of concealing assignment, that is, the participant or investigator could not predict assignment, such as opaque sealed envelopes this was scored as low risk. If a method enabling participants or investigators to be able to predict assignment was used, this was graded as high risk. Where information was not clear, this was scored as uncertain risk. For blinding of participants and personnel, if where possible studies reported blinding of participants and personnel this was scored as low risk. If it was possible to blind participants and personnel but this was not done, this was graded as high risk. It is acknowledged that blinding of participants and personnel is very difficult in exercise and rehabilitation studies, therefore if the reviewers felt that blinding was not possible it was scored as uncertain risk. For blinding of outcome assessors, studies where there was specific mention of steps to blind either outcome assessors, or those handling the data if outcomes were self-report questionnaires or surveys filled out at home, this was scored as low risk. If outcome assessors were not blinded this was rated as high risk. Where unclear this was graded as uncertain risk. For incomplete data, if there was little or no incomplete data, and if appropriate measures were taken to deal with missing data, this was scored as low risk. If there was a large amount of missing data, or no appropriate steps to manage missing data this was marked as high risk. Where it was unclear, this was scored as uncertain risk. For selective outcome reporting, if a study protocol was available and all outcomes described were reported this was scored as low risk. If not all outcomes were described this was scored as high risk. Where no study protocol was available this was rated as uncertain risk. For the final domain, other sources of bias, studies were scored as low risk if the reviewers felt there were no other sources of bias that could affect the results. As high risk if there were other potential sources of bias, such as small sample size, where unclear this was scored as uncertain risk. Disagreement between reviewers was resolved through discussion. If consensus was not met a third reviewer was available. If it was necessary authors were contacted for further information.
Data synthesis
The heterogeneous nature of the interventions and the different outcomes used for measuring exercise adherence prevented the use of meta-analysis. Therefore, the interventions are classified according to the behaviour change techniques that they employ, as described in the predefined BCTT.33 This taxonomy categorises behaviour change techniques by the active ingredients they use. Interventions from included studies were grouped into categories according to the techniques that they employed. Study interventions were reviewed and compared against the definitions used to define each technique. All techniques in the taxonomy fall within 1 of 16 categories. The interventions were placed into categories according to the techniques that were identified during the process of reviewing and comparing against technique definitions.
Results
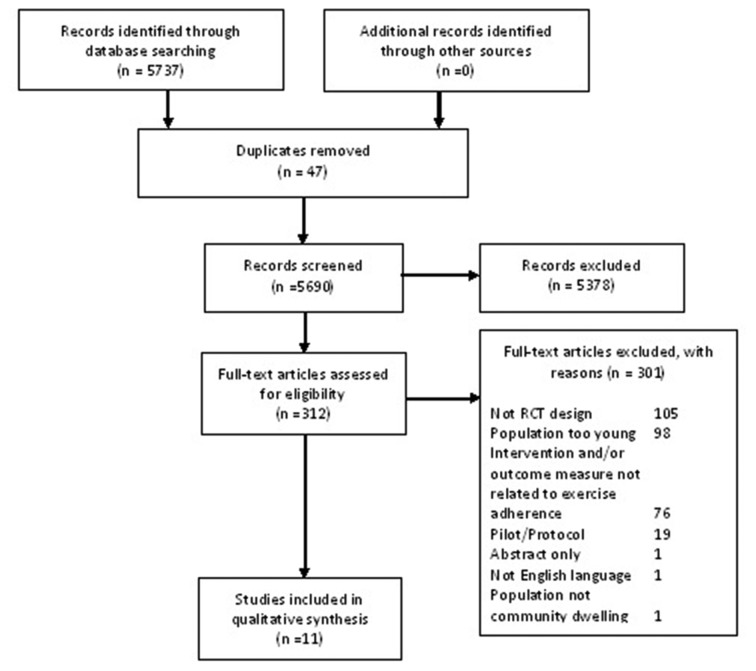
A total of 5737 papers were identified through database searches, after screening the title and abstract and removing duplicates 5425 were removed. The full text was retrieved for the remaining 312 papers, 301 papers were removed at this stage as they did not meet the inclusion criteria. This left 11 studies which were included in the review.40–42 46–53 A flow chart of this process can be seen in figure 2.
Figure 2.
Flow diagram of study selection. RCT, randomised controlled trial.
Risk of bias
Eleven studies were assessed using the Cochrane Collaboration’s tool for assessing risk of bias. No studies were rated as low risk of bias, two as moderate risk of bias and nine as high risk of bias. The scores for each domain can be seen in figure 3. The most common area where risk of bias was observed was in the relatively small sample sizes, and the lack of sample size justification of most studies.
Figure 3.
