Abstract
A prospective phase 2 study was conducted to evaluate the clinical utility of acupuncture-like transcutaneous nerve stimulation (ALTENS) for the treatment of chemotherapy-induced peripheral neuropathy (CIPN). Eligible cancer patients had a < 2 ECOG performance score, received neurotoxic chemotherapy, and developed CIPN symptoms for > two months. Randomization was used to eliminate bias in patient selection for ALTENS and was not to compare the effectiveness between the two treatments.ALTENS treatments were delivered using Codetron units. Bilateral acupuncture points included LI4 and LIV3, plus LI11 or ST36 were stimulated. Acupuncture treatments were administered to CV6, SP6, ST6, LI11, Bafeng, Baxie and selective Jing points bilaterally. Twelve treatments were delivered twice weekly over 6 to 8 weeks. The Modified Total Neuropathy Score (mTNS), Numbness Score, and Edmonton Symptom Assessment Score (ESAS) were assessed at baseline, treatment completion, plus at 3 and 6 months follow-up. The primary study endpoint was mTNS score at 6 months. We planned to recruit 23 patients into each group. After 30 patients were recruited, 2 were lost to follow-up at 3 months in the ALTENS group and 3 in the acupuncture group. The research team decided to recruit all remaining consecutive patients only to the ALTENS group to ensure an adequate evaluation of ALTENS, the primary object of evaluation. There were 27 patients in the ALTENS group, with an average symptom duration of 10 months after chemotherapy. Twenty four and 23 patients completed the 3 and 6 month follow-up respectively. The median mTNS scores were 7.1, 4.0, 3.6 and 3.1 at baseline, treatment completion, 3 and 6 months follow-up, respectively. One-way ANOVA analysis showed a significant improvement in mTNS scores (p<0.001) at 6 months. Numbness scores were also significantly improved at 6 months. ESAS pain scores and perception of well-being scores analyses were inconclusive. There were no significant reported side effects of ALTENS. There were only 13 patients in the acupuncture group and the number was insufficient for either an independent or a comparative analysis. The results of this study suggests that ALTENS significantly reduces the mTNS scores and numbness in patients suffering from CIPN symptoms.
Keywords: chemotherapy, ALTENS, Acupuncture, TENS, neuropathy
Introduction
Some chemotherapy agents are neurotoxic and can lead to chemotherapy-induced peripheral neuropathy (CIPN). Patients can present with sensory deficit, neuropathic pain, or motor and autonomic nervous system dysfunction.1 CIPN is a common cause for dose reduction or even termination of chemotherapy. Generally, the prevalence of CIPN decreases with time. However, 30% of patients with CIPN continue to suffer from symptoms at 6 months or more after terminating their chemotherapy.2
There are no proven prevention strategies for CIPN.3 Current treatments are mainly for controlling symptoms, particularly neuropathic pain, using pharmaceutical agents that often come with associated side effects that limit their use. Invasive procedures such as sympathetic nerve blocks and implantable spinal cord stimulators are rarely considered.4 Optimal management of CIPN is still undefined.
Results from multiple nonrandomized trials have suggested that acupuncture can improve CIPN symptoms.5 Needle acupuncture is an invasive procedure with minor risks. It requires a licensed acupuncturist, can be expensive, and may not be acceptable for all patients. Transcutaneous electrical nerve stimulation (TENS) to selected acupuncture points provides a noninvasive alternative to needle acupuncture. This treatment modality is called acupuncture-like TENS (ALTENS). It requires no acupuncture expertise in administering treatments and can be offered in conventional clinics. Moreover, ALTENS is very amenable to quality assurance in multicenter clinical trial settings.6 In 2 randomized controlled trials, ALTENS delivered comparable results to acupuncture and showed significantly better results than sham ALTENS for musculoskeletal pain.7-10 To date, there is no study examining the potential usefulness of ALTENS for alleviating CIPN symptoms.
This report presents our results of ALTENS for treating CIPN symptoms. Additional data for needle acupuncture are also presented, but comparisons cannot be made because of insufficient enrollment.
Materials and Methods
This prospective phase 2 study was approved by the Hamilton Health Sciences Research Ethics Board. Eligible patients had received neurotoxic chemotherapy (platinum compounds, taxanes, vinca alkaloids, and suramin) and had developed CIPN symptoms for at least 2 months. Eastern Cooperative Oncology Group (ECOG) performance was 2 or less. All patients were able to give informed consent.
Patients who had HIV infection, diabetes, multiple sclerosis, or unstable cardiac disease were not eligible. Patients who were pregnant, had a pacemaker, or were suffering from active psychiatric disorders were excluded. They were randomized to either ALTENS or acupuncture. Randomization was used to eliminate bias in patient selection for a particular treatment and was not intended to compare effectiveness between the 2 treatment modalities.
