Abstract
The principle steroidal androgens are testosterone and its metabolite 5α-dihydrotestosterone (DHT), which is converted from testosterone by the enzyme 5α-reductase. Through the classic pathway with androgens crossing the plasma membrane and binding to the androgen receptor (AR) or via mechanisms independent of the ligand-dependent transactivation function of nuclear receptors, testosterone induces genomic and non-genomic effects respectively. AR is widely distributed in several tissues, including vascular endothelial and smooth muscle cells. Androgens are essential for many developmental and physiological processes, especially in male reproductive tissues. It is now clear that androgens have multiple actions besides sex differentiation and sexual maturation and that many physiological systems are influenced by androgens, including regulation of cardiovascular function [nitric oxide (NO) release, Ca2+ mobilization, vascular apoptosis, hypertrophy, calcification, senescence and reactive oxygen species (ROS) generation]. This review focuses on evidence indicating that interplay between genomic and non-genomic actions of testosterone may influence cardiovascular function.
Keywords: androgen receptor, cardiovascular, genomic, non-genomic
Clinical perspectives
-
•
Androgens have many extragonadal effects, including regulation of the cardiovascular system.
-
•
Via activation of genomic and non-genomic signalling pathways, androgens can lead to divergent outcomes.
-
•
In the vascular system, androgens have the potential to cause NO release, Ca2+ mobilization, vascular apoptosis, hypertrophy, calcification, senescence and ROS generation.
Introduction
Steroid hormones, including androgens, are involved in many developmental and physiological processes [1–4]. Classically androgens mediate their effects via binding to the androgen receptor (AR), a ligand-dependent transcription factor and a member of the nuclear receptor gene superfamily [5,6]. Additionally, androgens can activate signalling pathways via non-DNA binding-dependent actions [7,8]. AR is expressed in many tissues, with the highest concentration being in the male reproductive organs [9]. The AR has three functional domains: exon 1 encodes the N-terminal transactivation domain (NBD), exons 2 and 3 encode the DNA-binding domain (DBD) and exons 4–8 encode the C-terminus ligand-binding domain (LBD) [10,11].
The AR is expressed in many cells of the cardiovascular system including cardiomyocytes [12], endothelial cells [13], vascular smooth muscle cells (VSMCs) [14], fibroblasts [15], macrophages [16] and platelets [17]. There are sex differences in AR expression; males have significantly higher levels of AR mRNA than females [18]. In addition, males demonstrate greater AR activation with endogenous testosterone, and prolonged exposure to endogenous testosterone leads to up-regulation of AR [19].
Testosterone is the principal male steroid hormone from the androgen family. Approximately 95% of endogenous testosterone is produced by the testes and it is secreted by the Leydig cells [20]. Small amounts of testosterone are also secreted by the zona reticularis of the adrenal glands [21]. The physiological levels of testosterone in men range from 10 to 30 nM with lower levels found in women (0.6–2.5 nM) [22]. Testosterone is synthesized from cholesterol and stored in lipid droplets through a series of reactions that occur in mitochondria and microsomes (smooth endoplasmic reticulum and surrounding cytoplasm). The first step of steroidogenesis is a transfer of cholesterol to the internal mitochondrial membrane with subsequent bioconversion in pregnenolone by the enzyme cytochrome P450 SCC [23]. Pregnenolone is then transferred to the endoplasmic reticulum where it is converted into testosterone through a series of enzymatic reactions via generation of 17α-hydroxypregnenolone and subsequent formation of dehydroepiandrosterone (DHEA) or via 17α-hydroxyprogesterone. Approximately 7% of testosterone can then be converted to a more potent metabolite, dihydrotestosterone (DHT) via 5α-reductase, and small amounts (approximately 0.5%) to oestrogen via P450 aromatase [24–26].
Testosterone binds with high affinity to the cytosolic or membrane AR and then regulates male sex development and maturation [25] as well as having crucial extra-gonadal effects including regulation of apoptosis via cleavage of procaspase 8 in VSMC [14], regulation of leucocyte migration and reactive oxygen species (ROS) generation [27], control of the nitric oxide (NO)–cGMP pathway [2] and improvement of insulin sensitivity [28]. Testosterone has also been used clinically in erectile dysfunction (ED), infertility, osteoporosis, to promote bone marrow stimulation and to stimulate penile enlargement and height growth [29,30]. In athletes, testosterone has been shown to enhance performance via muscle development, improved strength and endurance [31]. Moreover, androgens have been implicated to play a role in pathological processes when dysregulated [32].
Testosterone has been associated with cardiovascular pathology as evidenced by a higher male susceptibility to cardiovascular disease [19,33]. However, there is increasing evidence that low endogenous levels of testosterone may also be associated with cardiac dysfunction [34–36]. A reduction in total testosterone of 2.18 SD is associated with a 25% increased risk of cardiovascular mortality [37]. To date, the role of androgens in cardiovascular health and disease remains controversial.
AR is a single copy gene found on the X chromosome at Xq11-12 and mutations and polymorphisms in it are thought to be inversely proportional to the transcriptional response to testosterone [38]. To regulate target gene transcription, testosterone and DHT can bind to the AR in a DNA binding-dependent manner leading to new protein synthesis [25], or in a non-DNA binding-dependent manner that involves a rapid induction of secondary messengers to initiate cellular events, such as protein phosphorylation [39]. DHT is more biologically active than testosterone, which is associated with the 2-fold higher affinity for the AR and a reduction of 5-fold in the dissociation rate compared with testosterone [40].
