Abstract
Introduction
This study examined whether increasing availability of mental health services at school-based health centers in Oregon public schools would be associated with a decrease in the likelihood of depressive episodes and suicide risk among adolescents.
Methods
The study included 168 Oregon public schools that participated in the Oregon Healthy Teens Survey in 2013 and 2015. Twenty-five schools had a school-based health center, and 14 of those schools increased the availability of mental health services from 2013 to 2015. The Oregon Healthy Teens Survey included questions about having a depressive episode, suicidal ideation, and attempting suicide in the past year. Multilevel logistic regression analyses were conducted in 2017 to examine associations between increasing mental health services and the likelihood of past year depressive episodes, suicidal ideation, and suicide attempts. Analyses also compared student subgroups defined by demographic characteristics (e.g., gender).
Results
Students at school-based health center schools that increased availability of mental health services were less likely to report depressive episodes (OR=0.88, p<0.01), suicidal ideation (OR=0.84, p<0.01), and suicide attempts (OR=0.82, p<0.01) from 2013 to 2015 compared with all other schools. Significant risk reductions in past year depressive episodes and suicidal ideation were also observed in school-based health center schools that increased availability of mental health services relative to other schools with school-based health centers. No significant differences were observed for student demographic subgroups.
Conclusions
This study suggests that increasing availability of school-based mental health services can help to reduce depressive episodes and suicide risk among adolescents.
INTRODUCTION
Depressive episodes and suicidal thoughts are prevalent among adolescents in the U.S., especially females. The National Survey on Drug Use and Health indicates that from 2005 to 2014, the prevalence of major depressive episodes in the past year increased from 13.1% to 17.3% among adolescent girls, and from 4.5% to 5.7% among boys.1 The Youth Risk Behavior Survey indicates that from 2005 to 2015, the prevalence of past year suicidal ideation increased among girls from 21.8% to 23.4%, but did not change among boys (12.2%).2,3 Higher rates of depression and suicidal ideation among adolescent girls may be attributable to hormonal changes during puberty prior to menstruation, and internalizing symptoms.4
To identify and help adolescents who are at risk for depression and suicide, a growing number of schools offer mental health services through school-based health centers (SBHCs). SBHCs provide comprehensive, convenient healthcare services for school children and adolescents in all 50 states and the District of Columbia.5 From 1999 to 2017, the number of SBHCs increased from approximately 1,000 to 3,178 as part of a national effort to provide cost-effective healthcare services for youth who may lack access to affordable health care.5 The Affordable Care Act included a $200 million appropriation to improve delivery and expansion of SBHC services from 2010 to 2013.6 SBHCs typically have primary care and behavioral health providers and offer preventive and treatment services including immunizations and oral and vision screenings. Many SBHCs also provide reproductive, substance use, and mental health services.
However, research on the effectiveness of mental health services provided by SBHCs is very limited, as indicated by systematic reviews of studies on SBHCs.7–9 The majority of studies to date have focused on utilization of SBHCs, and have found consistently higher levels of use among girls for reproductive and mental health services.10–14 These studies support the premise that SBHCs can improve access to and utilization of mental health services needed by students, but leave questions about whether SBHCs contribute to improved mental health outcomes among students.
A prospective study of 109 students in six Ohio school districts with Medicaid medical records from 1997 to 2003 found greater increases in mental health service utilization among students at schools with SBHCs compared with students at non-SBHC schools.15 The study also found lower mental health care costs among students who utilized SBHC services than students who did not. There was also evidence of greater improvement in psychosocial health-related quality of life among students who utilized SBHC mental health services compared with students at non-SBHC schools. Although these results provide support for the effectiveness of SBHC mental health services, the study was limited by its reliance on Medicaid records for a cohort of students who represented only a small fraction of more than 9,000 students who were enrolled in the six school districts.
A study of more than 300 students in 12 California schools with SBHCs found significant improvements in mental health outcomes based on assessments conducted by mental health service providers.13 Students participated in at least three mental health visits and were asked about their level or anxiety or nervousness, depression or sadness, eating disorders, grief, loss or bereavement, self-injury, substance abuse, and suicidal ideation. Over a period of at least 3 months, students reported significant improvement for all of these mental health indicators.
