Abstract
Introduction
Human papillomavirus vaccination is less prevalent among foreign-born than U.S.-born women and may lead to disparities in human papillomavirus-related cancers in the future. There is limited research on factors associated with vaccination uptake between these two groups. This study examined the association between place of birth and human papillomavirus vaccine uptake, and what determinants of vaccination attenuate this relationship.
Methods
The 2013–2015 National Health Interview Survey data on women was analyzed in 2016, to determine differences in prevalence of human papillomavirus vaccination between foreign- and U.S.-born women. Multivariate binary logistic regression analysis was used to examine the association between foreign born status and human papillomavirus vaccine initiation, after controlling for health insurance status, having a usual source of care, obstetrician/gynecologist visits, Pap tests, length of U.S. residency, and citizenship.
Results
Human papillomavirus vaccination prevalence significantly varied among women born in different regions of the world. European and South American women had the highest vaccination rates among all foreign-born women. Compared with U.S.-born women, foreign-born women were significantly less likely to report human papillomavirus vaccine initiation. This relationship was partially attenuated after adjusting for the covariates. Among foreign-born women Asians were significantly less likely to report human papillomavirus vaccination uptake than white women. Additionally, living in the U.S. for >5 years was significantly associated with vaccine initiation, but attenuated by U.S. citizenship status.
Conclusions
Public health interventions to improve human papillomavirus vaccination need to be developed to address multicultural audiences with limited access to health insurance and health care.
INTRODUCTION
The foreign-born are the fastest growing population in the U.S., and represent diverse subgroups from various regions of the world.1 This population faces barriers to accessing health care, and foreign-born women in particular experience challenges to receiving preventive health care, such as cancer screening and prevention.2,3 Although evidence indicates a decreasing trend in cervical cancer incidence in the U.S., it remains the third most common cancer among women globally.4,5 Foreign-born women are at higher risk for cervical cancer, as secondary prevention through Pap testing in their countries of origin may be less accessible.6,7 For example, regions including Eastern Middle Africa, Central America, and the Caribbean have the highest incidence of cervical cancer globally, and yet most countries in these regions lack national level cancer screening and prevention programs.8 Further, women who migrate to the U.S. from such regions often face barriers to accessing and using healthcare services in the U.S.9 These barriers include limited English proficiency, lack of knowledge about cancer prevention, difficulty navigating the U.S. healthcare system, and structural barriers, which include lack of health insurance and transportation.10,11
Nearly all cervical cancer cases are caused by human papillomavirus (HPV) infections.12 HPV vaccination reduces the risk of infection from the most common HPV types that cause an estimated 70% 90% of cervical cancer cases.12,13 The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices recommends two doses of the HPV vaccine at least 6 months apart for females and males aged ≤14 years, and three doses for those who initiate the vaccine after age 15 years.14 Nationally, rates of HPV vaccination uptake remain quite low, and increase among females has slowed. Vaccine initiation rates increased from 20.7% in 2010 to 40.2% in 2014 among women aged 19–26 years, and from 53% in 2011 to 62.8% in 2015 among adolescent females aged 13–17 years.15-17 HPV vaccination rates are lower among foreign-born compared with U.S.-born women, even as cervical cancer rates are disproportionately high among these immigrants.11,15,18 A recent study of various routinely recommended adult vaccines in the U.S. revealed that foreign-born adults had lower vaccination coverage than U.S.-born adults, including HPV vaccination (14.7% vs 38.7%, respectively).11 Such evidence of HPV vaccination disparities is limited, and contains little detail on what characteristics are associated with HPV vaccination within different immigrant groups. Additionally, the available research has been limited by sample sizes too small to examine differences by world regions or countries of birth among foreign-born women.11,18
In order to decrease risk of HPV-related diseases in foreign-born women and children, it is important to improve access to primary prevention through HPV vaccination. Thus, there is a need to understand more about what characteristics contribute to HPV vaccination among different groups of foreign-born women, as these differences may lead to continued disparities in cervical cancer and other HPV-related diseases in the future. Further, a greater understanding of the barriers to vaccination can inform the efforts of healthcare providers to overcome barriers and better enable them to provide preventive care to their foreign-born patients. The purpose of this study is to examine factors associated with HPV vaccine uptake in U.S.-born and foreign-born women living in the U.S. who emigrated from different regions of the world.
METHODS
Study Sample
Data from the 2013–2015 National Health Interview Survey (NHIS) was analyzed in 2016. The NHIS is a nationally representative cross-sectional household surveillance of the U.S. civilian non-institutionalized population. A detailed description of the methods can be found elsewhere.19 Briefly, the NHIS uses a complex multistage clustered sample design to collect data through in-person interviews on different sociodemographic and health topics from household members using family, person, and sample adult modules. In order to improve the power of this study to detect differences in HPV vaccination among these groups, data from the NHIS 2013 to 2015 surveys were combined. The final response rate for each year was 61.2%, 58.9%, and 55.2%, respectively. Observed declines in the NHIS response rates over the years, because of nonresponse (e.g., refusal, noncontact, or other), has previously been documented.20 This study was exempted by the University of Texas Medical Branch’s IRB.
