Dear Editor,
A complete blood count (CBC) is one of the most frequently requested diagnostic tests in medical laboratories. This test is indicated, among others, for febrile patients who may be infected with malaria [1]. Currently available automated hematology analyzers are not designed to detect malaria-related signals. The incorporation of a ‘malaria flag’ into modern analyzers would allow for the development of an automated and adjuvant diagnostic tool for febrile patients who may have malaria, especially for patients with low pre-test expectation of the disease in non-endemic regions.
Regarding the unexpected detection of malaria during CBC analysis, we describe the case of a 21-year-old male who visited the Daejeon St. Mary's Hospital (Daejeon, Korea) with a persistent fever lasting 10 days and a pain in the left flank for two days at the time of diagnosis. The patient provided written informed consent for clinical analyses, and the study protocol was approved by the Institutional Review Board of the Catholic University of Korea. Physical examination revealed tertian fever of up to 40℃ with chills and rigors, a pulse rate of 90 bpm, and a blood pressure of 110/60 mmHg. The laboratory findings were as follows: white blood cell count, 4.1×109/L; hemoglobin, 125 g/L; platelet count, 53×109/L; high-sensitivity C-reactive protein, 178.2 mg/L; AST, 67 IU/L; ALT, 49 IU/L; lactate dehydrogenase, 884 IU/L; and creatine phosphokinase, 812 IU/L. Antigen and antibody tests for hepatitis B, C, and human immunodeficiency virus were negative. No pathogenic bacteria were identified in routine bacterial culture in blood, stool, and random urine samples.
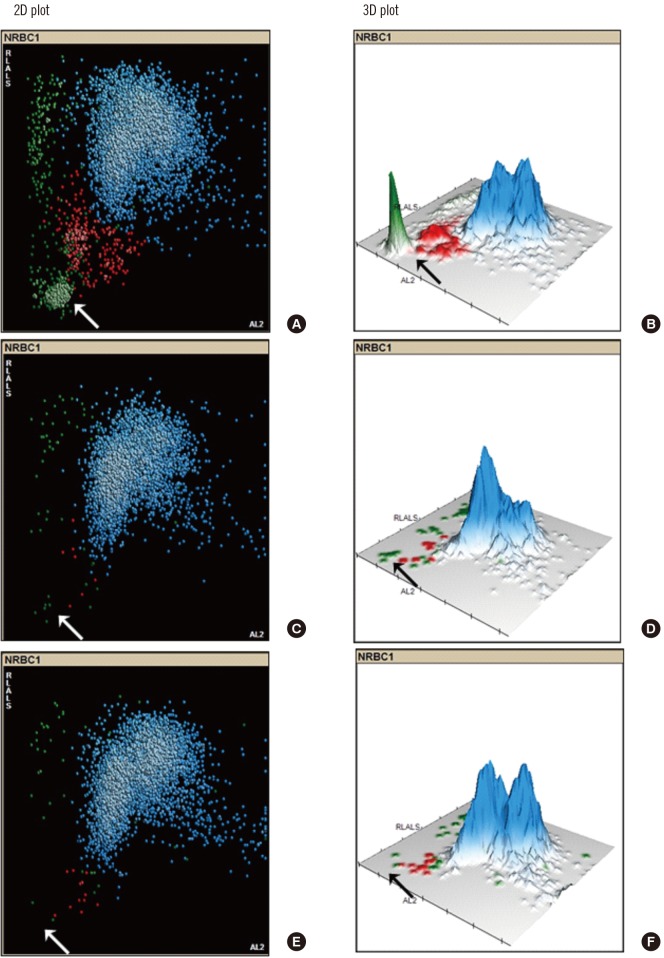
Thus, the patient was presumptively diagnosed as having severe fever with thrombocytopenia syndrome (SFTS) based on the low risk of malaria in his residential area (Ganam-eup, Yeoju-si, Gyeonggi-do) and his recent travel to Jeju island, which is a major endemic area of SFTS in southern Korea [2]. However, routine CBC analysis using the UniCel DxH 800 (Beckman Coulter, Inc., Miami, FL, USA) lead to an “nRBC flag” warning with abnormal levels of nucleated RBC (nRBC; 4.43% and 182×106/L) in the WBC differential. In addition, low rotated low angle light scatter (RLALS)/low axial light (AL2)/low rotated upper median angle light scatter (RUMALS) in the nRBC plot showed unusual signals with characteristic, aggregated, round to upright, spindle-shaped cells, similar to those described in a previous report [3] (Fig. 1A and 1B). The patient was initially treated by oral administration of 800 mg of hydroxychloroquine as a loading dose. This was followed by 400 mg at 6, 24, and 48 hours after the first dose; 48 parasites/µL were detected on hospital day (HOD) 3 (Fig. 1C and 1D), and no malarial parasites were observed on a thin PBS at HOD 7 (Fig. 1E and 1F). Primaquine (30 mg/day) was prescribed to prevent relapse for two weeks, and the patient was discharged from the hospital.