Students also reported improvements for a number of resiliency indicators, including school attendance and commitment, expressing feelings and emotions, expressing a sense of hope for the future, and involvement in recreational or vocational activities. Although providing further evidence for the effectiveness of SBHC mental health services, this study was limited by absence of a comparison group. Thus, the observed improvements in mental health outcomes may have occurred regardless of students’ exposure to mental health services.
These studies point to the need for additional research on the effectiveness of mental health services provided by SBHCs. This study compares public schools with SBHCs in Oregon that received additional funding for mental health services from 2013 to 2015 with other public schools that did not increase availability of mental health services, including other public schools with SBHCs. In 2013, the Oregon State Legislature appropriated funds to the Oregon Health Authority to increase mental health services in schools; $3.6 million was allocated to SBHCs, mainly to increase availability of mental health providers. Depending on the demonstrated need of the SBHC (e.g., no mental health provider, >50% of students eligible for free/reduced price lunch), grant dollars supported between 0.2 and 1.0 full-time employee (FTE) per site.
Using annual survey data from statewide samples of students, this study examines effects of the increase in availability of SBHC mental health services on the prevalence of depressive episodes and suicidal ideation and attempts. Study hypotheses are that: (1) schools with an increase in availability of SBHC mental health services would show improvement in these outcomes relative to other schools, and (2) females would benefit from the increase in availability of SBHC mental health services more so than males as they would be more likely than males to experience depressive episodes and utilize such services. This study also examines possible socioeconomic, ethnic, and racial differences in the effects of increased mental health services, as SBHCs are intended to improve access to health care among disadvantaged youth and youth of color.
METHODS
Study Sample
This study is based on 168 public schools in Oregon that participated in the Oregon Healthy Teens (OHT) Survey in both 2013 and 2015. Twenty-five of the 168 schools had SBHCs (16 high schools, five middle/high schools, four middle schools), and 14 of the schools with SBHCs (seven high schools, three middle/high schools, four middle schools) increased availability of mental health services between 2013 and 2015. Across the 14 SBHCs, there was an increase of 11.0 mental health provider FTEs (mean=0.8 FTE per SBHC). Available services included short- and long-term mental health therapy; several schools also hired behavioral health consultants to assist students with behavioral problems. This study compares changes in prevalence rates of having a depressive episode, suicidal ideation, and attempting suicide in the past year among students at schools with SBHCs that increased availability of mental health services after 2013 with all other schools in the sample, and with other schools with SBHCs that did not increase availability of mental health services after 2013. Prevalence rates of past year depressive episodes, suicidal ideation and suicide attempts in 2013 and 2015 are based on repeated cross-sectional samples of students.
Survey data for eighth and 11th grade students were obtained from the statewide OHT survey, which was administered prior to increases in availability of SBHC mental health services in 2013, and again in 2015.16 The OHT is an anonymous, voluntary self-administered survey of eighth and 11th graders modeled after the Youth Risk Behavior Survey. The OHT is conducted during the spring semester from February through May and is available either online or via paper and pencil, at the discretion of the school district. Students do not submit any personal information with their survey responses. The OHT survey is designed to be completed in a single class period.
The OHT sampling frame is based on the Youth Risk Behavior Survey, and comprises public middle and high schools sampled within each county. The sample is intended to be representative of eighth and 11th graders in each county and the state. Post-hoc sample weights were developed for each county and the state based on the actual number of eighth and 11th graders in each school, county, and the entire state.16
Measures
Students were asked: During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities? Students who responded yes to this question were classified as having a depressive episode in the past year. Students were also asked: During the past 12 months, did you ever seriously consider attempting suicide? And: During the past 12 months, how many times did you actually attempt suicide? Dichotomous variables were created to represent any suicidal ideation and any suicide attempts in the past year.
Students reported their grade, age, gender, ethnicity, race, and whether they were receiving free or reduced price lunch at school. Hispanic ethnicity and race (non-Hispanic white, African American, Asian, Native American, Pacific Islander) were treated as dichotomous variables. Survey year was also a student-level variable.
