Abstract
Over the past two decades, our internal medicine residency has created a unique postgraduate education in internal medicine by incorporating a formal curriculum in point-of-care cardiac ultrasound as a mandatory component. The details regarding content and implementation were critical to the initial and subsequent success of this novel program. In this paper, we discuss the evidence-based advances, considerations, and pitfalls that we have encountered in the program's development through the discussion of four unanticipated tasks unique to a point-of-care ultrasound curriculum. The formatted discussion of these tasks will hopefully assist development of ultrasound programs at other institutions.
Keywords: point-of-care ultrasound, internal medicine, residency, curriculum, graduate medical education, CLUE
Introduction
Ongoing technologic innovation has resulted in the development of pocket-sized ultrasound imaging devices,1,2 bringing the diagnostic power of ultrasound to the bedside. Ultrasound imaging, even when applied in a limited fashion, can rejuvenate and empower the art of bedside diagnosis.3,4 Such a timely renaissance in bedside examination is occurring as age-old physical and auscultative techniques have been waning in the hands of young physicians over recent decades,5 during the proliferation of modern imaging techniques such as echocardiography, computed tomography, and magnetic resonance imaging. Despite the potential to improve bedside examination, only a few subspecialists such as radiologists, cardiologists, and obstetrician–gynecologists have been traditionally trained in formal ultrasound interpretation and even fewer can image at the bedside. As the decision to embark on an expensive evaluation or perform screening often rests with the physician who establishes initial patient contact, there exists a need to develop and teach simplified ultrasound techniques to the many physicians involved in the primary care of patients. Learning the use of bedside ultrasound to augment physical examination has the potential to change general medical practice and therefore should be considered early in the education of the physician.
In this paper, we describe a successful integration of a formalized cardiac limited ultrasound curriculum within an internal medical residency that has persisted as a mandatory component for all residents for over a decade. As medical educators are rapidly examining the possibility of incorporating ultrasound training within their own program, this report hopes to decrease the inefficiencies, redundancies, and heterogeneity of program development by describing the pros and cons of unanticipated tasks that our program encountered.
Background and Setting
Scripps Mercy Hospital is a 500-bed urban community hospital with 36 residents at the Internal Medicine Residency, approved by the Accreditation Council of Graduate Medical Education (ACGME). In the late 1990s, research by a cardiologist-echocardiographer (BJK) at this site on the cost-efficacy of limited echocardiography imaging protocols6–8 provided the foundation for application of what were then recently-conceived prototypes for hand-carried ultrasound devices. The cardiologist was the medical director of the echocardiography and vascular ultrasound laboratory within the hospital where the residency was centered and later became faculty in the program, forging collaboration with the directors of medical education (DJS) and the internal medicine residency (SAA).
The combination of cost-effective limited imaging and the technologic miniaturization of ultrasound devices resulted in the creation of an evidence-based imaging protocol and teaching curriculum for bedside cardiac examination,9–12 which we have named cardiovascular limited ultrasound examination (CLUE) (see Fig. 1).
Figure 1.
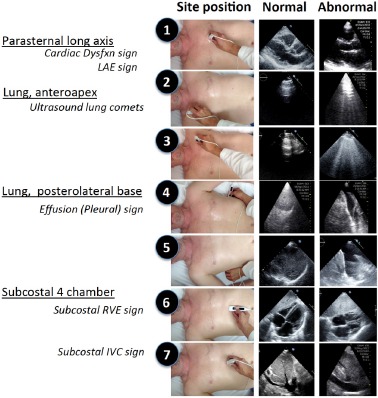
The CLUE examination.
Note: Composite figure listing CLUE signs (left column), hand positions (sites 1–7) (central column), and examples of normal and abnormal images (right column). Republished with permission of the American Institute of Ultrasound in Medicine, from Cardiac limited ultrasound exam techniques to augment the bedside cardiac physical. Kimura BJ, Shaw DJ, Amundson SA, Phan JN, Blanchard DG, DeMaria AN. J Ultrasound Med. 2015;34: 1683–1690;11 permission conveyed through Copyright Clearance Center, Inc.
The CLUE begins with a single parasternal long-axis view, a standard well-studied view in echocardiography, which allows for the efficient detection of two “signs”: cardiac systolic dysfunction and left atrial enlargement. Both these signs have documented diagnostic accuracy,13–16 prognostic value,10,17 and have been successfully taught to novices.13,16,18 Next, the lung views form a box around the chest cavity. The two apical lung views look for the ultrasound lung comet-tail sign, which can have high specificity for pulmonary edema or alternatively can denote interstitial lung disease.19 The basal pleural spaces are viewed for the effusion sign, the presence of dark fluid present posteriorly in the costophrenic or costovertebral spaces. The presence of apical comet tails or basilar pleural effusions has demonstrated diagnostic accuracy,20,21 are associated with a poor prognosis,22–25 and can be easily learned.26 Lastly, the subcostal view evaluates right ventricular enlargement and inferior vena cava (IVC) plethora and serves as an alternate view of the left ventricle when the parasternal view is poor or inaccessible. The presence of right ventricular enlargement or IVC dilation has both diagnostic and prognostic value.27,28 CLUE provides consolidation of multiple evidence-based techniques into a single physiologically-based bedside method for general cardiac examination of any patient, regardless of presentation. Research in the feasibility and accuracy of CLUE, often with resident physician co-investigators, has resulted in 26 peer-reviewed publications since 1998 and was recently assessed favorably in a systematic review of the literature.29 The ultrasound curriculum continued development under the ACGME Innovations Project in 2006–2016. A formal, mandatory curriculum with proficiency testing was adopted in 2005, with 80% of residents demonstrating proficiency in CLUE upon graduation since that time.12
Four Tasks Completed
Unlike in medical school where ultrasound can be integrated into basic anatomy or physiology courses, the use of ultrasound in residency as a clinical technique requires a curriculum, exam philosophy, and integration into a demanding time frame. In addition to the “nuts and bolts” required of any new curriculum development, which include proposing length and goals of training, identifying faculty leadership, determining site requirements, and procuring Funding, we encountered four unanticipated questions that were unique to the implementation of a point-of-care ultrasound program (Table 1). We list our program's response to these questions as four tasks we completed and felt were essential to our sustained success: (1) the fundamental decision to utilize bedside ultrasound as a physical examination technique rather than a limited ultrasound study, (2) progressive teaching of concepts and techniques within a vertical curriculum, (3) utilization of unrecognized resources within the hospital and (4) promotion of methods to facilitate retention of procedural memories specific to ultrasound application.