A total unweighted sample of 58,017 women participated in the NHIS survey between 2013 and 2015. This study included 17,027 of these women who were between the ages of 18 and 36 years, as they would have been eligible to have received the HPV vaccine at some point after it was licensed in the U.S. Women who did not respond to questions regarding their country of birth (n=9) and whether or not they initiated HPV vaccination (n=1,128) were excluded in the analysis. Thus, the final sample included 15,890 women.
Measures
HPV vaccine initiation was the outcome variable in this study. Participants were asked whether they had ever received an HPV vaccine, and their responses were dichotomized (yes or no). Participants were also asked how many doses of the HPV vaccine they had received. Responses were categorized as one, two, or three doses, as three doses were recommended by the Advisory Committee on Immunization Practices prior to 2016.21
The focal independent variable was foreign-born status. Participants were asked where they were born, and those who were not born in the U.S. or U.S. territory were categorized as foreign-born. Women born in the U.S. were categorized as U.S.-born. In order to evaluate a woman’s access to health care, participants were asked whether they had a usual source of health care, health insurance, whether they had visited an obstetrician/gynecologist (OB/GYN) in the past 12 months, and whether they had obtained a Pap smear/test (Pap test) in the past 12 months. Each variable was dichotomized, with 1=reported the behavior, and 0=did not report the behavior. Although Pap testing guidelines now recommend that young women between age 21 years and 30 years receive a Pap test every 3 years if their previous Pap test was negative for abnormalities, the 2013–2014 data only included whether women had received a Pap test in the past 12 months.22 As Pap test and OB/GYN visit were highly correlated, the variables were combined (OB/GYN visit/Pap test) and categorized as 3=Pap test and OB/GYN, 2=Pap test, 1=OB/GYN, and 0=none.
Additional covariates included self-rated health status, assessed by asking women how they would say their health is in general. Participants’ responses were categorized as excellent/very good, good, or fair/poor. Foreign-born women were asked which country they were born in, and their responses were categorized into geographic regions: U.S., Mexico/Central America/Caribbean Island, South America, Europe, Africa, Indian Subcontinent, Asia, Southeast Asia, and Other (including Russia and Middle East). Citizenship status was based on the question of whether foreign-born women were U.S. citizens. Their responses were dichotomized (yes or no). Total number of years lived in the U.S. was determined by asking foreign-born women how many years they lived in the U.S. Participants’ responses were dichotomized (<10 years or ≥10 years) based on cutoffs from previous literature.11 Sociodemographic characteristics included age, education, race/ethnicity (non-Hispanic white, Hispanic, non-Hispanic black, and Asian), household income (measure of federal poverty threshold), and U.S. region (Northeast, Midwest, South, and West).
Statistical Analysis
All analyses were conducted in SAS statistical software, version 9.4. Data were weighted to account for the complex sampling methods, by following directions for using these weights for pooling data from multiple NHIS survey years.19 Bivariable comparisons for all variables were made using chi-square test statistics to examine differences between foreign-born and U.S.-born women. The prevalence of HPV vaccine initiation by region of birth was graphed, with 95% CI indicated with error bars. Multivariable binary logistic regression was used to examine the association between foreign-born status and HPV vaccine initiation. Two models were used to examine whether this association may be attributable to healthcare access. The first model controlled for sociodemographic variables and overall self-rated health status. The second model controlled for health insurance status, usual source of care, and OB/GYN visit/Pap test in the past 12 months. Next, logistic regression analyses were stratified according to whether women were foreign-born or U.S.-born. These analyses were conducted because the interaction of foreign-born status and health insurance status was associated with HPV vaccination (p=0.04). Two models were developed for foreign-born women. The first model controlled for length of U.S. residency, and the second model added U.S. citizenship status.
RESULTS
The majority of study participants were U.S.-born. Among those who were foreign-born nearly half (49%) were from Mexico/Central America/Caribbean Island (Table 1). Almost 28% of all women had initiated HPV vaccination. HPV vaccine initiation was higher among U.S.-born than foreign-born women (30% vs 14%). HPV vaccine initiation was highest for women aged 18–26 years (49%), and this proportion was higher among foreign-born than U.S.-born women in the same age range (54% vs 48%). Only a small proportion of all women received all three HPV vaccinations (9%), and the rates were similar between the foreign-born and U.S.-born groups. In-depth examination of sociodemographics and covariates showed that foreign-born women had significantly lower (unadjusted) odds of HPV vaccination than U.S.-born women (Appendix Table 1).