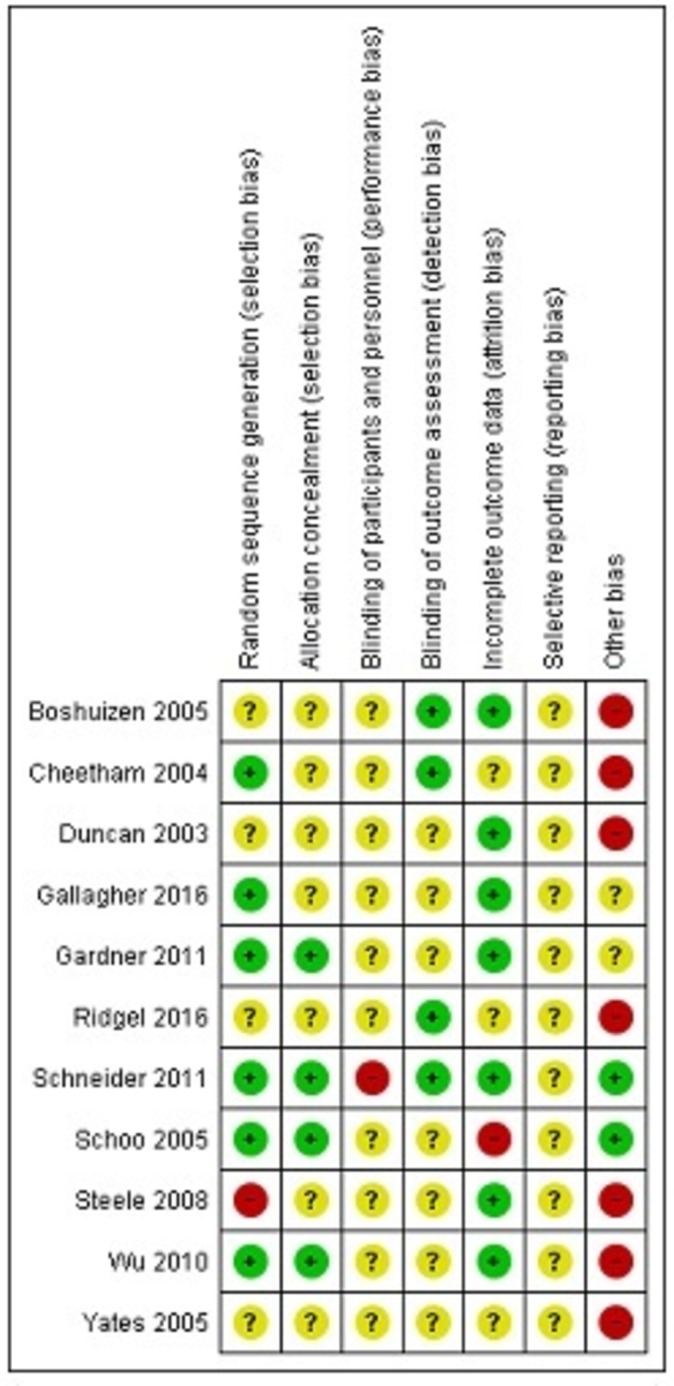
Risk of bias assessment.
Types of intervention
Several types of intervention were identified, these are categorised according to the BCTT developed by Michie et al.33 For a full description of the studies see table 1.
Table 1.
study characteristics
| Author | Population | Adherence intervention | Behavioural theory | Measure of adherence | Control or comparison | Results | Conclusion |
| Boshuizen et al 48 | Frail elderly Mean age years (SD) High guidance 80.0 (6.7), dropouts 80.8 (5.3) Medium guidance 79.3 (7.0), dropouts 79.9 (5.9), control 77.2 (6.5), dropouts 75.2 (10.5) Gender Male=5.6% |
Guidance and supervision 1) Two supervised sessions and one unsupervised a week 2) One supervised session and two unsupervised session a week |
None given | Percentage of exercise sessions (supervised+unsupervised), taken from physical therapists records and self-report diaries. At each location different physical therapists collected outcomes from those that lead the training |
Asked to remain habitually active | Percentage of exercise sessions undertaken High guidance 79 (range 57–100) Medium guidance 72 (range 20–93) (No significant difference between groups) |
No significant difference in the number of exercise sessions completed between the groups |
| Cheetham et al 52 | Intermittent claudication Mean age 67 years Gender Male=67% |
Weekly exercise and motivation class | None given | Self-reported compliance at 6 months—asked whether they walked <3 times, three times or >3 times a week Data compiled by blinded personnel |
Exercise advice: verbal and written | Average frequency of 30 min walks to near pain undertaken Supervised exercise <3 times 2 three times 8 >3 times 19 Advice <3 times 9 three times 11 >3 times 9 |
A larger number of people in the exercise class group reported to be walking either three times a week or >3 times a week (P=0.012) |
| Duncan and Pozehl 47 | Heart failure Mean age 66.4 years Gender Male=87.5% |
Individualised graphic feedback on exercise goals, participation and problem solving | Social learning theory | Exercise diaries—number of sessions completed | Exercise programme without adherence intervention | Exercise sessions completed 12 weeks Control 59.3 (SD 11.1) Intervention 62.3 (SD 6.4) 24 weeks Control 41.2 (SD 9.7) Intervention 59.6 (SD 10.6)* *Significant difference (P<0.01) |
The adherence intervention can increase exercise sessions completed after finishing a supervised exercise programme in patients with heart failure |
| Gallagher 49 | Physical therapy patients with low back, hip or knee symptoms Mean age years (SD) 69.3 (6.87) Gender Male=28.3% |
Printed messages and magnets underpinned by socioemotional selectivity theory 1) Emotional and meaningful message 2) Factual and information message |
Socioemotional selectivity theory | Self-reported adherence to their exercise programme (used to calculated adherence score) | One message group compared with the other | Average adherence score % Emotional 60% (SD 34.4%) Fact 55.3% (SD 34.0%) (No significant difference between groups) |
No significant difference found in participants’ adherence between the message groups |
| Gardner et al 50 | Intermittent claudication Mean age years (SD) Control 65 (10) Supervised ex 66 (12) Home ex 65 (11) Gender Male=47.9% |
Supervised vs unsupervised exercise 1) Home exercise (no supervision) for 12 weeks+step activity monitor 2) Supervised exercise for 12 weeks+step activity monitor |
None given | Total exercise sessions, using step activity monitor and exercise log book | Encouraged to walk more on their own | Total exercise sessions completed % Supervised group 84.8 (SD 20.9) Home group 82.5 (SD 27.7) (No significant difference between groups) |
The relatively high adherence rate in home-based exercise was similar to that found with the supervised exercise group |
| Ridgel et al 53 | Parkinson’s disease and depression Mean age years (SD) 70.2 (7.9) Gender Male=63.3% |
Psychoeducation, peer education/support, group exercise (Enhanced EXerCisE thErapy (EXCEED) group) | None given | Number of exercise sessions attended, recorded by a research assistant. Those performing outcome measures were blinded to group assignment | Self-guided psychoeducation and exercise (SGE). No group interactions or peer education | Number of exercise sessions attended at 12 weeks EXCEED=20.7 (SD 8.1) SGE=22.0 (SD 8.0) |