Table 1.
Considerations (pros/cons) are listed for four essential questions when creating an ultrasound curriculum.
| (1) HOW WILL ULTRASOUND BE USED IN THE PROGRAM? | |
|---|---|
| AS A PHYSICAL EXAM TECHNIQUE* | AS A “LIMITED ULTRASOUND” STUDY |
| Frequent (daily) reinforcement of a single exam. | Memorization and use of multiple imaging protocols. |
| Findings correlate with familiar physical techniques. | Specialty specific skills. |
| Subjective interpretation. | Documentation and archived images. |
| Incidental findings minimized. | More comprehensive interpretation. |
| Individual user-specific accuracy and utility. | Competency well defined by standards. |
| No reimbursement. | Significant reimbursement for time spent. |
| Requires a single exam formed by consensus opinion. | Difficulty with hospital staff privileging. |
| (2) HOW WILL THE CURRICULUM BE STRUCTURED? | |
| VERTICAL STRUCTURE* | HORIZONTAL STRUCTURE |
| Development of basic skill set. | Memorization of multiple, unrelated techniques and indications. |
| Repetition of a single, basic exam. | Published exams with known accuracies. |
| Longer lasting memory via repetition. | Multiple exams increase potential revenue. |
| Skills added based upon mastery of prior skills. | Requires reaching competency in each separate exam. |
| Suitable for general use by all residents during all rotations. | Better for motivated self-learners in an elective rotation. |
| Nonparticipating faculty become familiar with exam. | Faculty with subspecialty imaging expertise. |
| Metrics can improve overall program. | Difficult to identify deficiencies in curriculum due to heterogeneity. |
| (3) WHAT RESOURCES ARE AVAILABLE? | |
| MANDATORY PARTICIPATION* | ELECTIVE PARTICIPATION |
| Much larger volume of participants of varying motivation. | Fewer, motivated participants limit costs and improve success. |
| Teaching added in to general curriculum. | Imaging during existing subspecialty or elective rotations. |
| Use existing resources in echo and radiology labs. | Perform and bill limited studies with attending during training. |
| Resident-to-resident teaching. | Hire/recruit expert faculty in point-of-care ultrasound. |
| Faculty development within program. | Use subspecialists familiar with ultrasound. |
| Additional financial support often needed. | Fund new devices from program earnings. |
| Larger participant failure or dropout rate. | Higher competency rate due to selection bias. |
| (4) WHAT LEARNING CONSIDERATIONS ARE SPECIFIC TO ULTRASOUND? | |
| PHYSICAL SKILL* | DIDACTIC KNOWLEDGE |
| Teaching requires frequent repetition. | Lecture and/or study time required. |
| Requires more faculty/sonographer time. | Materials easily made for on-line, self-study. |
| Participants need frequent opportunities to practice and access to equipment for autonomous imaging. | Didactic material easily forgotten, if not reinforced. |
| Standardize exam, grip, approach and orientation. | Imaging skills are likely independent of knowledge. |
| Success more dependent upon teacher. | Success depends on learner and material presented. |
| Proficiency evaluation requires direct observation. | Retention of material easily tested. |
Note:
The pathway chosen by our program.
Prior to initiation of a cardiac ultrasound curriculum within an internal medicine residency, we now realize that a general consensus between graduate education, cardiology, and participating departments on these four tasks may provide the foundation for collaboration and resource support.
Question 1: How will ultrasound be used in the program?