The classical DNA binding-dependent actions of the androgens
In the basal state, without ligand binding, the AR is located primarily in the cytoplasm where it associates with heat shock proteins (HSPs), which are thought to tether AR via cytoskeletal proteins and modulate AR conformation in preparation for efficient ligand binding [41,42]. The classical AR signalling pathway commonly referred to as ‘genomic’ or ‘canonical’ AR signalling involves androgens crossing the plasma membrane, entering the cytoplasm and binding to the AR, resulting in a dissociation of chaperone proteins, translocation of the complex to the nucleus where it dimerizes and binds to androgen response element (ARE) to modulate gene transcription and subsequently protein synthesis [40]. AR binding to specific ARE results in recruitment of histone acetyltransferase (HAT) enzymes and a number of essential co-regulators [41]. This facilitates binding of TATA-binding protein (TBP) followed by general transcription factors (GTF and RNA pol II) to begin transcription and to regulate the expression of androgen-regulated genes [41,43].
Genomic action of the AR in vascular calcification
The relationship between testosterone and calcification, which is an important predictor of morbidity and mortality from cardiovascular disease, has been explored [44]. There is significant sexual dimorphism in the development of vascular calcification; males tend to have higher levels of calcium deposition, and this has been attributed as potentially secondary to the effects of the AR [45]. Recently, it was demonstrated that higher expression of AR occurs in calcified human aortic valve compared with controls. Treatment with androgens (testosterone or DHT) for 9 days resulted in up-regulation of AR expression in WT mice and also induced calcification, as shown by elevated calcium deposition and mRNA expression of Alpl, a marker of cellular mineralization, effects reduced in specific AR-ablated VSMC with a concurrent reduction in the mRNA expression of the osteogenic marker Osterix [46]. Other studies indicate the opposite, testosterone as an anti-calcification agent. Growth arrest-specific gene 6 (Gas6) is an important molecule regulating calcification of VSMC [47]. Gas6 is considered a pro-survival agent that reduces apoptosis, an essential process for VSMC calcification [48]. In VSMC, AR was found to directly bind to the ARE in the Gas6 promoter region and to transactivate Gas6. This resulted in inhibition of inorganic phosphate (Pi)-induced calcification of vascular cells. Restoration of Gas6 signalling induced by testosterone is mediated by phosphorylation of the phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) pathway, and an increase in anti-apoptotic Bcl2 family proteins. This effect is blunted by AR antagonists [49] and provides a mechanism behind the possible cardioprotective action of androgens, as suggested by the high levels of vascular calcification in men with hypogonadism [45]. Testosterone also regulates VSMC senescence via Gas6 activation. Angiotensin II (Ang II)-induced down-regulation of Gas6 in VSMC is restored by testosterone, which is followed by reduced expression and activity of MMP-2 and reduced Ang II-induced collagen synthesis effects not observed in the presence of Gas6 blockers and Axl-Fc and PI3K inhibitors. These results suggest a novel mechanism that involves Gas6/Axl and Akt in the protective effects of testosterone on vascular ageing [50].
Genomic action of the AR in renal function, cardiac function and vasodilation
Functionally, active AR is also thought to be integral to the maintenance of normal cardiac and renal function. Cardiac and renal hypertrophy is common in Fabry disease, a condition caused by the deficiency of lysosomal enzyme α-galactosidase A [51]. The α-galactosidase A knockout mice, a model of Fabry disease, demonstrate increased mRNA and activity of AR in heart and kidneys, as indicated by increased expression of insulin-like growth factor 1, an androgen regulated gene, and reduced expression of transforming growth factor-β1, which is negatively regulated by AR. Castration and the consequent hypogonadism or AR-antagonism therapy results in a significant reduction in Akt phosphorylation and an improved phenotype in the heart and kidneys of Fabry disease model mice [52]. Echocardiography demonstrated improved heart-to-body weight ratios and left ventricle wall thickness and cardiac atrial natriuretic peptide mRNA levels in castrated mice. Kidney weight also remained at WT level in these mice [52].
To explore the role of the AR in cardiac growth, Ikeda et al. used 25-week-old AR knockout (ARKO) mice and age-matched wild-type male mice, which were treated with or without Ang II stimulation at a dose of 2mg/kg per day for 2 weeks [53]. The importance of the AR in cardiac development and function is highlighted by the phenotype of AR knockout animals, as ARKO mice have a significant reduction in cardiac hypertrophy induced by Ang II and heart-to-body weight ratio compared with WT, events associated with lower activation of extracellular signal-regulated kinases (ERKs) 1/2 and ERK5. In addition, impairment of left ventricle function and cardiac fibrosis induced by Ang II is reduced in ARKO mice [53].
Cross-talk between cytosolic and nuclear signalling pathways is involved in testosterone-induced cardiac hypertrophy. Glycogen synthase kinase 3 (GSK-3β) is considered an anti-hypertrophic factor in cardiac cells [54]. In cardiomyocytes, treatment with testosterone leads to phosphorylation of GSK-3β inhibitory site (Ser9), an increase in intracellular levels of calcium with consequent activation of calcineurin and nuclear factor of activated T cells (NFAT) and an increase in both cell size and [3H]-leucine incorporation, which suggest cardiomyocyte hypertrophy [55], suggesting that GSK-3β may be a pharmacological target to inhibit testosterone-induced cardiac hypertrophy.