School characteristics included having an SBHC, increasing availability of SBHC mental health services after 2013, school type (middle, middle/high school, high school), total school enrollment, the percentage of students who were non-Hispanic and non-white, and the percentage of students receiving free or reduced price meals. These data were obtained from the Oregon Health Authority, Public Health Division, Adolescent and School Health Program.
Statistical Analysis
Data analyses were conducted in 2017. Descriptive statistics were examined for the study sample, and characteristics of schools with and without SBHC services were compared. Multilevel logistic regression analyses were then conducted to test study hypotheses. Models were based on student (level 1) and school (level 2) variables. Initial regression models included cross-level interaction terms (e.g., increase in availability of SBHC mental health services at school level X year at student level) to compare the likelihood of depressive episodes, suicidal ideation, and suicide attempts from 2013 to 2015 among students at schools with SBHCs that increased availability of mental health services relative to all other schools and other schools with SBHCs. Analyses then examined possible moderating effects of gender, grade level, ethnicity, race, and free/reduced price lunch status by including a three-way interaction term in the regression model (e.g., increase in availability of SBHC mental health services X year X gender). All analyses were conducted with HLM, version 7.01 software to adjust for variance attributable to observations nested within schools.17
RESULTS
School and enrolled student characteristics are provided in Table 1, along with comparisons of schools with SBHCs that did and did not increase availability of mental health services after 2013, and schools without SBHCs. Although schools with SBHCs had a larger number of students, on average, than non-SBHC schools, those differences were not statistically significant. SBHC and non-SBHC schools were also similar with respect to the overall percentage of students eligible for free or reduced price meals and percentage of students who were non-Hispanic and non-white. Among SBHC schools, a significantly higher percentage of schools that increased availability of mental health services after 2013 were middle schools.
Table 1.
School and Baseline Student Characteristics by SBHC Mental Health Services Status, Mean (SD) or Percenta
| Variable | Total sample | Non-SBHC schools | SBHC schools (n=25)
|
|
|---|---|---|---|---|
| No change in mental health services | Increase in mental health services | |||
| School level | N=168 | n=143 | n=11 | n=14 |
| Middle school (%) | 42.3 | 46.9 | 0.0b | 28.6c |
| Middle/high school (%) | 14.3 | 13.3 | 18.2 | 21.4 |
| High school (%) | 43.4 | 39.9 | 81.8b | 50.0 |
| Student enrollment | 704.6 (549.2) |
672.3 (502.6) |
961.8 (607.3) | 831.9 (864.0) |
| Percent eligible for free/reduced price meals | 55.5 (17.9) | 55.3 (18.3) | 54.9 (14.8) | 58.6 (16.8) |
| Percent non-Hispanic, non-white | 33.9 (18.5) | 34.4 (18.8) | 37.2 (10.0) | 26.5 (19.3) |
| Student level | N=17,307 | n=14,856 | n=1,230 | n=1,221 |
| 8th grade (%) | 47.7 | 53.5 | 3.7 | 20.6 |
| 11th grade (%) | 52.3 | 46.5 | 96.3b | 79.4b,c |
| Age | 15.2 (1.6) | 15.0 (1.6) | 16.4 (0.8)b | 15.9 (1.4)c |
| Female (%) | 51.6 | 51.6 | 51.5 | 51.4 |
| Hispanic | 22.4 | 23.2 | 18.6 | 15.8b |
| Non-Hispanic white | 74.4 | 74.2 | 77.4 | 73.7 |
| Received free/reduce price lunch (%) | 39.4 | 39.1 | 33.6 | 50.6 |
| Depressive episode, past year (%) | 25.2 | 25.1 | 24.3 | 26.8 |
| Suicidal ideation, past year (%) | 15.2 | 15.2 | 13.9 | 15.8 |
| Suicide attempt, past year (%) | 6.2 | 6.2 | 5.7 | 6.4 |
Student sample sizes are unweighted, while descriptive statistics for study variables were obtained with sample weights.