Task 1: We chose to utilize ultrasound as a physical examination technique
Every program must decide whether their use of ultrasound will be in the form of a standard limited ultrasound study or as a general physical examination technique. Traditionally, ultrasound is utilized as a diagnostic imaging modality that is interpreted by a radiologist and requires that images are stored and a formal report is made available in the patient's chart. With the advent of portable ultrasound devices, point-of-care limited ultrasound imaging has become common practice in emergency and critical care medicine to obtain quick answers for immediate treatment of life-threatening illnesses familiar to these specialties, such as in the use of the Focused Assessment with Sonography for Trauma (FAST) examination.30 In the emergency setting, the physician determines that a specific ultrasound examination is indicated based on history and physical or mechanism of injury and must be justifiably limited due to urgency. The limited ultrasound examination itself, although not comprehensive by radiographic or echocardiographic standards, is similar to laboratory or radiographic testing and should follow strict uniformity standards in order to seek reimbursement for a diagnostic test.31
However, the use of any bedside examination tool such as ultrasound, when inserted earlier in the diagnostic process, can affect formative thinking in patient diagnosis. Physical examination is an unblinded, biased, skill-based process of detecting a set of specific anatomic findings through observation, palpation, percussion, and auscultation. Interpreting and integrating bedside examination findings with the patient's history to formulate an assessment and plan is a process familiar to all physicians. Notably, only the physician performing the examination knows his or her own personal accuracy in specific examination skills and accordingly often omits techniques that are time consuming, are overly sensitive or non-specific, or do not affect immediate decision-making. The unblinded nature and the variability in individual physician performance clearly differentiate this form of ultrasound practice from formal limited studies. In addition, the use of ultrasound as a physical examination tool, having precedence in the use of the otoscope, ophthalmoscope, stethoscope, and bedside Doppler, should not require image archival nor precise quantitation of results.
At the residency level, the choice of using ultrasound either as a physical examination technique or as a diagnostic imaging test is a fundamental philosophical decision in the initiation of an ultrasound program and has financial, medicolegal, and educational implications (Table 2). Professional societies have attempted to define the use of bedside cardiac ultrasound as a “quick look,” “focused,” “limited,” or “point-of-care” ultrasound study31,32 in order to clarify practice, set standards and expectations of competency, and structure training programs. In our program, we chose to teach ultrasound as a physical examination tool, which allowed the ultimate measure of success to be an improvement in the user's overall bedside diagnostic capability. Ultrasound has been shown to complement physical examination, as exemplified by a study which demonstrated that a quick-look ultrasound examination improved most residents’ capabilities to detect left ventricular systolic dysfunction when considered after attentive bedside palpation and auscultation.13 Ultrasound use is not meant to replace the physical exam but to improve deficiencies in a manner determined by the user. Certainly, in terms of cardiac entities such as left atrial enlargement, small effusions, or small atheromatous plaque in the carotid, ultrasound is a more sensitive technique, as there are no physical examination equivalents to detect these disease states.
Table 2.
Physical examination vs. limited ultrasound study.
| PHYSICAL EXAM TECHNIQUE | LIMITED ULTRASOUND STUDY | |
|---|---|---|
| Equipment requirements | Pocket-sized, minimal features, ease of rapid application. equipment cost ~$8,000 | Cart-based, fully-featured, archival of images, report generation, equipment cost ~$30,000 |
| Use frequency | Performed daily on multiple patients, multiple follow up exams per patient | Typically once per patient for diagnosis, occasional follow up |
| Diagnostic biases | History/physical results bias accuracy, application, accuracy, and use varies by physician | None, can be applied by sonographer, or another physician with equivalent results |
| Specialty | All physicians practicing physical examination | Specialty training in each specific exam |
| Documentation | Presence/absence of ultrasound “signs” noted in physical examination | Formal image archival; report generation |
| Reimbursement | None | $100–$500 patient |
| Liability | User accountable for signs sought | User accountable for all abnormalities recorded |
| Curriculum/training | Medical school or general medicine residency | Subspecialty, competency thresholds determined by expert consensus |
Our decision to use ultrasound as a physical examination tool allowed us to maintain the philosophy of physical examination and integrate the findings as subjective signs into the initial evaluation. This physical examination philosophy reduces the liability of missing incidental findings that have not been taught to nor intently searched for by the user. Furthermore, this philosophy results in the reduction of the educational, economic, and medicolegal burden of understanding and diagnosing all pathologic findings, incidental or otherwise, in each view.
In choosing a physical examination philosophy, the undeniable loss of immediate revenue by not seeking reimbursement of limited echo or limited ultrasound studies is hopefully regained by an earlier and more accurate diagnosis that reduces downstream costs of inappropriate triage, testing, and consultation. Conversely, the revenue obtained by choosing a limited ultrasound pathway could be allocated to develop training, quality assurance and research programs, and purchase devices, as evidenced by the success of such practice in emergency medicine. In our program, device and training costs have been subsidized primarily by our hospital, philanthropy, or volunteerism.
Question 2: How will the curriculum be structured?
Task 2: We teach a simplified core examination within a vertical curriculum
While ultrasound can be used to detect multiple cardiopulmonary diseases, we have chosen to image only select views to detect prevalent structural pathologies that reflect prognostic information. We use seven quick-look two-dimensional views (without Doppler) using a low-frequency (3 MHz) cardiac transducer to find ultrasonic signs of left ventricular systolic dysfunction, left atrial enlargement, pulmonary edema, right ventricular enlargement, and elevated central venous pressures. CLUE targets augment a physician's cardiac physical examination by detecting the ultrasound equivalents of traditional physical findings such as rales, gallops, heaves and pulsations. During the development of this curriculum, we found that creating a core general examination from which to build upon, rather than teaching separate diagnosis-based examinations independent from one another, created a more efficient and redundant learning process for the residents.
The instruction of simplified criteria for each sign with the concomitant teaching of one to two pitfalls per sign can easily be performed as detailed elsewhere.12 CLUE is a synthetic exam, where each individual component is interpreted in the context of the whole exam with historical data, in order to make a wide range of diagnoses from subclinical atherosclerosis to severe pulmonary edema. With practice, the examination itself takes less than two minutes, and skilled residents are able to complete the basic examination in less than 30 seconds. The initial brevity of the core examination is essential for repetitive learning. The student can use the mnemonic “working backward” against the flow of blood to remember the CLUE imaging protocol from left ventricle to inferior vena cava.
