Abstract
Objective. The aim of this study was to determine the feasibility, acceptability, and safety of using moxibustion for treating anorexia and improving quality of life in patients with metastatic cancer. Methods. We conducted a randomized sham-controlled trial of moxibustion. Sixteen patients with metastatic cancer were recruited from Daejeon, South Korea. The patients were randomly placed into a true or a sham moxibustion group and received 10 true or sham moxibustion treatments administered to the abdomen (CV12, CV8, CV4) and legs (ST36) over a 2-week period. Outcome measures included interest in participating in the trial, identification of successful recruitment strategies, the appropriateness of eligibility criteria, and compliance with the treatment plan (ie, attendance at treatment sessions). Clinical outcomes included results of the Functional Assessment of Anorexia/Cachexia Therapy (FAACT), answers on the European Organization for Research and Treatment of Cancer 30-item core quality of life (EORTC QLQ-C30) questionnaires, scores on the visual analogue scale (VAS), and the results from blood tests and a safety evaluation. Results. Moxibustion was an acceptable intervention in patients with metastatic cancer. Compliance with the treatment protocol was high, with 11 patients completing all 10 treatments. No serious adverse events related to moxibustion occurred, but 4 patients in the true moxibustion group reported mild rubefaction, which disappeared in a few hours. Conclusion. This study suggests that moxibustion may be safely used to treat anorexia and improve quality of life in patients with metastatic cancer. However, further research is needed to confirm this result.
Keywords: moxibustion, metastatic cancer, anorexia, quality of life, feasibility study
Introduction
Moxibustion is a noninvasive procedure that involves burning moxa, the herb Artemisia vulgaris, on or above the skin at acupoints so as to warm the acupoints in order to alleviate symptoms.1 The therapeutic components of moxibustion are assumed to be heat, tar, aroma, psychological stress, and combinations thereof.2 Among them, heat stimulation and the chemical action of the ignited moxa are the most important variables for moxibustion.3 Moxibustion has been widely used for various reasons, including the treatments of cancer, ulcerative colitis, constipation, hypertension, and pain, as well as, stroke rehabilitation and facilitation of breech presentation.4
Patients with cancer require support to cope with the disease, its symptoms, and the side effects of treatment with surgery, radiation therapy, and chemotherapy. Also, interest in the investigation of moxibustion for treating cancer-related symptoms has continued,5(pp83-120, pp223-248). and according to the systematic review by Lee et al6 of moxibustion for cancer care, 2 randomized controlled trials demonstrated that moxibustion was beneficial for treating nausea and vomiting in patients with cancer. Moreover, moxibustion has been shown to be a safe and potentially effective modality for treating cancer-related pain in patients with metastatic cancer.7
Anorexia—defined as a loss of appetite—is a symptom with high prevalence in patients with cancer.8 Anorexia in patients with cancer has several causes, such as the stress from the cancer diagnosis,9 cancer-related inflammatory responses and changes in the hypothalamic function, all of which may impact appetite.8,10 Moreover, antitumor treatments, such as chemotherapy or radiotherapy, may negatively affect appetite.11 The prognosis for patients with cancer is adversely affected by the presence of anorexia as it limits food intake and, in combination with cancer cachexia, induces the wasting of muscles and the loss of weight, eventually leading to increased morbidity and mortality.8 Thus, anorexia in patients with cancer is significantly correlated with unsatisfactory health and physical function.12
Moxibustion has been widely used to treat chronic diseases because of the efficacy of thermal energy in the prevention of disease. Now, it is often used in clinics to improve immune function, combat fatigue, reduce edema, and reduce mortality.13(pp661-697) In Korea, moxibustion has often been clinically used at acupoints on the abdomen and the extremities to treat cancer-related anorexia,13,14(p173, pp280-284) but, to the best of the authors’ knowledge, no objective studies have addressed that use. Thus, in this study, we aimed to determine the feasibility, acceptability and safety of using moxibustion for treating anorexia and improving quality of life in patients with metastatic cancer.
Methods
Trial Design
A randomized sham-controlled feasibility study was conducted in which true moxibustion was compared with sham moxibustion. The intervention lasted 2 weeks.