Significantly different from schools without an SBHC (p<0.05)
Significantly different from schools with SBHCs that did not increase mental health services (p<0.05).
SBHC, school-based health center.
At the student level, a significantly higher percentage of students at SBHC schools were 11th graders and had a higher mean age than non-SBHC schools. SBHC and non-SBHC schools were similar with respect to the percentage of students who were female. However, SBHC schools that increased availability of mental health services had a lower percentage of students of Hispanic ethnicity, and a somewhat higher percentage of students who received free or reduced price lunch compared with non-SBHC schools and other schools with SBHCs. The baseline prevalence of depressive episodes, suicidal ideation, and suicide attempts in the past year was similar across the subgroups of schools.
Results of multilevel logistic regression analyses for the total sample of schools are provided in Table 2. At the student level, age was positively associated with the likelihood of past year depressive episodes and suicidal ideation. Females and students who received free or reduced price lunch were also significantly more likely to report past year depressive episodes, suicidal ideation, and suicide attempts than males and students who didn’t receive free or reduced price lunch, respectively. At the school level, there was a greater likelihood of suicidal ideation at middle and middle/high schools relative to high schools, and a greater likelihood of suicidal attempts at middle schools relative to high schools. The cross-level interaction terms indicate a significant relative reduction in the likelihood of past year depressive episodes, suicidal ideation, and suicide attempts from 2013 to 2015 among students at SBHC schools that increased availability of mental health services during this period compared with other schools. Figure 1A indicates a 15% lower relative increase in the prevalence of past year depressive episodes among students at SBHC schools that increased availability of mental health services compared with students at schools that did not increase availability of mental health services. Figures 1B and 1C show relative decreases in the prevalence of past year suicidal ideation (26%) and suicide attempts (32%) among students at SBHC schools that increased availability of mental health services compared with students at schools that did not increase availability of mental health services. There were no significant moderating effects of students’ gender, grade level, ethnicity, race, or free/reduced price lunch status.
Table 2.
Associations Between Increasing MH Services and the Likelihood of Past-year Depressive Episodes, Suicidal Ideation, and Suicide Attempts From 2013 to 2015
| Variable | Depressive episode | Suicidal ideation | Suicide attempt |
|---|---|---|---|
| Student level | |||
| Age | 1.09 (1.02, 1.16)** | 1.08 (1.01, 1.17)* | 1.08 (0.96, 1.22) |
| Female | 2.50 (2.32, 2.70)** | 2.24 (2.03, 2.47)** | 2.52 (2.18, 2.90)** |
| Hispanic | 1.14 (1.04, 1.25)** | 0.98 (0.86, 1.19) | 1.18 (1.01, 1.39)* |
| Non-Hispanic white | 1.07 (0.98, 1.17) | 1.12 (0.98, 1.28) | 1.04 (0.87, 1.24) |
| Receive free/reduced price lunch | 1.38 (1.27, 1.49)** | 1.29 (1.18, 1.40)** | 1.38 (1.22, 1.55)** |
| Year | 1.05 (1.02, 1.09)** | 1.04 (1.01, 1.08)* | 1.06 (1.01, 1.11)* |
| School level | |||
| Middle schoola | 1.09 (0.87, 1.39) | 1.35 (1.02, 1.78)* | 1.82 (1.23, 2.71)** |
| Middle/high schoola | 1.08 (0.93, 1.25) | 1.30 (1.05, 1.62)* | 1.27 (0.97, 1.64) |
| Student enrollment | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| Percent eligible for free/reduced price meals | 1.00 (1.00, 1.01)** | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| Percent non-Hispanic, non-white | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) |
| Increase in MH services | 0.95 (0.84, 1.09) | 0.89 (0.78, 1.03) | 0.95 (0.79, 1.14) |
| Cross-level | |||
| Increase in MH services × year | 0.88 (0.81, 0.97)** | 0.84 (0.74, 0.95)** | 0.82 (0.70, 0.96)** |
Notes: Data presented as OR (95% CI). Boldface indicates statistical significance
p<0.05,
p<0.01
High schools are the referent group.
MH, mental health
Figure 1.