Vasodilation, a well-described event associated with testosterone, seems to be, at least in part, regulated by AR activation. Hydrogen sulphide (H2S) is considered a prominent endothelium-derived hyperpolarizing factor that induces vasodilation via TRPV4 and large-conductance Ca2+-activated K channels [56]. Testosterone stimulation in thoracic aorta from male Wistar rat results in a concurrent increase in the production of H2S, and associated vasodilation, which is AR-dependent [57–59]. Interestingly high levels of H2S inhibit AR binding in human prostate cancer cells, suggesting a tissue-specific feedback loop, which may offer future treatment options for castration resistant prostate cancer [60]. Moreover, chronic stimulation with androgens (24 h) seems to have a direct effect in endothelial cells. DHT increases the levels of vascular endothelial growth factor and improves the proliferative, migratory and adhesive abilities of endothelial progenitor cells, events regulated by the RhoA/ROCK pathway [4].
Androgens also have a direct effect on Ang II type-2 receptor (AT2R) expression. In aortas isolated from male rats, AT2R mRNA and protein expression levels are lower than in females. The elevated level of AT2R mRNA and protein expression in endothelium-intact aorta from female rats can be reversed by DHT administration, an effect attenuated through co-administration of AR antagonist and not observed in the presence of an ERK1/2 inhibitor. Interestingly, DHT therapy in females did not alter AT2R expression in endothelium-denuded aorta. On the other hand, castration of male rats significantly elevated AT2R mRNA and protein expression, suggesting that independent of the sex, testosterone via AR has a direct effect on expression of the Ang II receptor [61].
Genomic action of the AR in erectile function
ED provides another example of the clinical significance of the genomic effects of androgens. ED is considered a complex neurovascular phenomenon and hypogonadism is the most common risk factor for this, leading to insufficient arterial blood flow to the penis [62–65]. Castrated rats exhibit impaired erectile function and internal pudendal arteries from castrated animals demonstrate impairment in vasoconstrictor and vasodilator function, which is associated with hypotrophic vascular remodelling, decreased neuronal nitric oxide synthase (nNOS) and α-actin expression and increased collagen expression, p38 mitogen-activated protein kinases (p38) phosphorylation and caspase 3 cleavage [66]. In penile tissue, AR expression reduces in an age-dependent manner and also in a testosterone dose-dependent manner. The reduced AR expression may therefore play a role in the ED vascular phenotype [67].
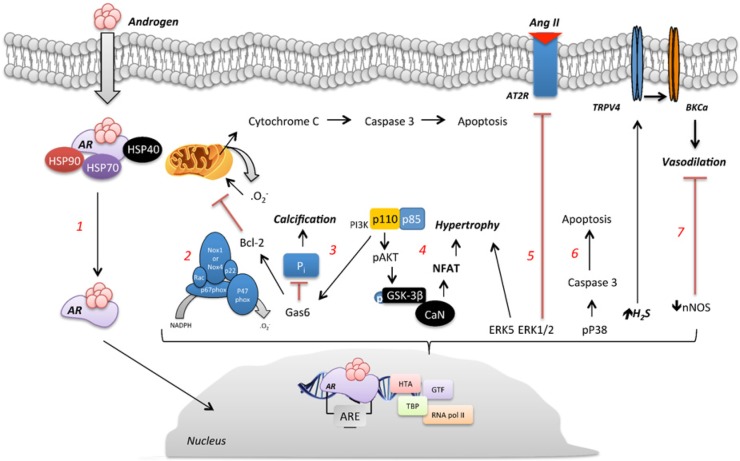
Table 1 and Figure 1 summarise the genomic actions of androgens on the vasculature [4,46,49,50,52,53,55–59,61].
Table 1. Summary of the genomic effects of androgens.
| Androgen | Cell/Tissue | Effect | Reference |
|---|---|---|---|
| Testosterone DHT |
VSMC mouse | ↑ AR expression ↑ Calcium deposition ↑ mRNA expression Alpl |
Zhu et al. (2016) [46] |
| Testosterone | Human aortic smooth muscle cells | Phosphorylation of PI3K/Akt Transactivation Gas6 |
Son et al. (2010) [49] |
| Testosterone | VSMC mouse | ↓ Senescence ↓ Expression MMP-2 ↓ Ang II-induced collagen synthesis |
Chen et al. (2016) [50] |
| Testosterone | α-galactosidase A knockout mice | ↑ AR expression and mRNA ↓ Akt phosphorylation with castration |
Shen et al. (2015) [52] |
| Testosterone | ARKO mice | ↓ ERK 1/2 and ERK 5 | Ikeda et al. (2005) [53] |
| Testosterone | Cardiomyocytes | Phosphorylation GSK-3β inhibitory site (Ser9) ↑ Intracellular calcium ↑ Calcineurin and NFAT ↑ Cell size |
Duran et al. (2016) [55] |
| Testosterone | Thoracic aorta rat | ↑ H2S production ↑ Vasodilation |
Bucci et al. (2009) [57] Brancaleone et al. (2015) [58] Mustafa et al. (2011) [59] |
| DHT | Endothelial progenitor cells | ↑ VEGF ↑ Proliferation, migration and adhesion of cells |
Zhang et al. (2016) [4] |
| DHT | Rat aorta | ↓ AT2R mRNA and protein expression ↑ ERK 1/2 activation |
Mishra et al. (2016) [61] |
Figure 1. DNA binding-dependent signalling induced by androgens.