Participants
The patients were recruited through recruitment posters placed inside Dunsan Korean Medicine Hospital of Daejeon University from February 2015 to September 2015. Eligibility criteria were age 19 years or older, histologically or cytologically documented cancer, radiologically diagnosed metastatic cancer, a complaint of more than 40 mm when the degree of anorexia was evaluated by using the 100-mm visual analogue scale (VAS), and Eastern Cooperative Oncology Group (ECOG) performance status ≤2; in addition, patients had to have volunteered to participate in this clinical study and to have provided informed consent. Exclusion criteria were intention to receive chemotherapy or radiotherapy during the study period, intention to receive chemotherapy or radiotherapy in the 4 weeks prior to the study, the existence of local skin problems at or near the moxibustion sites, inability for oral intake, severe insomnia or depression, the existence of diseases that could influence the appetite, such as hypoadrenalism, and so on, and having taken or intending to take appetite-enhancing drugs, such as megestrol acetate, corticosteroids, and others. In addition, those judged not to be able to participate appropriately in this clinical study were excluded. Informed consent was obtained from all patients before enrollment, and the study protocol was approved by the institutional review board at Dunsan Korean Medicine Hospital of Daejeon University (protocol registered on www.cris.nih.go.kr KCT0001155: https://cris.nih.go.kr/cris/en/search/search_result_st01.jsp?seq=5692).
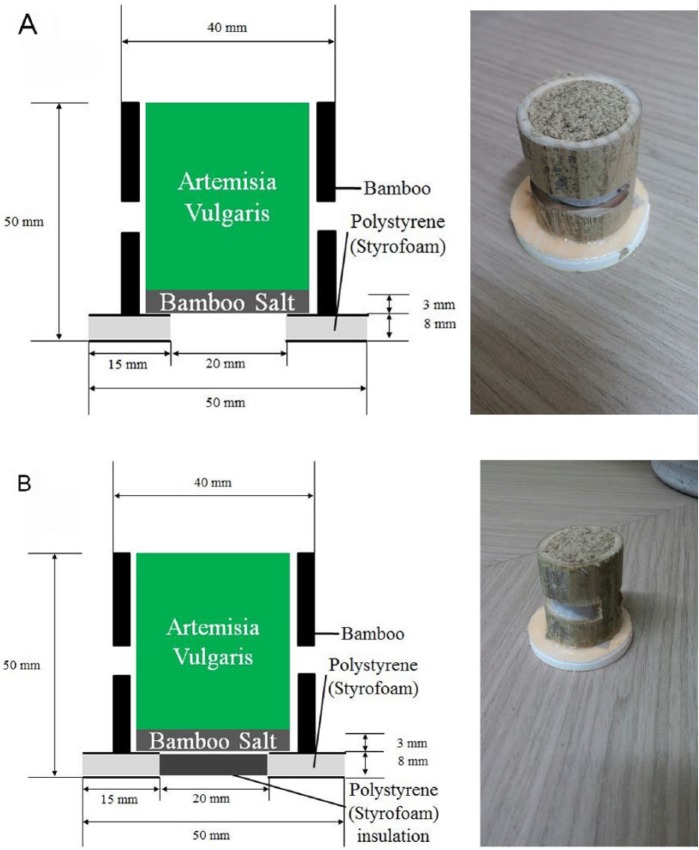
True and Sham Moxibustion Device
We used a commercially available moxibustion device (Guo-Ku Industrial Co Ltd, Gimpo, Korea). The moxibustion device had a cylindrical shape and was covered with pipes measuring 4 cm in diameter and 5 cm in height. The pipes were packed with bamboo salt from the bottom to a height of 3 mm. The remainder of the pipes above the bamboo salt were filled with dried mugwort. Polystyrene (Styrofoam) insulation was placed under the pipes for application to the skin, which is an indirect type of moxibustion (Figure 1). The sham moxibustion device was the same as the true moxibustion device, but 8 mm of Styrofoam insulation was used in order to prevent heat and smoke from getting to the skin (Figure 1).
Figure 1.
Diagrams of the true and the sham moxibustion devices. The true and the sham moxibustion devices appear to be identical. (A) The true moxibustion has holes at the bottom to allow heat and smoke to radiate to the acupoints. (B) The sham moxibustion has polystyrene (Styrofoam) insulation at its base to block heat and smoke from getting to the acupoint.
