Abstract
Most curricula for medical education have been integrated horizontally and vertically–-vertically between basic and clinical sciences. The Flexnerian curriculum has disappeared to permit integration between basic sciences and clinical sciences, which are taught throughout the curriculum. We have proposed a different form of integration where the horizontal axis represents the defined learning outcomes and the vertical axis represents the teaching of the sciences throughout the courses. We believe that a mere integration of basic and clinical sciences is not enough because it is necessary to emphasize the importance of humanism as well as health population sciences in medicine. It is necessary to integrate basic and clinical sciences, humanism, and health population in the vertical axis, not only in the early years but also throughout the curriculum, presupposing the use of active teaching methods based on problems or cases in small groups.
Keywords: integrated curriculum types, sciences integration, curricular architecture and development
Introduction
Shoemaker1 defines an integrated curriculum as “education that is organized in such a way that it cuts across subject matter lines, bringing together various aspects of the curriculum into meaningful association to focus upon broad areas of study.” There is an ongoing discussion about whether medical curriculum should be discipline based or integrated.
The method of teaching medicine, since Flexner's days, implies that students should first learn basic and biomedical sciences and then move to clinical sciences; however, this is not how patients are presented. A common criticism of this approach is that students will not see the relevance of basic and biomedical sciences applied to clinical practice, and it is preferable to encourage students to think as doctors from the day they enter medical school.2
Integration is therefore of key importance for medical education because basic science learning is placed in the context of clinical and professional practice and is considered by students to be more meaningful and relevant. In the vast majority of curriculum reforms, vertical integration combines basic and clinical sciences, early clinical experience, clinician–scientist partnerships, and incorporation of sciences in the later years of the course. This is undoubtedly an advantage, but is based on a biologist's vision of the health-illness process.
The medical curriculum has historically changed with the definition of health and illness. From the definition of disease as an anatomical alteration of the organs in the eighteenth century to the understanding of its multicausality and influence on lifestyles, the social determinants and social, political, and economical realities of defining health disease as a biological, social, and cultural (historic) process were considered. According to the authors of this article, vertical integration should include not only basic and clinical sciences but also sociohumanistic and population health sciences, leading to a broader conception of ways to teach and learn medicine.
Aware of the limitations emerging from biologist-based medical curricula, the medical school at Rosario University, Colombia, undertook a significant curriculum reform to improve students’ knowledge integration to meet the more complex demands of the health system. With a view toward facilitating this integration, this article aims to present the design and implementation of our integrated curriculum in the past three years and to discuss the advantages and disadvantages faced in this endeavor. It will offer some considerations and implications of curriculum integration.
Curriculum Integration Architecture Based on Reconceptualization of the Health-illness Process
After a historical analysis of the health-illness concept, we constructed a theoretical basis of this process that changed our former learning perspective, that is, the traditional discipline-based or “Flexnerian” learning perspective. The meaning of the health-illness process changed from a biological to an anthropological approach. In other words, it was defined as a social, cultural, biological, and psychological process embedded and determined socially and culturally by group of human beings.3 As this approach implies that society and culture are no longer simply risk or etiological factors, our medical curriculum had to evolve into a new structure based on a bio-psycho-sociocultural concept of health and illness.
The practical implications of such reconceptualization of curriculum design involved integrating generic learning outcomes into learning activities that represented the whole health-illness approach and establishing the horizontal integration axis. These generic learning outcomes were classified as scientific, professional, practical, civil, and “new trivium” (communication) outcomes. New trivium is an adapted version of the method used in medieval universities to learn liberal arts.4 Here, new trivium incorporated three subjects of critical thinking into the curriculum: cognitive–linguistic skills, learning how to learn, and oral-written communication skills.5 These skills and learning habits were considered fundamental to integrating learning outcomes from all the mentioned knowledge areas. Furthermore, regarding the vertical integration axis, we also merged the basic/biomedical, clinical, sociohumanistic, and population health sciences (Fig. 1).
Figure 1.
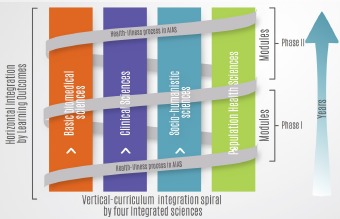
Integrated curriculum architecture.