(1) The genomic AR signalling involves androgen crossing the plasma membrane, entering the cytoplasm, dissociation of chaperone proteins and binding to the AR. (2) Testosterone induced-ROS generation is followed by an increase in Nox1 and Nox4 mRNA levels and p47phox protein expression. (3) Gas6 signalling induced by testosterone is mediated by phosphorylation of the PI3K/Akt pathway, and an increase of anti-apoptotic Bcl2 family proteins. (4) Hypertrophy induced by testosterone involves recruitment of NFAT through calcineurin activation and GSK-3β inhibition. (5) Testosterone down-regulates the AT2R receptor via AR-mediated ERK1/2 activation. (6) Hypogonadism is shown to decrease nNOS and α-actin expression and increase p38 phosphorylation and caspase 3 cleavage. (7) Testosterone stimulation results in a concurrent increase in the production of H2S, and consequently vasodilation via TRPV4 and large-conductance Ca2+-activated K-channels.
Non-DNA binding-dependent actions of the androgens
In the past, interactions with a nuclear sex hormone receptor followed by transcription factor activity were implicated as the principal molecular mechanism responsible for androgen activity. However, there is increasing evidence that androgens can also act via mechanisms independent of the ligand-dependent transactivation function of nuclear receptors [68]. This is known as ‘non-genomic’ signalling, which typically occurs within a short time frame [69].
To be considered a non-genomic response, the androgen-induced response must occur in a time frame not long enough to allow gene transcription, normally seconds to minutes. The response should be observed even when the androgen is conjugated to molecules such as bovine serum albumin (BSA) that prevent it from entering into the cytoplasm. A third criterion requires that the non-genomic response should not be blunted by inhibitors of transcription and does not require a functional nucleus or transcription/translation machinery activation [39,69,70]. The non genomic actions of androgens in the vasculature are summarised in Figure 2 and Table 2.
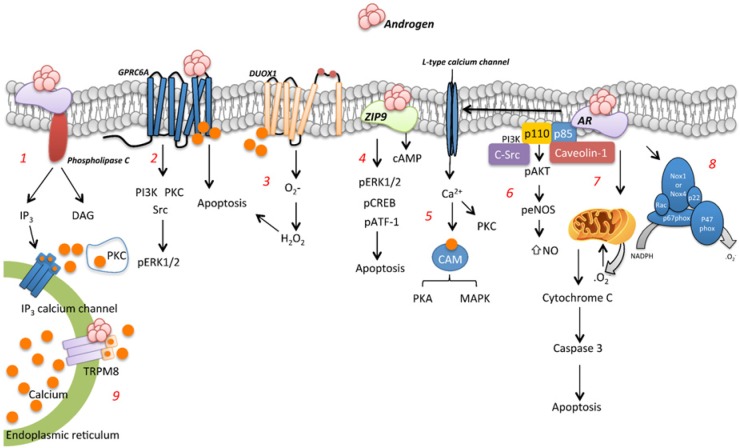
Figure 2. Non-DNA binding-dependent signalling induced by androgens.
(1) Testosterone via rapid response activates PLC, IP3 and DAG and initiates intracellular calcium release and PKC activation. (2) Via binding to GPRC6A, testosterone leads to ERK phosphorylation by mechanisms involving PI3K, PKC and Src. (3) GPRC6A mediates the non-genomic effects of testosterone on intracellular calcium mobilization and H2O2 through Duox1. (4) ZIP9 activation induced by testosterone is involved in testosterone induced ERK1/2, CREB and pATF-1 phosphorylation. (5) Via interaction with AR, androgens activate L-type calcium channels, which increase the intracellular levels of calcium, activate PKC, and via calmodulin activate PKA and MAPK pathways. (6) Activation of PI3k/Akt signalling and the direct interaction of AR with p85α/c-Src/caveolin1 are involved in testosterone-induced eNOS phosphorylation. (7) Testosterone increases mitochondrial-ROS generation and procaspase-8 and -3 activation in VSMC, an effect followed by reduction of O2 consumption, increased expression of death receptors and apoptosis. (8) Rapid generation of ROS induced by testosterone involves NAPH oxidase activation. (9) Androgen binding to TRPM8 is followed by an increase in TRPM8-induced increase in intracellular levels of Ca2+.
Table 2. Summary of non-genomic effects of androgens on vascular tissue.