Intervention
Five acupoints, CV12, CV8, CV4, and bilateral ST36, were selected for the treatment (Figure 2). These acupoints, which are located in the abdomen (CV12, CV8, CV4) and legs (ST36) and which are known to useful for treating anorexia, vomiting, abdominal pain, and so on,1 are widely used in South Korea.13,14 The participants were in the supine position during treatments and were treated with true or sham moxibustion 5 times per week for 2 weeks (total of 10 times). Patients in both groups were treated at the same 5 acupoints (CV12, CV8, CV4, and ST36). Two moxibustion devices were burned at each point for about 40 minutes; that is, after 1 moxibustion had been burned for about 20 minutes, another moxibustion was burned for another 20 minutes. Moxibustion was administered by Korean medicine doctors who had 2 or more years of clinical experience practicing moxibustion therapy. During each treatment, the procedure was carefully monitored by practitioners to prevent any adverse events related to moxibustion, and all vital signs and any changes in medical history were determined at each visit. After each treatment, the practitioner returned the box with burned moxibustion pillars to a box keeper, who was responsible for disposing of the used devices and was unable to identify the patients treated.
Figure 2.

Five acupoints (CV12, CV8, CV4, and bilateral ST36) were used for moxibustion in this trial (the patient approved the use of this photograph).
Outcome Measures
Outcome measures included interest in participation in the trial, identification of successful recruitment strategies, the appropriateness of eligibility criteria and compliance with treatment protocol (attendance at the scheduled treatments). Clinical outcomes included answers on the Functional Assessment of Anorexia/Cachexia Therapy (FAACT) and the European Organization for Research and Treatment of Cancer 30-item core quality of life (EORTC QLQ-C30) questionnaires, scores on the visual analogue scale (VAS), and the results from blood tests and a safety evaluation.
To evaluate the degree of anorexia, we used the FAACT and the EORTC QLQ-C30 questionnaires and the VAS. The FAACT questionnaire is specifically used to evaluate both the quality of life for cancer patients and anorexia-/cachexia-related concerns, the EORTC QLQ-30 questionnaire is generally used to evaluate various cancer-related symptoms, and the VAS is a convenient way to check the degree of anorexia. To determine quality of life, we used the FAACT and the EORTC QLQ-C30 questionnaires. The answers on the FAACT and the EORTC QLQ-C30 questionnaires, as well as the VAS scores, were collected and evaluated at baseline (visit 1), after the 5th moxibustion treatment (visit 6), and after the 10th moxibustion treatment (visit 11) (Table 1).
Table 1.
Study Schedule and Outcome Measures.
| Screening | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit → | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| Week | ←━ ━ ━1st week━ ━ ━→ | ←━ ━ ━2nd week━ ━ ━→ | |||||||||
| Informed consent | ✓ | ||||||||||
| Demographic characteristics | ✓ | ||||||||||
| FAACT | ✓ | ✓ | ✓ | ||||||||
| EORTC QLQ-C30 | ✓ | ✓ | ✓ | ||||||||
| Anorexia VAS | ✓ | ✓ | ✓ | ||||||||
| Blood test | ✓ | ✓ | |||||||||
| Inclusion/exclusion decision | ✓ | ||||||||||
| Random allocation | ✓ | ||||||||||
| Moxibustion treatment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Safety assessment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
Abbreviations: FAACT, Functional Assessment of Anorexia/Cachexia Therapy; EORTC QLQ-C30, European Organization for Research and Treatment of Cancer 30-item core quality of life.