Table 1.
Characteristics of Women by Birth Status, NHIS 2013–2015
| Variable | Total N=15,890 | U.S.-born (n=12,810) | Foreign-born N=3,080 | Chi-square |
|---|---|---|---|---|
| n (%) | % (95% CI) | % (95% CI) | ||
| Initiated HPV vaccine | <0.0001 | |||
| Yes | 3,868 (27.56) | 30.12 (28.82, 31.42) | 14.14 (12.42, 15.86) | |
| No | 11,132 (72.45) | 69.88 (68.58, 71.18) | 85.86 (84.14, 87.58) | |
| Age at HPV vaccine initiation | <0.0001 | |||
| 8–12 years | 219 (5.70) | 5.54 (4.49, 6.59) | 7.52 (4.16, 10.88) | |
| 13–17 years | 1,557 (41.95) | 42.93 (40.64, 45.22) | 30.91 (25.62, 36.21) | |
| 18–26 years | 1,926 (48.64) | 48.14 (45.62, 50.66) | 54.20 (48.92, 59.48) | |
| 27–35 years | 165 (3.71) | 3.39 (2.53, 4.24) | 7.36 (4.66, 10.07) | |
| Received all three HPV vaccinations | 0.0609 | |||
| Yes | 344 (8.77) | 8.82 (7.49, 10.16) | 8.12 (4.53, 11.71) | |
| No | 3,194 (83.34) | 83.62 (81.92, 85.32) | 80.28 (77.23, 84.18) | |
| Don’t know | 330 (7.89) | 7.56 (6.42, 8.70) | 11.60 (8.12, 15.08) | |
| Age | <0.0001 | |||
| 18–26 years | 6,289 (45.03) | 47.04 (45.59, 48.48) | 34.47 (32.35, 36.59) | |
| 27–30 years | 3,862 (25.03) | 24.60 (23.67, 25.54) | 27.24 (25.42, 29.06) | |
| 31–36 years | 4,849 (29.95) | 28.36 (27.28, 29.43) | 38.29 (36.06, 40.51) | |
| Education level | <0.0001 | |||
| No high school degree | 1,802 (10.30) | 7.93 (7.33, 8.54) | 22.79 (20.74, 24.84) | |
| High school degree | 3,118 (19.59) | 19.62 (18.62, 20.62) | 19.42 (17.60, 21.24) | |
| Some college | 3,853 (26.89) | 28.40 (26.99, 29.12) | 17.63 (15.63, 19.63) | |
| Associate/college degree or higher | 6,203 (43.42) | 44.04 (42.60, 45.48) | 40.16 (37.67, 42.66) | |
| Household income | <0.0001 | |||
| 0–100% FPL | 3,951 (24.79) | 23.69 (22.11, 25.26) | 30.60 (28.15, 33.06) | |
| <100% 200% FPL | 3,230 (20.34) | 19.81 (18.91, 20.72) | 23.09 (21.35, 24.83) | |
| <200% 300% FPL | 3,872 (26.45) | 27.13 (25.89, 28.36) | 22.89 (20.82, 24.95) | |
| >300% FPL | 3,175 (23.04) | 24.06 (22.78, 25.34) | 17.69 (15.85, 19.54) | |
| Race/Ethnicity | <0.0001 | |||
| Non-Hispanic white | 7,951 (59.81) | 67.93 (66.68, 69.18) | 17.10 (14.12, 19.38) | |
| Hispanic | 3,484 (17.92) | 11.84 (11.16, 12.51) | 49.87 (47.30, 52.44) | |
| Black | 2,526 (16.33) | 17.71 (16.65, 18.76) | 9.08 (7.80, 10.37) | |
| Asian | 1,039 (5.95) | 2.53 (2.20, 2.86) | 23.94 (21.67, 26.21) | |
| Marital status | <0.0001 | |||
| Married | 5,134 (33.41) | 30.37 (29.02, 31.72) | 49.37 (46.92, 51.83) | |
| Living with partner | 8,118 (55.18) | 57.87 (56.40, 59.33) | 41.06 (38.66, 43.47) | |
| Other (not married) | 1,728 (11.42) | 11.77 (10.98, 12.56) | 9.56 (8.19, 10.94) | |
| Region | <0.0001 | |||
| Northeast | 2,116 (14.98) | 14.52 (13.41, 15.62) | 17.39 (15.11, 19.67) | |
| Midwest | 3,058 (23.19) | 25.07 (23.47, 26.67) | 13.32 (10.93, 15.71) | |
| South | 5,683 (39.69) | 39.81 (38.01, 41.61) | 39.04 (36.10, 41.97) | |
| West | 4,143 (22.15) | 20.61 (19.16, 22.05) | 30.25 (27.65, 32.86) | |
| Region of birth | NA | |||
| U.S. | 12,143 (84.03) | 100 | 48.14 (45.60, 50.68) | |