Using a vertical curriculum (Fig. 2), we can expand upon the CLUE examination to include advanced imaging of other high-risk targets using constant hand-positions and similar imaging sites. In contrast to a horizontal curriculum where residents learn large sets of different skills in series, our students add to the fundamental knowledge they have gained while reinforcing procedural and didactic memories of prior skills. For example, it is part of the basic curriculum that residents learn to assess abdominal aortic aneurysm while evaluating the IVC diameter and to assess jugular venous distension at the time of screening for carotid plaque. By tilting the probe so as to differentiate the artery from the vein in the same view, a simple procedural memory is formed that prevents disastrous clinical errors that can result from mistaking arteries for veins in estimating central venous pressures or inserting intravenous catheters. After screening for the abdominal aorta, the bladder can be easily imaged, preferably for any post-void residual. In more advanced CLUE imaging, we extended the basic CLUE examination to include brief screening of the kidneys for hydronephrosis, the liver for fatty liver disease, and the spleen of splenomegaly by simply dropping down one interspace from the basic CLUE lung base views.
Figure 2.
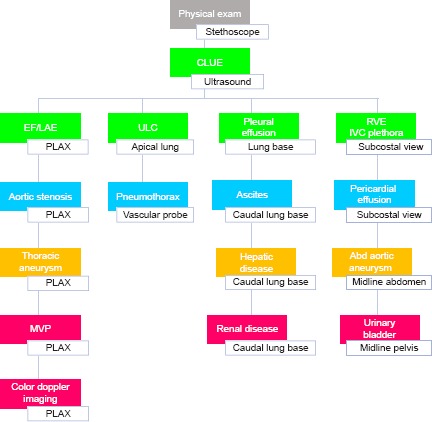
Vertical curriculum.
Note: Diagram demonstrating the vertical nature of the curriculum where the basic CLUE (green) is seen in the upper rows with subsequent lessons (advanced CLUE) noted under each initial imaging site, progressive levels separated by color groupings (blue, yellow, red).
Abbreviations: CLUE, cardiovascular limited ultrasound examination; EF, ejection fraction; LAE, left atrial enlargement; ULC, ultrasound lung comet; RVE, right ventricular enlargement; IVC, inferior vena cava; PLAX, parasternal long axis view; Abd, abdomen; MVP, mitral valve prolapse.
In summary, the basic CLUE-imaging protocol weaves together procedural imaging of evidence-based targets that would assist in a wide range of cardiovascular presentations. The derivation of such a short memorable “backbone” examination allows frequent reinforcement of skills during daily rounds, hospital follow-up or new outpatient visits and provides a structure in which to expand more advanced, specialized imaging. Determining the curriculum structure needs to be done prior to the initiation of an ultrasound program.
Question 3: What resources are available?
Task 3: We found unrecognized resources within the hospital and residency program
One of the largest hurdles in creating a residency curriculum is finding teachers and a mechanism in which residents can learn and reinforce imaging skills. In our program, we have accepted a “bottom-up” approach to teaching, meaning that we have taught the residents the techniques required to become proficient at CLUE to the point that they are allowed autonomous use and teaching under Graduate Medical Education after documenting proficiency. This bottom-up model of teaching creates a foundation for the program among the residents by investing in an initial year of intense learning of new concepts followed by two years of independent imaging with expert assistance made available. Although we have attempted individual and group instruction to faculty attendings who voluntarily participated in the curriculum, overall success has been observed to be limited of a “top-down” approach. A similar phenomenon is noted in the point-of-care ultrasound field itself, where development, promotion, and teaching have been dominated by relatively younger, recently graduated faculty members. Consequently, it is not unusual in our program for a ward team to have a CLUE-proficient resident under an attending without that designation. Making available pocket-sized devices to successfully trained second- and third-year residents has not only allowed frequent use, teaching and advanced imaging, but has promoted a better understanding of disease presentations through observing bedside physiology and correlation with traditional physical exam findings. In recent observations, we have noted improved patient care by providing residents with a device during a night-hospitalist rotation.33 We rely on the well-recognized tradition of resident-to-resident teaching to augment clinical learning and consider the senior resident class as instructors in basic CLUE for interns, medical, students and interested attendings. As residents graduate and become attendings themselves or with recruitment of trained graduates from other institutions, a program can slowly create a faculty nucleus that is competent in point-of-care ultrasound.
Our program took a total immersion philosophy of making the curriculum mandatory as opposed to elective, allowing our program to scientifically study the process of learning ultrasound without enrollment bias. As a consequence, we have invested teaching resources in each resident and note a persistent 20–25% failure rate of competency in formal CLUE proficiency testing.12 Alternatively, a program choosing to offer an ultrasound elective has obvious advantages compared to mandatory involvement and can utilize the pre-existing curriculum structure of elective months within the schedule. The recruitment of only those residents who want to learn ultrasound creates a healthy environment of self-starters, often residents hoping to apply for cardiology or critical care residencies, who are motivated to learn and eager to apply and teach their imaging skills. By presenting ultrasound as an elective, productive learners will promote the success of the ultrasound curriculum and minimize costs. Importantly, initial success may be necessary to create overall institutional buy-in to later support device purchase or adoption of a mandatory curriculum.