The patients were asked to complete a FAACT questionnaire (version 4).15 The FAACT questionnaire was designed to complement the Functional Assessment of Cancer Therapy–General (FACT-G) by addressing anorexia/cachexia-related concerns. The FACT-G is a validated 27-item, patient-rated measure of quality of life for patients with cancer of any type. It covers the areas of physical well-being (7 items), social/family well-being (7 items), emotional well-being (6 items), and functional well-being (7 items). In addition to the FACT-G items, the FAACT has 12 additional items under the anorexia/cachexia subscale (ACS) category. All FAACT items are scored from 0 = “not at all” to 4 = “very much,” so the total score ranges from 0 to 156. Higher scores imply a better state of the patient. The EORTC QLQ-C30 questionnaire (version 3) was used.16 The EORTC QLQ-C30 questionnaire is composed of both multi-item scales and single-item measures. These include 5 functional scales, 3 symptom scales, a global health status/QOL scale, and 6 single items. The EORTC QLQ-C-30 assesses global quality of life, functional domains (physical, emotional, social, role, and cognitive) and symptoms (fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulty), which commonly occur in patients with cancer. All of the scales and the single-item measures range in score from 0 to 100. A high score on a functional scale represents a high/healthy level of function, and a high score for global health status/quality of life represents a high quality of life, but a high score on the symptom scale represents a high level of symptomatology. The score on the VAS anorexia scale, which ranged from 0 mm = normal appetite to 100 mm = no food intake possible, was also used.17
Moxibustion acceptability was evaluated by using the answers to brief questions to determine the patients’ likes or dislikes concerning both the moxibustion treatment and the study. The safety of this study was determined by using the numbers and the types of adverse events, such as burns and infections at the moxibustion site, coughing, headaches, allergic reactions related to the moxa or the moxibustion smoke, and so on, at each visit. Also, blood tests, including white blood cells, neutrophils, platelets, C-reactive protein, and fibrinogen, were done to ensure safety. Blood test results were collected at baseline (visit 1) and after the 10th moxibustion treatment (visit 11) (Table 1).
Study Size and Statistical Analysis
Our initial aim was to recruit 20 patients for this study: 10 patients in the true moxibustion group and 10 patients in the sham moxibustion group. However, we only managed to recruit 16; 9 in the true moxibustion group and 7 in the sham moxibustion group. No power analysis was undertaken for this feasibility study. The purpose of this study was not to establish efficacy, but to carefully measure the effect of moxibustion in a small sample and to test the safety, feasibility and acceptability of using moxibustion to treat anorexia in patients with metastatic cancer. The data analysis was blind to the study group. The outcome analysis was based mainly on the intention to treat (ITT) and was undertaken per-protocol (PP). Baseline demographic and clinical characteristics were summarized, and comparisons of the clinical endpoints were made between groups by using nonparametric statistics. The level of significance was set at .05.
Randomization
A random number allocation sequence was generated by using the SPSS 21 statistical software package. Eligible patients were randomly distributed into the true moxibustion or the sham moxibustion treatment group via a random permuted block of size 20 in a ratio of 1:1. This was done to help reduce the predictability associated with a conventional balanced block randomization, for which the patient, at the end of each block, might be able to predict the next treatment. The randomization schedule was concealed in sequentially numbered, opaque, sealed envelopes by a researcher independent of the study.
Results
From February to October 2015, 16 of the patients responding to the posters placed inside the hospital in an attempt to recruit volunteers were included in this study based on the eligibility and the exclusion criteria described above. These 16 patients had already had experience with acupuncture and moxibustion treatment and had been subjected to 2 screenings: a prescreening with short questions and answers and a more thorough and comprehensive main screening. The patients were randomized into either the true moxibustion group (n = 9) or the sham moxibustion group (n = 7). Compliance with the treatment protocol was relatively high (75.625%), with 11 of the 16 patients completing all treatments. Five participants of the true moxibustion group dropped out for the following reasons: other hospital treatment (1), commuting difficulties (1), personal reasons (1), and poor physical condition (“not myself today” or “not feeling good”) (2). The flowchart for the study is presented in Figure 3.
Figure 3.
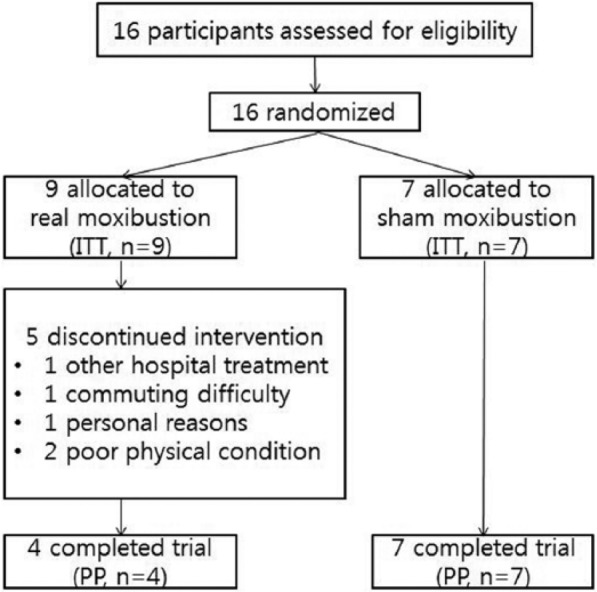
Flowchart for this study. ITT, intention to treat; PP, per protocol.
