Abstract
Introduction
The current study aimed to characterize weight change trajectories, and their concomitant associations with prospectively measured dieting and other disordered eating behaviors, among initially non-overweight adolescents during the transition to adulthood.
Methods
A population-based sample (n=1,091) self-reported their height/weight, dieting, unhealthy weight control behaviors, and binge eating at 5-year intervals between 1998/1999 and 2013/2014, spanning early/middle adolescence through middle/late young adulthood. Data were analyzed in 2016/2017.
Results
Groups were categorized as those who were never overweight (n=562); were overweight during at least one measurement point and gained weight more rapidly (n=246) or gradually (n=238) than their peers; or were overweight during at least one measurement point but returned to non-overweight status by middle/late young adulthood (n=45). Thus, nearly half of adolescents became overweight during the transition to adulthood. Those who were never overweight had the lowest rates of dieting (males: F[9,1314]=2.54, p=0.0069, females: F[9,1927]=3.02, p=0.0014) and unhealthy weight control behaviors (males: F[9,1313]=3.30, p=0.0005, females: F[9,1927]=3.02, p=0.0014), whereas some of these behaviors tended to track with weight gain in rapid and gradual weight gainers.
Conclusions
Although adolescents who are already overweight are most frequently targeted for weight gain prevention and early intervention programs, results suggest that healthy lifestyle interventions could also benefit individuals who may be perceived as low risk for overweight in adulthood by nature of being non-overweight in adolescence. Dieting and unhealthy weight control behaviors tended to be associated with weight gain, suggesting that they are ineffective in addition to being potentially harmful.
INTRODUCTION
Youth with overweight/obesity are at elevated risk for tracking excess weight status into adulthood,1–3 and show steeper weight gain trajectories throughout development than non-overweight youth.4,5 Certain weight change trajectories may predict adverse health outcomes later in life.6–10 However, in the current obesogenic environment, risk for overweight/obesity is not limited only to those with excess weight early in life.
The transition from adolescence to young adulthood, which is characterized by increased autonomy over eating behavior related to greater financial independence and new living environments, is critical for the consolidation of health-related behaviors that may set the stage for later overweight/obesity risk.11,12 Indeed, prospective data suggest that aging-related weight gain is steeper during young adulthood than other developmental periods in adulthood.13–15 Moreover, early rapid weight gain during young adulthood is not only associated with steeper weight gain trajectories later in life,16 but also with enhanced risk for obesity-related comorbidities.6 Thus, weight change patterns during this transition warrant further attention.
It is important to identify behavioral factors associated with weight change trajectories among adolescents to inform foci of prevention efforts. Previous longitudinal research suggests that dieting and disordered eating behaviors (e.g., unhealthy weight control behaviors [UWCBs], such as skipping meals or using laxatives; binge eating] exert the strongest effects on obesity risk, whereas other diet- and activity-related patterns (e.g., energy dense food consumption, sedentary behavior) are less consistent predictors.17 Binge eating, dieting, and other UWCBs peak in onset during adolescence,18,19 are associated with weight gain,20 and have severe medical and psychosocial consequences aside from overweight/obesity.21 Whether and how they track with weight change patterns and associated overweight/obesity risk is currently unclear.
This study aims to characterize weight trajectories related to healthy versus unhealthy weight status in young adulthood among adolescents who were initially non-overweight. A secondary aim is to investigate whether dieting and disordered eating behaviors are associated with distinct weight change trajectories throughout this developmental transition. Based on the previous literature,13–15 most adolescents were expected to gain weight during the transition to young adulthood, and dieting and disordered eating behaviors in adolescence were expected to be associated with the steepest weight gain trajectories.20 Findings from this study are intended to inform the selection of adolescents at initially low risk for overweight/obesity who could nevertheless benefit from healthy lifestyle interventions, as well as timing and content of prevention and early intervention programs for excess weight gain during young adulthood.
METHODS
Study Sample
Data were drawn from four waves of Project Eating and Activity in Teens and Young Adults (Project EAT), a 15-year longitudinal study of eating, activity, and weight-related factors among young people. Baseline participants were 4,746 middle and high school students in the Minneapolis/St. Paul, Minnesota metropolitan area who completed in-class surveys and anthropometric measures during early/middle adolescence (EAT-I: Time 1 [T1], ages 11–18 years) during the 1998–1999 school year.22 Follow-up data were collected via mailed and online surveys 5-, 10-, and 15-years later (EAT-II: Time 2 [T2]=middle adolescence/early young adulthood, mean age=19.3, SD=1.7 years; EAT-III: Time 3 [T3]=early/middle young adulthood, mean age=25.2, SD=1.6 years; EAT-IV: Time 4[T4]=middle/late young adulthood, mean age=31.0, SD=1.7 years) to investigate changes in weight-related outcomes and their correlates. Among the 3,304 participants who were not overweight at T1, 443 males and 648 females self-reported their height and weight at all four time points and are included in the current analyses. Non-overweight participants with and without complete BMI data did not differ on BMI, dieting, UWCBs, or binge eating at T1 (all p>0.05). Study protocols were approved by the University of Minnesota’s IRB.
Measures
The EAT survey assesses weight status, dietary and weight control behaviors, physical activity, and associated factors. Test–retest data at T1 were collected on 161 adolescents completing identical versions of the EAT-I survey approximately two weeks apart23; likewise, test–retest reliability at T4 were collected on 103 adult participants who completed the EAT-IV survey twice within a 1- to 4-week period.