| Mexico, Central America, Caribbean Island | 1,550 (7.69) | NA (NA) | 5.54 (4.66, 6.42) | |
| South America | 159 (0.89) | NA (NA) | 8.51 (6.86, 10.17) | |
| Europe | 171 (1.36) | NA (NA) | 5.77 (4.79, 6.74) | |
| Africa | 147 (0.92) | NA (NA) | 8.25 (6.89, 9.60) | |
| Indian subcontinent | 226 (1.32) | NA (NA) | 8.70 (7.30, 10.09) | |
| Asia | 238 (1.39) | NA (NA) | 7.12 (6.07, 8.17) | |
| Southeast Asia | 224 (1.14) | NA (NA) | 7.97 (6.40, 9.55) | |
| Other (includes Russia and Middle East) | 140 (1.27) | NA (NA) | 34.47 (32.35, 36.59) | |
| U.S. citizenship | NA | |||
| Yes | 13,131 (90.01) | 100 | 37.20 (34.85, 39.55) | |
| No | 1,853 (9.99) | NA (NA) | 62.80 (60.45, 65.15) | |
| Years in the U.S. | NA | |||
| <10 years | NA (NA) | 40.91 (38.80, 43.03) | ||
| ≥10 years | NA (NA) | 59.09 (56.97, 61.20) | ||
| Usual source of care | <0.0001 | |||
| No | 2,808 (187.53) | 16.78 (15.92, 17.63) | 27.77 (25.77, 29.78) | |
| Clinic/health center | 4,048 (23.58) | 21.93 (20.91, 22.96) | 32.20 (29.80, 34.60) | |
| Doctor’s office/HMO | 7,422 (53.33) | 56.74 (55.51, 57.97) | 35.39 (33.01, 37.77) | |
| Other | 719 (4.56) | 4.55 (4.10, 5.00) | 4.64 (3.71, 5.56) | |
| OB/GYN visit/Pap test in the past 12 months | <0.0001 | |||
| OB/GYN and Pap test | 6,500 (45.07) | 47.48 (46.22, 48.74) | 32.36 (30.48, 34.25) | |
| OB/GYN | 1,095 (7.36) | 7.09 (6.46, 7.71) | 8.77 (7.56, 9.98) | |
| Pap test | 2,144 (13.44) | 13.46 (12.69, 14.22) | 13.36 (11.90, 14.82) | |
| None | 5,193 (34.13) | 31.97 (30.88, 33.06) | 45.51 (43.33, 47.69) | |
| Health insurance | <0.0001 | |||
| Yes | 12,029 (82.62) | 85.81 (84.98, 86.64) | 65.87 (63.47, 68.26) | |
| No | 2,910 (17.38) | 14.19 (13.36, 15.02) | 34.13 (31.74, 36.53) | |
| Self-rated health status | <0.0001 | |||
| Excellent/Very good | 1,535 (72.19) | 72.39 (71.31, 73.46) | 71.16 (69.17, 73.14) | |
| Good | 3,441 (21.56) | 21.04 (20.03, 22.05) | 24.33 (22.40, 26.25) | |
| Fair/Poor | 1,021 (6.25) | 6.58 (6.08, 7.08) | 4.52 (3.71, 5.32) |
Note: Boldface indicates statistical significance (p<0.05). Values are unweighted sample sizes, and all percentages and 95% CI were weighted; Chi-square represents association between U.S.-born and foreign-born women by each of characteristics.
NA, not applicable; HPV, human papilloma virus; OB/GYN, obstetrics and gynecology visit; NHIS, National Health Interview Survey; FPL, federal poverty level
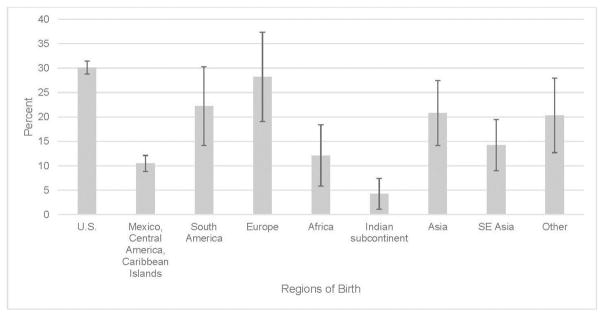
Among foreign-born women, there was significant heterogeneity in HPV vaccine initiation by region of birth, p<0.0001 (Figure 1). European (28.19%, 95% CI=19.02, 37.35) and South American women (22.24%, 95% CI=14.2, 30.29) had the highest vaccination rates among all foreign-born women. Women from the Indian subcontinent had the lowest HPV vaccination rate (4.28%, 95% CI=1.09, 7.46). Notably, the rate was 12.12% (95% CI=5.86, 18.38) among women who originated from Africa, 20.78% (95% CI=4.13, 27.43) among Asians, and 10.46% (95% CI=8.8, 12.12) among Hispanics from Mexico, Central American, and the Caribbean Islands.