Eleven of the participants were women and 5 were men. The patients were mostly in their late 50s or early 60s and were of average weight (mean of body mass indices of 19.7 and 20.6 kg/m2, respectively, in the true and the sham moxibustion groups). The demographic data and the baseline characteristics of the patients are shown in Table 2. No statistically significant differences between the true and the sham moxa groups in terms of descriptive characteristics were noted. The types of cancer and metastatic lesions are shown in Table 3 by patient.
Table 2.
Demographic Information and Baseline Characteristics.
| True Moxibustion (n = 9) | Sham Moxibustion (n = 7) | |
|---|---|---|
| No. of participants | 9 | 7 |
| Sex, n | ||
| Male | 1 | 4 |
| Female | 8 | 3 |
| Age, years | 63.3 ± 8.3 | 57.3 ± 12.0 |
| Weight, kg | 47.6 ± 4.9 | 56.1 ± 11.6 |
| Height, cm | 156.2 ± 9.2 | 165.9 ± 8.1 |
| Body mass index, kg/m2 | 19.7 ± 3.0 | 20.6 ± 5.2 |
| Anorexia-cachexia subscale in FAACT | 14.67 ± 9.73 | 26.57 ± 9.50 |
| FAACT | 70.44 ± 23.84 | 83.48 ± 22.22 |
| Appetite loss in EORTC QLQ-C30 | 85.19 ± 24.22 | 57.14 ± 31.71 |
| General health status in EORTC QLQ-C30 | 27.78 ± 22.82 | 32.14 ± 22.79 |
| Anorexia VAS, mm | 72.00 ± 18.78 | 57.43 ± 11.34 |
Abbreviations: FAACT, Functional Assessment of Anorexia/Cachexia Therapy; EORTC QLQ-C30, European Organization for Research and Treatment of Cancer 30-item core quality of life; VAS, visual analogue scale.
Table 3.
Patients’ Cancer Type and Metastatic Lesions.
| Cancer Type and Metastatic Lesions | |
|---|---|
| True moxa group patient number | |
| 1 | Ampulla of Vater cancer, metastasized to liver |
| 2 | Common bile duct cancer, metastasized to colon |
| 3 | Pancreatic cancer, metastasized to peritoneum, lung |
| 4 | Colon cancer, metastasized to lung, peritoneum |
| 5 | Hepatocellular carcinoma, metastasized to lymph nodes in liver |
| 6 | Colon cancer, metastasized to lung, peritoneum |
| 7 | Pancreatic cancer, metastasized to liver |
| 8 | Hepatocellular carcinoma, metastasized to lymph nodes in liver |
| 9 | Ovarian cancer, metastasized to peritoneum, uterus, diaphragm |
| Sham moxa group patient number | |
| 1 | Ovarian cancer, metastasized to both ovaries, uterus, cecum, small intestine, peritoneum, liver |
| 2 | Pancreatic cancer, metastasized to common bile duct, lymph nodes |
| 3 | Uterine cervical cancer, metastasized to lung |
| 4 | Lung cancer, metastasized to bone |
| 5 | Lung cancer, metastasized to liver, bone |
| 6 | Ovarian cancer, metastasized to omentum, diaphragm, peritoneum, liver |
| 7 | Gastric cancer, metastasized to peritoneum, small intestine, descending colon |
Generally, the moxibustion treatment met the expectations of the patients who participated in this study. Most patients stated that moxibustion might have helped improve their anorexia to some degree while other answered that they were uncertain of its effect. During the study period, some patients felt uncomfortable due to the moxa smoke, and some patients complained of redness of the skin although that disappeared in a few hours. Some patients complained about the uncomfortable posture during treatment because lying on their backs for 40 minutes without movement caused back pain and muscle tension. Another thing that bothered the patients was the tight schedule. In this study, patients were required to visit the hospital 5 times a week for 2 weeks (total 10 times) because of the short study period. We were concerned that the patients might tire of the treatment or have trouble meeting the treatment schedule, and actually, 1 patient did drop out due to commuting difficulties.