In order to create and sustain a teaching program in CLUE, a facility must exist in which interns and residents can initially learn, practice, and/or refresh imaging skills. In our institution, as in most hospitals, a full-time echocardiographic laboratory is an important and available resource. We formed an early collaboration with the sonographers that allowed residents to learn CLUE on patients undergoing echocardiography. As most of CLUE involves simple cardiac ultrasound and pulmonary imaging, sonographers quickly became eager and competent teachers of the imaging technique. Our sonographers attended the CLUE didactic lectures and helped during the hands-on portion of the class. In addition, we have integrated the CLUE pulmonary views into the standard echocardiographic imaging protocol, which has provided residents with a gold-standard CLUE obtained by a sonographer on every patient undergoing echocardiography. In this manner, residents can use the hospital's echo lab not only to practice imaging skills under the guidance of sonographer experts but also to review and compare their imaging with prior CLUE studies in a large, growing clinical database of all patients who have undergone echocardiography.
Although initiating a program may be a daunting task, substantial resources already exist in sonographers, the hospital echo or radiology lab, and resident teachers. Furthermore, identifying young faculty in cardiology, emergency medicine, obstetrics-gynecology, or radiology to mentor an ultrasound elective will provide the start for motivated internal medicine residents to self-perpetuate teaching within the program's elective rotations, particularly in the setting of device availability.
Question 4: What learning considerations are specific to ultrasound?
Task 4: We emphasize practical imaging skill acquisition
By testing graduates who have completed our program, we strongly suspect that the learning of ultrasound is highly related to imaging skills. The CLUE-CEX, a clinical exercise assessment method similar in format to that of the mini-CEX procedure endorsed by the American Board of Internal Medicine,34 has been our program's mechanism to assess imaging and interpretative skills and didactic knowledge and has been described previously.12 In a study of the first four years of consecutive CLUE-CEX testing, we have found that individual performance (n = 41) on the CLUE CEX does not correlate with in-training examination scores, suggesting that the resident who had good knowledge-retention capabilities did not necessarily have good imaging skills. Similarly, in a study of 57 medical students randomized to three different ultrasound curriculum models, it was noted that expert-guided image acquisition was important to a focused cardiac ultrasound examination.35 In a recent study of retention of separate imaging and knowledge-based ultrasound skills as stratified by repeat CLUE CEX testing, residents (n = 30) quickly lost ultrasound imaging skills when not physically practiced within one to two years.36
Recognizing the significant educational requirement to perform physical imaging, we have concluded that a majority of teaching must occur in the clinical setting in a consistent, standardized manner. We emphasize right-handed imaging, approaching from the patient's right, and visualizing hand positions and imaging sites as starting in the patient's center (parasternal), drawing a box (lung imaging) around it, and then returning to the center (subcostal). Imaging is always performed in the Cardiac dysfunction, Left atrial enlargement, Ultrasound lung comets, Effusions and Subcostal views (CLUES) sequence accompanied by simultaneous inductive reasoning (“working backward”) to form differential diagnoses. We have incorporated formal CLUE bedside teaching into our cardiology, ward, and ICU rotations where residents can carry pocket-sized ultrasound devices throughout their rotation. Our internal survey of graduating residents has demonstrated that ICU CLUE rounds were the preferred learning environment when compared to all other venues, lectures, website, or echo laboratory training. Typically, we expect residents to image under guidance of an expert physician or sonographer for the first 30 CLUE studies they perform. Recently, through the development of the program we have advanced the CLUE-CEX proficiency testing to occur after the internship year rather than the third year, and therefore, residents perform many more autonomous studies by graduation than originally published.12 We are currently exploring the potential of telementoring37 as a mechanism in which users outside of our hospital can learn to image with real-time feedback through readily available social networking internet sites.
In addition to emphasizing imaging skills, we also recognized the need to educate residents on image interpretation and diagnostic criteria and therefore employed numerous teaching techniques including didactics, self-directed learning, and bedside teaching. A core curriculum of lectures is used to provide initial instruction on how to use the ultrasound device and obtain and interpret images. Over the years of development, these didactic lectures have been shortened and now frequently last less than 20 minutes and are supplemented by other teaching modalities such as using “earworms” and hands-on training, resulting in a cumulative hour dedicated to a single topic each month (Table 3). A CLUE earworm video lesson is set to a song with frequently repeated phrases set to repetitive images that pertain to a CLUE key concept, with the intent to enhance the student's retention.38,39 Also during the conference, residents image and have their live CLUE images projected in front of the entire class, often in a race against the clock or another resident to increase catecholamines during imaging practice. Such catecholamine-enhancement has been shown to increase amygdala learning and memory storage.40,41 Each month a new topic is introduced and old topics are reviewed, with constant reinforcement of the vertical curriculum structure of procedural skills.
Table 3.