Figure 1.
Percentage of HPV vaccine initiation by birth region among women (aged 18–36 years), NHIS 2013–2015.
HPV, human papillomavirus; NHIS, National Health Interview Survey
In order to evaluate the independent effects of health access variables on the association between foreign-born status and HPV vaccine initiation, two models were developed (Table 2). Model 1 included sociodemographic variables, self-rated health status, and foreign-born status. Foreign-born women had significantly lower odds of HPV vaccination compared with U.S. born women (OR=0.51, 95% CI=0.43, 0.62). This association was made slightly smaller in Model 2 when the health access variables were included in the model (OR=0.58, 95% CI=0.49, 0.70). Women with health insurance compared with those without were more likely to have been vaccinated (OR=1.54, 95% CI=1.31, 1.81). Women who had a usual source of care from clinic/health center, compared with those who did not have usual source of care, were more likely to report HPV vaccine initiation (OR=1.20, 95% CI=1.03, 1.41). Women who had an OB/GYN visit and Pap test in the past 12 months were more likely to have been vaccinated, compared with those who had none (OR=1.86, 95% CI=1.64, 2.11). Also, women who had either an OB/GYN visit (OR=1.71, 95% CI=1.39, 2.10) or Pap test (OR=1.53, 95% CI=1.29, 1.81) were more likely to have been vaccinated, compared with those who had none.
Table 2.
Logistic Regression of Factors Associated With HPV Vaccine Initiation Among Women, NHIS 2013–2015
| Variable | AOR (95% CI) | |
|---|---|---|
|
|
||
| Model 1 | Model 4 | |
| Foreign | ||
| No | ref | ref |
| Yes | 0.51 (0.43, 0.62)*** | 0.58 (0.49, 0.70)*** |
| Health insurance | ||
| No | ref | |
| Yes | 1.54 (1.31, 1.81)*** | |
| Usual source of care | ||
| No | ref | |
| Clinic/Health center | 1.20 (1.03, 1.41)* | |
| Doctor’s office/HMO | 1.12 (0.95, 1.31) | |
| Other | 1.43 (1.05, 1.96)* | |
| OB/GYN visit/Pap test in the past 12 months | ||
| None | ref | |
| OB/GYN and Pap test | 1.86 (1.64, 2.11)*** | |
| OB/GYN | 1.71 (1.39, 2.10)*** | |
| Pap test | 1.53 (1.29, 1.81)*** | |
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). Models adjusted for age, education, race/ethnicity, income level, marriage, region, self-rated health status, and OB/GYN visit/Pap test in the past 12 months.
HPV, human papilloma virus; NHIS, National Health Interview Survey; OB/GYN, obstetrics and gynecology visit
In the analyses stratified by foreign- or U.S.-born status, among foreign-born women Asians were significantly less likely to report HPV vaccination than whites (OR=0.59, 95% CI=0.37, 0.93; Table 3). Notably, among U.S.-born women race/ethnicity was not associated with HPV vaccine initiation. Foreign-born women who had lived in the U.S. for ≥10 years were more likely to report vaccine initiation compared with those who had lived in the U.S. <10 years (OR=1.55, 95% CI=1.14, 2.11 [Model 1]). However, this relationship lost statistical significance after controlling for U.S. citizenship status in the final model (Model 2). Foreign-born women who were U.S. citizens were significantly more likely to report HPV vaccine initiation than noncitizens (OR=1.60, 95% CI=1.16, 2.20).
Table 3.
Logistic Regression of Factors Associated HPV Vaccine Initiation Among Women by Foreign-born Status, NHIS 2013–2015
| Variable | U.S.-born AOR (95% CI) |
Foreign-born AOR (95% CI) |
|
|---|---|---|---|
|
|
|||
| Model 1 | Model 2 | ||
| Race/Ethnicity | |||
| Non-Hispanic white | ref | ref | ref |
| Hispanic | 0.96 (0.83, 1.12) | 1.08 (0.69, 1.71) | 1.11 (0.70, 1.76) |
| Black | 0.86 (0.74, 1.00) | 1.01 (0.59, 1.72) | 0.98 (0.58, 1.67) |
| Asian | 1.05 (0.81, 1.37) | 0.59 (0.37, 0.93)* | 0.62 (0.39, 0.98)* |
| Years lived in the U.S. | |||
| <10 years | ref | ref | |
| ≥10 years | 1.55 (1.14, 2.11)** | 1.26 (0.90, 1.76) | |
| U.S. citizenship | |||
| No | ref | ||
| Yes | 1.60 (1.16, 2.20)** | ||
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). Models adjusted for age, education, income level, marriage, region, self-rated health status, usual source of care and OB/GYN visit/Pap test in the past 12 months.
