Abstract
Chronic nonbacterial prostatitis/chronic pelvic pain syndrome is unsatisfactorily defined and insufficiently studied illness. Also, the treatment success is questionable and therefore, this illness is a therapeutical problem for urologists - which medications are the best choice in treating this uncomfortable condition?
This paper presents results of prospective, open, analytical, comparative study that was performed on 90 patients with diagnosed chronic nonbacterial prostatitis/chronic pelvic pain syndrome. Patients were divided into three groups and were treated with two medications ciprofloxacin (C), doxazosin (D) and combination of ciprofloxacin + doxazosin (C+D). The effects were measured using symptom questionnaire for prostate illnesses of the National Institute for Health - USA (NIH-CPSI). During the basic evaluation, sum ranging from 0 to 43 was calculated for each patient. This number is called total sum NIH-CPSI (National Institutes of Health Chronic Prostatitis Symptom Index) of the questionnaire, which generates the questions from 1 to 9.
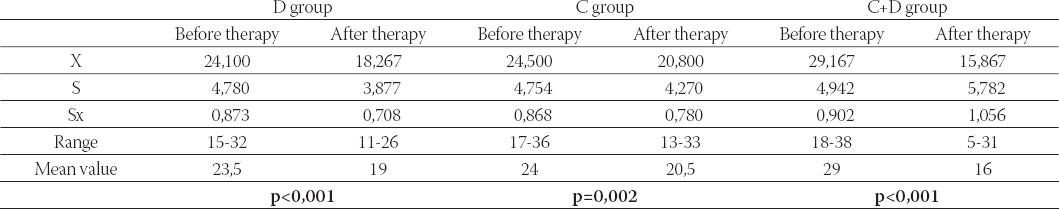
The most significant change occurred in C+D group where the total sum changed from 18-38 in the beginning to 5-31 at the end of the treatment (55,1% (p<0,001)). Significant changes were also found in D group where the change was 46, 4% (p<0,001). At the end of the treatment no significant change was registered in C group (p<0,005): p<0,001 – significance threshold. Combination of ciprofloxacin + doxazosin proved to be the best choice for treatment.
Keywords: chronic nonbacterial prostatitis/chronic pelvic pain syndrome, therapy
INTRODUCTION
Chronic prostatitis is an illness that usually develops in men 20 to 50 of age and represents major health issue worldwide (1, 2). Prevalence of prostatitis increases with age and it reaches the highest value at the age of 40 to 50 - 12.6%. Its lowest value is at the age of 30 - 6.3% (3). The illness itself is unsatisfactorily defined and insufficiently studied. Subjectively, the illness is very uncomfortable for the patient. Success of the treatment is also questionable and that makes this illness therapeutical problem for urologists. Although, at the first glance, this illness doesn’t appear to be causing loss in working ability, in some cases it is a social problem and despite of its benignity it effects the psychical constitution of the patient (4, 5). Patients loose interest in work and sex, have low self-esteem and sometimes show signs of severe neurasthenia. On the other hand, complexity of the procedures and high treatment costs highlight the importance of chronic prostatitis as medical and public health problem (6, 7, 8). Research done by the National Institute for Health USA shows that around billion dollars is spent on prostatitis treatments annually, which means that chronic prostatitis presents a great socio-economical problem (9,10). Patients visit their doctors because of the pain in their lower urinary tract, impaired life quality, sleeping problems, pain and discomfort in the pelvic region. Researches that were done to help the patients resulted from verifying symptom questionnaire for prostate illnesses (NI-HCP symptom questionnaire - National Institute for Health Chronic Prostatitis Symptom Index) 1999 (4).
Furthermore, diagnosis of chronic prostatitis is usually the wrong one in urological practice. Therefore, it is necessary to adopt categorization of prostatitis based on planed diagnostic procedures. It is an imperative in order to determine an adequate therapy approach and a successful treatment. There are different therapy trends in treating this condition. New trends in treating this chronic urological condition (combination of qui-nolones antibiotics and postsynapthic alpha 1 blockers) are successful in a relatively short period of time (12).