Lecture schedule and goals.
| MONTHLY CONFERENCE TOPIC CONTENT | |
|---|---|
| Introductory lecture | CLUE program requirements, competency, recording of results, terminology |
| CLUE imaging sequence | How to hold the probe, imaging sequence, device operation |
| Cardiac dysfunction, LAE signs | Obtaining the parasternal long-axis view for estimation of LVEF and left atrial size. diagnostic criteria and pitfalls |
| Ultrasound lung comets | Obtaining lung apical views, defining lung comets, distribution and prognosis. pitfalls, interstitial disease vs. edema, pneumothorax |
| Effusions, pleural | Lung basilar imaging, empyema, CHF |
| Subcostal IVC, RV enlargement | Subcostal four-chamber view for RV enlargement, back-up view for LVEF, pericardial effusion, importance and limitations of IVC vs JVP estimates |
| Ultrasound physics | Device knobology, discussion and demonstration of common artifacts, clinical pitfalls |
| Advanced topic: atherosclerosis | Carotid plaque, fatty liver, abdominal aortic aneurysm |
| Advanced topics: code blue, DVT, hydronephrosis | Use in code blue, deep vein thrombosis 2-point imaging, hydronephrosis |
| March madness: imaging speed competition | Speed competitions in CLUE to reinforce imaging under pressure |
| Cases: unknowns | Patient or review case studies |
| CLUE final | Summary lecture of year's research, journal club, program development, resident recognition |
Self-directed learning importantly helps the program to shift valuable conference time from lecturing to hands-on imaging while enabling continued instruction during residency off-hours. Recognizing that diagnostic knowledge, interpretative skills, and physiologic mechanisms could be taught online, a mobile website was created to allow residents access to a myriad of materials for reference such as monthly lectures slides, a self-guided seven-day course, CLUE-case videos, audio “How to” guides, and pocket references (Fig. 3). Each resident has a unique login to allow them to take image quizzes and “save lives,” indicative of the number of correct responses to online CLUE illustrative case questions. As they accumulate saved lives (ie, points), a scoreboard of all of their classmates is posted at the beginning of each monthly conference and on the homepage of our website to encourage friendly competition and more practice. A total of >250 lives saved is a necessary requirement prior to a resident taking the CLUE-CEX. Ten lives is automatically subtracted each month from the resident's total if no website use is detected, in order to motivate students to frequently revisit the website. Questions within the quizzes are categorized based on different views or clinical competencies such as general knowledge, PLAX, subcostal view, lung imaging, and vascular imaging. These groupings allow for the website system to track topics in which the student's knowledge is deficient and direct questions specifically toward that area.
Figure 3.
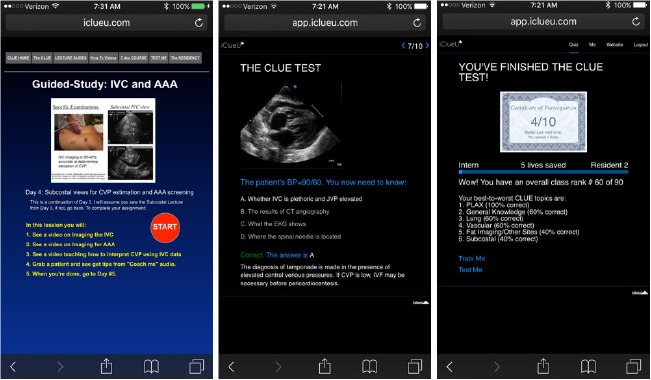
Website learning.
Notes: Three “screen shots” of mobile website. Left panel, example of 7-day Guided Study; center panel, example of quiz question that is worth a life saved if answered correctly; right panel, example of summary screen after a 10-question quiz showing user ranking within class and correct answers by category.
Summary and Conclusions
In retrospect, we believe that our program's navigation through Tasks 1–4 in succession was necessary in order to create a viable curriculum. The philosophy choice of Task 1 determined that a vertical curriculum was needed, where repetition of a fundamental examination was emphasized and more advanced topics were progressively added upon mastery of prior lessons. The alternative was a horizontal curriculum where separate standardized limited examinations would have to be learned in series, each imaging protocol chosen based on program-specific biases such as faculty subspecialty or patient mix. Since a vertical curriculum was used, Task 2 defined the necessary core examination to reinforce and build upon. Such a core examination was easily mastered by sonographers and residents, unrecognized teaching resources, as described in Task 3, that spread within our institution a common methodology and language in which to describe, teach, and reproduce findings. Finally, in the environment provided by Tasks 1–3, Task 4 created an innovative curriculum that emphasized the formation and reinforcement of procedural memories in order to retain imaging skills through clinical practice.
We recognize that our particular pathway has been made in retrospect to structure the discussion of ultrasound curricula development as a whole and is subject to a recollection bias. However, since the time our program was developed, multiple residencies and fellowships in emergency medicine, critical care, and internal medicine have created ultrasound curriculae that can be categorized by the structure provided in this paper. We hope that this discussion of our program's observations and specific tasks in a collaborative environment will assist the initial development of other ultrasound programs in general medicine.
Author Contributions
Conceived: MN, BJK. Wrote the first draft of the manuscript: MN, BJK. Contributed to the writing of the manuscript: MN, BJK, SAA, DJS, JNP. Agreed with manuscript results and conclusions: MN, BJK, SAA, DJS, JNP. Jointly developed the structure and arguments for the paper: MN, BJK. Made critical revisions and approved final version: MN, BJK, SAA, DJS, JNP. All authors reviewed and approved of the final manuscript.
Acknowledgments
We thank Melisa Reasner McGuire Health Sciences Library at Scripps Mercy Hospital for their help in obtaining articles for our review and the sonographers at the Scripps Mercy echo lab. We also thank Dudie Keane for her administrative assistance.
Footnotes
Peer Review:Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1612 words, excluding any confidential comments to the Academic Editor.
Competing Interests:Authors disclose no potential conflicts of interest.