Self-reported height and weight were used to determine BMI (kg/m2). Overweight refers to a BMI ≥85th percentile for age and gender24 at T1 and T2 when participants were still primarily adolescents,25,26 and a BMI ≥25 kg/m2 at T3 and T4 when participants were adults.27 Correlations between reported and measured BMI were r =0.85 for females and r =0.89 for males at T1,28 and at T3 were r =0.98 for females and r =0.95 for males.17,29 Age, sex, and race/ethnicity (dichotomized as white versus non-white) were self-reported. Five levels of SES were based on participant report of the highest educational attainment by either parent at T1. Eligibility for public assistance, eligibility for free/reduced-price school meals, and parental employment status were used to approximate missing SES information.22
Dieting was assessed with the question: How often have you gone on a diet during the last year? By ‘diet’ we mean changing the way you eat so you can lose weight.30 Responses included never, one to four times, five to 10 times, more than 10 times, and I am always dieting (test–retest: T1, r =0.71, T4, r =0.77). Responses at T1 and T4 were associated with measures of weight perceptions, weight control attempts, importance of weight/shape, and body dissatisfaction (all p<0.001). UWCBs were assessed with the question: Have you done any of the following things in order to lose weight or keep from gaining weight during the past year? Options included: fasted, ate very little food, used a food substitute (powder or a special drink), skipped meals, smoked more cigarettes, took diet pills, made myself vomit, used laxatives, and used diuretics. The most commonly reported UWCBs across most time points for males and females were ate very little food (males, 9.5%–19.2%, females, 36.2%–45.7%) and skipped meals (males, 10.4%–18.7%, females, 30.5%–50.4%); 10.9%–16.9% of males and 35.0%–46.9% of females reported engaging in multiple types of UWCBs across T1 to T4. Because of low base rates of many individual UWCBs in this sample, and consistent with previous EAT research,20 responses were dichotomized into any versus no UWCBs (test–retest agreement: T1=83%, T4=86%, Cronbach’s α range across T1 to T4=0.66–0.78 for males, 0.63–0.71 for females). Binge eating was ascertained by an affirmative response to both of the following questions: In the past year, have you ever eaten so much food in a short period of time that you would be embarrassed if others saw you?; During the times when you ate this way, did you feel you couldn’t stop eating or control what or how much you were eating?31 These items have good concurrent validity and test–retest reliability32 (T1 test–retest agreement=92% for overeating, 84% for loss of control, T4=90% for overeating, 78% for loss of control).
Statistical Analysis
Analyses included 1,091 adolescents (59.4% female) who had BMI data at all four time points and were non-overweight at T1. Participants’ T1–T4 weight trajectories were categorized heuristically based on preselected weight change patterns. Categories were derived separately for the older (n=800) and younger cohort (n=291), because cohorts were in different developmental stages when presenting for data collection at each time point which could impact their weight change patterns across developmental transitions.24
Trajectory groups were characterized by those who were non-overweight at all four time points, those whose BMI increased to overweight at T4 with a rate of increase below the median for his/her cohort, those whose BMI increased to overweight at a rate above the median for his/her cohort, and those who were overweight at T2 or T3 but returned to non-overweight status by T4. Rates of BMI increase for the gradual and rapid gainers were calculated by fitting a linear regression to the four BMI values among those who became overweight stratified by gender and age cohort. Trajectory groups were compared on demographic variables and dieting, UWCBs, and binge eating at T1 using chi-square tests for categorical variables and ANOVA for continuous variables. Because prior research suggests that the developmental timing of shifts in weight and initiation of dieting/disordered eating behaviors differs by gender,33–35 and the three-way interaction between trajectory group × time-point × gender was significant or trending towards significance for UWCB (F[9,3233]=2.72, p=0.0037) and dieting (F[9,3241]=1.78, p=0.0663), respectively (but not binge eating, p=0.9834), gender-stratified repeated-measures logistic regressions were used to model the odds of dieting, UWCBs, and binge eating from T1 to T4 across the four trajectory groups. Generalized estimating equations were used to account for correlations within individuals. All models included main effects for trajectory group and time point, and their interaction, and were adjusted for age, race, and SES. Significant main effects and interactions were probed using pairwise contrasts, with the never overweight group serving as the reference.
Because attrition from the T1 sample was not random, data (including repeated-measures logistic regressions) were weighted with the inverse of the estimated probability that an individual responded at all four time points.36 Use of nonresponse sampling weights along with subpopulation analysis generates estimates representing the demographic composition of the original EAT sample corresponding to the analytic subgroups. Percentages reported henceforth are weighted to represent the baseline population.
RESULTS
The trajectory group characterized by participants who were non-overweight at all four time points (mean T4 BMI=22.48, SD=0.11) included 381 females (54.2%) and 181 males (37.5%). The gradually gaining group, characterized by participants whose BMI increased to overweight at T4 (mean T4 BMI=28.30, SD=0.16) at a rate below the median for his or her cohort, included 115 females (20.7%) and 131 males (29.3%). The rapidly gaining group, characterized by participants whose BMI increased to overweight at a rate above the median for his or her cohort (mean T4 BMI=30.31, SD=0.16), included 132 females (22.4%) and 106 males (26.3%). Finally, the group characterized by participants who were overweight at T2 or T3 but returned to non-overweight by T4 (mean T4 BMI=23.68, SD=0.36), included 20 females (2.6%) and 25 males (7.0%). Within the full sample, significant trajectory group differences were observed for gender, race/ethnicity, and SES (all p<0.001), but not age (p=0.22).