Preliminary data from this study indicated that moxibustion was potentially effective for treating anorexia and improving quality of life in patients with metastatic cancer. After 10 sessions of treatment, the patients in the true moxibustion group showed lesser degrees of anorexia and appetite loss on the anorexia-cachexia subscale of the FAACT questionnaire and on the EORTC QLQ questionnaire, respectively. Additionally, the true moxibustion group showed less fatigue, nausea and vomiting, and pain, and lower diarrhea scores on the EORTC QLQ questionnaire. No remarkable changes were noted in the scores on the VAS and the results of the blood tests.
No serious adverse events related to moxibustion occurred during study. Four patients in the true moxibustion group reported mild rubefaction, but the symptom quickly disappeared within 1 or 2 hours after moxibustion.
Discussion
In this feasibility study, we found that moxibustion was an acceptable intervention for treating anorexia in patients with metastatic cancer. However, recruitment of patients was not successful (only 16 were recruited vs the original goal of 20), which might have been caused by the lack of recruitment strategies, including social and multimedia approaches. When planning a future study of moxibustion for treating anorexia in patients with cancer, various recruitment methods, such as newspaper advertising, referrals from health professionals, contact with patient community groups, and so on, should be used. In addition, future studies should be multicenter trials when possible.
Despite an intensive moxibustion treatment schedule requiring attendance 10 times over 2 weeks and 40 minutes for each treatment, compliance with the study protocol was relatively good, and the patients faithfully completed the questionnaires during the study period. We originally planned a total of 10 moxibustion treatments of 40 minutes each so that we could compare our conclusion with that of an earlier study, which found that increasing the amount of burning moxa per unit time could significantly improve lingering effects.18 Because this study had to be completed within 8 months and because the patients were to undergo treatment individually, the treatment protocol called for 5 treatments per week for 2 weeks per patients. Based on patient input, we found that the treatment schedule (5 times a week for 2 weeks) was too tight and was a contributing factor in the dropout rate. We also found that the long treatment time (40 minutes per session) imposed a heavy strain on the patients’ body, especially patients who had thin body shapes or chest/abdominal discomfort. When planning a future study of moxibustion for the treatment of patients with metastatic cancer, the treatment time should be less than 40 minutes if possible, and a less restrictive schedule of treatments should be considered. Additionally this study was a feasibility study and lacked follow-up. Future trials to investigate the efficacy of moxibustion for treating anorexia and improving quality of life in patient with metastatic cancer should include follow-up.
Although moxibustion was acceptable to the patients who participated in this study, 5 patients dropped out. We think that was due to the short recruitment and treatment schedules. Also, when we recruited and enrolled patients at the baseline, our exclusion criteria did not include personal reasons, such as (busy schedule, commuting time, personal problems, unstable and moody personalities, etc) or health problems necessitating simultaneous treatments at other hospitals. We included any patient with cancer-related symptoms such as mild fatigue, ennui, indigestion, and so on. During the study, 2 patients stopped treatment reportedly for reasons of poor physical condition (not feeling good today). This “not feeling good today” might have 2 origins: Patients with cancer-related symptoms might feel too tired when trying to keep the tight treatment schedule and might be influenced by mood swings. A further analysis of the dropout rate found that patients who dropped out had personal reasons or other scheduled hospital treatment schedule, not that they felt uncomfortable or dissatisfied with the moxibustion treatment. Unfortunately, the high dropout rate occurred in the true moxibustion group. Thus, future studies should consider these factors during the planning stage.
Evidence from sham-controlled trials of moxibustion for treating the symptoms of cancer is very important.19 Sham moxibustion devices can be divided into 2 categories: those for treatment at non-acupuncture points and those for preventing heat stimulation of acupuncture points, each having its pros and cons. Recent studies on sham moxibustion20,21 used the latter category of device and successfully validated it use. Thus, in this study, we used a sham moxibustion device that blocked heat stimulation in a similar way. Also, sham moxibustion was used only after practitioners had confirmed that sufficient insulation was present. The moxa device is safe because the heat is moderated by bamboo salt and the heat in the bottom of the moxa is not high enough to affect the polystyrene surface. More studies to develop a convenient, effective, and safe sham moxibustion method are needed.