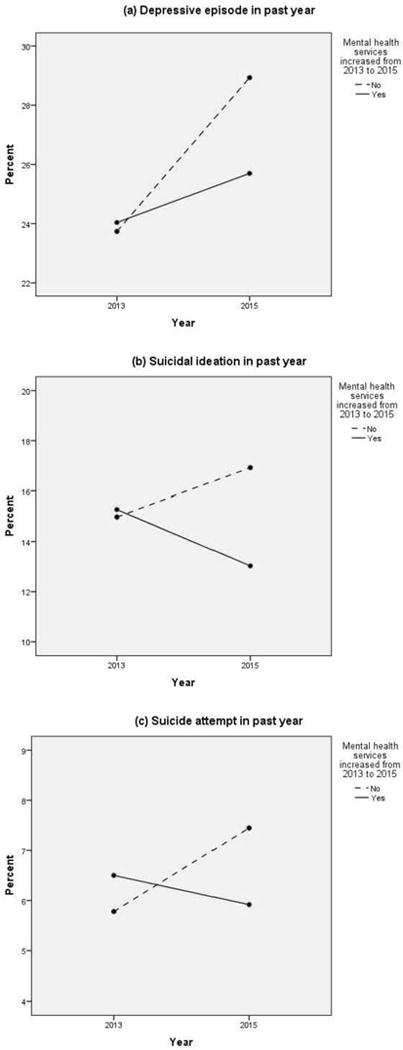
For the total sample of schools, change in the prevalence of past-year (A) depressive episodes, (B) suicidal ideation, and (C) suicide attempts, by increase in availability of mental health services at SBHC schools from 2013 to 2015. Prevalence rates are adjusted for school and student demographic characteristics.
SBHC, school-based health centers
Within the subsample of SBHC schools, similar relative reductions in past year depressive episodes (OR=0.82, 95% CI=0.72, 0.93, p<0.01) and suicidal ideation (OR=0.81, 95% CI=0.69, 0.94, p<0.01) were observed from 2013 to 2015 for SBHC schools that increased availability of mental health services compared with other SBHC schools. These results are illustrated in Figures 2A and 2B, showing lower relative increases in the prevalence of past year depressive episodes (38%) and suicidal ideation (33%), respectively, among students at SBHC schools that increased availability of mental health services. There was no significant difference in the likelihood of suicide attempts from 2013 to 2015 among students at SBHC schools that increased availability of mental health services relative to other SBHC schools (OR=0.92, 95% CI=0.73, 1.17, NS). There were also no significant moderating effects of gender, grade level, ethnicity, race or free/reduced price lunch status. As in analyses with the total sample of schools, there was a greater likelihood of past year depressive episodes, suicidal ideation and suicide attempts among females and among students who received free/reduced price lunch.
Figure 2.
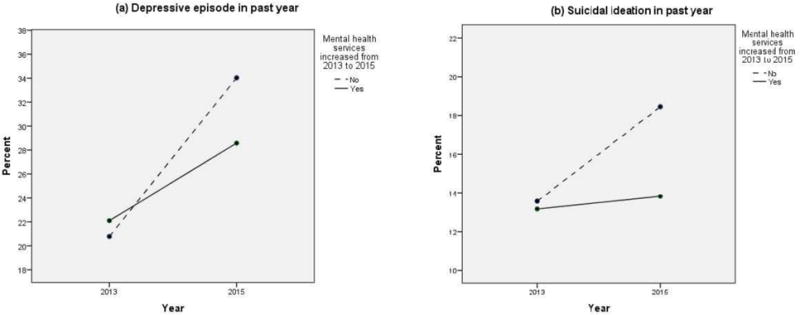
For the subgroup of schools with SBHCs, change in the prevalence of past-year (A) depressive episodes and (B) suicidal ideation by increase in availability of mental health services from 2013 to 2015. Prevalence rates are adjusted for school and student demographic characteristics.