Additionally, more decisions around the curriculum integration design were made for the reform. The decisions consisted of adopting the SPICES model, which includes strategies such as student-centered learning, problem-based learning, integrated teaching, community-based education, elective programs, and a systemic approach.6 We believed that such a shift from the traditional learning perspective toward the SPICES learning model was imperative for aligning curriculum integration with the current health-illness concept. As our former traditional learning perspective was aligned with the discipline-based curriculum and the biologist-based health-illness concept, it was unsuitable for supporting the current curriculum design.
More precisely, the curriculum integration design adopted a constructivist learning perspective mainly based on the concept of teaching for understanding (TfU),7 supported by Perkins‘8 approach, which delineated the problem of segmented learning in which people learn parts of a repertoire of knowledge and skills but have difficulty combining the parts into a whole. Medical education needs to encompass a range of learning/teaching strategies to foster the development and integration of knowledge, skills, understanding, and wisdom. TfU is conceived as a flexible capability to apply one's knowledge appropriately and creatively in a range of varied circumstances, including practical settings and situations. This conception is suitable for implementing an integrated medical curriculum.
In adopting a constructivist learning perspective, we introduce teaching and learning methods based on problems or cases by adopting learning activities where the generic and specific learning outcomes from the horizontal axis are applied in an outcome-focused core curriculum as described by Newble et al,9 through integrative learning activities. These changes do not apply only in the basic science years of medical school, as our conception of the curricular reform does not have such a division. It applies to the entire curriculum and has advantages and disadvantages that we have discussed later.
Description of Integration in the Curriculum Reform
In this section, in order to reflect and address the importance of humanism in medical education, we present the details of the integration of sociohumanism into our curriculum. This integration is twofold: the Integrated-Systems Learning Activities (AIAS, acronym of its full name in Spanish) and the lecture courses. In the AIAS, students in small groups discuss clinical cases considering the biopsychosociocultural components of health illness in a determined historical context. For instance, the clinical case in the hematology/oncology/infectology AIAS involves a child with anemia caused by hookworm infection. As students engage in determining the known and unknown information, they are provided with a set of learning outcomes that are individually investigated and collaboratively discussed over two weeks. In the discussion sessions, the patient's sociocultural characteristics were analyzed, including malnutrition, hygiene habits, life in rural zones, and his or her relation to the health system in Colombia. Students also conduct a historical review of the intervention of the Rockefeller Foundation in the campaign against hookworm in Colombia. In this case, the biomedical–clinical–social integration is intended to promote students’ thinking of health illness not as a state but as a process determined by a social context, in a geographical and historical setting.
Regarding the lecture courses, three modules of sociohumanism are implemented in semesters 1, 4, and 6. The Introduction of Medical Sociohumanism is taught in semester 1, and it includes a historical perspective of medical sciences, addressing four basic concepts: structure, function, infections, and heritage. The second module, History of Health and Disease, is taught in semester 4, and it includes the construction of the health-illness concept, the health system crisis, and its implications for society. The last module, Sociology and Anthropology of Health, is taught in semester 6, and it addresses the meanings of health from a holistic perspective, using the concepts and methods of social sciences. The integration of sociohumanism courses is intended to promote students’ critical thinking for learning biomedical and clinical sciences, considering an extended framework of the health-illness process.
Advantages of Integrated Curriculum Reform
In our experience, there are a number of advantages to an integrated curriculum. In this article, we only describe the most relevant advantages of the curriculum practice. We identified these advantages through curriculum assessment, using a large number of evaluation tools such as surveys of perception, program participants’ interviews, and focal groups. The following section relates the story of the curriculum participants’ experiences in light of our current medical education program.