The ALTENS treatments were administered by trained clinical trial nurses/therapists using Codetron units (model 902-C, EHM Rehabilitation Technologies Ltd, ON, Canada). Two-inch square self-adhesive skin electrodes were used. The positive (common) electrode was placed next to the T7 spinous process, if symptoms occurred in both hands and feet, or next to the L3 spinous process, if only the feet were affected. Six negative electrodes were placed bilaterally on LI 4 and LIV 3 and, for more severe symptoms involving the hands or feet, on LI 11 or ST 36, respectively. Square electrical pulses of 250 ms duration were delivered in trains with a 4-Hz repetition rate (pulse code III on the machine). Random switching among electrodes was used to prevent habituation.10 Each electrode was switched on for 10 s at a time. Each treatment session lasted 20 minutes. Patients were treated twice weekly for 12 treatments over 6 to 8 weeks.
Acupuncture was administered by certified medical acupuncturists using 34 G (0.25 mm), 40-mm sterilized acupuncture needles. All patients were treated without electrical stimulation. CV 6, SP 6, ST36, and LI 11 were needled with the tonification technique: needle insertion and withdrawal were during patients’ inspiration, with closure of acupuncture points after needle withdrawal. Bafeng and Baxie points were needled to 2 to 3 mm deep with the sedation technique: needle insertion and withdrawal were during patients’ expiration; points were not covered after needle withdrawal. For severe numbness and dysfunction of particular fingers or toes, respective Jing points were needled with sedation technique (Table 1). Each treatment lasted 30 minutes. Acupuncture was administered twice weekly for 12 treatments over 6 to 8 weeks.
Table 1.
Anatomical Locations of Acupuncture Points Used.
| Acupuncture Point | Anatomical Locations |
|---|---|
| LI 4 (Hegu) | On the dorsum of the hand, between the first and second metacarpal bones |
| LIV 3 (Taichong) | On the dorsum of the foot, in the depression proximal to the first metatarsal space |
| LI 11 (Quchi) | At the lateral end of the transverse cubital crease |
| ST 36 (Zusanli) | 4 Finger-breadths below the lower border of the patella and 1 finger-breadth lateral to the anterior tibia crest |
| CV 6 (Qihai) | At the body midline, 2 finger-breadths below the umbilicus |
| SP 6 (Sanyinjian) | 4 Finger-breadths above the tip of the medial malleolus on the posterior border of the tibia |
| Bafeng | On the dorsum of the foot between the toes, half a finger-breadth proximal to the web margin |
| Baxie | On the dorsum of the hand, between the fingers, half finger-breadth proximal to the web margin |
| Jing | Tips of fingers or toes |
Patients’ CIPN symptoms were assessed using the following tools:
Modified total neuropathy score (mTNS)11: This consists of 2 symptom categories: motor and sensory symptoms and 4 neurological examination items: 1-g monofilament sensation level, vibration sense, motor strength, and reflexes. Each item was scored from 0 to 4, and all scores were summed to obtain a total score from 0 to 24. A higher score indicates worse neuropathy.
Numbness score: This used a Stoelting touch test sensory evaluator (a validated monofilament touch instrument) for mapping touch sensation of 4 limbs.12 Three filaments of different selected calibrated pressure—0.04, 1.0, and 10.0 g—were used on the ventral and dorsal sides of 4 areas: palm, finger, foot, and toe. In each area, reported sensation of the 0.04-g filament was scored as 1, representing normal sensation. Reported sensation of the 1-g filament was scored as 2 and of the 10-g filament was scored as 3, representing diminished light touch and a loss of protective sensation. In any area where a lower-weight filament was not felt, higher-weight filaments were tested. In each predefined area where reported sensation of different filaments occurred, an average score was obtained. The total scores for each area were the sum of scores of the ventral and dorsal sides of both limbs and ranged from 4 to 12. A higher score indicates increased numbness.
Edmonton Symptoms Assessment Scale (ESAS)13: This is a validated patient-reported outcome scale that assesses 10 common symptoms experienced by patients with cancer or under palliative care: pain, tiredness, nausea, depression, anxiety, drowsiness, lack of appetite, constipation, shortness of breath, and sense of well-being. For each item, a score from 0 to 10 was obtained from patients. A higher score indicates worse symptoms. Each item was interpreted independently from the other items.
All assessments were conducted at baseline within 2 weeks before start of treatment, at treatment completion, as well as 3 and 6 months after treatment completion.
When designing the study, there were no previous published data that could be used for calculating the sample size of a single-arm phase 2 evaluation of ALTENS. There were only limited data regarding the usefulness of acupuncture in CIPN. An estimate was made of 23 patients in each group, based on a hypothesized clinically important effect size.