Quinolones /ciprofloxacin/ is, currently, the medication of choice in treating chronic nonbacterial prostatitis. They easily penetrate into prostate, in stroma and in the prostate secretion as well (13). As amphoteric medications, they have two dissociation constants, one in acid and the other in basic pH. Standard therapy includes continuous dosage of 2x500 mg for 30 days. Many authors consider the therapy for a period less then 30 days insufficient and suggest that those patients often suffer from recurrent infections. Long-term treatment is necessary because the very cause of illness is located in isolated micro colonies that are well protected from antibiotics (14). Doxazosin is selective alpha 1 blocker with minimal blocking effect on alpha 2 receptors. It is clinically proven that alpha 1 blockers improve the symptoms and urodynamic characteristics in terms of improving urine flow and reducing dynamic obstruction. It is believed that they influence smooth musculature of the prostate and bladder by blocking alpha-adrenergic receptors, resulting in decrease of urethral pressure and improvement in bladder discharge. Partially mediated effect is trough spinal alpha-adrenergic receptors (15).
MATERIAL AND METHODS
Prospective, comparative, open, clinical, manipulative study was done on a sample of 90 patients diagnosed with chronic nonbacterial prostatitis /chronic pelvic pain syndrome, at Urology Clinic in a period from January - November 2004. Diagnostics and categorization of chronic nonbacterial prostatitis is based on the following analysis: SE, blood count, blood sugar level, BUN, creatinine, urine, urethral smear, ejaculate culture, urine cultures x 3, microbiological examination of prostate discharge (done by digitorectal examination of prostate), trans-abdominal ultrasound examination of prostate with determining residual urine, uroflowm-etry with determination of the shape of uroflow curve and completion of NIH-CPSI questionnaire independently or with the physicians assistance. The treatment effect was measured by the mentioned questionnaires, which were filled by the patients following the completion of the treatment. Patient list was made for all the patients in whom all the results were included. Pain intensity was monitored by VAPS pain scale (visual analogue pain scale) during the last seven days and was presented in numbers on a scale from 1 to 10. The criteria for exclusion from the study were: urinary infection, indication of prostate cancer, acute prostati-tis, urethral disease, calculosis of the lower urinary tract, identified allergy to one of the medications, diagnosed psychiatric disorder, diabetes, BUN and creatinine level in their blood, consumption of medications that interfere with the act of voiding. Patients were distributed in the three therapy groups at random. D+C, C and D group were treated for a period of 30 days. Dox-azosin was taken before retiring to bed in 2 mg tablets while ciprofloxacin was taken in 2 doses of 500mg. In statistical data processing the following tests were used: χ2 test, T student test, Pearson’s correlation index, exact test of probability by Fisher.
RESULTS
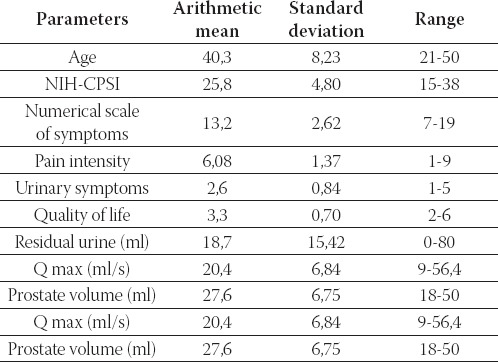
The results of this study are given in Table 1. They show the basic characteristics of the examined group.
TABLE 1.
Basic group characteristics
At the beginning of the study, numerical sum was calculated for each patient in the range from 0 to 43 and it is called ‘total sum’. It is derived from patients’ answers to questions from parts I to IX of symptom questionnaire for chronic prostatitis (4, 16). After one month, during control examination, total sum was used for assessing the success of the therapy. No significant differences in total sum were found among the groups before the beginning of the treatment (table 2). In D group the score was in the range from 15 to 32 with median 23, 5. In D group total score after the therapy was between 11 and 26 points (p<0,001). In C group total score after the therapy was between 13 and 33, median 20, 5 (p=0,002). In C+D group total score was in the range from 18 to 38, median 19. In C+D group total score after the therapy was in from 5 to 31, median 19 (p<0,001). In D and C+D group, significant change was found between the score values at the beginning and after the completed therapy p<0,001 (Table 2).
TABLE 2.