No serious adverse events related to moxibustion treatment occurred during this study. Though four patients reported mild rubefaction, they recovered rapidly in a matter of a few hours. Park et al22 reported burns, allergic reactions, and infections as potential adverse events of moxibustion. However, in our opinion, these can be avoided by using indirect moxibustion and careful observation by the practitioner.
At present, treatment guidelines and pilot studies on the use of moxibustion for treating patients with cancer-related anorexia do not exist. In this study, we used moxibustion at the CV4, CV8, CV12, and ST36 acupoints, which are frequently used clinically in Korea to reduce dyspepsia, nausea and vomiting, general body weakness, and anorexia, to treat patients with metastatic cancer.13,14 Regarding acupoints for the treatment of anorexia, one report indicated that moxibustion at ST21 and ST36 significantly decreased gastric injury and apoptosis of gastric mucosal cells in rats with stress-induced ulcers23 and that moxibustion at CV8 reduced chemotherapy-induced nausea and vomiting in patients with a nasopharyngeal carcinoma or gastric cancer.24 Also, moxibustion at ST36 and CV4 has been reported to improve cancer-related fatigue.25 Aung et al recommended moxibustion at PC6, ST34, ST36, and CV12 to prevent nausea and vomiting, moxibustion at CV4 to improve general condition, energy and wellness, and moxibustion at ST36 to reduce general fatigue in patients with cancer. Also, moxibustion at CV12 is useful for treating generalized Fu organ dysfunction, and moxibustion at ST36 is useful for treating chronic stomach disorders.5 More discussion on the selection of acupoints when using moxibustion to treat patients with metastatic-cancer-related anorexia is encouraged.
Interestingly, the cancer-related symptoms of fatigue, nausea and vomiting, pain, and diarrhea, as well as cancer-related anorexia, were alleviated after 10 true moxibustion treatments, but the same effects were not observed in the sham moxibustion group. These results are similar to those of preceding studies.7,24,26,27 In this feasibility study, we did not aim to evaluate the effect of moxibustion for treating anorexia, improving the quality of life, and alleviating the symptoms in patient with metastatic cancer; neither did we aim to determine the mechanisms behind the effects of moxibustion. Thus, further studies of these topics are necessary.
Conclusion
Anorexia is common in patients with metastatic cancer and is often associated with increased morbidity and mortality. Our study suggests that moxibustion may be effective and safe in treating anorexia and improving the quality of life in patients with metastatic cancer. However, further studies are required to confirm these findings and to identify the underlying mechanisms.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by grant of Korean Ministry of Health & Welfare, Republic of Korea (Project No. : CIMI-14-01-23).
References
- 1. Lao L. Traditional Chinese medicine: part III. In: Jonas WB, Levin JS. eds. Essentials of Complementary and Alternative Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:219-232. [Google Scholar]
- 2. Yamashita H, Ichiman Y, Tanno Y. Changes in peripheral lymphocyte subpopulations after direct moxibustion. Am J Chin Med. 2001;29:227-235. [DOI] [PubMed] [Google Scholar]
- 3. Im ST, Kim KH, Kim KS. A study of physical characteristics of moxibustion. J Korean Acupunt Moxibust Soc. 1994;11:327-336. [Google Scholar]
- 4. Lee MS, Kang JW, Ernst E. Does moxibustion work? An overview of systematic reviews. BMC Res Notes. 2010;3:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cho WC. Acupuncture and Moxibustion as an Evidence-Based Therapy for Cancer. New York, NY: Springer; 2012. [Google Scholar]
- 6. Lee MS, Choi TY, Park JE, Lee SS, Ernst E. Moxibustion for cancer care: a systematic review and meta-analysis. BMC Cancer. 2010;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee J, Yoon SW. Efficacy and safety of moxibustion for relieving pain in patients with metastatic cancer: a pilot, randomized, single-blind, sham-controlled trial. Integr Cancer Ther. 2013;13:211-216. [DOI] [PubMed] [Google Scholar]