Both groups attended a similar number of exercise sessions |
| Schneider et al 42 | Older adults who engage in aerobic or strengthening exercise <3 or more days a week Mean age years (SD) 71.8 (5.1) Gender Male=24.1% |
Cognitive behavioural therapy (CBT) 1) CBT group 2) Attention-control education group |
CBT | Time spent exercising in the past month. Exercise behaviour was assessed by a research assistant blinded to group allocation | Control group—no CBT, no education group | Time spent exercising Strengthening exercises (h) 3 months to 6 months CBT 1.0 (SD 0.8) 1.0 (0.7) Education 1.1 (SD 0.8) 1.0 (0.7) Control 1.3 (SD 1.3) 1.2 (1.3) 9 months 12 months CBT 1.0 (1.2) 0.9 (1.0) Education 1.2 (2.3) 1.2 (2.4) Control 1.0 (1.0) 1.1 (1.1) (No significant difference between groups) |
No significant difference with time spent exercising between groups |
| Schoo et al 41 | Osteoarthritis of the hip and/or knee Mean age Years (SD) Brochure 71.1 (6.83) Audio 70.9 (7.23) Video 69.2 (6.36) Gender Male=33% |
Exercise programme instruction method: 1) Brochure+audio tape 2) Brochure+video tape |
None given | Home exercise log sheets | Brochure-only group | Home exercise adherence (median) 1–4 weeks: Brochure 93% Video 92% Audio 89% 5–8 weeks: Brochure 89.5% Video 81.5% Audio 87% (No significant differences) |
Audio and video tapes given in addition to an exercise brochure, did not show an increase in adherence compared with the brochure only group |
| Steele et al 46 | Chronic lung disease Mean age 67 years Gender Male=92.5% |
Weekly phone calls and one home visit over 3 months Consisting of dealing with queries about exercise adherence, problem solving, exercise maintenance, recommendations about health problems, encouragement, evaluated home safety, assistance in establishing an individualised exercise routine. Receiving a digital pedometer and exercise handbook |
None given | Exercise diary—total minutes of exercise | Continued care from referring provider. Recommendation for continuation of the exercise programme. Invited to attend the lung club group sessions. |
Minutes of exercise Pre-intervention Control 14 (SD 14) Intervention 21 (SD 19)* Postintervention Control 28 (SD 21) Intervention 30 (SD 32) 20 weeks Control 16 (SD 19) Intervention 32 (SD 46)* 1 year Control 22 (SD 25) Intervention 33 (SD 36) *Significant differences (P<0.05) |
The adherence intervention gave limited improvement in the short term regarding self-reported maintenance of exercise after pulmonary rehabilitation in highly sedentary chronic lung disease patients. No long-term benefit was found |
| Wu et al 40 | People at risk of falling Mean age Years (SD) Tele ex 76.1 (7.9) Comm ex 74.1 (6.9) Home ex 75.9 (6.3) Gender Male=15.6% |
Method of delivering exercise programme: 1) Instructor lead video call at home 2) Instructor lead community-based group |
None given | Log sheets -Number of sessions -Time exercising |
Home exercise with a digital versatile disc (DVD) | Total time exercising (h) Tele 30 (SD 12) Comm 31 (SD 12) Home 17 (SD 17) Attendance rate (%) Tele 69 (SD 27) Comm 72 (SD 27) Home 38 (SD 46) (Tele and comm significantly higher for time exercising and attendance rate (both P<0.01) |
Compared with home exercise, tele ex (video conferencing) and comm ex (community class) were better for total time spent exercising and number of exercise sessions completed |
| Yates et al 51 | Postcardiac rehabilitation Mean age years (SD) 66.7 (9.4) Gender Male=69% |
Booster sessions, structured education and counselling given 1) Over the phone 2) In clinic |
Self-efficacy theory | Considered adherent if they had performed exercise ≥3 times a week | Usual care—one telephone call at 4–6 weeks | Adherence rate at 3 months Control 50% Clinic 70% Phone 75% Adherence rate at 6 months Control 50% Clinic 40% Phone 63% (No significant difference were found between groups) |
Adherence to the recommended exercise programme was greater in the two treatment groups compared with usual care, but differences were not significant |
*Significant (P<0.05) difference between control and intervention.