Descriptive statistics were used for patients’ characteristics. Statistical analysis and graphs were completed using GraphPad Prism version 4.00 for Windows (GraphPad Software, San Diego, CA). An intention-to-treat analysis was conducted. Prior to the study, it was decided that a horizontal data imputation method, using the average of the patient’s previous 2 scores, would be used for missing data to account for an individual patient’s symptom profile and the expected randomness of missing data.14 A 1-way ANOVA test was used to determine statistically significant differences between baseline scores and scores at 6 months from treatment completion. The primary study end point was mTNS score at 6 months.
Results
A total of 47 patients consented to the study. Seven patients withdrew consent or were unable to start the study intervention for reasons including a change in decision (n = 4); recurrent disease (n = 1) and feeling too unwell (n = 2).
All remaining 40 patients completed their prescribed treatments. Of these patients, 27 received ALTENS and 13 received acupuncture treatments. After 30 patients were recruited, an interim review showed that in the ALTENS and acupuncture groups, 2 and 4 patients, respectively, had been lost to follow-up at the 3-month assessment. Of these 6 patients, 4 expressed work and family reasons for not returning. The other 2 did not reply. The research team decided to recruit all remaining consecutive patients to the ALTENS group to ensure that enough patients were recruited to assess the effectiveness of ALTENS in a phase 2 evaluation. The Research Ethics Board was notified.