Fig. 1. Sizes of malaria signals (green population indicated by white arrow in 2D plot and black arrow in 3D plot) in nucleated red blood cell plot (rotated low angle light scatter [RLALS] vs axial light [AL2]) is roughly correlated with the parasite burden. (A and B) Positive: 9,134 parasites/µL on hospital day (HOD) 1. (C and D) Positive: 48 parasites/µL on HOD 3. (E and F) Negative: not found on HOD 7 in 2D and 3D plots.
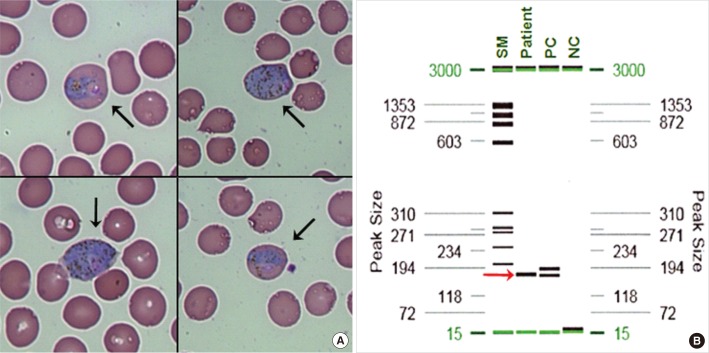
To evaluate this abnormal population, we performed a thin peripheral blood smear (PBS), which revealed different stages of Plasmodium vivax, including mature trophozite, schizont, and gametocytes. Cell counting detected 9,134 parasites/µL (black arrow in Fig. 2A), while no nRBCs were detected. In addition, in-house PCR for screening malaria (Green Cross Co., Yongin, Korea), with the use of modified primers described previously [4,5] confirmed the presence of Plasmodium spp. (red arrow in Fig. 2B). Abdominal computed tomography scan revealed diffusely decreased attenuation on the liver and severe splenomegaly (about 16 cm in size).
Fig. 2. Results of thin peripheral blood smear and malaria PCR. (A) Morphology of different stages of the Plasmodium vivax (indicated by black arrows) in a thin peripheral blood smear. (B) Positive result (indicated by the red arrow) of electrophoresis after PCR screening for malaria.
Abbreviations: SM, size marker; PC, positive control; NC, negative control.
One of the most important advantages of the automated hematology analyzer is that it allows for the timely screening of patients who are clinically unsuspected of malaria, but who may develop malaria rapidly and progress to an adverse clinical prognosis [1]. Compared with automated hematology analyzers such as the Cell-Dyn 4000 (Abbott Diagnostics, Santa Clara, CA, USA) [6], the Coulter GEN.S and LH750 (Beckman Coulter, Inc, Miami, FL, USA) [7,8], and the Sysmex XE-2100 (Sysmex Corporation, Kobe, Japan) [9], the UniCel DxH 800 showed superior analytical performance for screening malarial infection, with sensitivity and specificity of 100% [3]. Lee et al [3] suggested that gametocytes might be the only parasite stage detectable in nRBC through the 5-part differential channels of the DxH800; mature trophozites and gametocytes are larger than other stages of P. vivax and seem to occupy most of the infected RBC, which has a diameter of 6–8 µm [10]. Furthermore, providing appropriate education and training to medical technicians would allow them to recognize CBC parameters associated with malaria infection. A flag for malaria could be incorporated and used to guide rapid malaria antigen tests, PBS, or malarial PCR for patients suspected of having malaria, in order to establish a diagnosis and start treatment promptly [11,12] .