SBHC, school-based health centers
DISCUSSION
The need for accessible and effective services to prevent or reduce emotional health problems among adolescents has been emphasized by the U.S. Surgeon General and WHO.18,19 The growth of SBHCs is one example of how communities across the U.S. are attempting to address this need. However, very few studies have investigated whether mental health services provided by SBHCs have a beneficial effect on adolescents’ emotional well-being.7–9 In general, prior studies of SBHC effects on mental health and health-related behaviors have been methodologically limited by cross-sectional designs, small sample sizes, and comparisons of only SBHC and non-SBHC schools.7–9,20 The current study advances prior research by using a school-level longitudinal design with a large sample of public schools to examine associations between an increase in availability of mental health services at schools with SBHCs and the prevalence of depressive episodes, suicidal ideation, and suicide attempts among adolescents in Oregon.
Findings of this study suggest that the increase in availability of mental health services provided by 14 Oregon public schools with SBHCs from 2013 to 2015 was associated with significant reductions in the likelihood of depressive episodes and suicide risk among adolescents. However, contrary to expectations, there were no differences in the associations between increasing availability of mental health services and mental health indicators among student demographic subgroups. This is especially surprising for gender, given the greater utilization of SBHC mental health services by females.10–14 The 2015 OHT Survey also indicated that a larger percentage of females reported using the SBHC at their school at least once in the past year compared with males. These findings suggest that the increase in availability of mental health services was beneficial for males and females, and students in other demographic subgroups, including those who were socioeconomically disadvantaged.
SBHCs can play a critical role in addressing the apparent increase in major depressive episodes among adolescents in the U.S. by supporting youth in need of mental health services. Further research is needed to (1) identify effective strategies to reach at-risk adolescents who otherwise may not seek mental health services at schools with SBHCs, (2) examine the range of mental health services provided across SBHCs, and (3) ascertain what services or constellation of services are particularly effective in achieving positive mental health outcomes. Additional research is also needed to determine how those services could be improved.
Limitations
Although this study advances prior research on SBHC mental health services, findings should be considered in light of several limitations. The subsample schools with SBHCs may not be representative of all schools with SBHCs in Oregon. It is possible that the observed relationships between increased availability of SBHC mental health services and past year depressive episodes and suicide risk were attributable to some other unmeasured differences between the Oregon schools. However, analyses with the subgroup of SBHC schools helped to address concern about possible school selection effects. The study also could not account for any other changes in availability of mental health services in schools or communities that may have impacted student mental health. Survey measures for past year depressive episodes, suicidal ideation, and suicide attempts may have been subject to social desirability and recall bias as students may have underreported these mental health indicators because of stigma or inaccurate memory. The single-item measures for past year depressive episodes, suicidal ideation, and suicide attempts are intended for population-based epidemiologic surveys and do not meet standards for clinical diagnosis. Finally, some of the analyses may have been underpowered because of the number of schools and students in subgroups being compared.
CONCLUSIONS
This study suggests that increasing availability of SBHC mental health services may have a beneficial effect on the emotional health of adolescents. Natural experimental studies with longitudinal designs in other populations are needed, however, to determine whether these findings can be replicated. Existing data from school-based surveys in other states should be useful for that purpose.
Acknowledgments
This study was supported by grants from the National Institute on Child Health and Human Development (NICHD Grant No. R01 HD073386) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA Grant No. R01 AA021726). The content is solely the responsibility of the authors and does not necessarily represent the official views of NICHD, NIAAA, or NIH. Dr. Paschall was responsible for conceptualizing and writing the manuscript, and data analysis. Dr. Bersamin shared responsibility for conceptualizing and writing the manuscript. All study procedures involving human subjects were in accordance with the ethical standards of the IRB of the Pacific Institute for Research and Evaluation. We would like to thank Dr. Sarah Knipper of the Oregon Health Authority, Public Health Division, Adolescent and School Health Program for her assistance in providing information regarding school-based health centers mental health services and for providing comments on earlier drafts of this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare that they have no financial conflict of interest.