Values of NIH-CPSI symptom score in tested groups before and after therapy
DISCUSSION
Therapy of chronic non-bacterial prostatitis/chronic pelvic pain syndrome should be established on the understanding of pathology and pathogenetic mechanisms, which lead to prostatitis, and pharmacological characteristics of therapeutic agents. Also, chronic prostatitis is most frequently misdiagnosed illness in urology practice (4). There are dilemmas on the proper way towards quantitative and qualitative description of subjective patients’ discomforts, the evaluation of therapy effect, and establishment of correlation between the symptoms of the disease and patients’ objective status. For every patient, at the beginning, sum was estimated ranging from 0 to 43 called total sum of NIH-CPSI questionnaire. Total sum at the beginning was from 15 to 38, with median 23,5. Most significant change was found in C+D group where total sum at starting point was in range between 18-38, median 29, and at the and of therapy between 5-31, median 16, expressed in percentage 55,1%. Symptom score scale is a sum of points for pain and urination, and derives from questions from 1 to 6 with the sum ranging from 1 to 31. According to the total score, patients are divided in groups with mild symptoms, range 1-9, moderate symptoms 10-18, and severe symptoms 19-31. In this research there were 50 (55, 6%) patients with severe symptoms at starting point, and 40 patients (44, 4%) with moderate symptoms. There were no patients with mild symptoms. Following the therapy 2 patients (2, 22%) had severe symptoms, 61 of them (67, 7%) had moderate symptoms, and 17 of them (34, 4%) were with mild symptoms. There is statistically significant change in C+D group and D group (p<0,001). Pain and discomfort, which are dominant in NIH-CPSI questionnaire, are considered in relation to localization, intensity and frequency. At starting point the pain was in the range 7-18, with median 13. There is statistical significant change in C+D group and D group (p<0,001). Most distinctive change was in C+D group, at starting point sum of pain and discomfort was 14, and after the therapy 8 (57, 1%). Most frequent localizations of pain and discomfort were in pubic region and region of urinary bladder, while pain and feeling of discomfort in top of the penis independent of urination act were uncommon. 29 (99, 9%) of the patients expressed feeling pain or discomfort in pubic region or in bladder region, while 48 (57, 3%) of them had pain in top of the penis independent of urination act. Intensity of pain ranged from 1 to 9, with median 6, 3, at the end of treatment intensity of pain or discomfort was in range of 1 to 7 with median 4,6. After the therapy, in groups C and C+D there was statistically significant difference in pain intensity before and after therapy (p<0, 001). Urinary symptoms are related to patient’s subjective feeling regarding urine discharge from urinary bladder, and the frequency of less-than-two-hours interval between two urinations. Most of the patients in the three examined groups felt incomplete urine discharge, in approximately half of the total number of urinations, while small number of patients did not report that symptom. After the therapy completion, significant change was found in groups D and C+D (p<0,001). Need for frequent subsequent urination is discomfort that accompanies chronic prostatitis. In the examined groups D and C+D there was statistically significant change (p<0, 001). Influence on the quality of life should be observed from several aspects. In NIH-CPSI questionnaire, questions are related to the level of disease symptoms that influence usual daily activities, and questions on how they feel about spending the rest of their life with those symptoms. Considering how the disease symptoms affect the quality of life, care should be taken that these patients, men with chronic prostatitis, are inclined to change personality structure, and that they often exaggerate in disclosure of their subjective discomfort, and that questionnaire report about personal difficulty’s is proportional to symptoms that difficulties provoke. The most frequent answer to the question about the disruption in performance of usual daily activities were „cer-tain level” and „a lot”, while only one patient answered that he did not have any problems in performing usual daily activities. After the therapy no statistical changes were found in either group!!! The effect of prostatitis on the quality of life is multifactorial and Boehminghausis claim that once acquired prostatitis persists throughout the life is not far away from the truth. From previously mentioned statistical data it is clear that patients are burdened with their disease and in spite of its benign nature, disease undermines patients’ psychical constitution. This study showed that even the best therapeutic response gives only partial result (55%) and that further clinical and laboratory studies are necessary to achieve optimal diagnostics and treatment for individual patient.