| Androgen | Cell/Tissue | Effect | Reference |
|---|---|---|---|
| Testosterone | Murine macrophages | ↑ Intracellular calcium ↑ PLC Activation RAS/MEK/ERK MAPK pathways |
Wunderlich et al. (2002) [75] Foradori et al. (2008) [39] |
| Testosterone | Cardiac myocytes | ↑ Release Ca2+ from endoplasmic reticulum and mitochondria | Bennett et al. (2010) [41] Foradori et al. (2008) [39] |
| Testosterone | Male rat osteoblasts | ↑ Cytosolic free calcium ↑ IP3 and DAG formation |
Lieberherr et al. (1994) [74] |
| Testosterone | AEC | Rapid ↑ NO eNOS phosphorylation PI3K, cavceolin-1 and c-Src binding to AR AKT phosphorylation |
Son et al. (2010) [49] Yu et al. (2010) [79] |
| Testosterone | VSMC | Inhibits PGF2α induced Ca2+ influx | Ma et al. (2009) [81] |
| Testosterone | Fingertip arterial pulse | ↓ Arterial stiffness Acute vasodilation |
Francomano et al. (2016) [82] |
| Testosterone | Prostate cancer cells | TRPM-8 induced ↑ intracellular Ca2+ | Zhang et al. (2004) [89] |
| Synthetic R1881 Testosterone |
HEK-293 cells transfected with GPRC6A | ↑ ERK activity | Pi et al. (2010) [128] |
| Testosterone | VSMC rats | ROS generation ↑ Nox1 and Nox4 mRNA ↑p47phox protein VSMC migration |
Chignalia et al. (2012) [129] |
| Testosterone | Epidermal keratinocytes | Rapid Ca2+ mobilization from endoplasmic reticulum ↑ H2O2 generation ↓ Mitochondrial membrane potential ↓ Apoptosis ↑ Duox1 stimulation ROS generation |
Ko et al. (2014) [96] |
| Testosterone | 93RS2 Sertoli cells | ERK1/2 phosphorylation CREB phosphorylation ATF-1 phosphorylation |
Bulldan et al. (2016) [86] |
| Testosterone | Prostate and breast cancer cell lines | Activation of G proteins Up-regulation JNK gene expression ERK phosphorylation ↑ Pro-apoptotic Bax, caspase 3, cytochrome c proteins Apoptosis |
Thomas et al. (2014) [87] |
| Testosterone | VSMC | Mitochondrial ROS generation Procaspase-8 and -3 activation ↓ O2 consumption Apoptosis |
Lopes et al. (2014) [14] |
Calcium mobilization and vascular function
The most robust evidence that androgens induce cellular effects through non-genomic signalling is the rapid rise of intracellular calcium concentration [71,72]. Hypogonadism is associated with an increased risk of osteopenia and osteoporosis, an effect normalized by testosterone replacement [73]. In male rat osteoblasts, low concentrations of testosterone, 10 pm/l–1 nM/l increase cytosolic free calcium and membrane phospholipid metabolism in a very rapid time (5–60 s), an effect followed by an increase in the cellular content of inositol 1,4,5-trisphosphate (IP3) and diacylglycerol (DAG) formation, events not observed in female rat osteoclasts, which suggest that the rapid effect induced by testosterone is sex dependent. Interestingly, androgen-induced increases in intracellular levels of calcium are also observed in testosterone conjugated with BSA, suggesting a response that involves membrane embedded or associated receptors or binding proteins [74]. Androgens/AR can also activate L-type calcium channels, which increase the intracellular levels of calcium, activate protein kinase C (PKC) and via calmodulin activate protein kinase A (PKA) and MAPK pathways [39].
Non-genomic Ca2+ mobilization by androgens was also observed in murine macrophages. In macrophages, testosterone increases intracellular levels of Ca2+ [75]. During this process, androgen interacts with membrane-associated AR, modulates G-protein activity and subsequently activates phospholipase C (PLC). This results in the rapid release of intracellular calcium stores from the sarcoplasmic reticulum and consequently activation of the RAS/MEK/ERK MAPK pathway [39]. Likewise through activation of plasma membrane AR associated with GPCR signalling in cardiac myocytes, stimulation with testosterone induces the release of Ca2+ from internal stores, such as endoplasmic reticulum and mitochondria [39,41].
Acute testosterone-induced non-genomic vasodilatation is mediated in part via endothelium-derived NO [76,77]. Aortic endothelial cells (AEC) stimulated with testosterone or non-permeable testosterone-BSA at physiological concentrations (1–100 nm) present rapid (15–30 min) increases in NO level in AEC; testosterone also induces endothelial nitric oxide synthase (eNOS) phosphorylation (Ser1177) without changing the total protein level. Activation of eNOS occurs via PI3K, caveolin-1 and c-proto-oncogene tyrosine-protein kinase (Src) binding to AR and consequently phosphorylation of AKT. AR and s-Src mediate testosterone-induced rapid eNOS phosphorylation, since pre-treatment with nilutamide or PP2, an AR and s-Src antagonist respectively, abolishes the testosterone responses. Transcriptional inhibitor, actinomycin D does not affect testosterone-induced increase in NO, which excludes the classical genomic actions [78,79]. Anastrozole or other oestrogen receptor antagonists do not interfere in NO generation induced by testosterone, suggesting that this is not an event associated with the aromatization of testosterone to oestradiol [80]. In addition, testosterone at physiological concentrations inhibits PGF2α-induced Ca2+ fluxes by a non-genomic mechanism in VSMC [81], which may contribute to testosterone-induced vasodilatation.
Vasodilatation not associated with DNA-binding induced by testosterone is also observed in humans. A recent paper demonstrated that administration of transdermal testosterone in men with hypogonadism and severe hypotestosteronaemia causes an acute vasodilation and improves arterial stiffness by non-genomic mechanisms, although interestingly, the improvement is also evident after 96 h of treatment, which would suggest a combination of genomic and non-genomic effects to reach the same response [82].
The molecular mechanisms underlying non-genomic actions include not only the translocation of the AR to the cell surface membrane [25] as many types of cells that demonstrate a rapid androgen response do not express the classic nuclear AR or are not blocked by AR antagonists, suggesting that in addition to the traditional AR, other proteins are capable of binding androgens and activating signal transduction cascades [39]. In addition to AR, androgens can also bind to lipids of the plasmatic membrane, promoting direct modification of ion channels [69], activation of GPRC6A [83–85] and interaction with ZIP9, a Zn2+ transporter from the family of the zinc-regulated transporter (ZRT), iron-regulated transporter (IRT)-like proteins [86,87].