T1 dieting was associated with increased odds of falling into the gradually gaining (p=0.01) and rapid gaining groups (p=0.047), relative to the never overweight group (chi-square, 9.06; p=0.03); no other T1 dieting or disordered eating construct predicted trajectory group membership in females or males (all p>0.05). Weight trajectories of each group are illustrated in Figures 1 and 2, and demographic characteristics are reported in Table 1.
Figure 1.
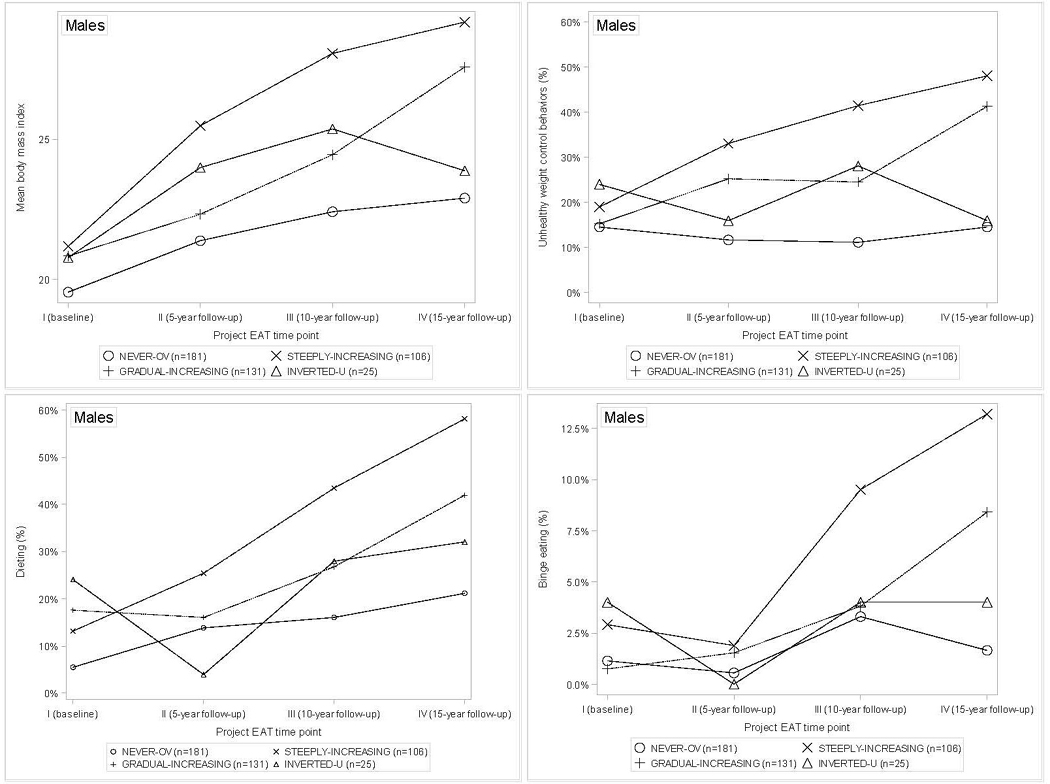
Weight trajectories and unhealthy weight-related behavior trajectories by weight trajectory group over the 15-year transition from adolescence (EAT-I) to adulthood (EAT-IV) among males.
Note: NEVER-OV=never overweight; STEEPLY-INCREASING=overweight at ≥1 of the four time-points and BMI increasing at a rate above the median for age cohort; GRADUAL-INCREASING=overweight at ≥1 of the four time-points and BMI increasing at a rate below the median for age cohort; INVERTED-U=overweight at EAT-II or EAT-III but returned to non-overweight status by EAT-IV. Mean BMIs across the four Project EAT time-points for each weight trajectory group are included for illustrative purposes only, and do not reflect statistical comparisons across the trajectory groups.
Figure 2.