Comparison of behaviour
One study with high risk of bias41 compared exercise instruction given in audio and video format in addition to written instructions, they found no significant difference in mean exercise adherence between groups at 1–4 weeks (P=0.690) and 5–8 weeks (P=0.538).
Feedback and monitoring
One study47 with a high risk of bias, provided heart failure participants with individual graphic feedback, related to their exercise goal. They found a significant difference between number of exercise sessions completed between a group that received the intervention and a control group at 24 weeks (P<0.01).
Another study40 with a high risk of bias, compared adherence with a Tai Chi exercise programme delivered through an interactive telecommunication approach, or a class in a community centre, compared with exercising at home with a digital versatile disc (DVD) for people at risk of falling. They found the telecommunication and community-based groups had significantly higher results for time exercising and attendance rate compared with home exercise (P<0.01).
A further study52 with a high risk of bias, compared a weekly exercise and motivation classes lasting 6 months against written and verbal exercise advice, for those with intermittent claudication. Participants were advised to walk at least three times a week to near maximal pain. At 6 months, there were more participants in the intervention group who reported to be walking either three times a week, or more than three times a week, in comparison to the advice group (P<0.012).
Social support
A study46 with a high risk of bias, tested an adherence intervention for participants with chronic lung disease. The intervention included weekly phone calls and one home visit over a 3-month period. The phone calls and visit included dealing with queries about exercise adherence and exercise maintenance, problem solving, discussion and recommendations about health problems and encouragement. With home visits that evaluated home safety and helped establish an individualised exercise routine. This study found a short-term difference in minutes of exercise undertaken, between the intervention and a control at 20 weeks (P<0.05). Although this difference was absent at 1 year follow-up.
A second study with a high risk of bias48 looked at guidance and supervision for the frail elderly, testing the difference between a high guidance group and a medium guidance group. They found no difference between groups for percentage of exercise sessions undertaken.
A third study with a high risk of bias53 compared a group that received psychoeducation, peer support and group exercise, with a group that undertook self-guided psychoeducation and exercise. They found that both groups attended a similar number of exercise sessions at 12 weeks.
A study50 with a moderate risk of bias, investigated supervised exercise versus home-based exercise with no supervision. They found no significant difference between groups with regard to total exercise sessions completed (P=0.712).
Natural consequences
One study49 with moderate risk of bias provided two different types of adherence messages based on Socioemotional Selectivity Theory,54 one message emphasised emotionally meaning reasons to exercise, for example, spending time with loved ones. The other message emphasised knowledge-related goals, for example, stronger muscles. No significant difference was found in an average adherence score between the two groups 2 weeks after discharge from physical therapy (P=0.03).
Identity
One study42 with a high risk of bias, compared cognitive behavioural therapy (CBT), an attention control education group and a control group. The primary emphasis of the CBT was to teach older people to recognise and modify their thoughts or interpretations about exercise. They found no significant difference in time spent exercising between groups at 3, 6, 9 and 12 months.
Goals and planning
A study51 with a high risk of bias, compared a structured educational counselling booster session, given over the phone, or face to face, compared with usual care. During the booster sessions, participant’s individualised goals were used as a basis for intervening. Where participants were progressing towards goal achievement they received praise, and were encouraged to attribute their accomplishment to their own ability. In addition, discussion of factors inhibiting achievement of goals took place. They found no significant differences in adherence rates between groups at 3 and 6 months.