Funding:Authors disclose no external Funding sources.
Paper subject to independent expert single-blind peer review. All editorial decisions made by independent Academic Editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of Competing Interests and Funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
References
- 1.Kimura B.J., Gilcrease GW III, Phan J.N., Showalter B.K., Wolfson T. Diagnostic performance of a pocket-sized ultrasound device using a quick-look cardiac imaging protocol. Am J Emerg Med. 2012; 30: 32–36. [DOI] [PubMed] [Google Scholar]
- 2.Liebo M.J., Israel R.L., Lillie E.O., Smith M.R., Rubenson D.S., Topol E.J. Is pocket mobile echocardiography the next-generation stethoscope? A cross-sectional comparison of rapidly acquired images with standard transthoracic echocardiography. Ann Intern Med. 2011; 155(1): 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kimura B.J., DeMaria A.N. Technology insight: hand-carried ultrasound cardiac assessment—evolution, not revolution. Nat Clin Pract Cardiovasc Med. 2005; 2(4): 217–223. [DOI] [PubMed] [Google Scholar]
- 4.Kimura B.J., DeMaria A.N. Empowering physical examination: the “laying on” of ultrasound (editorial). JACC Cardiovasc Imaging. 2008; 1: 602–604. [DOI] [PubMed] [Google Scholar]
- 5.Mangione S., Neiman L.Z. Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency. JAMA. 1997; 278(9): 717–722. [PubMed] [Google Scholar]
- 6.Kimura B.J., Pezeshki B., Frack S.A., DeMaria A.N. Feasibility of “limited” echo imaging: characterization of incidental findings. J Am Soc Echocardiogr. 1998; 11: 746–750. [DOI] [PubMed] [Google Scholar]
- 7.Kimura B.J., DeMaria A.N. Indications for limited echo imaging: a mathematical model. J Am Soc Echocardiogr. 2000; 13: 855–861. [DOI] [PubMed] [Google Scholar]
- 8.Kimura B.J., Willis C.L., Blanchard D.G., DeMaria A.N. Limited cardiac ultrasound examination for cost-effective echo referral. J Am Soc Echocardiogr. 2002; 15: 640–646. [DOI] [PubMed] [Google Scholar]
- 9.Kimura B.J., Shaw D.J., Agan D.L., Amundson S.A., Ping A.C., DeMaria A.N. Value of a cardiovascular limited ultrasound examination using a hand-carried ultrasound device on clinical management in an outpatient medical clinic. Am J Cardiol. 2007; 100: 321–325. [DOI] [PubMed] [Google Scholar]
- 10.Kimura B.J., Yogo N., O'Connell C., Phan J.N., Showalter B.K., Wolfson T. Cardiopulmonary limited ultrasound examination for “quick-look” bedside application. Am J Cardiol. 2011; 108(4): 586–590. [DOI] [PubMed] [Google Scholar]
- 11.Kimura B.J., Shaw D.J., Amundson S.A., Phan J.N., Blanchard D.G., DeMaria A.N. Cardiac limited ultrasound exam techniques to augment the bedside cardiac physical. J Ultrasound Med. 2015; 34: 1683–1690. [DOI] [PubMed] [Google Scholar]
- 12.Kimura B.J., Amundson S.A., Phan J.N., Agan D.L., Shaw D.J. Observations during development of a training program in cardiovascular limited ultrasound examination for internal medicine residency. J Hosp Med. 2012; 7(7): 537–542. [DOI] [PubMed] [Google Scholar]
- 13.Kimura B.J., Amundson S.A., Willis C.L., Gilpin E.A., DeMaria A.N. Usefulness of a hand-held ultrasound device for the bedside examination of left ventricular function. Am J Cardiol. 2002; 90(9): 1038–1039. [DOI] [PubMed] [Google Scholar]
- 14.Lew W., Henning H., Schelbert H., Karliner J.S. Assessment of mitral valve E point-septal separation as an index of left ventricular performance in patients with acute and previous myocardial infarction. Am J Cardiol. 1978; 41(5): 836–845. [DOI] [PubMed] [Google Scholar]
- 15.Kimura B.J., Kedar E., Weiss D.E. et al. A hand-carried ultrasound sign of cardiac disease: the left atrium-to-aorta diastolic ratio. Am J Emerg Med. 2010; 28(2): 203–207. [DOI] [PubMed] [Google Scholar]
- 16.Kimura B.J., Fowler S.J., Fergus T.S. et al. Detection of left atrial enlargement using hand-carried ultrasound devices: implications for bedside examination. Am J Med. 2005; 118(8): 912–916. [DOI] [PubMed] [Google Scholar]
- 17.Bouzas-Mosquera A., Broullón F.J., Álvarez-García N. et al. Left atrial size and risk for all-cause mortality and ischemic stroke. CMAJ. 2011; 183(10): E657–E664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Secko M.A., Lazar J.M., Salciccioli L.A., Stone M.B. Can junior emergency physicians use E-point septal separation to accurately estimate left ventricular function in acutely dyspneic pateints? Acad Emerg Med. 2011; 18(11): 1223–1226. [DOI] [PubMed] [Google Scholar]
- 19.Volpicelli G., Elbarbary M., Blaivas M. et al. ; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38(4): 577–591. [DOI] [PubMed] [Google Scholar]