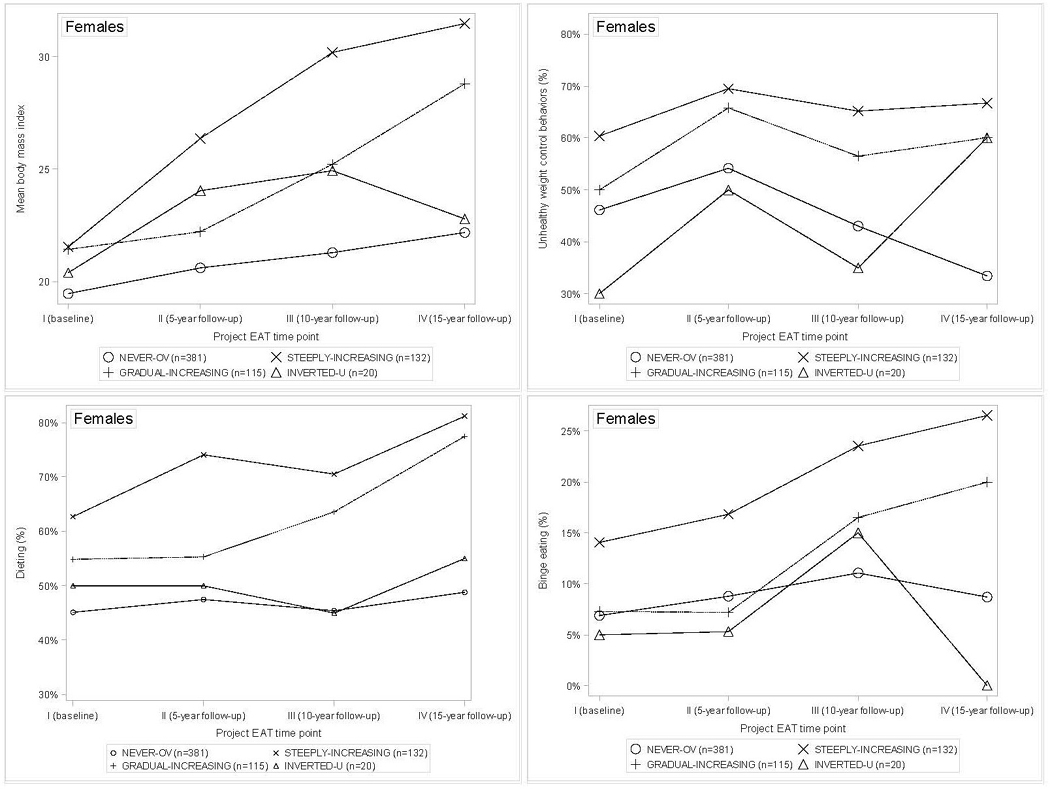
Weight trajectories and unhealthy weight-related behavior trajectories by weight trajectory group over the 15-year transition from adolescence (EAT-I) to adulthood (EAT-IV) among females.
Note: NEVER-OV=never overweight; STEEPLY-INCREASING=overweight at ≥1 of the four time-points and BMI increasing at a rate above the median for age cohort; GRADUAL-INCREASING=overweight at ≥1 of the four time-points and BMI increasing at a rate below the median for age cohort; INVERTED-U=overweight at EAT-II or EAT-III but returned to non-overweight status by EAT-IV. Mean BMIs across the four Project EAT time-points for each weight trajectory group are included for illustrative purposes only, and do not reflect statistical comparisons across the trajectory groups.
Table 1.
Descriptive Characteristics at EAT-I
| Variable | Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|---|
| Males | n=181 | n=131 | n=106 | n=25 |
| Age, years | 14.60±1.62 | 14.91±1.60 | 15.37±1.87 | 15.38±1.64 |
| SES | ||||
| High | 119 (47%) | 73 (29%) | 48 (19%) | 13 (5%) |
| Medium | 34 (34%) | 33 (36%) | 26 (27%) | 4 (3%) |
| Low | 24 (28%) | 24 (26%) | 31 (36%) | 7 (10%) |
| Race/ethnicity | ||||
| White | 140 (40%) | 98 (30%) | 79 (24%) | 18 (6%) |
| Black | 11 (32%) | 13 (41%) | 7 (27%) | 0 (0%) |
| Hispanic | 3 (23%) | 3 (18%) | 5 (58%) | 0 (0%) |
| Asian | 18 (26%) | 13 (26%) | 12 (29%) | 6 (19%) |
| Mixed/Other | 8 (72%) | 3 (16%) | 2 (11%) | 0 (0%) |
| BMI (kg/m2) | 19.18±1.97 | 20.63±2.29 | 21.35±2.13 | 20.93±1.92 |
| Females | n=381 | n=115 | n=132 | n=20 |
| Age, years | 14.83±1.33 | 15.10±1.38 | 14.67±1.41 | 14.71±1.24 |
| SES | ||||
| High | 221 (65%) | 52 (18%) | 52 (15%) | 10 (3%) |
| Medium | 83 (48%) | 25 (20%) | 34 (26%) | 8 (5%) |
| Low | 73 (48%) | 36 (23%) | 43 (28%) | 2 (1%) |
| Race/ethnicity | ||||
| White | 283 (61%) | 73 (16%) | 89 (19%) | 17 (4%) |
| Black | 16 (32%) | 14 (43%) | 9 (22%) | 1 (2%) |
| Hispanic | 12 (54%) | 3 (11%) | 6 35%) | 0 (0%) |
| Asian | 57 (58%) | 16 (15%) | 21 (25%) | 2 (2%) |
| Mixed/Other | 10 (40%) | 7 (29%) | 6 (31%) | 0 (0%) |
| BMI (kg/m2) | 19.44±1.74 | 21.48±2.04 | 21.46±1.68 | 20.30±1.52 |
Note: Group 1=never overweight; Group 2=overweight at ≥1 of the four time-points and BMI increasing at a rate below the median for age cohort; Group 3=overweight at ≥1 of the four time-points and BMI increasing at a rate above the median for age cohort; Group 4=overweight at EAT-II or EAT-III but returned to non-overweight status by EAT-IV.