Behavioural theories
Four studies used behavioural theories to justify their chosen intervention. Duncan and Pozehl47 delivered an intervention which offered individual graphic feedback, related to the exercise goal. This was underpinned by Social Learning Theory, a theory in which Bandura suggested that people can learn through observation of others, their behaviour and the outcomes of their behaviour.55 Gallagher’s49 intervention used two different types of adherence messages, one message emphasised emotionally meaning reasons to exercise, while the other message emphasised knowledge related goals. This was based on Socioemotional Selectivity theory,54 a theory that posits that time effects the pursuit of social goals. Social motives can fall into those that deal with the acquisition of knowledge, or those that relate to regulation of emotion. Once time is perceived as limited emotional goals take priority over knowledge acquisition. Schneider et al 42 used a CBT intervention. CBT works on the principle that thoughts, emotions, physical feelings, situations and actions are connected, CBT aims to help people break down any negative thought cycles.56 Finally, Yates et al 51 used booster sessions delivered over the phone or face to face. Bandura’s self-efficacy57 was used to inform their intervention. Self-efficacy refers to the magnitude of a person’s belief in their ability to undertake a task and achieve a desired goal. Seven studies did not cite a specific behavioural theory to justify their intervention. Of the studies which reported a behavioural theory, one reported a significant improvement in exercise adherence, this was Duncan and Pozehl.47
Discussion
This review investigated interventions tested in RCTs to improve exercise adherence in older adults. Interventions were categorised using the BCTT.33 Interventions categorised in the feedback and monitoring group demonstrated positive results for exercise adherence, although risk of bias limits generalisability of these results. The inconclusive results mirror similar results to adherence prompting interventions in other populations. Peek et al 35 investigated interventions to support adherence to physiotherapy prescribed self-management strategies, they found that although some interventions had a positive impact on adherence, there was insufficient data to recommend their use clinically. Another review by McLean et al 58 investigated interventions to improve adherence to musculoskeletal physiotherapy treatment, they found moderate evidence that a motivational cognitive behavioural programme is effective at enhancing attendance to clinic sessions which were exercise based, but conflicting evidence that adherence approaches improve short-term exercise adherence, and strong evidence that adherence interventions were not effective at enhancing long-term exercise adherence. Although it has previously been found that there is evidence that interventions can improve exercise adherence in disease-specific populations which are relevant to older people, such as osteoarthritis and rheumatoid arthritis,36 back pain and hip and knee osteoarthritis.37
This review provides a synthesis of evidence specifically for older patients, without considering a specific condition. Four papers reported positive results. Three of these interventions were categorised in the feedback and monitoring category. Namely, exercise delivered by telecommunication or in a community class setting,40 supervised exercise and motivation classes52 and graphic feedback delivered by a healthcare professional.47 Interestingly, the method of feedback or monitoring differed across these studies, yet they all demonstrated positive results. Although the limitations of these studies reduce their generalisability, there may be scope for further investigation in this area. It may be that monitoring and feedback interventions can help to overcome some of the barriers to exercise adherence in older people, such as low self-efficacy and motivation,27 or help to facilitate exercise adherence, for example, it has been previously reported that adherence is generally better in programmes with supervision.21 Peek et al 35 reported that activity monitoring and feedback systems may help to promote adherence. This is in line with evidence from other populations.59 60 It has been reported that feedback may improve adherence to an exercise programme, for adults with borderline hypertension.59 Feedback is also of use in areas such as self-care in those with diabetes.60 One of the common factors that these interventions possess is that the number of contacts with healthcare professionals is greater than the control. This is reflective of work in other areas where number of contacts can affect behaviour change, such as with using exercise advice to treat young adults with prehypertension and hypertension.61
Prescribed exercise is a prominent treatment option, which is likely to be used further as people live longer,62 with more likelihood of LTCs.26 Strategies to promote adherence should therefore remain an important factor for those who prescribe exercise. An area in which exercise adherence research could move forwards would be to consider the theory that underpins interventions. Measuring adherence is essentially measuring behaviour change in participants, that is, the participant’s behaviour corresponding to recommendation from a healthcare provider,16 in this case following an exercise programme. It is interesting that seven of the studies included did not appear to have used any behavioural theory. This could have potential impact on the effectiveness of interventions. An important aspect in developing complex interventions, as outlined by the MRC’s guidance is using the best available evidence and appropriate theory.63 If adherence interventions lack theoretical underpinning, then the chances of successfully changing people’s behaviour may be limited. It may also affect the ability to appropriately categorise and replicate interventions.
Even where behavioural approaches are considered, there may still be room for further consideration. Michie et al 64 developed a framework for behaviour change interventions, The Behaviour Change Wheel. This model posits that the three crucial components to behaviour change are capability, opportunity and motivation. Interventions may need to target one, two or even all three components to facilitate change. Approaches targeting only one area may not result in the desired change in behaviour. For example, giving information may target capability, while having no effect on opportunity or motivation. Well-developed interventions underpinned by appropriate theory, are likely to maximise the potential for behaviour change, in this case adherence to prescribed exercise.
One of the challenges to research in the field of exercise adherence is measuring adherence itself. It has previously been reported that numerous methods for reporting exercise adherence exist, however, on the whole there is a lack of measures with reported validity and reliability.65 This is in line with the results of this review. The papers included used a diverse range of adherence outcome measures. Robust outcome measures would offer greater confidence in the effects of interventions, in addition to making the comparison of interventions and meta-analysis more straightforward. A further consideration in the area of exercise adherence interventions is that of contextual equivalence of intervention and control groups. Bishop et al 66 reviewed the contextual effects and behaviour change techniques of both control and target interventions, in trials from a Cochrane review of physical activity. They conclude that a broad range of control interventions are used in this field. This in turn may influence effect size, due to the different behaviour change techniques that are included within the numerous different control interventions. It is important that future work considers the contextual equivalence of control and intervention groups in the area of exercise adherence, such as considered in the review by Nicolson et al.37
Strengths and limitations
This review systematically searched the literature with clear inclusion and exclusion criteria using an appropriate risk of bias assessment tool. It also used a predefined BCTT allowing the categorisation and evaluation of interventions. Limitations of this review include the moderate to high risk of bias of the studies, in particular due to small sample sizes leading to underpowered studies. Also, it was not possible to perform meta-analyses due to the heterogeneous nature of the interventions and measurements of adherence, it is also known that there is a lack of well-developed measures of adherence for therapeutic exercise,65 making it more challenging to capture the effect of adherence interventions. Another consideration is that although it was beyond the scope of this review to analyse health outcomes, adherence promoting interventions do need to be considered in the context of these health outcome results. For it is appropriate to ensure that intervening to promote adherence also offers an improvement in health outcome, or at least causes no harm. Finally, only papers published in English were considered for this review. It is possible that there are studies published in languages other than English that would have changed the results of the review.