- 20.Liteplo A.S., Marill K.A., Villen T. et al. Emergency thoracic ultrasound in the differentiation of the etiology of shortness of breath (ETUDES): sonographic B-lines and N-terminal pro-brain-type natriuretic peptide in diagnosing congestive heart failure. Acad Emerg Med. 2009; 16(3): 201–210. [DOI] [PubMed] [Google Scholar]
- 21.Kataoka H., Takada S. The role of thoracic ultrasonography for evaluation of patients with decompensated chronic heart failure. J Am Coll Cardiol. 2000; 35: 1638–1646. [DOI] [PubMed] [Google Scholar]
- 22.Mai T.V., Shaw D.J., Amundson S.A. et al. Learning to apply the pocket ultrasound device on the critically-ill: comparing six “quick look” signs for quality and prognostic values during initial use by novices. Crit Care. 2013; 17(5): 448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ercan S., Davutoglu V., Altunbas G. et al. Prognostic role of incidental pleural effusion diagnosed during echocardiographic evaluation. Clin Cardiol. 2014; 37(2): 115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gustafsson M., Alehagen U., Johansson P. Imaging congestion with a pocket ultrasound device: prognostic implications in patients with chronic heart failure. J Card Fail. 2015; 21: 548–554. [DOI] [PubMed] [Google Scholar]
- 25.Garibyan V.N., Phan J.N., Showalter B.K., Kimura B.J. Can a quick-look lung ultrasound exam performed during echocardiography provide valuable information? The prognostic value of comets and effusions. J Am Coll Cardiol. 2014; 63: A259. [Google Scholar]
- 26.Bedetti G., Gargani L., Corbisiero A., Frassi F., Poggianti F., Mottola G. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound. 2006; 4: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fremont B., Pacouret G., Jacobi D. et al. Prognostic value of echocardiographic right/left ventricular end-diastolic diameter ration in patients with acute pulmonary embolism. Chest. 2008; 133: 358–362. [DOI] [PubMed] [Google Scholar]
- 28.Goonewardena S.N., Gemignani A., Ronan A. et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008; 1: 595–601. [DOI] [PubMed] [Google Scholar]
- 29.Kanji H.D., McCallum J.L., Bhagirath K.M. et al. Curriculum development and evaluation of hemodynamic critical care ultrasound: a systematic review of the literature. Crit Care. 2016; 44(8): e742–e750. [DOI] [PubMed] [Google Scholar]
- 30.Bahner D., Blaivas M., Cohen H.L. et al. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med. 2008; 27(2): 313–318. [DOI] [PubMed] [Google Scholar]
- 31.Spencer K.T., Kimura B.J., Korcarz C.E., Pellikka P.A., Rahko P.S., Siegel R.J. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013; 26(6): 567–581. [DOI] [PubMed] [Google Scholar]
- 32.Via G., Hussain A., Wells M. et al. ; International Liaison Committee on Focused Cardiac UltraSound (ILC-FoCUS); International Conference on Focused Cardiac UltraSound (IC-FoCUS). International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014; 27(7): 683.e1–683.e33. [DOI] [PubMed] [Google Scholar]
- 33.Tsai B.T., Dahms E.B., Waalen J., Kimura B.J. Actual use of pocket-size ultrasound devices for cardiovascular examination by trained physicians during a hospitalist rotation (abstract, presented at AIUM, NY, New York, 2016). [DOI] [PMC free article] [PubMed]
- 34.Norcini J.J., Blank L.L., Duffy F.D., Fortna G.S. The mini-CEX: a method for assessing clinical skills. Ann Intern Med. 2003; 138(6): 476–481. [DOI] [PubMed] [Google Scholar]
- 35.Cawthorn T.R., Nickel C., O'Reilly M. et al. Development and evaluation of methodologies for teaching focused cardiac ultrasound skills to medical students. J Am Soc Echocardiogr. 2014; 27: 302–309. [DOI] [PubMed] [Google Scholar]
- 36.Kimura B.J., Sliman S., Waalen J., Amundson S.A., Shaw D.J. Retention of ultrasound skills and training in “point-of-care” cardiac ultrasound. J Am Soc Echocardiogr. 2016. pii: S0894-7317(16)30177-8. doi: 10.1016/j.echo.2016.05.013. [Epub ahead of print] PMID: 27372559. [DOI] [PubMed] [Google Scholar]
- 37.Mai T.V., Ahn D.T., Phillips C., Agan D.L., Kimura B.J. Feasibility of remote real-time guidance of a cardiac examination performed by novices using a pocket-sized ultrasound device. Emerg Med Int. 2013; 2013: 627230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Purnell-Webb P., Speelman C.P. Effects of music on memory for text. Percept Mot Skills. 2008; 106(3): 927–957. [DOI] [PubMed] [Google Scholar]
- 39.Kilgour A.R., Jakobson L.S., Cuddy L.L. Music training and rate of presentation as mediators of text and song recall. Mem Cognit. 2000; 28(5): 700–710. [DOI] [PubMed] [Google Scholar]
- 40.Joëls M., Pu Z., Wiegert O., Oitzl M.S., Krugers H.J. Learning under stress: how does it work? Trends Cogn Sci. 2006; 10(4): 152–158. [DOI] [PubMed] [Google Scholar]
- 41.McGaugh J.L. The amygdala modulates the consolidation of memories of emotionally arousing experiences. Annu Rev Neurosci. 2004; 27: 1–28. [DOI] [PubMed] [Google Scholar]