EAT, Eating and Activity in Teens and Young Adults
Among males, weight trajectory group, time, and their interaction all were associated with concomitant prospectively measured dieting and UWCBs (all p<0.05; Table 2). Both dieting and UWCBs generally increased over time across weight trajectory groups, and the never overweight group generally showed the lowest rates of engaging in these behaviors across time relative to the other three groups. Significant interactions are illustrated in Figure 1. For most weight trajectory groups, endorsement of dieting and UWCBs largely paralleled weight trajectories over time. That is, males in the never overweight category endorsed consistently low rates of dieting and UWCBs from T1 to T4, whereas gradual gainers showed gradually rising rates of both behaviors from T1 to T4, and rapid gainers showed the most rapid increases in rates of both behaviors from T1 to T4 (with ≅ 50% of this latter trajectory group engaging in each of these behaviors by T4). The group that was overweight but later returned to non-overweight status showed the most inconsistent patterns of dieting and UWCBs over time. For males, weight trajectory group was marginally associated with concommitant prospectively measured binge eating (p=0.05), whereas time (p=0.09) and the time × group interaction (p=0.29) were not significantly associated.
Table 2.
Associations Between Weight Trajectory Group and Concomitant, Prospectively Measured Unhealthy Weight-related Behaviors
| Predictor | Main effect for trajectory group | Main effect for time | Interaction | Group contrasts |
|---|---|---|---|---|
| Males | ||||
| Unhealthy weight control behaviors | F(3,430)=17.32; p<0.0001;ηp2=0.03 | F(3,1313)=3.55; p=0.014; ηp2=0.01 | F(9,1313)=3.30; p=0.0005; ηp2=0.02 | EAT-I: 1=2=3=4 EAT-II: 1,2,4<3 EAT-III: 1<2,3,4; 2<3 EAT-IV: 1<2,3; 2>4 |
| Dieting | F(3,430)=14.97; p<0.0001; ηp2=0.03 | F(3,1314)=21.48; p<0.0001; ηp2=0.05 | F(9,1314)=2.54; p=0.0069; p=0.0069; ηp2=0.02 | EAT-I: 1<4 EAT-II: 1,2,4<3; 1>4 EAT-III: 1,2<3 EAT-IV: 1,2,4<3; 1<2; |
| Binge eating | F(3,430)=2.66; p=0.048; ηp2=0.01 | F(3,1304)=2.20; p=0.0862; ηp2=0.01 | F(9,1304)=1.20; p=0.2938; ηp2=0.01 | EAT-I: 1=2=3=4 EAT-II: 1=2=3=4 EAT-III: 1<3,4 EAT-IV: 1<2,3 |
| Females | ||||
| Unhealthy weight control behaviors | F(3,635)=30.74; p<0.0001; ηp2=0.04 | F(3,1920)=2.85; p=0.0363; ηp2=0.00 | F(9,1920)=3.01; p=0.0014; ηp2=0.01 | EAT-I: 1<2; 4<2,3 EAT-II: 1<2,3 EAT-III: 1<2,3 EAT-IV: 1<2,3,4 |
| Dieting | F(3,635)=39.91; p<0.0001; ηp2=0.05 | F(3,1927)=5.16; p=0.0015; ηp2=0.01 | F(9,1927)=3.02; p=0.0014; ηp2=0.01 | EAT-I: 1<2,3 EAT-II: 1<2,3; 3>2,4 EAT-III: 1<2,3; 4<2,3 EAT-IV: 1<2,3; 4<2,3 |
| Binge eating | F(3,635)=9.60; p<0.0001; ηp2=0.01 | F(3,1905)=2.18; p=0.0883; ηp2=0.00 | F(9,1905)=1.46; p=0.1560; ηp2=0.01 | EAT-I: 1=2=3=4 EAT-II: 1<3 EAT-III: 1<3 EAT-IV: 1<2,3 |
Note: Group 1=never overweight; Group 2=overweight at ≥1 of the four time-points and BMI increasing at a rate below the median for age cohort; Group 3=overweight at ≥1 of the four time-points and BMI increasing at a rate above the median for age cohort; Group 4=overweight at EAT-II or EAT-III but returned to non-overweight status by EAT-IV. All models adjusted for age, race, and SES. Boldface indicates statistical significance (p<0.05). ηp2 represents partial eta-squared, obtained from linear model of dichotomous outcomes on same predictors (0.01=a small effect; 0.06=a medium effect; and 0.14=a large effect). For all significant contrasts, p<0.05.
EAT, Eating and Activity in Teens and Young Adults
A similar pattern emerged for females, with weight trajectory group, time, and their interaction all significantly associated with concommitant, prospectively measured dieting and UWCBs (all p<0.05; Table 2), whereas only weight trajectory group was significantly associated with concommitant prospectively measured binge eating (p<0.001). Rates of dieting in females increased over time across trajectory groups, and were lowest for the never overweight group at most time points. However, rates of UWCBs increased from T1 to T2 for all weight trajectory groups, after which longitudinal trends diverged by weight trajectory group (Figure 2). From T2 to T4, rates of UWCBs generally leveled out or slightly decreased among gradual and rapid gainers, and decreased more rapidly for the never overweight group. For the group that became overweight but later returned to non-overweight status, UWCBs decreased from T2 to T3, and then increased from T3 to T4.