In conclusion, this report proves that the UniCel DxH 800 can easily recognize P. vivax populations without additional reagents or special procedures during routine CBC analysis. Automatic flags generated in automated hematology analyzers would allow us to identify incidental malaria cases and would be useful in endemic and non-endemic regions.
Footnotes
Authors' Disclosures of Potential Conflicts of Interest: No potential conflicts of interest relevant to this article were reported.
References
- 1.Mace KE, Arguin PM. Malaria Surveillance - United States, 2014. MMWR Surveill Summ. 2017;66:1–24. doi: 10.15585/mmwr.ss6612a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi SJ, Park SW, Bae IG, Kim SH, Ryu SY, Kim HA, et al. Severe fever with thrombocytopenia syndrome in South Korea, 2013–2015. PLoS Negl Trop Dis. 2016;10:e0005264. doi: 10.1371/journal.pntd.0005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee HK, Kim SI, Chae H, Kim M, Lim J, Oh EJ, et al. Sensitive detection and accurate monitoring of Plasmodium vivax parasites on routine complete blood count using automatic blood cell analyzer (DxH800(TM)) Int J Lab Hematol. 2012;34:201–207. doi: 10.1111/j.1751-553X.2011.01383.x. [DOI] [PubMed] [Google Scholar]
- 4.Kimura M, Miyake H, Kim HS, Tanabe M, Arai M, Kawai S, et al. Species-specific PCR detection of malaria parasites by microtiter plate hybridization: clinical study with malaria patients. J Clin Microbiol. 1995;33:2342–2346. doi: 10.1128/jcm.33.9.2342-2346.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ciceron L, Jaureguiberry G, Gay F, Danis M. Development of a Plasmodium PCR for monitoring efficacy of antimalarial treatment. J Clin Microbiol. 1999;37:35–38. doi: 10.1128/jcm.37.1.35-38.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suh IB, Kim HJ, Kim JY, Lee SW, An SS, Kim WJ, et al. Evaluation of the Abbott Cell-Dyn 4000 hematology analyzer for detection and therapeutic monitoring of Plasmodium vivax in the Republic of Korea. Trop Med Int Health. 2003;8:1074–1081. doi: 10.1046/j.1360-2276.2003.01135.x. [DOI] [PubMed] [Google Scholar]
- 7.Fourcade C, Casbas MJ, Belaouni H, Gonzalez JJ, Garcia PJ, Pepio MA. Automated detection of malaria by means of the haematology analyser Coulter GEN.S. Clin Lab Haematol. 2004;26:367–372. doi: 10.1111/j.1365-2257.2004.00648.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma P, Bhargava M, Sukhachev D, Datta S, Wattal C. LH750 hematology analyzers to identify malaria and dengue and distinguish them from other febrile illnesses. Int J Lab Hematol. 2014;36:45–55. doi: 10.1111/ijlh.12116. [DOI] [PubMed] [Google Scholar]
- 9.Huh HJ, Oh GY, Huh JW, Chae SL. Malaria detection with the Sysmex XE-2100 hematology analyzer using pseudoeosinophilia and abnormal WBC scattergram. Ann Hematol. 2008;87:755–759. doi: 10.1007/s00277-008-0486-8. [DOI] [PubMed] [Google Scholar]
- 10.McPherson RA, Pincus MR. Henry's Clinical Diagnosis and Management by Laboratory Methods E-Book. St. Louis, MO: Elsevier Health Sciences; 2017. [Google Scholar]
- 11.Campuzano-Zuluaga G, Hanscheid T, Grobusch MP. Automated haematology analysis to diagnose malaria. Malar J. 2010;9:346. doi: 10.1186/1475-2875-9-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma S, Sethi N, Pujani M, Kushwaha S, Sehgal S. Abnormal WBC scattergram: a clue to the diagnosis of malaria. Hematology. 2013;18:101–105. doi: 10.1179/1607845412Y.0000000029. [DOI] [PubMed] [Google Scholar]