An important example of testosterone-induced signal transduction cascades not dependent of binding to AR is the androgen binding to transient receptor potential cation channel subfamily M member 8 (TRPM8). TRPM8 plays an important role in the pathophysiology of prostate cancer and is considered an ionotropic testosterone receptor [88]. In prostate cancer LNCaP cells, TRPM8 acts as a Ca2+-permeable channel and is expressed in the endoplasmic reticulum and plasma membrane. siRNA or inhibition of TRPM8 is associated with apoptosis of LNCaP cells. Increased levels of testosterone are followed by a greater TRPM8-induced increase in intracellular levels of Ca2+ [89]. Picomolar concentrations of testosterone elicited Ca2+ responses and channel currents, and those were inhibited in the presence of a TRPM8 antagonist [90]. Considering that TRPM8 has an important role in cell survival and that TRPM8 is modulated by androgens, it might be predicted that anti-androgen therapy decreases the percentage of LNCaP viable cells via reduction of TRPM8.
GPRC6A is expressed in many tissues including bone marrow stromal cells, monocytes, prostate cancer cells, skeletal muscle cells, vascular smooth muscle and endothelial cells and Leydig cells [83,91]. Synthetic androgen R1881 and testosterone alone or conjugated with BSA, in a calcium dependent manner, rapidly stimulate ERK activity in HEK-293 cells (which lack both the AR and GPRC6A receptor) transfected with GPRC6A, but not in the non-transfected HEK-293 controls. This effect is reversed by an MAPK inhibitor, PI3K inhibitor, Src inhibitor and PKC inhibitor; flutamide has no effect on testosterone-stimulated GPRC6A activation of p-ERK. Interestingly, R1881 does not stimulate ARE-luciferase activity in HEK-293 cells expressing only GPRC6A, but does stimulate HEK-293 cells transfected with AR, suggesting activation of nuclear receptor signalling. In vivo, testosterone-induced ERK phosphorylation in the bone marrow and testes is markedly attenuated in GPRC6A−/− mice, demonstrating that GPRC6A is a non-classical receptor for which androgens induce ERK activation both in vitro and in vivo [92].
ROS generation and apoptosis
Testosterone has been implicated in hypertension-induced vascular remodelling, an event associated with ROS generation. ROS have been recognized as important messengers in cell signalling [93]. Testosterone induces ROS generation in VSMC isolated from normotensive (Wistar Kyoto, WKY) and hypertensive (spontaneously hypertensive rat, SHR) rats, an effect followed by an increase in nicotinamide adenine dinucleotide phosphate oxidase (Nox)1 and Nox4 mRNA levels and p47phox protein expression and VSMC migration. Curiously, rapid ROS generation in SHRSP is not inhibited by flutamide or actinomycin D, indicating a non-genomic effect. The complexity of the assessment of the genomic and non-genomic effects of testosterone in the vasculature is highlighted in this study as testosterone augmented ROS formation after 2 h was blocked by flutamide and actinomycin D, suggesting a genomic pathway and demonstrating that testosterone has the potential to act in multiple different ways in the same cells [94].
In addition to Nox1 and Nox4, the aforementioned isoforms, the Nox family includes five others isoenzymes (gp91 phox, renamed Nox2, Nox3, Nox5, Duox1 and Duox2) [95]. In epidermal keratinocytes, testosterone stimulation results in rapid and transient Ca2+ mobilization from the endoplasmic reticulum within 1 min, an effect reduced by transfection of GPRC6A siRNA and followed by an increase in H2O2 generation. Testosterone-induced H2O2 generation is not reverted by flutamide but not observed in the presence of DPI, an Nox inhibitor. ROS generation is not observed in Duox1-silenced or GPRC6A-silenced keratinocytes. Stimulation of keratinocytes with testosterone results in decreased mitochondrial membrane potential and apoptosis, an event also regulated by GPRC6A-dependent Ca2+ mobilization. Together, these results suggest that GPRC6A-dependent Ca2+ mobilization stimulates the activity of Duox1, leading to ROS generation and apoptosis [96]. The pro-apoptotic effect of testosterone is also observed in VSMC. Testosterone increases mitochondrial-ROS generation and procaspase-8 and -3 activation in VSMC, an effect followed by reduction of O2 consumption, increased expression of death receptors and apoptosis [14]. It has not yet been investigated whether GPRC6A or Duox-1 are also involved in testosterone-induced ROS generation and apoptosis in VSMC, which would be a new mechanism by which testosterone influences vascular function and may play a role in cardiovascular diseases. Together, the previous results suggest that it is possible that the effects in the vascular system induced by androgens are mediated by signalling cascades activated by oxidative stress, which highlights ROS as an important target particularly in patients with augmented testosterone levels.
It has been demonstrated that GPRC6A is not only an androgen target but also an androgen regulator. GPRC6A knockout mice display feminization of the external genitals, characterized by reduction in genitoanal distance as well as testicular size, which is followed by reduced levels of testosterone, but no difference in AR levels. Interestingly, oestradiol concentrations are significantly higher in male GPRC6A−/− mice compared with wild-type littermates, an event associated with the increase in aromatase expression, a protein responsible for catalysing the oestrogen biosynthesis from androgens. GPRC6A is highly expressed in the kidney [97] and GPRC6A−/− mice present an increase in urinary calcium and phosphate excretion and also excretion of β2-microglobulin. In addition, liver from GPRC6A−/− mice exhibits histological markers of hepatic steatosis [98]. Considering that GPRC6A is involved in the rapid effects of testosterone and that GPRC6A has multiple functions, it is possible that many important non-genomic effects induced by testosterone are still unknown.