Future research
Interventions that focused on feedback and monitoring demonstrated significant results. However, these types of intervention need to be tested in appropriately powered trials. Second, there is need for the development of adherence interventions underpinned by appropriate theory. Finally, there is need for robust adherence measures that are valid and reliable to be developed, in order to adequately assess the effectiveness of interventions.
Conclusion
This review provides an overview of interventions to improve exercise adherence in older people. Interventions grouped in the feedback and monitoring category of the BCTT demonstrated positive effects on exercise adherence, although risk of bias limits the generalisability of these approaches. There is need for better reporting, use and the development of theoretically derived interventions in the field of exercise adherence for older people. Robust measures of adherence, in order to adequately test these interventions would also be of use.
Supplementary Material
Acknowledgments
The authors acknowledge Mary Boulton who provided supervision to JR through the study.
Footnotes
Contributors: JR conceived the study and was responsible for study design and search strategy, JR and EH were responsible for data extraction, quality assessment and data analysis. KB and HD provided methodological advice. JR drafted the manuscript, this was revised with input from EH, KB and HD. All authors approved the final version.
Funding: This work was supported by the Centre for Movement and Occupational Rehabilitation Science (MOReS) Oxford Brookes University, and the Physiotherapy Research Unit, Nuffield Orthopaedic Centre, Oxford.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data available for this review.
References
- 1. Hoffmann TC, Maher CG, Briffa T, et al. . Prescribing exercise interventions for patients with chronic conditions. CMAJ 2016;188:510–8. 10.1503/cmaj.150684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Naci H, Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347:f5577 10.1136/bmj.f5577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985;100:126–31. [PMC free article] [PubMed] [Google Scholar]
- 4. Chartered Society of Physiotherapy. What is physiotherapy? 2013. http://www.csp.org.uk/your-health/what-physiotherapy (accessed 18 Jun 2015).
- 5. Chartered Society of Physiotherapy. NHS in England reports rise in physio numbers. 2015. http://www.csp.org.uk/news/2015/04/09/nhs-england-reports-rise-physio-numbers
- 6. Chartered Society of Physiotherapy. Physiotherapy outpatient services survey 2012. London 2013. [Google Scholar]
- 7. Artz N, Dixon S, Wylde V, et al. . Physiotherapy provision following discharge after total hip and total knee replacement: a survey of current practice at high-volume NHS hospitals in England and wales. Musculoskeletal Care 2013;11:31–8. 10.1002/msc.1027 [DOI] [PubMed] [Google Scholar]
- 8. Rushton A, Wright C, Heap A, et al. . Survey of current physiotherapy practice for patients undergoing lumbar spinal fusion in the United Kingdom. Spine 2014;39:E1380–7. 10.1097/BRS.0000000000000573 [DOI] [PubMed] [Google Scholar]
- 9. Palmer S, Cramp F, Lewis R, et al. . Diagnosis, management and assessment of adults with joint hypermobility syndrome: a UK-wide survey of physiotherapy practice. Musculoskeletal Care 2015;13:101–11. 10.1002/msc.1091 [DOI] [PubMed] [Google Scholar]
- 10. Grieve R, Palmer S. Physiotherapy for plantar fasciitis: a UK-wide survey of current practice. Physiotherapy 2017;103:193–200. 10.1016/j.physio.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 11. Smith TO, Chester R, Clark A, et al. . A national survey of the physiotherapy management of patients following first-time patellar dislocation. Physiotherapy 2011;97:327–38. 10.1016/j.physio.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 12. Sluijs EM, Kok GJ, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther 1993;73:771–82. http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=8234458&retmode=ref&cmd=prlinks%5Cnpapers2://publication/uuid/B42C2D96-9561-42D1-89E0-C5621F8BF246 10.1093/ptj/73.11.771 [DOI] [PubMed] [Google Scholar]
- 13. Alexandre NM, Nordin M, Hiebert R, et al. . Predictors of compliance with short-term treatment among patients with back pain. Rev Panam Salud Publica 2002;12:86–95. 10.1590/S1020-49892002000800003 [DOI] [PubMed] [Google Scholar]
- 14. Pisters MF, Veenhof C, Schellevis FG, et al. . Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res 2010;62:1087–94. 10.1002/acr.20182 [DOI] [PubMed] [Google Scholar]
- 15. van Gool CH, Penninx BW, Kempen GI, et al. . Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Rheum 2005;53:24–32. 10.1002/art.20902 [DOI] [PubMed] [Google Scholar]
- 16. World Health Organisation. Adherence to long-term therapies. Geneva: 2003. [Google Scholar]
- 17. van Dulmen S, Sluijs E, van Dijk L, et al. . Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res 2007;7:55 10.1186/1472-6963-7-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nieuwlaat R, Wilczynski N, Navarro T, et al. . Interventions for enhancing medication adherence (Review). Cochrane Database Syst Rev 2014;11:CD000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev 2004;3:CD004804 10.1002/14651858.CD004804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Essery R, Geraghty AW, Kirby S, et al. . Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil 2017;39:519–34. 10.3109/09638288.2016.1153160 [DOI] [PubMed] [Google Scholar]