CONCLUSION
Chronic bacterial prostatitis/chronic pelvic pain syndrome is a very unpleasant health disorder and urologists do not have suitable treatment for it. Additional research into its etiology and pathogenesis of this disease are indispensable. Objectivity of discomfort is very important for the evaluation of therapeutic efficiency and NIH-CPSI questionnaire gives great importance to that issue. Therapy of this unpleasant condition with combination of ciprofloxacin and doxazosin during 30 days is the best therapeutic choice and leads to significant discomfort reduction and better quality of life.
REFERENCES
- 1.McRae S.N. Dairiki Shortlliffe Bacterial Infections of the Genitourinary Tract. In: Tanago E.A, McAninch J.W, editors. Smith’s General Urology. 15th edition. San Francisco: Lange Medical Book; 2000. [Google Scholar]
- 2.Dainel A, Shoskes G. Use of antibiotics in chronic prostatitis syndromes. Canadian J. Urol. 2001;8(1):24–28. [PubMed] [Google Scholar]
- 3.Jeannette M, Potts F. The four categories of prostatitis: Practical approach to treatment. Clev. Clin. J. Med. 2001;61:389–397. doi: 10.3949/ccjm.68.5.389. [DOI] [PubMed] [Google Scholar]
- 4.Litwin S.M. A review of the development and validation of the National Institutes of Health Chronic Prostatitis Symptom Index. Urology. 2002;60(6A):14–18. doi: 10.1016/s0090-4295(02)02296-3. [DOI] [PubMed] [Google Scholar]
- 5.Palermo J, Budia A, et al. Stamey-Meares test in Chronic Prosta-titis Diagnosis is Still Valid Procedure? Eur. Urol. 2003;2(1):15. [Google Scholar]
- 6.Fowler J. Antimicrobial therapy for bacterial and nonbacterial prostatitis. Urology. 2002;60(6A):24–26. doi: 10.1016/s0090-4295(02)02300-2. [DOI] [PubMed] [Google Scholar]
- 7.Pontari A.N. Inflammation and anti-inflammatory therapy in chronic prostatitis. Urology. 2002;60(6A):29–34. doi: 10.1016/s0090-4295(02)02381-6. [DOI] [PubMed] [Google Scholar]
- 8.McNaughton M, MacDonald R, With T.J. Diagnosis and treatment of chronic abacterial prostatitis: systemis review. J. Urol. 2000;163(4):1130–1133. [Google Scholar]
- 9.Bjerklund J.E, Weider W. Understading chronic pelvic pain syndrome. Urology. 2003;61(6):1156–1155. [Google Scholar]
- 10.Jacobsen S.J, Girman C.J, Guess H.A, Oesterling J.E. New di-agnostis and treatment guidelines for prostatitis-original ivestiga-tion. Arch. Intern. Med. 2001;155:477–486. [PubMed] [Google Scholar]
- 11.Barbalias G.A, Nikifordin G, et al. Alfa blockers for treatment of chronic prostatitis in combination with antibiotics. J. Urol. 1998;159:883–887. [PubMed] [Google Scholar]
- 12.Jackson E, Fowler J. Prostatis in Gillen water. In: Grayhack J.Y, editor. Adult and Pedi-atric Urology. 3rd edition. St. Luois: Mosby-Year Book; 1996. [Google Scholar]
- 13.Das A.K, Legget R.E, Whitbeck C, Eagen G, Lewin R.M. Effect of doxazosin on rat urinary bladder function after partial obstruction. Neurourol. Urodyn. 2002;21(2):160–166. doi: 10.1002/nau.10045. [DOI] [PubMed] [Google Scholar]
- 14.Weidner W, Schiefer H.G, Dalhoff A. Treatment of chronic bacterial prostatitis with ciprofloxacin. Results of a one-year follow study. J Med. 1998;82:280–283. [PubMed] [Google Scholar]
- 15.Weidner W, Schiefer H.G, Brachles E. Refractory chronic bacterial prostatitis: a reevaluation of ciprofloxacin treatment after a median follow up of 30 months. J. Urol. 2001;146:350–352. doi: 10.1016/s0022-5347(17)37791-1. [DOI] [PubMed] [Google Scholar]
- 16.Nickel J.C. Recommendation for the evaluation of patients with prostatitis. World. J. Urol. 2003;21(2):75–81. doi: 10.1007/s00345-003-0328-1. [DOI] [PubMed] [Google Scholar]