In addition to GPRC6A, non-DNA binding-dependent actions of testosterone can also be associated with androgen binding to ZIP9, a membrane-integrated receptor [86]. In this case, ZIP9 would perform dual functions as a membrane AR and zinc transporter. In 93RS2 Sertoli cells, a cell line that does not express AR, testosterone (10 nM) induces ERK1/2 phosphorylation. Similar effects were also observed in cAMP response element-binding protein (CREB) and activating transcription factor 1 (ATF-1) phosphorylation, effects suppressed by ZIP9 siRNA, indicating that ZIP9 is involved in the testosterone-induced signalling pathway [86].
As previously mentioned, testosterone induces apoptosis in different types of cells, including VSMC [14,89,96], an event where ZIP9 seems to play an important role. In cancer cells, testosterone stimulation induces activation of G proteins, up-regulation of JNK gene expression, ERK phosphorylation and increased expression of pro-apoptotic Bax, caspase 3 and cytochrome c proteins, culminating in apoptosis. Transfection of ZIP9 siRNA is accompanied by a complete loss of testosterone-induced apoptosis [87]. It has not yet been investigated whether this novel steroid signalling pathway is initiated through the zinc transporter ZIP9 in VSMC also.
Implications for androgen therapy in cardiovascular disease
The use of androgens leads to effects that range from protective to deleterious [99], resulting in an ongoing debate regarding the clinical benefits and long-term risks of testosterone therapy. As previously mentioned, genomic and non-genomic effects of testosterone can result in different responses, which may help us to understand the divergent outcomes of testosterone therapy in the cardiovascular system.
Men with low testosterone have a high prevalence of cardiovascular disease and metabolic syndrome [100–102] and testosterone therapy in these individuals has been associated with reduced obesity, fat mass, waist circumference and mortality as well as improved glycaemic control and overall cardiometabolic status compared with placebo [103]. On the other hand, testosterone supplements are known to increase haematocrit levels and reduce HDL (high-density lipoprotein) cholesterol levels and have been implicated in cases of cardiovascular morbidity and mortality [104]. Despite this, a systematic review and meta-analysis evaluating the cardiovascular effects of testosterone supplementation in 3016 men who were supplemented with testosterone and 2448 placebo-treated men found no causal role between testosterone supplementation and cardiovascular events [105]. The results are so divergent that even the route of administration of testosterone may be associated with differing cardiovascular risk [106].
A prospective study with 11,606 men, aged 40–79 years, found that testosterone baseline levels are inversely related to mortality due to all causes, cardiovascular diseases and cancer [34]. All-cause mortality is increased in hypogonadal men with Type 2 diabetes and testosterone therapy reduces mortality to 8.4% compared with 19.2% in the untreated group [107]. Corroborating these results, a large multi-centre, randomized, double-blind, placebo-controlled study undertaken in eight European countries in men with Type 2 diabetes and/or the metabolic syndrome showed that testosterone replacement therapy (TRT) improves cardiovascular risk factors in men, including body fat composition, cholesterol, insulin resistance and sexual function [28].
In humans, low testosterone levels are associated with endothelial dysfunction [108], which can be reverted by testosterone therapy. The vascular function of male patients as examined by the vasomotor function of the brachial artery and intima-media thickness of the carotid artery demonstrated that low levels of testosterone are associated with endothelial dysfunction, independent of body mass index, presence of diabetes, hyperlipidaemia or hypertension and age [109].
However, protective effects in the heart are also observed with testosterone therapy. Haemodynamic parameters in patients and animal models of heart failure are improved by testosterone therapy, mainly via increased coronary blood flow through vasodilation, reduction in peripheral vascular resistance and via direct effects in the cardiac tissue such as inhibition of cardiac cAMP phosphodiesterases [110,111]. These potentially protective effects have been considered in a recent clinical study by Cheetham et al. [112], which compared a group of 8808 men who had received TRT and 35,527 men who had never received TRT. The primary outcome of the study was an amalgamation of incidence of acute myocardial infarction, coronary revascularization, unstable angina, stroke, transient ischaemic attack and sudden cardiac death. The rates of cardiovascular disease, as determined by this amalgamation of information were 23.9 in the no-TRT group versus 16.9 per 1000 in the TRT groups, demonstrating that testosterone supplementation in men with androgen deficiency results in a reduced risk of adverse cardiovascular outcomes [112].
Low-density lipoprotein, total cholesterol and triglycerides are reduced by testosterone therapy; in addition, testosterone replacement increases high-density lipoprotein (HDL) and inhibits fatty streak formation, suggesting a protective effect against atherosclerosis [113–115]. Similarly, some studies including 4-year follow-up study found that the degree of atherosclerosis progression is inversely associated with testosterone levels [116,117].
Despite the results mentioned above, androgens may have a deleterious influence in the cardiovascular system via an increase in blood pressure and renal dysfunction. Increased renal vascular resistance and ROS generation in male elderly SHR are prevented by orchiectomy [118,119]. Likewise infusion of DHT in animals is associated with an increase in blood pressure, increase in sodium and water reabsorption and also ROS generation, an effect reversed by 6 weeks of treatment with the SOD mimetic tempol [120,121]. As mentioned before testosterone also induces ROS generation and apoptosis of VSMC [14], increases the level of important sources of ROS and NADPH oxidase [94] and also decreases the expression of antioxidant enzymes [122], which suggests that detrimental effects induced by testosterone can involve an imbalance between pro- and-antioxidant systems, leading to oxidative stress.