DISCUSSION
This study investigated weight trajectories and their associations with dieting and disordered eating behaviors among young adults who were non-overweight during adolescence. One prominent pathway to adult overweight/obesity is through tracking of pediatric overweight/obesity,1 but the gap between pediatric and adult prevalence rates37 suggests that there are individuals in whom overweight/obesity develops in adulthood. Indeed, nearly half of non-overweight adolescent participants in the current sample became overweight during at least one time point while transitioning from adolescence to adulthood, suggesting that healthcare providers should promote healthy lifestyle behaviors with all adolescents, even those who are non-overweight and may not require an overt focus on weight regulation. Moreover, although binge eating did not track with any specific weight gain trajectories (likely because of low base rates at each time point), dieting and UWCBs tracked longitudinally with weight gain trajectories in most trajectory groups. Thus, in addition to being harmful, these behaviors may be ineffective at preventing weight gain (although it is possible that these behaviors develop after weight begins to increase, to counteract weight gain). These data may be useful to clinicians seeking to dissuade young people from engaging in maladaptive weight control behaviors.
The never overweight group, representing the majority of participants in the sample, was characterized by non-overweight status and low rates of dieting and disordered eating behaviors at all four time points. However, despite remaining in the non-overweight category, members of the never overweight group still experienced gradual weight gain throughout follow-up. The gradual and steady weight gain evidenced by this group highlights the need for healthcare providers to track and address patients’ weight gain curves over time,38 as opposed to tailoring interventions to a patient’s weight status at a single time point. Healthcare providers do not routinely discuss healthy eating and activity with their non-overweight patients,39 perhaps because they are perceived to be at low risk for new onset overweight once they have passed key developmental milestones typically associated with weight gain (e.g., transition to young adulthood, pregnancy40,41). However, the current research suggests that interventions focused on promoting healthy weight-related behaviors (e.g., avoiding dieting/UWCBs, increasing physical activity) may have a relevant message at different points throughout the lifespan.42
Gradual and rapid gainers both were characterized by consistent weight gain across each follow-up time point, although rates varied by group. Interestingly, these groups also showed the highest rates of dieting and UWCBs over time, underscoring that these behaviors are not only potentially harmful (e.g., as evidenced by biological markers of undernutrition43), but also are not associated with weight reduction/maintenance. Indeed, previous EAT data suggest that dieting and UWCBs predicted BMI increases over 10 years of follow-up, and the current findings extend these data by including an additional 5 years of follow-up, and reporting specific weight change trajectories associated with engagement in these behaviors. Practitioners should routinely assess for the presence of unhealthy weight control practices, particularly among patients who are gaining weight, in order to provide appropriate psychoeducation about the consequences these practices. Patients who are both gaining weight and engaging in UWCBs may require more intensive interventions focused on the importance of gradual and sustainable lifestyle changes intended to promote prolonged weight regulation without adverse effects on health and well-being (e.g., decreasing portion sizes rather than engaging in extreme dietary restriction).
Individuals who gained weight from early/middle adolescence to early/middle young adulthood, followed by a near return to baseline BMI by middle/late young adulthood, comprised the smallest weight trajectory group. This group’s weight loss was accompanied by increased rates of many UWCBs, although findings differed by behavior and by participant gender. Weight loss may reinforce use of these behaviors, potentially marking an enhanced risk for escalation of risky behaviors or even eating disorders. Research shows that it is possible to lose weight and exit overweight/obesity using healthy means,44,45 but it may be challenging for clinicians to help patients who have already remitted from overweight/obesity to discontinue dieting and UWCBs because of concerns about weight regain. Thus, similar to individuals who are gaining weight and engaging in unhealthy weight control practices, those who have lost weight through unhealthy means may benefit from intensive interventions addressing healthful approaches to weight loss/maintenance.
Limitations
Study strengths include the large, diverse, community-based sample; prospective assessments of weight, dieting, and disordered eating behaviors over 15 years of follow-up; and the heuristic approach to defining weight trajectory categories, which was informed by methods which healthcare providers would likely use to characterize weight change patterns over time. The use of self-reported height and weight to characterize BMI, which was the main focus of the study, constituted the primary limitation. Although self-reported and measured height and weight had good concordance in this sample,17,28 they are not as accurate as objective measures and may be confounded by lack of knowledge or social desirability factors, thus necessitating replication with investigator-measured indices. Other limitations included the assessment of weight control behaviors based on brief survey items, and the significant attrition that occcured between T1 and T2 (although attrition tapered off during later time points, and sample weighting was utilized to represent the original EAT-I sample).
CONCLUSIONS
Overall, results suggest that weight gain is common during the transition from adolescence to adulthood, although the rate of weight change may vary, or even reverse, at different points in development. Different weight trajectories may be associated with elevated risk for engaging in dieting and UWCBs, which has important implications for screening and intervention. Notably, the authors examined the relationship between weight trajecories and disordered eating bidirectionally and acknowledge the small effect sizes in both directions. Therefore, future research should identify other concomitant prospective predictors of weight change trajectories, such as behavioral or environmental factors (e.g., physical activity, access to energy dense foods in the home), in order to optimize weight control interventions.