HPV, human papilloma virus; NHIS, National Health Interview Survey; OB/GYN, obstetrics and gynecology visit
DISCUSSION
Overall, data on a national sample of women aged 18–36 years revealed that foreign-born women were less than half as likely as U.S.-born women to have initiated HPV vaccination. Previous studies have found lower prevalence in uptake of other vaccines (e.g., tetanus, diphtheria, and cellular pertussis, hepatitis B, pneumococcal polysaccharide, and shingles) among foreign-born women compared with U.S.-born women.11,15,23 For example, Lu et al.11 found that vaccination prevalence was highest in the U.S. and Europe, and lower in certain regions like Asia and South America. The present study builds on such research by demonstrating that even after controlling for sociodemographic variables and other health indicators, foreign-born women had lower odds of HPV vaccine initiation. One likely explanation of the independent association between being foreign-born women and HPV vaccination is the context of healthcare access in their home countries. Most of these women are from countries where the majority of HPV related cancers occur, but access to preventive care, such as HPV vaccination, may be very limited.23 Thus, foreign-born women come to the U.S. with a higher risk of cervical cancer and with lower knowledge about preventive care that is available to mitigate their risks of developing this disease.
As expected, health insurance was associated with increased HPV vaccine initiation. This is consistent with other studies that observed a strong relationship between having health insurance and HPV vaccination.24,25 The present study also suggests that health insurance is an important determinant of healthcare access in the U.S., independent of native- or foreign-born status. Consequently, foreign-born women who have insurance are more likely to obtain important preventive services, such as vaccination.11 Previous studies on HPV vaccination among adolescents and adult women support the findings that health indicators including usual source of care, OB/GYN visit and Pap test in the past 12 months were significantly associated with HPV vaccine initiation.26,27 These findings suggest the importance of implementing public health programs aimed at providing preventive healthcare access, such as HPV vaccination, to immigrant populations. For example, the Vaccines for Children program that uses public funding to provide HPV vaccination for uninsured and underinsured children could be extended to young adults (aged 19–26 years) immigrating to the U.S.28 Provision of free or low-cost vaccination to eligible foreign-born women could also be an important step to preventing cervical cancer in this population, and a cheaper alternative to treating cancer in these women.
Besides challenges to healthcare access, it is likely that other factors may prevent foreign-born women from initiating HPV vaccination. For instance, previous studies have suggested that higher levels of acculturation among foreign-born women is associated with HPV vaccination.29 These women are more likely to assimilate to life in the U.S. with longer years of residence. This study shows that among foreign-born women, those who have lived in the U.S. for ≥10 years had higher odds of HPV vaccine initiation, which is consistent with previous studies.11,15 Unlike those studies, however, this study further revealed that the relationship between years lived in the U.S. and vaccination was not significant after adjusting for citizenship. This indicates that citizenship is crucial to long-term foreign-born residents of the U.S. in overcoming barriers to accessing preventive and healthcare services. It is possible that women who become citizens have the resources to overcome barriers that they may face in accessing health care, which include: socioeconomic, linguistic, cultural, and knowledge-related barriers.2,3
The present study contributes to research on unique differences in vaccination uptake by region of birth and racial/ethnic subgroups of foreign-born women. The previous research has been sparse, and limited by issues which include sample sizes that were too small to examine differences by place of birth. For example, one available estimate of HPV vaccination prevalence by region of birth using the 2012 NHIS data did not contain a large enough sample to examine places such as South America, Asia, and others.11 In this study, women from Europe and South America had the highest HPV vaccination prevalence among foreign-born women. Although it was not possible to examine HPV vaccination status of foreign-born women by country of birth because of the small sample size for some countries, this study demonstrated clear variations in HPV vaccination among foreign-born women depending on what continent they were born in.
Moreover, this study extended Lu et al.’s11 earlier examination of racial and ethnic differences in HPV vaccination among foreign-born individuals by further adjusting for factors associated with vaccination. Compared with non-Hispanic whites, Asian women had significantly lower odds of HPV vaccination. This finding is even more concerning as recent data shows that Asian women in the U.S. had the lowest rates of vaccine initiation (22.8%) compared with other race and ethnic groups.15 National level data monitoring preventive behaviors, such as HPV vaccination, should account for heterogeneity among foreign-born women, as this is important in determining which groups of foreign-born women are most vulnerable to negative health outcomes, and also in informing appropriate interventions to prevent cervical cancer.