Of the 40 patients, 10 were male and 30 were female, and the mean age was 58 (range = 30-79) years. Primary diagnoses were breast cancer (n = 20), colon cancer (n = 7), ovarian cancer (n = 6), cervical cancer (n = 2), fallopian tube cancer (n = 1), prostate cancer (n = 1), rectal cancer (n = 1), nasopharyngeal cancer (n = 1), and lung cancer (n = 1).
All patients received neurotoxic agents in their chemotherapy regimens, including FOLFOX (folinic acid, fluorouracil, and oxaliplatin; n = 6); FOLFOX plus eribitux (n = 1); ACT (doxorubicin, cyclophosphamide, and paclitaxel) (n = 9); ACT plus trastuzumab (n = 4); carboplatinum and taxol (n = 6); cisplatinum (n = 3); cisplatinum plus taxol (n = 1); cisplatinum plus vinorelbine (n = 1); taxol (n = 1); docetaxel (n = 1); cisplatinum plus vinorelbine (n = 1); epirubicin, cyclophosphamide. and docetaxel (n = 2); capecitabine and oxaliplatin (n = 1); FEC (fluorouracil, epirubicin, and cyclophosphamide) plus docetaxel (n = 1); patupilone (n = 1); and CMF (cyclophosphamide, methotrexate, and fluorouracil) plus AC (doxorubicin and cyclophosphamide; n = 1).
The 27 patients who received ALTENS had CIPN symptoms for an average of 10 months (range = 2-36; median = 6) after completing their chemotherapy, whereas the 13 patients who received acupuncture had an average symptom duration of 7 months (range = 2-19; median = 6).