Acknowledgments
The project described was supported by grant R01-HL093247 from the National Heart, Lung, and Blood Institute (PI: Dianne Neumark-Sztainer). Dr. Goldschmidt’s time was supported by grant K23-DK105234 from the National Institute of Diabetes and Digestive and Kidney Diseases, and Dr. Evans’ time was support by grant K01-DK110142 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76(3):653–658. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 2.Freedman DS, Khan LK, Serdula MK, et al. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28(1):10–16. doi: 10.1038/sj.ijo.0802544. https://doi.org/10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. Risk factors and adult body mass index among overweight children: the Bogalusa Heart Study. Pediatrics. 2009;123(3):750–757. doi: 10.1542/peds.2008-1284. https://doi.org/10.1542/peds.2008-1284. [DOI] [PubMed] [Google Scholar]
- 4.Willers SM, Brunekreef B, Smit HA, et al. BMI Development of Normal Weight and Overweight Children in the PIAMA Study. PLoS ONE. 2012;7(6):e39517. doi: 10.1371/journal.pone.0039517. https://doi.org/10.1371/journal.pone.0039517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stuart B, Panico L. Early-childhood BMI trajectories: Evidence from a prospective, nationally representative British cohort study. Nutr Diabetes. 2016;6(3):e198. doi: 10.1038/nutd.2016.6. https://doi.org/10.1038/nutd.2016.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Attard SM, Herring AH, Howard AG, Gordon-Larsen P. Longitudinal trajectories of BMI and cardiovascular disease risk: the national longitudinal study of adolescent health. Obesity (Silver Spring) 2013;21(11):2180–2188. doi: 10.1002/oby.20569. https://doi.org/10.1002/oby.20569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imai CM, Gunnarsdottir I, Gudnason V, et al. Faster increase in body mass index between ages 8 and 13 is associated with risk factors for cardiovascular morbidity and mortality. Nutr Metab Cardiovasc Dis. 2014;24(7):730–736. doi: 10.1016/j.numecd.2014.01.001. https://doi.org/10.1016/j.numecd.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Ziyab AH, Karmaus W, Kurukulaaratchy RJ, Zhang H, Arshad SH. Developmental trajectories of Body Mass Index from infancy to 18 years of age: Prenatal determinants and health consequences. J Epidemiol Community Health. 2014;68(10):934–941. doi: 10.1136/jech-2014-203808. https://doi.org/10.1136/jech-2014-203808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang RC, de Klerk NH, Smith A, et al. Lifecourse childhood adiposity trajectories associated with adolescent insulin resistance. Diabetes Care. 2011;34(4):1019–1025. doi: 10.2337/dc10-1809. https://doi.org/10.2337/dc10-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thearle MS, Votruba SB, Piaggi P, et al. The effect of differing patterns of childhood body mass index gain on adult physiology in American Indians. Obesity (Silver Spring) 2015;23(9):1872–1880. doi: 10.1002/oby.21162. https://doi.org/10.1002/oby.21162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.VanKim NA, Larson N, Laska MN. Emerging adulthood: A critical age for preventing excess weight gain? Adolesc Med State Art Rev. 2012;23(3):571–588. [PubMed] [Google Scholar]
- 12.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring) 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. https://doi.org/10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 13.Williamson DF, Kahn HS, Remington PL, Anda RF. The 10-year incidence of overweight and major weight gain in U.S. adults. Arch Intern Med. 1990;150(3):665–672. https://doi.org/10.1001/archinte.1990.00390150135026. [PubMed] [Google Scholar]
- 14.Rissanen A, Heliovaara M, Aromaa A. Overweight and anthropometric changes in adulthood: A prospective study of 17,000 Finns. Int J Obes. 1988;12(5):391–401. [PubMed] [Google Scholar]
- 15.Dutton GR, Kim Y, Jacobs DR, Jr, et al. 25-year weight gain in a racially balanced sample of U.S. adults: The CARDIA study. Obesity (Silver Spring) 2016;24(9):1962–1968. doi: 10.1002/oby.21573. https://doi.org/10.1002/oby.21573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malhotra R, Ostbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obesity (Silver Spring) 2013;21(9):1923–1934. doi: 10.1002/oby.20318. https://doi.org/10.1002/oby.20318. [DOI] [PubMed] [Google Scholar]
- 17.Quick V, Wall M, Larson N, Haines J, Neumark-Sztainer D. Personal, behavioral and socio-environmental predictors of overweight incidence in young adults: 10-yr longitudinal findings. Int J Behav Nutr Phys Act. 2013;10:37. doi: 10.1186/1479-5868-10-37. https://doi.org/10.1186/1479-5868-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stice E, Killen JD, Hayward C, Taylor CB. Age of onset for binge eating and purging during late adolescence: A 4-year survival analysis. J Abnorm Psychol. 1998;107(4):671–5. doi: 10.1037//0021-843x.107.4.671. https://doi.org/10.1037/0021-843X.107.4.671. [DOI] [PubMed] [Google Scholar]
- 19.Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, Loth K. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. J Am Diet Assoc. 2011;111(7):1004–1011. doi: 10.1016/j.jada.2011.04.012. https://doi.org/10.1016/j.jada.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J Adolesc Health. 2012;50(1):80–86. doi: 10.1016/j.jadohealth.2011.05.010. https://doi.org/10.1016/j.jadohealth.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lock J, Reisel B, Steiner H. Associated health risks of adolescents with disordered eating: How different are they from their peers? Results from a high school survey. Child Psychiatry Hum Dev. 2001;31(3):249–265. doi: 10.1023/a:1026433506298. https://doi.org/10.1023/A:1026433506298. [DOI] [PubMed] [Google Scholar]