Limitations
A strength of this study includes the use of a sample representative of the U.S. adult population, and containing a significant proportion of foreign-born individuals. However, there were a few limitations. First, the study was based on self-reported data, and thus responses provided by the women may be subject to recall bias. Second, given that data collection for the NHIS is based on a cross-sectional design, it impossible to draw causal inference from the findings. Next, the study did not distinguish between different types of health insurance, which may have enabled a more nuanced examination of its effect on vaccine uptake. Additionally, some respondents may have mistaken a pelvic exam for a Pap test. However, the Pap test was well described in the survey, and it is unlikely that this problem occurred at a high frequency. Examination of Pap test in the past 12 months does not follow current guidelines which are complicated, but generally recommends that women undergo a Pap test every 3 years.22 Women aged ≥30 years have the option of screening every 5 years after a negative Pap test and negative HPV DNA test.
CONCLUSIONS
This study provided evidence of an independent association between immigration status and HPV vaccination, as well as unique variation in HPV vaccination among different groups of foreign-born women. A more robust national level data monitoring of the HPV vaccination behavior, is needed to further improve understanding the process through which immigrant populations adapt to their new healthcare landscape—including changes to their sociocultural views, adaptation to the U.S. medical system, or general acculturation into American culture and healthcare viewpoints. Also, there is a need for targeted outreach across various immigrant communities to improve access to health care in general, and to develop population specific strategies to address the vaccination needs of different groups of foreign-born women.
Supplementary Material
Acknowledgments
Dr. Cofie was supported by an institutional training grant (National Research Service Award T32HD055163, Berenson, PI) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development at NIH. Dr. Guo is supported by a research career development award (K12HD052023: Building Interdisciplinary Research Careers in Women’s Health Program-BIRCWH; Berenson, PI) from the Office of Research on Women’s Health and National Institute of Child Health and Human Development at NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Trevelyan E, Gambino C, Gryn T, et al. The Characteristics of the U.S. Population by Generational Status: 2013. U.S. Government Printing Office; Washington, DC: 2016. [Google Scholar]
- 2.Derose KP, Escarce JJ, Lurie N. Immigrants and health care: sources of vulnerability. Health Aff (Millwood) 2007;26(5):1258–1268. doi: 10.1377/hlthaff.26.5.1258. https://doi.org/10.1377/hlthaff.26.5.1258. [DOI] [PubMed] [Google Scholar]
- 3.Derose KP, Bahney BW, Lurie N, Escarce JJ. Immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66(4):355–408. doi: 10.1177/1077558708330425. https://doi.org/10.1177/1077558708330425. [DOI] [PubMed] [Google Scholar]
- 4.Benard VB, Thomas CC, King J, et al. Vital signs: cervical cancer incidence, mortality, and screening—United States, 2007–2012. MMWR Morb Mortal Wkly Rep. 2014;63(44):1004–1009. [PMC free article] [PubMed] [Google Scholar]
- 5.SEER Cancer Statistics Review, 1975–2013. Bethesda, MD: National Cancer Institute; 2016. [Google Scholar]
- 6.Tsui J, Saraiya M, Thompson T, Dey A, Richardson L. Cervical cancer screening among foreign-born women by birthplace and duration in the United States. J Womens Health (Larchmt) 2007;16(10):1447–1457. doi: 10.1089/jwh.2006.0279. https://doi.org/10.1089/jwh.2006.0279. [DOI] [PubMed] [Google Scholar]
- 7.Schleicher E. Immigrant women and cervical cancer prevention in the United States. Baltimore, MD: Women’s and Children's Health Policy Center, Johns Hopkins Bloomberg School of Public Health; 2007. [Google Scholar]
- 8.Forman D, de Martel C, Lacey CJ, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30:F12–F23. doi: 10.1016/j.vaccine.2012.07.055. https://doi.org/10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- 9.Marshall KJ, Urrutia-Rojas X, Mas FS, Coggin C. Health status and access to health care of documented and undocumented immigrant Latino women. Health Care Women Int. 2005;26(10):916–936. doi: 10.1080/07399330500301846. https://doi.org/10.1080/07399330500301846. [DOI] [PubMed] [Google Scholar]
- 10.Barnack-Tavlaris JL, Garcini LM, Macera CA, Brodine S, Klonoff EA. Human Papillomavirus Vaccination Awareness and Acceptability Among U.S.-Born and U.S. Foreign-Born Women Living in California. Health Care Women Int. 2016;37(4):444–462. doi: 10.1080/07399332.2014.954702. https://doi.org/10.1080/07399332.2014.954702. [DOI] [PubMed] [Google Scholar]
- 11.Lu P-j, Rodriguez-Lainz A, O’Halloran A, Greby S, Williams WW. Adult Vaccination Disparities Among Foreign-Born Populations in the U.S., 2012. Am J Prev Med. 2014;47(6):722–733. doi: 10.1016/j.amepre.2014.08.009. https://doi.org/10.1016/j.amepre.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370(9590):890–907. doi: 10.1016/S0140-6736(07)61416-0. https://doi.org/10.1016/S0140-6736(07)61416-0. [DOI] [PubMed] [Google Scholar]
- 13.Joura EA, Giuliano AR, Iversen O-E, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. New Engl J Med. 2015;372(8):711–723. doi: 10.1056/NEJMoa1405044. https://doi.org/10.1056/NEJMoa1405044. [DOI] [PubMed] [Google Scholar]
- 14.CDC. CDC recommends only two HPV shots for younger adolescents. https://www.cdc.gov/media/releases/2016/p1020-hpv-shots.html. Published 2016.