References
- 1.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. doi: 10.1542/peds.2016-1878. https://doi.org/10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance – United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(SS-6):1–178. doi: 10.15585/mmwr.ss6506a1. https://doi.org/10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 3.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance – United States, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(SS-5):1–108. https://doi.org/10.1111/j.1746-1561.2006.00127.x. [PubMed] [Google Scholar]
- 4.Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. 2015;40(4):219–221. doi: 10.1503/jpn.150205. https://doi.org/10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.School-Based Health Alliance. 2013–14 Digital census report on school-based health centers. http://censusreport.sbh4all.org Accessed March 6, 2017.
- 6.National Conference of State Legislatures. States implement health reform: School-based health centers. National Conference of State Legislatures; 2011. www.ncsl.org/portals/1/documents/health/HRSBHC.pdf Accessed on May 29, 2017. [Google Scholar]
- 7.Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–156. doi: 10.1016/j.cppeds.2012.03.002. https://doi.org/10.1016/j.cppeds.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bains RM, Diallo AF. Mental health services in school-based health centers: Systematic review. J Sch Nurs. 2016;32(1):8–19. doi: 10.1177/1059840515590607. https://doi.org/10.1177/1059840515590607. [DOI] [PubMed] [Google Scholar]
- 9.Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. doi: 10.1186/2046-4053-1-49. https://doi.org/10.1186/2046-4053-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juszczak L, Melinkovich P, Kaplan D. Use of health and mental health services by adolescents across multiple delivery sites. J Adolesc Health. 2003;32(6):108–118. doi: 10.1016/s1054-139x(03)00073-9. https://doi.org/10.1016/S1054-139X(03)00073-9. [DOI] [PubMed] [Google Scholar]
- 11.Langille D, Asbridge M, Kisely S, et al. The relationship of sex and risk behaviours to students’ use of school-based health centres in Cape Breton, Nova Scotia. Pediatr Child Health. 2008;13(7):605–609. doi: 10.1093/pch/13.7.605. https://doi.org/10.1093/pch/13.7.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pastore DR, Techow B. Adolescent school-based health care: A description of two sites in their 20th year of service. Mt Sinai J Med. 2004;71(3):191–196. [PubMed] [Google Scholar]
- 13.Soleimanpour S, Geierstanger SP, Kaller S, McCarter V, Brindis CD. The role of school health centers in health care access and client outcomes. Am J Public Health. 2010;100(9):1597–1603. doi: 10.2105/AJPH.2009.186833. https://doi.org/10.2105/AJPH.2009.186833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szumilas M, Kutcher S, LeBlanc JC, Langille DB. Use of school-based health centres for mental health support in Cape Breton, Nova Scotia. Can J Psychiatry. 2010;55(5):319–328. doi: 10.1177/070674371005500508. https://doi.org/10.1177/070674371005500508. [DOI] [PubMed] [Google Scholar]
- 15.Guo JJ, Wade TJ, Keller KN. Impact of school-based health centers on students with mental health problems. Public Health Rep. 2008;123(6):768–780. doi: 10.1177/003335490812300613. https://doi.org/10.1177/003335490812300613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oregon Health Authority, Public Health Division. Oregon Health Teens Survey. https://public.health.oregon.gov/BirthDeathCertificates/Surveys/OregonHealthyTeens/Pages/index.aspx Accessed on March 6, 2017. Documentation for Oregon Healthy Teens survey methodology was also provided by the Oregon Health Authority.
- 17.Raudenbush S, Bryk A, Cheong YF, Congdon R, du Toit M. HLM 7: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, IL: Scientific Software International; 2011. [Google Scholar]
- 18.Murthy VH. Surgeon General’s perspectives: Improving the physical and mental health of adolescents to ensure success in adulthood. Public Health Rep. 2015;130(3):193–195. doi: 10.1177/003335491513000303. https://doi.org/10.1177/003335491513000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO. Health for the world’s adolescents: A second chance for the second decade. http://apps.who.int/adolescent/second-decade. Accessed March 6, 2017.
- 20.Bersamin M, Garbers S, Gold MA, et al. Measuring success: Evaluation designs and approaches to assessing the impact of school-based health centers. J Adolesc Health. 2016;58(1):3–10. doi: 10.1016/j.jadohealth.2015.09.018. https://doi.org/10.1016/j.jadohealth.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]