Perception of the learning environment
One of the advantages of our integrated curriculum is a good perception of the learning environment. As noted by Miles et al,10 the educational environment in which students are enrolled influences their satisfaction with the curriculum and their academic success. Consequently, our curriculum committee conducted evaluations of the students’ perceptions from the beginning of the reform to diagnose deficiencies in the learning atmosphere. The Dundee Ready Educational Environment Measure (DREEM) was used to evaluate the learning environment because this instrument has been widely used and validated for this purpose.11,12 The DREEM inventory has been translated into Spanish, and it consists of 50 Likert questions, with a maximum score of 200, indicating an ideal environment.13 The result analysis from the last two years of our curriculum reform, which included ~9,300 students’ surveys, provided a score of 152.5/200, indicating an excellent learning environment.14
The inferences of these findings include the possibility that the integrated curriculum offers enjoyable learning experiences, leading to students’ satisfaction with the educational environment. A possible implication of this result is that the positive perception of the educational environment is associated with students’ improved perceptions of their quality of life, thereby increasing the likelihood of them achieving adequate learning development during medical school.15 We relate this positive perception to the shift toward a lower hierarchy in the classroom and the collaboration-oriented learning methodology, which may make the experience less stressful than in the fully traditional model.
Students’ desertion
Our curriculum reform was considered useful for avoiding students’ desertion. Possibly because of the positive perception of the learning environment and the mentorships implemented in the preclinical phase, the overall desertion rate declined from ~40% to 1.3%. As academic desertion is an important issue in several Latin American medical schools,16 achieving a low attrition rate involves a substantial reduction in financial and emotional costs for our students, faculty, and society.17
Are these advantages attributable to curriculum integration? We did not find evidence of a cause–effect relationship between the described advantages and curriculum integration. However, we do estimate that the combination of vertical and horizontal integration, the SPICES model, mentorships, and inclusion of the academic community in the curriculum reform may have a positive relationship with a good perception of the learning environment and students’ retention. We believe that these advantages are valuable, even if students from the reformed and traditional curriculum score similarly in standardized tests. What could allow our medical students to have a propitious learning development and a low desertion rate? We speculate that the answer to this question may be found in their future clinical practice as physicians engaged in life-long learning and well prepared for the complex health system. However, future research is needed to explore this hypothesis.
Disadvantages of Integrated Curriculum Reform
As noted by Bland et al,18 reforms entail resistance of those who experience change, and we were not the exception to this principle. In the curriculum assessment conducted, we also recognized several issues emerging from the current curriculum practice. Although these issues were a matter of debate and concern for our curriculum committee, their analyses also contributed to the curriculum design and integration improvements. We describe these issues and subsequent curriculum improvements in the next section.
Resistance to the curriculum reform
Several participants of the program, including students, were reluctant about the curriculum reform, which is understandable if we consider that the medical curriculum at Rosario University began in 1653. As the first medical education program in Colombia, the traditional learning perspective at Rosario Medical School reflects certain values and attitudes, for instance, reinforcing the structures of power and hierarchy, which are more aligned with the teacher-centered learning perspective. As explained by one teacher, “decreasing lectures to incorporate social discussions of learning outcomes in small groups sets aside many important topics that students will not learn, hence affecting the quality of our graduate medical students.”
Concerning this issue, some researchers consider integration in curriculum reform as a cyclizing issue. For example, Hopkins et al19 claim curriculum integration has been historically revisited in medical education conversations, but no meaningful changes have emerged from the repeated recommendations in such meetings. These researchers attribute the “change without difference” in medical curriculum reforms to the focus given for changing the curricular structure instead of examining the learning needs of the medical education community and transforming the curriculum based on these needs. As learning needs are paid little attention in reforms focused on structure, which is on the curriculum organization, medical educators from varied disciplines or sciences may struggle with curriculum integration if they seek different learning outcomes. Therefore, the ongoing problem of curriculum integration may be overcome if the educational community addresses the learning challenges faced by individual educators involved in the reform.19
Aware of the tension between the traditional and constructivist learning perspectives, and concerned about the possibility of making changes without substantial transformations because of this tension, the curriculum reform committee considered both perspectives relevant as they involved values that were significant to the stakeholders, namely, instructors and students. Therefore, the committee included both learning perspectives in the reform under the form of a hybrid curriculum. Put simply, courses based on the traditional and constructivist learning perspectives were integrated into the curriculum. For example, one component of the new curriculum included student-centered learning activities, AIAS, organized in organ system courses. The other component of the curriculum was the lecture courses framed by the traditional learning perspective. We think both components enhance social (in AIAS courses) and individual (in lecture courses) learning, which are crucial for addressing the issues between the two learning perspectives we identified from the results of the curriculum assessment.