For all patients, at baseline, the average mTNS score (24-point scales) was 6.68. The average ESAS pain score was only 2.88. Numbness in the extremities presented in all patients. Numbness was more severe on the toes (average score was 7.96) than the feet (7.4), fingers (6.2), and the palms (5.19).
All patients who received ALTENS completed their scheduled treatments (24 patients within 6 weeks and 3 within 8 weeks). All patients completed the initial post treatment assessment, but there were only 24 patients who completed the 3-month and 23 who completed the 6-month follow-up assessment.
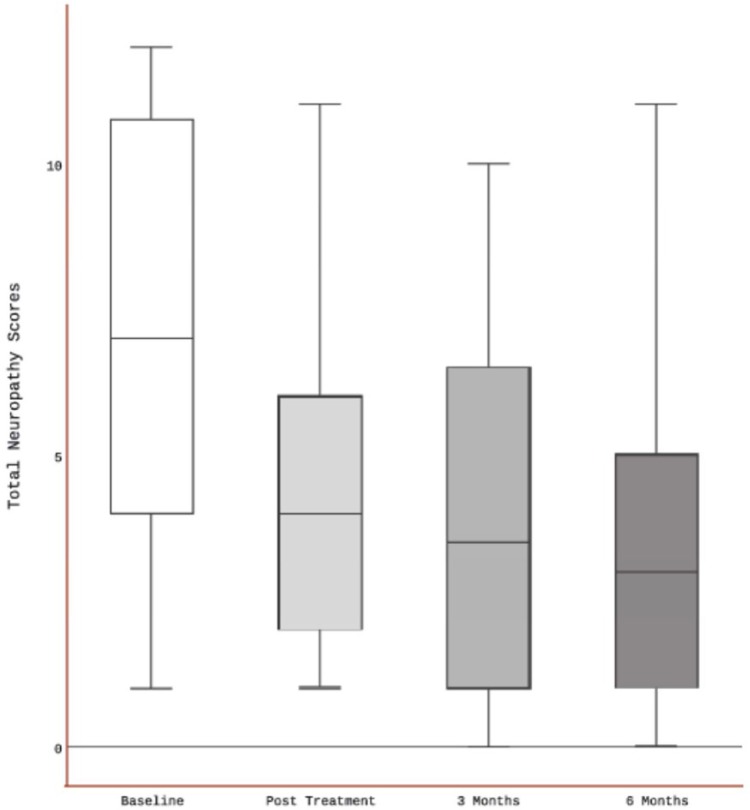
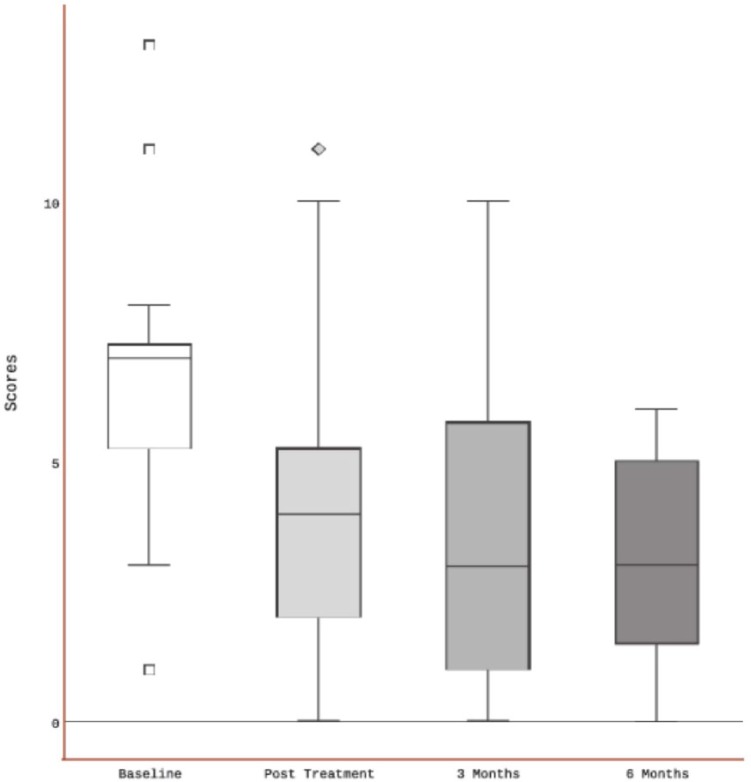
The mTNS and ESAS scores for the patients who received ALTENS are shown in the box plots, Figures 1 to 3. The nonparametric Kruskal-Wallis 1-way ANOVA test was conducted on the raw mTNS scores because of non-Gaussian distribution and the presence of missing data. After ALTENS treatment, patients had a significant reduction (P < .001) in mTNS scores at the 6-month follow-up, indicating an improvement in CIPN symptoms. A significant difference consistently existed after analysis of the imputed data using the Friedman test with repeated measures; P < .0001.
Figure 1.
Total neuropathy scores in patients who received ALTENS.
Abbreviation: ALTENS, acupuncture-like transcutaneous electrical nerve stimulation.
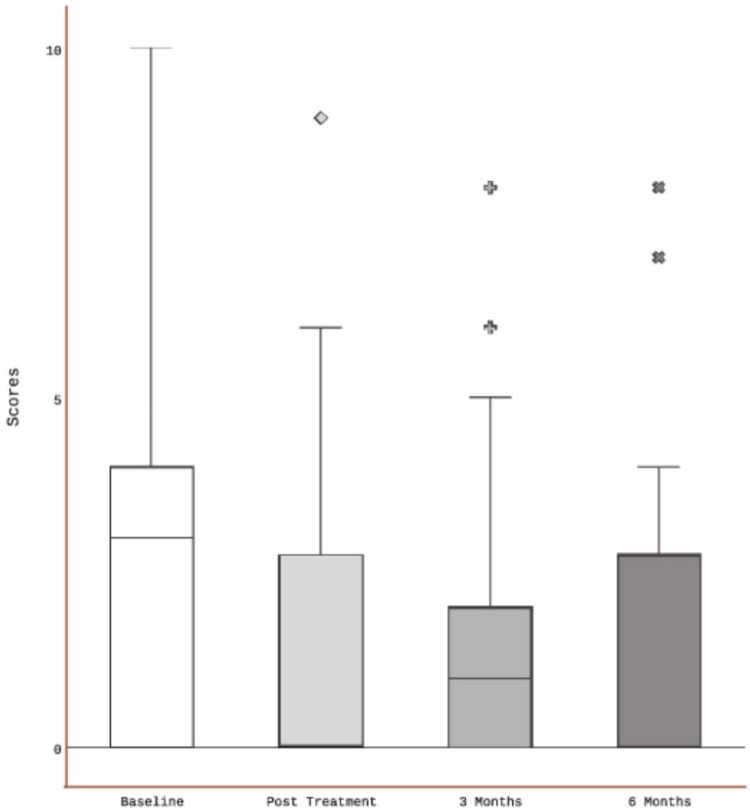
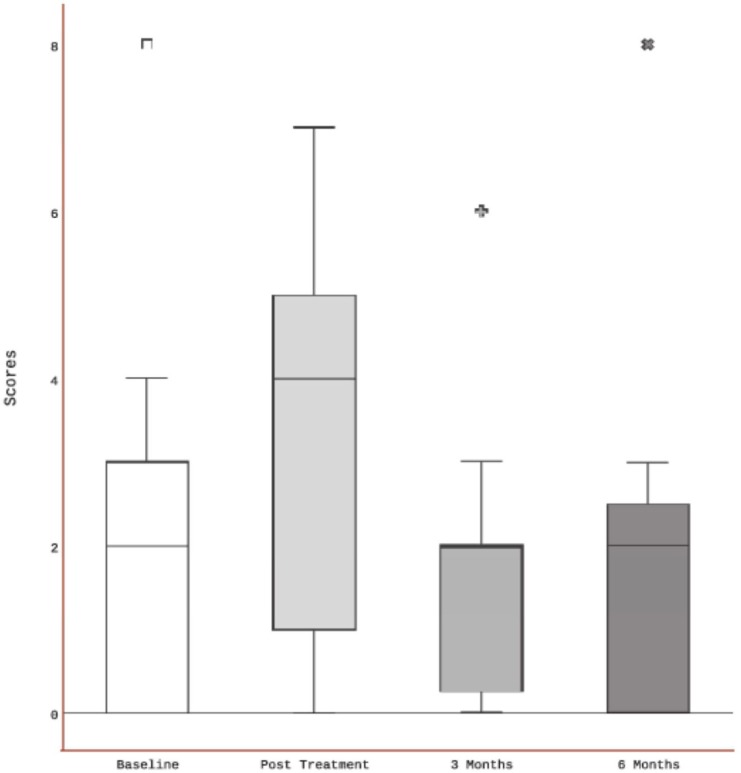
Figure 3.
Feeling of well-being scores in patients who received ALTENS.
Abbreviation: ALTENS, acupuncture-like transcutaneous electrical nerve stimulation.
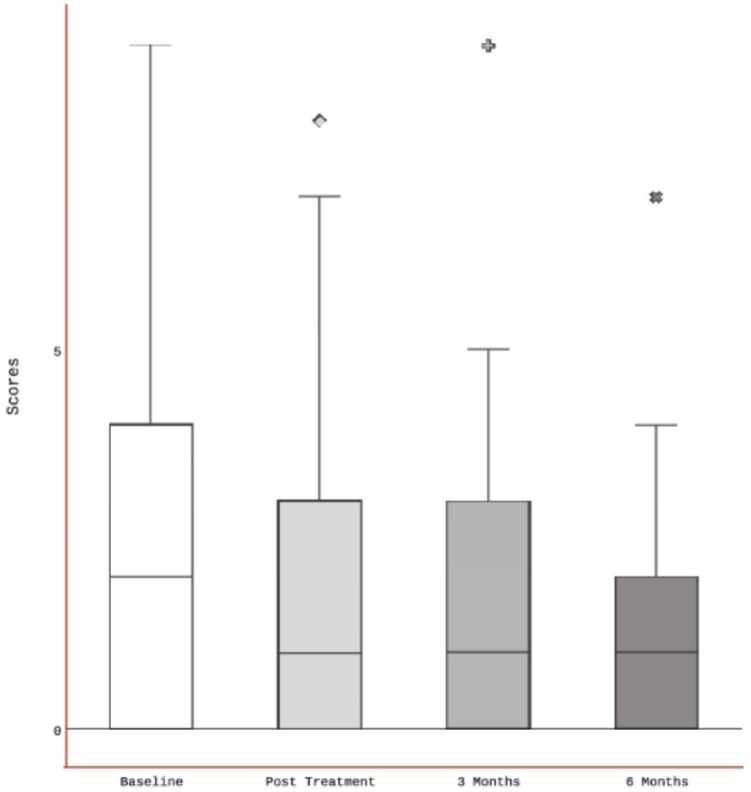
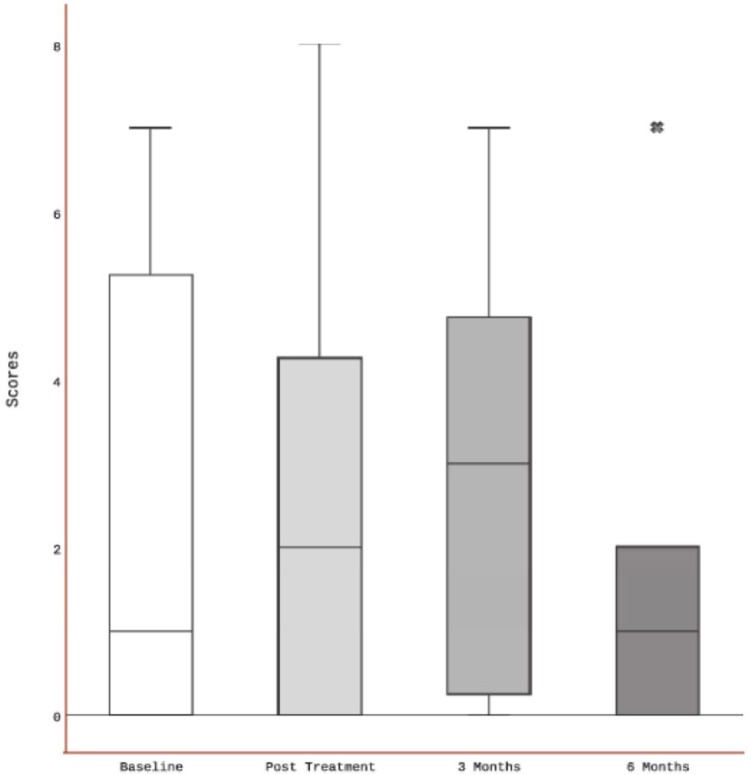
Figure 2.