- 15.Williams WW, Lu PJ, O’Halloran A, et al. Surveillance of Vaccination Coverage Among Adult Populations - United States, 2014. MMWR Surveill Summ. 2016;65(1):1–36. doi: 10.15585/mmwr.ss6501a1. https://doi.org/10.15585/mmwr.ss6501a1. [DOI] [PubMed] [Google Scholar]
- 16.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(33):850–858. doi: 10.15585/mmwr.mm6533a4. https://doi.org/10.15585/mmwr.mm6533a4. [DOI] [PubMed] [Google Scholar]
- 17.CDC. National and state vaccination coverage among adolescents aged 13–17 years United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(34):671–677. [PubMed] [Google Scholar]
- 18.Lu PJ, O’Halloran A, Williams WW, Lindley MC, Farrall S, Bridges CB. Racial and ethnic disparities in vaccination coverage among adult populations in the U.S. Vaccine. 2015;33(Suppl 4):D83–91. doi: 10.1016/j.vaccine.2015.09.031. https://doi.org/10.1016/j.vaccine.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 19.CDC National Center for Health Statistics. National Health Interview Survey (NHIS): Questionnaires, datasets, and related documentation 2013–2015. [Google Scholar]
- 20.Czajka JL, Beyler A. Declining Response Rates in Federal Surveys: Trends and Implications (Background Paper) Washington, DC: Mathematica Policy Research; 2016. [Google Scholar]
- 21.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56(RR-2):1–24. [PubMed] [Google Scholar]
- 22.Moyer VA. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;156(12):880–891. doi: 10.7326/0003-4819-156-12-201206190-00424. https://doi.org/10.7326/0003-4819-156-12-201206190-00424. [DOI] [PubMed] [Google Scholar]
- 23.Dallo FJ, Kindratt TB. Disparities in vaccinations and cancer screening among U.S.- and foreign-born Arab and European American non-Hispanic White women. Womens Health Issues. 2015;25(1):56–62. doi: 10.1016/j.whi.2014.10.002. https://doi.org/10.1016/j.whi.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Laz TH, Rahman M, Berenson AB. Human papillomavirus vaccine uptake among 9–17 year old males in the United States: the National Health Interview Survey, 2010. Hum Vaccin Immunother. 2013;9(4):874–878. doi: 10.4161/hv.23190. https://doi.org/10.4161/hv.23190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt S, Parsons HM. Vaccination interest and trends in human papillomavirus vaccine uptake in young adult women aged 18 to 26 years in the United States: an analysis using the 2008–2012 National Health Interview Survey. Am J Public Health. 2014;104(5):946–953. doi: 10.2105/AJPH.2013.301828. https://doi.org/10.2105/AJPH.2013.301828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sauer AG, Jemal A, Simard EP, Fedewa SA. Differential uptake of recent Papanicolaou testing by HPV vaccination status among young women in the United States, 2008–2013. Cancer Epidemiol. 2015;39(4):650–655. doi: 10.1016/j.canep.2015.05.002. https://doi.org/10.1016/j.canep.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Tiro JA, Tsui J, Bauer HM, Yamada E, Kobrin S, Breen N. Human papillomavirus vaccine use among adolescent girls and young adult women: an analysis of the 2007 California Health Interview Survey. J Womens Health (Larchmt) 2012;21(6):656–665. doi: 10.1089/jwh.2011.3284. https://doi.org/10.1089/jwh.2011.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Advisory Committee on Immunization Practices. [Accessed July 24, 2017];Vaccines for Children Program - vaccines to prevent human papillomavirus. www.cdc.gov/vaccines/programs/vfc/downloads/resolutions/2016-10-2-hpv.pdf.
- 29.Gerend MA, Zapata C, Reyes E. Predictors of human papillomavirus vaccination among daughters of low-income Latina mothers: the role of acculturation. J Adolesc Health. 2013;53(5):623–629. doi: 10.1016/j.jadohealth.2013.06.006. https://doi.org/10.1016/j.jadohealth.2013.06.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.