How does a hybrid curriculum enhance students’ learning? A multimodality approach to curriculum design seems to improve social and individual learning because students learn in different ways just as different teachers teach differently.20,21 Although the current medical curriculum reforms in Europe and North America are intended to reduce lecture hours, promote student-centered learning activities, and increase integration of sciences,22 some stakeholders prefer teaching and learning “by ear”–-that is, exchanging information through speeches21–-while others want multisensory learning experiences,23 for instance, individual and social inquiry of real clinical problems, creating patterns of information in graphs, discussing abstract concepts with peers, reflecting about the learning process, or “flipping the classroom” (as occurs in AIAS).21,24 Stakeholders in our setting may prefer one curriculum approach instead of another because they might believe that the chances for academic success may be higher. We think that incorporating a multimodel approach into the curriculum enhances learning, as this model possibly offers diverse possibilities for addressing the stakeholders’ learning expectations and needs. Thus, our curriculum reform may not face the cyclizing issue of curriculum integration, as our biopsychosociocultural integration approach takes into consideration the students’ and instructors’ learning expectations.
Students’ academic self-confidence
Another issue emerged from the coexistence of the former and current medical school curriculum. Since the first cohort after the curriculum reform was admitted in 2013, students from the traditional curriculum have been in contact with those from the integrated curriculum for the last three years. The perceptions of students taught under the previous curriculum about differences between both curricula included that the reformed curriculum had less learning quality than their own. This perception could have undermined the self-confidence in learning of the students studying the current curriculum, even though they had good grades. Although the negative beliefs about learning, especially those of the cohort after the reform, manifested in meetings and program evaluation sessions, good results on anonymous academic self-perception surveys have shown a different view. This contradictory phenomenon may be a reflection of the complex social dynamics among students and the evidence for inferring that more than one method to evaluate confidence in learning is required.
Reforms in Curriculum Integration are Dynamic and Sometimes Baffling
Although there is ample literature on curriculum integration,25–31 including its dynamic approach,32,33 we reached an in-depth understanding of it when faced by the challenges entailed in integrated curriculum practice. The challenges provided us with opportunities to construct the meaning of our particular curriculum design, which was supported by our reconceptualization of the health-illness process. What does curriculum integration considering the understanding of our academic community's health system mean? We believe it means transforming academic stakeholders’ learning perspectives and adapting them into the curriculum improvement and comprehending the value of these efforts by exploring their benefits and issues in students’ development.
We acknowledge that the medical education literature contains numerous examples of curriculum reforms in which resistance to change is an ongoing theme. However, the underlying causes of resistance may emerge from varied factors that are dependent on the context. For instance, in a study conducted by Muller et al,34 interdisciplinary faculty teams perceived that resistance emerged from their diverse disciplinary assumptions, which made communication with each other difficult. In contrast, we speculate that the resistance to curriculum reform in our case was related to the fear of losing the university traditional values rather than to dissimilar theoretical frameworks. Although resistance to change may be considered an obvious response to a medical curriculum reform, we believe that the contextually dependent factors that cause resistance are diverse. This implies that different strategies have to be implemented in order to achieve the curriculum reform.
What type of factors medical education communities may face in curriculum reforms? Lane35 claims that varied factors contribute to resistance to change in health professional education: “strong existing traditions, lack of perceived need for change, strong disciplinary identification of faculty members, departmental protection of curriculum time, skepticism of alternative pedagogical views, lack of experience, lack of time to implement changes, fear of loss of resources or accreditation, among others.” The factors that affect curriculum integration may be different for different settings, making resistance to reforms a complex, diverse phenomenon.
Conclusion
This experience has several implications. First, curriculum reform in medical education is both difficult and challenging, but considering and understanding the issues emerging from the reform may help the academic community to succeed in the new curriculum practice. Second, designing curriculum integration, as a component of the reform, should begin with an in-depth understanding of the setting in which it will be implemented. In our case, it required a shift in the health-illness meanings before the curriculum integration design. A reform without such a shift would have had little impact on the curriculum practice. By contrast, changing the health-illness concept demands a corresponding transformation in medical students’ training. Finally, curriculum integration evaluation should entail collecting information about its issues and benefits using different instruments and methodologies. This approach may provide some valid insights about the curriculum integration implementation that can lead to adequate decisions about adjusting it.