Pain scores in patients who received ALTENS.
Abbreviation: ALTENS, acupuncture-like transcutaneous electrical nerve stimulation.
Analysis of the ESAS pain data failed to show statistically significant difference at 6 months from the baseline pain score; P = .138. However, in analysis of the imputed data, a significant difference was detected at 6 months; P = .0004. There was no significant difference detected in the analysis of the raw ESAS feeling of well-being scores at 6 months; P = .157. However, this was significant after analysis of the imputed data set; P = .03.
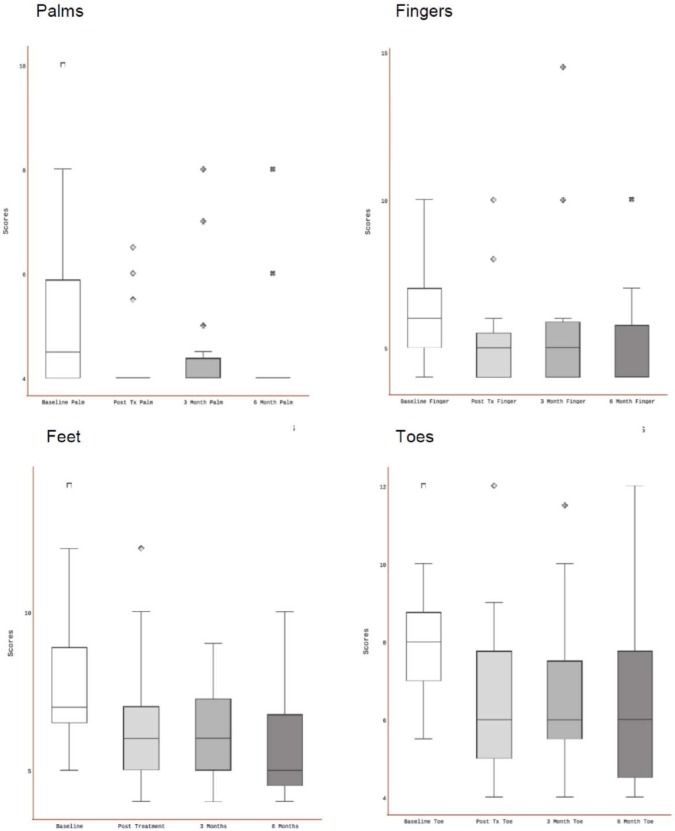
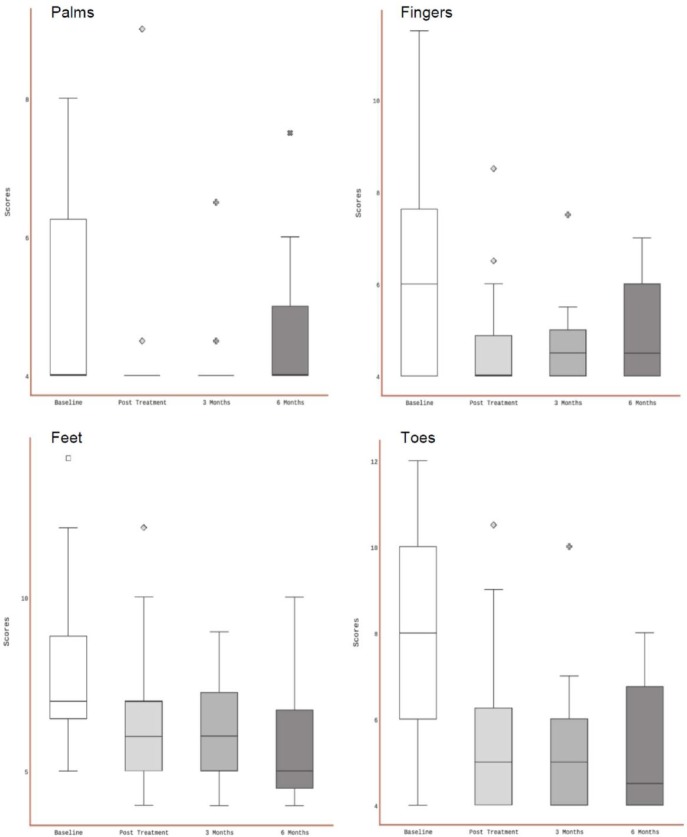
The numbness scores of patients who received ALTENS are shown in Figure 4. Numbness scores of all patients receiving ALTENS showed a significant reduction at 6 months compared with baseline. For the palm, finger, foot, and toe, P values were .0066, .0014, .0016, and .004, respectively. The numbness scores of the foot and toe remained higher than those of the hand and finger throughout the study period. The analysis of the imputed data consistently showed a significant improvement in numbness scores for all areas. The P values were .0002 and <.0001 for the palm and the other areas, respectively.