- 22.Neumark-Sztainer D, Story M, Hannan PJ, Croll J. Overweight status and eating patterns among adolescents: Where do youths stand in comparison with the healthy people 2010 objectives? Am J Public Health. 2002;92(5):844–851. doi: 10.2105/ajph.92.5.844. https://doi.org/10.2105/AJPH.92.5.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neumark-Sztainer D, Croll J, Story M, et al. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. J Psychosom Res. 2002;53(5):963–974. doi: 10.1016/s0022-3999(02)00486-5. https://doi.org/10.1016/S0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 25.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. https://doi.org/10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 26.Must A, Anderson SE. Body mass index in children and adolescents: considerations for population-based applications. Int J Obes. 2006;30(4):590–594. doi: 10.1038/sj.ijo.0803300. https://doi.org/10.1038/sj.ijo.0803300. [DOI] [PubMed] [Google Scholar]
- 27.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. https://doi.org/10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 28.Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Ann Epidemiol. 2005;15(4):272–278. doi: 10.1016/j.annepidem.2004.08.010. https://doi.org/10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 29.Sirard JR, Hannan PJ, Cutler GJ, Graham DJ, Neumark-Sztainer D. Evaluation of two self-report measures of physical activity with accelerometry in young adults. J Phys Act Health. 2013;10(1):85–96. doi: 10.1123/jpah.10.1.85. https://doi.org/10.1123/jpah.10.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Larson NI, Neumark-Sztainer D, Story M, van den Berg P, Hannan PJ. Identifying correlates of young adults’ weight behavior: Survey development. Am J Health Behav. 2011;35(6):712–725. https://doi.org/10.5993/AJHB.35.6.7. [PMC free article] [PubMed] [Google Scholar]
- 31.Yanovski SZ. Binge eating disorder: Current knowledge and future directions. Obes Res. 1993;1(4):306–324. doi: 10.1002/j.1550-8528.1993.tb00626.x. https://doi.org/10.1002/j.1550-8528.1993.tb00626.x. [DOI] [PubMed] [Google Scholar]
- 32.Nangle DW, Johnson WG, Carr-Nangle RE, Engler LB. Binge eating disorder and the proposed DSM-IV criteria: Psychometric analysis of the Questionnaire of Eating and Weight Patterns. Int J Eat Disord. 1994;16(2):147–157. doi: 10.1002/1098-108x(199409)16:2<147::aid-eat2260160206>3.0.co;2-p. https://doi.org/10.1002/1098-108X(199409)16:2<147::AID-EAT2260160206>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 33.Field AE, Aneja P, Austin SB, et al. Race and gender differences in the association of dieting and gains in BMI among young adults. Obesity (Silver Spring) 2007;15(2):456–464. doi: 10.1038/oby.2007.560. https://doi.org/10.1038/oby.2007.560. [DOI] [PubMed] [Google Scholar]
- 34.Liechty JM, Lee MJ. Longitudinal predictors of dieting and disordered eating among young adults in the U.S. Int J Eat Disord. 2013;46(8):790–800. doi: 10.1002/eat.22174. https://doi.org/10.1002/eat.22174. [DOI] [PubMed] [Google Scholar]
- 35.Guo SS, Huang C, Maynard LM, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord. 2000;24(12):1628–1635. doi: 10.1038/sj.ijo.0801461. https://doi.org/10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 36.Little RJA. Models for non-response in sample surveys. J Am Statist Assoc. 1982;77(378):237–250. https://doi.org/10.1080/01621459.1982.10477792. [Google Scholar]
- 37.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. https://doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tang JW, Kushner RF, Thompson J, Baker DW. Physician counseling of young adults with rapid weight gain: A retrospective cohort study. BMC Fam Pract. 2010;11:31. doi: 10.1186/1471-2296-11-31. https://doi.org/10.1186/1471-2296-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82(1):123–129. doi: 10.1016/j.pec.2010.02.018. https://doi.org/10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laska MN, Pelletier JE, Larson NI, Story M. Interventions for weight gain prevention during the transition to young adulthood: a review of the literature. J Adolesc Health. 2012;50(4):324–333. doi: 10.1016/j.jadohealth.2012.01.016. https://doi.org/10.1016/j.jadohealth.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muktabhant B, Lumbiganon P, Ngamjarus C, Dowswell T. Interventions for preventing excessive weight gain during pregnancy. Cochrane Database Syst Rev. 2012;4:CD007145. doi: 10.1002/14651858.CD007145.pub2. https://doi.org/10.1002/14651858.CD007145.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wing RR, Tate D, Espeland M, et al. Weight gain prevention in young adults: Design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13:300. doi: 10.1186/1471-2458-13-300. https://doi.org/10.1186/1471-2458-13-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guest J, Bilgin A, Pearce R, et al. Evidence for under-nutrition in adolescent females using routine dieting practices. Asia Pac J Clin Nutr. 2010;19(4):526–533. [PubMed] [Google Scholar]
- 44.Watts AW, Loth KA, Peterson C, Boutelle KN, Neumark-Sztainer D. Characteristics of a favorable weight status change from adolescence to young adulthood. J Adolesc Health. 2016;58(4):403–409. doi: 10.1016/j.jadohealth.2015.09.009. https://doi.org/10.1016/j.jadohealth.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boutelle KN, Libbey H, Neumark-Sztainer D, Story M. Weight control strategies of overweight adolescents who successfully lost weight. J Am Diet Assoc. 2009;109(12):2029–2035. doi: 10.1016/j.jada.2009.09.012. https://doi.org/10.1016/j.jada.2009.09.012. [DOI] [PubMed] [Google Scholar]