Author Contributions
Wrote the first draft of the manuscript: GAQ. Contributed to the writing of the manuscript: J V. Agreed with manuscript's results and conclusions: GAQ, JV, MA, M-CA, PG, and A-MP-B. Jointly developed the structure and arguments for the article: GAQ and J V. Gathered the information from the curriculum evaluation: MA, M-CA, PG, and A-MP-B. Made critical revisions and approved the final version: GAQ and JV. All authors reviewed and approved the final manuscript.
Footnotes
Peer Review:Two peer reviewers contributed to the peer review report. Reviewers’ reports totaled 467 words, excluding any confidential comments to the Academic Editor.
Competing Interests:Authors disclose no potential conflicts of interest.
Funding:Authors disclose no external Funding sources.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent Academic Editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of Competing Interests and Funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
References
- 1.Shoemaker B.J.E. Integrative Education: A Curriculum for the Twenty-First Century. OSSC Bulletin. 1989; 33(2): n2. [Google Scholar]
- 2.Harden R.M. Approaches to curriculum planning. Med Educ. 1986; 20(5): 458–466. [DOI] [PubMed] [Google Scholar]
- 3.Quevedo E. Comprensión histórico crítica del proceso salud-enfermedad: base para una reforma curricular en medicina. In: Quintero G.A., ed. Educación Médica. Diseño e implementación de un currículo basado en resultados del aprendizaje. Bogotá: Colección Pedagogía; 2012: 269–314. [Google Scholar]
- 4.Conrad L. Integration and the liberal arts: a historical overview. On Horizon. 2014; 22(1): 46–56. [Google Scholar]
- 5.Alvarez B., Rodriguez L. El nuevo trivium. In: Quintero G., ed. Educación Médica. Diseño e Implementación de un Currículo Basado en Resultados del Aprendizaje. Bogota: Colección Pedagogía; 2012: 167–177. [Google Scholar]
- 6.Harden R.M., Sowden S., Dunn W.R. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984; 18(4): 284–297. [DOI] [PubMed] [Google Scholar]
- 7.Wiske M. Enseñanza para la comprensión en educación médica. In: Quintero G., ed. Educación Médica. Diseño e Implementación de un Currículo Basado en Resultados del Aprendizaje. Bogota: Colección Pedagogía. Editorial Universidad del Rosario; 2012: 151–166. [Google Scholar]
- 8.Perkins D. Making Learning Whole: How Seven Principles of Teaching Can Transform Education. San Francisco: Jossey-Bass; 2009. [Google Scholar]
- 9.Newble D., Stark P., Bax N., Lawson M. Developing an outcome-focused core curriculum. Med Educ. 2005; 39(7): 680–687. [DOI] [PubMed] [Google Scholar]
- 10.Miles S., Swift L., Leinster S.J. The Dundee ready education environment measure (DREEM): a review of its adoption and use. Med Teach. 2012; 34(9): e620–e634. [DOI] [PubMed] [Google Scholar]
- 11.Xu X., Wu D., Zhao X. et al. Relation of perceptions of educational environment with mindfulness among Chinese medical students: a longitudinal study. Med Educ Online. 2016; 21: 30664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nosair E., Mirghani Z., Mostafa R.M. Measuring students’ perceptions of educational environment in the PBL program of Sharjah Medical College. J Med Educ Curric Dev. 2015; 2015(2): 71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pantelidis P., Staikoglou N., Paparoidamis G. et al. Medical students’ satisfaction with the applied basic clinical seminar with scenarios for students, a novel simulation-based learning method in Greece. J Educ Eval Health Prof. 2016; 13: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chhabra S., Misra A., Shah S., Kole T. Survey of student perception of medical education environment among emergency medicine residents of an academic medical centre in Northern India. Int J Emerg Med. 2016; 9(1): 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Enns S.C., Perotta B., Paro H.B. et al. Medical students’ perception of their educational environment and quality of life: is there a positive association? Acad Med. 2016; 91(3): 409–417. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez-Mata J.M., Hernandez-Castro R., Nieto-Caraveo A., Hernandez-Sierra J.F. [Risk factors for students desertion from the UASLP School of Medicine, Mexico]. Gac Med Mex. 2005; 141(5): 445–447. [PubMed] [Google Scholar]