Figure 4.
Numbness scores of patients who received ALTENS.
Abbreviation: ALTENS, acupuncture-like transcutaneous electrical nerve stimulation.
For the 13 patients who received acupuncture treatments, the data were analyzed similarly. The mTNS scores of these patients are presented in Figure 5. The results showed that mTNS scores were improved at 6 months from the start of acupuncture treatments; P = .0414. After analysis of the imputed data, the differences remained significant; P = .0019.
Figure 5.
Total neuropathy scores in patients who received acupuncture.
Figure 6 shows the ESAS pain scores of patients who received acupuncture. There was no significant difference in the ESAS pain scores (data not shown) at 6 months in both raw and imputed data sets. P values were .6600 and .6823, respectively. Similarly, for the ESAS perception of well-being scores, there were no significant differences at 6 months for both the original and imputed data sets (Figure 7); P = .3913 and P = .1034, respectively.
Figure 6.
Pain scores in patients who received acupuncture.
Figure 7.
Feeling of well-being scores in patients who received acupuncture.
In analysis of the raw data sets, there were no significant differences at 6 months from baseline in the numbness scores of the palm, finger, and foot areas (P = .276, .2491, and .069, respectively). There was a detected significance of the scores in the toe areas; P = .015. However, in the imputed data sets, the numbness scores in all areas were improved significantly. P values were .0116, .001, .0056, and .0004 for the palm, finger, foot, and toe areas, respectively (Figure 8).
Figure 8.
Numbness scores in patients who received acupuncture.
Three patients in the ALTENS group reported a moderate aching discomfort at the stimulation sites during treatments. One developed mild skin rashes at one of the electrode sites. There were no side effects reported in the acupuncture group.
Discussion
This phase 2 study suggests that ALTENS can improve CIPN symptoms. The TNS scores at the 6-month follow-up of patients who received ALTENS were significantly reduced compared with baseline. Spontaneous symptom improvement could have occurred with time. However, from the reported literature, it is suggested that further symptom improvement after 6 months from the onset of CIPN is uncommon.2 Because our study patient population had a median symptom duration of 6 months from the onset of CIPN, the symptom improvement was likely accelerated by the ALTENS.
Although our patient sample size was small, we believe that the results obtained are valuable data in evaluating ALTENS as a modality in managing CIPN symptoms. Our results also show the significance and severity of numbness as a component of CIPN symptoms. Interestingly, pain was not a main complaint in the patients we studied. However, data regarding specific hyperalgesia or allodynia were not obtained. These symptoms may not have been captured by the ESAS scores. The baseline TNS scores of the studied patients were compatible with reports in the literature.
Numbness was significantly improved after ALTENS treatment. This finding suggests the occurrence of functional recovery of the myelinated A-beta and delta fibers that convey general touch and light touch sensation.15 The ALTENS electrical stimulation parameters have been shown to preferentially stimulate A-fibers and to result in the muscle contractions seen in ALTENS treatments.16 The observation that selective stimulation of A-fibers may induce functional improvement is clinically important.
We failed to demonstrate that ALTENS reduced pain at the 6-month follow-up assessment. Given that 14 out of the 27 patients reported a baseline pain score of 3 or less, the symptom of pain was not a significant complaint. Therefore, a detection of significant change may not occur with a small sample size, particularly in the presence of missing data. For the 13 patients who had baseline pain scores greater than 3, 10 had a reduction in scores at 6 months, 2 had no change in score, and 1 had an increase in score. These results suggest that patient-reported pain outcomes remain unclear.
To gauge the patients’ general quality of life, we analyzed the ESAS feeling of well-being scores. The study results were inconclusive in regard to the effectiveness of ALTENS on patients’ perception of well-being. The effect of missing data and the existence of multiple factors, apart from those of peripheral neuropathy, that could affect the sense of well-being may explain these results. The smaller sample size of patients treated with acupuncture clearly limited the interpretation of the study results. In this study, there was improvement in the TNS scores but not in the pain or perception of well-being scores at 6 months after acupuncture.