- 21. Picorelli AM, Pereira LS, Pereira DS, et al. . Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother 2014;60:151–6. 10.1016/j.jphys.2014.06.012 [DOI] [PubMed] [Google Scholar]
- 22. Jack K, McLean SM, Moffett JK, et al. . Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther 2010;15:220–8. 10.1016/j.math.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Resnick B, D’Adamo C, Shardell M, et al. . Adherence to an exercise intervention among older women post hip fracture. J Clin Sport Psychol 2008;2:41–56. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2859720&tool=pmcentrez&rendertype=abstract 10.1123/jcsp.2.1.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slovinec D’Angelo ME, Pelletier LG, Reid RD, et al. . The roles of self-efficacy and motivation in the prediction of short- and long-term adherence to exercise among patients with coronary heart disease. Health Psychol 2014;33:1344–53. 10.1037/hea0000094 [DOI] [PubMed] [Google Scholar]
- 25. Palazzo C, Klinger E, Dorner V, et al. . Barriers to home-based exercise program adherence with chronic low back pain: Patient expectations regarding new technologies. Ann Phys Rehabil Med 2016;59:107–13. 10.1016/j.rehab.2016.01.009 [DOI] [PubMed] [Google Scholar]
- 26. Department of Health. Long term conditions compendium of information. Leeds 2012. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4100717%5Cnhttp://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publications [Google Scholar]
- 27. Hill AM, Hoffmann T, McPhail S, et al. . Factors associated with older patients’ engagement in exercise after hospital discharge. Arch Phys Med Rehabil 2011;92:1395–403. 10.1016/j.apmr.2011.04.009 [DOI] [PubMed] [Google Scholar]
- 28. Forkan R, Pumper B, Smyth N, et al. . Exercise adherence following physical therapy intervention in older adults with impaired balance. Phys Ther 2006;86:401–10 http://www.ncbi.nlm.nih.gov/pubmed/16506876 [PubMed] [Google Scholar]
- 29. Fairhall N, Sherrington C, Cameron ID, et al. . A multifactorial intervention for frail older people is more than twice as effective among those who are compliant: complier average causal effect analysis of a randomised trial. J Physiother 2017;63:40–4. 10.1016/j.jphys.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 30. Farrance C, Tsofliou F, Clark C. Adherence to community based group exercise interventions for older people: a mixed-methods systematic review. Prev Med 2016;87:155–66. 10.1016/j.ypmed.2016.02.037 [DOI] [PubMed] [Google Scholar]
- 31. NICE. Behaviour change: individual approaches. London: 2014. [Google Scholar]
- 32. Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. Silverback Publishing 2014. [Google Scholar]
- 33. Michie S, Richardson M, Johnston M, et al. . The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 34. Jordan JL, Holden MA, Mason EE, et al. . Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2010;1:CD005956 10.1002/14651858.CD005956.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Peek K, Sanson-Fisher R, Mackenzie L, et al. . Interventions to aid patient adherence to physiotherapist prescribed self-management strategies: a systematic review. Physiotherapy 2016;102:127–35. 10.1016/j.physio.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 36. Ezzat AM, MacPherson K, Leese J, et al. . The effects of interventions to increase exercise adherence in people with arthritis: a systematic review. Musculoskeletal Care 2015;13:1–18. 10.1002/msc.1084 [DOI] [PubMed] [Google Scholar]
- 37. Nicolson PJA, Bennell KL, Dobson FL, et al. . Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: a systematic review and meta-analysis. Br J Sports Med 2017;51:791–9. 10.1136/bjsports-2016-096458 [DOI] [PubMed] [Google Scholar]
- 38. Burton E, Farrier K, Hill KD, et al. . Effectiveness of peers in delivering programs or motivating older people to increase their participation in physical activity: Systematic review and meta-analysis. J Sports Sci 2017;25:1–13. 10.1080/02640414.2017.1329549 [DOI] [PubMed] [Google Scholar]
- 39. Williamson W, Kluzek S, Roberts N, et al. . Behavioural physical activity interventions in participants with lower-limb osteoarthritis: a systematic review with meta-analysis. BMJ Open 2015;5:e007642 10.1136/bmjopen-2015-007642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wu G, Keyes L, Callas P, et al. . Comparison of telecommunication, community, and home-based Tai Chi exercise programs on compliance and effectiveness in elders at risk for falls. Arch Phys Med Rehabil 2010;91:849–56. 10.1016/j.apmr.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 41. Schoo AMM, Morris ME, Bui QM. The effects of mode of exercise instruction on compliance with a home exercise program in older adults with osteoarthritis. Physiotherapy 2005;91:79–86. 10.1016/j.physio.2004.09.019 [DOI] [Google Scholar]