- 17.Yates J. When did they leave, and why? A retrospective case study of attrition on the Nottingham undergraduate medical course. BMC Med Educ. 2012; 12: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bland C.J., Starnaman S., Wersal L., Moorehead-Rosenberg L., Zonia S., Henry R. Curricular change in medical schools: how to succeed. Acad Med. 2000; 75(6): 575–594. [DOI] [PubMed] [Google Scholar]
- 19.Hopkins R., Pratt D., Bowen J.L., Regehr G. Integrating basic science without integrating basic scientists: reconsidering the place of individual teachers in curriculum reform. Acad Med. 2015; 90(2): 149–153. [DOI] [PubMed] [Google Scholar]
- 20.Drake R.L. A retrospective and prospective look at medical education in the United States: trends shaping anatomical sciences education. J Anat. 2014; 224(3): 256–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleming N.D. I'm different; not dumb. Modes of presentation (VARK) in the tertiary classroom. Paper presented at: Research and Development in Higher Education, Proceedings of the 1995 Annual Conference of the Higher Education and Research Development Society of Australasia (HERDSA), HERDSA; 1995.
- 22.Brauer D.G., Ferguson K.J. The integrated curriculum in medical education: AMEE guide no. 96. Med Teach. 2015; 37(4): 312–322. [DOI] [PubMed] [Google Scholar]
- 23.Drake R.L., Pawlina W. Multimodal education in anatomy: the perfect opportunity. Anat Sci Educ. 2014; 7(1): 1–2. [DOI] [PubMed] [Google Scholar]
- 24.Hurtubise L., Hall E., Sheridan L., Han H. The flipped classroom in medical education: engaging students to build competency. J Med Educ Curricul Dev. 2015; 2: 35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McNaughton S., Barrow M., Bagg W., Frielick S. Capturing the integration of practice-based learning with beliefs, values, and attitudes using modified concept mapping. J Med Educ Curricul Dev. 2016; 2016(3): 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burgess A., Mellis C. Engaging medical students in the basic science years with clinical teaching. J Med Educ Curricul Dev. 2015; 2015(2): 49–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Furmedge D.S., Smith L-L, Sturrock A. Developing doctors: what are the attitudes and perceptions of year 1 and 2 medical students towards a new integrated formative objective structured clinical examination? BMC Med Educ. 2016; 16(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Achike F.I. The challenges of integration in an innovative modern medical curriculum. Med Sci Educ. 2016; 26(1): 153–158. [Google Scholar]
- 29.Loftus S. Understanding integration in medical education. Med Sci Educ. 2015; 25(3): 357–360. [Google Scholar]
- 30.Haramati A. Educating the educators: a key to curricular integration. Acad Med. 2015; 90(2): 133–135. [DOI] [PubMed] [Google Scholar]
- 31.Kadirvelu A., Gurtu S. Integrated learning in medical education: are our students ready? Med Sci Educ. 2015; 25(4): 549–551. [Google Scholar]
- 32.Mennin S. Self-organisation, integration and curriculum in the complex world of medical education. Med Educ. 2010; 44(1): 20–30. [DOI] [PubMed] [Google Scholar]
- 33.Aron D.C. Developing a complex systems perspective for medical education to facilitate the integration of basic science and clinical medicine. J Eval Clin Pract. 2016. Mar 8. doi: 10.1111/jep.12528. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 34.Muller J., Jain S., Loeser H., Irby D. Lessons learned about integrating a medical school curriculum: perceptions of students, faculty and curriculum leaders. Med Educ. 2008; 42(8): 778–785. [DOI] [PubMed] [Google Scholar]
- 35.Lane I. Change in higher education: understanding and responding to individual and organizational resistance. J Vet Med Educ. 2007; 34(2): 85–92. [DOI] [PubMed] [Google Scholar]