- 8. Laviano A, Meguid MM, Rossi-Fanelli F. Cancer anorexia: clinical implications, pathogenesis, and therapeutic strategies. Lancet Oncol. 2003;4:686-694. [DOI] [PubMed] [Google Scholar]
- 9. Holland JCB, Rowland J, Plumb M. Psychological aspects of anorexia in cancer patients. Cancer Res. 1977;37:2425-2428. [PubMed] [Google Scholar]
- 10. Argiles JM, Busquets S, Toledo M, Lopez-Soriano FJ. The role of cytokines in cancer cachexia. Curr Opin Support Palliat Care. 2009;3:163-168. [DOI] [PubMed] [Google Scholar]
- 11. von Meyenfeldt M. Cancer-associated malnutrition: an introduction. Eur J Oncol Nurs. 2005;9(suppl 2):S35-S38. [DOI] [PubMed] [Google Scholar]
- 12. Lis CG, Gupta D, Grutsch JF. Can anorexia predict patient satisfaction with quality of life in advanced cancer? Support Care Cancer. 2009;17:129-135. [DOI] [PubMed] [Google Scholar]
- 13. Korean Society of Acupuncture. Acupuncture and Moxibustion. Seoul, Korea: Jipmoon Publishing; 2012. [Google Scholar]
- 14. Daejeon Korean Medicine University 11st Alumni Group. Appropriate Use of Acupuncture and Moxibustion (鍼灸準用). Seoul, Korea: Eui Sung Dang Publishing; 1999. [Google Scholar]
- 15. Functional Assessment of Chronic Illness Therapy. FACIT. 2010. http://www.facit.org/. Accessed May 30, 2016.
- 16. Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-376. [DOI] [PubMed] [Google Scholar]
- 17. Stubbs RJ, Hughes DA, Johnstone AM, et al. The use of visual analogue scales to assess motivation to eat in human subjects: a review of their reliability and validity with an evaluation of new hand-held computerized systems for temporal tracking of appetite ratings. Br J Nutr. 2000;84:405-415. [DOI] [PubMed] [Google Scholar]
- 18. Deng H, Shen X. The mechanism of moxibustion: ancient theory and modern research. Evid Based Complement Alternat Med. 2013;2013:379291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhao BX, Chen HY, Shen XY, Lao L. Can moxibustion, an ancient treatment modality, be evaluated in a double-blind randomized controlled trial? A narrative review. J Integr Med. 2014;12:131-134. [DOI] [PubMed] [Google Scholar]
- 20. Zhao L, Cheng K, Wang L, et al. Effectiveness of moxibustion treatment as adjunctive therapy in osteoarthritis of the knee: a randomized, double-blinded, placebo-controlled clinical trial. Arthritis Res Ther. 2014;16(3):R133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Park JE, Sul JU, Kang K, Shin BC, Hong KE, Choi SM. The effectiveness of moxibustion for the treatment of functional constipation: a randomized, sham-controlled, patient blinded, pilot clinical trial. BMC Complement Altern Med. 2011;11:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Park JE, Lee SS, Lee MS, Choi SM, Ernst E. Adverse events of moxibustion: a systematic review. Complement Ther Med. 2010;18:215-223. [DOI] [PubMed] [Google Scholar]
- 23. Yi SX, Peng Y, Chang XR, Peng N, Yan J, Lin YP. Effect of pre-moxibustion on apoptosis and proliferation of gastric mucosa cells. World J Gastroenterol. 2007;13:2174-2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chen K, Jiang Y, Wen H, et al. Clinical study on treatment of nasopharyngeal carcinoma by radio and chemotherapy with supplementary moxibustion on Shenque point. Chin J Integr Med. 2000;20:733-735. [PubMed] [Google Scholar]
- 25. Vickers AJ, Straus DJ, Fearon B, Cassileth BR. Acupuncture for postchemotherapy fatigue: a phase II study. J Clin Oncol. 2004;22:1731-1735. [DOI] [PubMed] [Google Scholar]
- 26. Cao JX, Xiao XH, Tang XY. Elemene fluorouracil Moxibustion “Shenque” effect in the treatment of advanced gastric cancer observed. Chin J Clin Oncol. 1997;24:549-550. [Google Scholar]
- 27. de Valois BA, Young TE, Melsome E. Assessing the feasibility of using acupuncture and moxibustion to improve quality of life for cancer survivors with upper body lymphedema. Eur J Oncol Nurs. 2012;16:301-309. [DOI] [PubMed] [Google Scholar]