- 42. Schneider JK, Cook JH, Luke DA. Unexpected effects of cognitive-behavioural therapy on self-reported exercise behaviour and functional outcomes in older adults. Age Ageing 2011;40:163–8. 10.1093/ageing/afq137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Reprinted from Annals of Internal Medicine). Phys Ther 2009;89:873–80. [PubMed] [Google Scholar]
- 44. Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 45. Higgins JP, Altman DG. Assessing risk of bias in included studies : Higgins JP, Green S, Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley-Blackwell, 2008:187–241. [Google Scholar]
- 46. Steele BG, Belza B, Cain KC, et al. . A randomized clinical trial of an activity and exercise adherence intervention in chronic pulmonary disease. Arch Phys Med Rehabil 2008;89:404–12. 10.1016/j.apmr.2007.11.003 [DOI] [PubMed] [Google Scholar]
- 47. Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabil Nurs 2003;28:117–22. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed6&AN=12875144%5Cnhttp://sfx.scholarsportal.info/uhn?sid=OVID:embase&id=pmid:12875144&id=&issn=0278-4807&isbn=&volume=28&issue=4&spage=117&pages=117-122&date=2003&title=Rehabilita 10.1002/j.2048-7940.2003.tb01728.x [DOI] [PubMed] [Google Scholar]
- 48. Boshuizen HC, Stemmerik L, Westhoff MH, et al. . The effects of physical therapists’ guidance on improvement in a strength-training program for the frail elderly. J Aging Phys Act 2005;13:5–22. 10.1123/japa.13.1.5 [DOI] [PubMed] [Google Scholar]
- 49. Gallagher KM. Helping older adults sustain their physical therapy gains. J Geriatr Phys Ther 2016;39:20–9. 10.1519/JPT.0000000000000040 [DOI] [PubMed] [Google Scholar]
- 50. Gardner AW, Parker DE, Montgomery PS, et al. . Efficacy of quantified home-based exercise and supervised exercise in patients with intermittent claudication: a randomized controlled trial. Circulation 2011;123:491–8. 10.1161/CIRCULATIONAHA.110.963066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yates BC, Anderson T, Hertzog M, et al. . Effectiveness of follow-up booster sessions in improving physical status after cardiac rehabilitation: health, behavioral, and clinical outcomes. Appl Nurs Res 2005;18:59–62. 10.1016/j.apnr.2004.06.012 [DOI] [PubMed] [Google Scholar]
- 52. Cheetham DR, Burgess L, Ellis M, et al. . Does supervised exercise offer adjuvant benefit over exercise advice alone for the treatment of intermittent claudication? A randomised trial. Eur J Vasc Endovasc Surg 2004;27:17–23. 10.1016/j.ejvs.2003.09.012 [DOI] [PubMed] [Google Scholar]
- 53. Ridgel AL, Walter BL, Tatsuoka C, et al. . Enhanced Exercise Therapy in Parkinson’s disease: a comparative effectiveness trial. J Sci Med Sport 2016;19:12–17. 10.1016/j.jsams.2015.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously. A theory of socioemotional selectivity. Am Psychol 1999;54:165–81. 10.1037/0003-066X.54.3.165 [DOI] [PubMed] [Google Scholar]
- 55. Bandura A. Social learning theory. Soc Learn Theory 1971;1:46. [Google Scholar]
- 56. NHS Choices. Cognitive Behavioural Therapy (CBT). 2016. http://www.nhs.uk/Conditions/Cognitive-behavioural-therapy/Pages/Introduction.aspx (accessed 15 Jan 2017).
- 57. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 58. McLean SM, Burton M, Bradley L, et al. . Interventions for enhancing adherence with physiotherapy: a systematic review. Man Ther 2010;15:514–21. 10.1016/j.math.2010.05.012 [DOI] [PubMed] [Google Scholar]
- 59. Shakudo M, Takegami M, Shibata A, et al. . Effect of feedback in promoting adherence to an exercise programme: a randomized controlled trial. J Eval Clin Pract 2011;17:7–11. 10.1111/j.1365-2753.2009.01342.x [DOI] [PubMed] [Google Scholar]
- 60. Polonsky WH, Fisher L. When does personalized feedback make a difference? A narrative review of recent findings and their implications for promoting better diabetes self-care. Curr Diab Rep 2015;15:50 10.1007/s11892-015-0620-7 [DOI] [PubMed] [Google Scholar]
- 61. Williamson W, Foster C, Reid H, et al. . Will exercise advice be sufficient for treatment of young adults with prehypertension and hypertension? A systematic review and meta-analysis. Hypertension 2016;68:78–87. 10.1161/HYPERTENSIONAHA.116.07431 [DOI] [PubMed] [Google Scholar]
- 62. Suzman R, Beard J. Global Health and Aging, US Department of State; 2011:1–32. [Online] papers2://publication/uuid/150A301A-0A61-489C-80D4-3C889BE672E2 [Google Scholar]
- 63. Craig P, Dieppe P, Macintyre S, et al. . Developing and evaluating complex interventions: New Guidance. London, 2008. http://eprints.ucl.ac.uk/103060/ (accessed 30 Jul 2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bollen JC, Dean SG, Siegert RJ, et al. . A systematic review of measures of self-reported adherence to unsupervised home-based rehabilitation exercise programmes, and their psychometric properties. BMJ Open 2014;4:e005044 10.1136/bmjopen-2014-005044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bishop FL, Fenge-Davies AL, Kirby S, et al. . Context effects and behaviour change techniques in randomised trials: a systematic review using the example of trials to increase adherence to physical activity in musculoskeletal pain. Psychol Health 2015;30:104–21. 10.1080/08870446.2014.953529 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.