One of the obvious drawbacks in our study was the unanticipated higher number of patients lost to follow-up. Of the 27 patients recruited in the ALTENS group, there were only 23 patients who completed the assessment at the 6-month follow-up, amounting to 15% (4/27) lost to follow-up. However, the total number of evaluable patients still reached the planned number of patients for the ALTENS single-arm phase 2 evaluation. A future CIPN intervention study should allow for the 15% loss to follow-up rate.
The observed mild side effects of ALTENS treatment were similar to that reported in previous studies,6,17 supporting the low toxicity profile of this noninvasive treatment modality.
Conclusions
The results of our pilot study suggested that ALTENS is effective in reducing symptoms associated with CIPN. The TNSs were significantly improved at 6 months after 12 ALTENS treatments given within 6 to 8 weeks. Numbness of the extremities was significantly improved. This study provides data for the design of a phase 3 study, using a sham ALTENS control device, to assess the efficacy of this noninvasive treatment modality in managing this CIPN.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the Lotte & John Hecht Memorial Foundation, Vancouver, Canada.
References
- 1. Bhagra A, Rao RD. Chemotherapy-induced neuropathy. Curr Oncol Rep. 2007;9:290-299. [DOI] [PubMed] [Google Scholar]
- 2. Seretny M, Currie GL, Sena ES, et al. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain. 2014;155:2461-2470. [DOI] [PubMed] [Google Scholar]
- 3. Avan A, Postma TJ, Ceresa C, et al. Platinum-induced neurotoxicity and preventive strategies: past, present, and future. Oncologist. 2015;20:411-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim JH, Dougherty PM, Abdi S. Basic science and clinical management of painful and non-painful chemotherapy-related neuropathy. Gynecol Oncol. 2015;136:453-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Franconi G, Manni L, Schröder S, Marchetti P, Robinson N. A systematic review of experimental and clinical acupuncture in chemotherapy-induced peripheral neuropathy. Evid Based Complement Alternat Med. 2013;2013:516916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wong RKW, James JL, Sagar S, et al. Phase 2 results from Radiation Therapy Oncology Group Study 0537: a phase 2/3 study comparing acupuncture-like transcutaneous electrical nerve stimulation versus pilocarpine in treating early radiation-induced xerostomia. Cancer. 2012;118:4244-4252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Laitinen J. Acupuncture and transcutaneous electric stimulation in the treatment of chronic sacrolumbalgia and ischialgia. Am J Chin Med. 1976;4:169-175. [DOI] [PubMed] [Google Scholar]
- 8. Fargas-Babjak AM, Pomeranz B, Rooney PJ. Acupuncture-like stimulation with codetron for rehabilitation of patients with chronic pain syndrome and osteoarthritis. Acupunct Electrother Res. 1992;17:95-105. [DOI] [PubMed] [Google Scholar]
- 9. Fox EJ, Melzack R. Transcutaneous electrical stimulation and acupuncture: comparison of treatment for low-back pain. Pain. 1976;2:141-148. [PubMed] [Google Scholar]
- 10. Pomeranz B, Niznik G. Codetron, a new electrotherapy device overcomes the habituation problems of conventional TENS devices. Am J Electromed. 1987;2:22-26. [Google Scholar]
- 11. Wampler M, Miaskowski C, Hamel K, Byl N, Rugo H, Topp K. The modified total neuropathy score: a clinical feasible and valid measure of taxane-induced peripheral neuropathy in women with breast cancer. J Support Oncol. 2006;4:9-16. [Google Scholar]
- 12. Kamei N, Yamane K, Nakanishi S, et al. Effectiveness of Semmes-Weinstein monofilament examination for diabetic peripheral neuropathy screening. J Diabetes Complications. 2005;19:47-53. [DOI] [PubMed] [Google Scholar]
- 13. Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7(2):6-9. [PubMed] [Google Scholar]
- 14. Walters SJ. Quality of Life Outcomes in Clinical Trials and Health-Care Evaluation: A Practical Guide to Analysis and Interpretation. New York, NY: Wiley; 2009. [Google Scholar]
- 15. Guyton AC. Structure and Function of the Nervous System. Philadelphia, PA: W B Saunders; 1976. [Google Scholar]
- 16. Watson T. Key concepts with electrophysical agents. Phys Ther Rev. 2010;15:351-359. [Google Scholar]
- 17. Wong RK, Deshmukh S, Wyatt G, et al. Acupuncture-like transcutaneous electrical nerve stimulation versus pilocarpine in treating radiation-induced xerostomia: results of RTOG 0537 phase 3 study. Int J Radiat Oncol Biol Phys. 2015;92:220-227. [DOI] [PMC free article] [PubMed] [Google Scholar]