Deleterious effects of testosterone are also observed in females. Increased testosterone levels in women with polycystic ovary syndrome are associated with cardiovascular and metabolic disease. These patients have a 2-fold-increased risk for arterial disease independent of body mass index, hypertension and diabetes status [123,124]. In addition, women with cardiovascular disease have higher levels of free androgen compared with controls [125].
Many studies have demonstrated that an equilibrium in testosterone levels is essential for the appropriate function of many signalling pathways in different organs and tissues (Figures 1 and 2). However, the protective/deleterious effect induced by testosterone therapy remains controversial. Differential effects are possibly due to activation of distinct sets of signalling pathways. The European Male Ageing Study (EMAS) is a prospective multi-centre approach that followed up 1887 men over a median of 4.3 years [126]. They investigated the AR gene exon 1 CAG repeat length of these men, as this may be associated with androgen action [127]. In individuals with longer repeats, an intact gonadal axis compensated for this adverse genetic background, meaning that affected individuals with normal hormone biochemistry did not have an increased risk of cardiovascular or other medical conditions, suggesting that the effect of testosterone may be mediated through non-genomic actions in these individuals [126]. It is clear that the improved understanding of genomic and non-genomic effects of testosterone will therefore lead to the potential for development of novel therapeutic targets for patients with cardiovascular disease.
Conclusions
It is clear that genomic and non-genomic effects induced by androgens have implications for the development of cardiovascular disease. These effects range from protective, such as reduced fat mass, to deleterious including activation of pro-apoptotic and pro-oxidant signalling pathways. Accordingly, a consensus has yet to be reached regarding the effects of testosterone on the cardiovascular system. Considering that even testosterone-induced genomic and non-genomic responses could lead to divergent outcomes such as rapid improvement of vascular function via release of NO and hydrogen sulphide or chronic vascular dysfunction associated with calcification, the improved understanding of the mechanisms by which testosterone induces acute or chronic responses could be crucial to comprehend the discrepant outcomes induced by androgens. Given that cardiovascular disease remains a major cause of human death, particularly in males and post-menopausal women, further translational research in the field of genomic and non-genomic effects of testosterone may lead to novel therapeutic targets for patients in the future.
Abbreviations
- AEC
aortic endothelial cells
- Akt
protein kinase B
- Ang II
angiotensin II
- AR
androgen receptor
- ARE
androgen response element
- ARKO
androgen receptor knockout
- ATF-1
activating transcription factor 1
- AT2R
angiotensin II type-2 receptor
- Bax
bcl-2-like protein 4
- Bcl2
B cell lymphoma 2
- BSA
bovine serum albumin
- cAMP
cyclic adenosine monophosphate
- CREB
cAMP response element-binding protein
- DAG
diacylglycerol
- DBD
DNA-binding domain
- DHEA
dehydroepiandrosterone
- DHT
dihydrotestosterone
- DNA
deoxyribonucleic acid
- DPI
diphenyleneiodonium
- Duox1
L dual oxidase 1
- ED
erectile dysfunction
- eNOS
endothelial nitric oxide synthase
- ERK
extracellular signal-regulated kinases
- ERK 1/2
extracellular signal-regulated kinases 1/2
- GPCR
G protein coupled receptor
- GSK-3β
glycogen synthase kinase 3
- H2O2
hydrogen peroxide
- H2S
hydrogen sulfide
- HAT
histone acetyltransferase
- HDL
high-density lipoprotein
- HSP
heat shock protein
- IP3
inositol trisphosphate
- IRT
iron-regulated transporter
- JNK
c-Jun N-terminal kinases
- LBD
ligand-binding domain
- LNCaP
cell line derived from androgen sensitive human prostate adenocarcinoma cells
- MAPK
mitogen activated protein kinase
- MEK
mitogen activated protein kinase kinase
- MMP-2
matrix metalloproteinase 2
- mRNA
messenger RNA
- NADPH
nicotinamide adenine dinucleotide phosphate
- NFAT
nuclear factor of activated T cells
- nNOS
neuronal nitric oxide synthase
- NO
nitric oxide
- Nox
nicotinamide adenine dinucleotide phosphate oxidase
- O2−
superoxide anion
- p38
p38 mitogen-activated protein kinases
- Pi
inorganic phosphate
- PGF2alpha
prostaglandin F2 alpha
- PI3K
phosphoinositide 3-kinase
- PKA
protein kinase A
- PKC
protein kinase C
- PLC
phospholipase C
- RhoA
Ras homolog gene family member A
- RNA
ribonucleic acid
- ROCK
Rho associated kinase
- ROS
reactive oxygen species
- SD
standard deviation
- SHR
spontaneously hypertensive rat
- SHRSP
spontaneously hypertensive stroke prone
- siRNA
small interfering RNA
- Src
proto-oncogene tyrosine-protein kinase
- TBP
TATA-binding protein
- TRPM8
transient receptor potential cation channel subfamily M member 8
- TRPV4
transient receptor potential cation channel subfamily V member 4
- TRT
testosterone replacement therapy
- VSMC
vascular smooth muscle cell
- WT
wild type
- WKY
Wistar Kyoto
- ZIP9
zinc transporter protein 9
- ZRT
zinc-regulated transporter
Author contribution
All authors contributed equally to this review.
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work was supported by the British Heart Foundation (BHF) [grant number RE/13/5/30177 (to A.K.L.H., R.A.-L., A.C.M. and R.M.T.)]; and a BHF Chair [grant number CH/12/4/29762 (to R.M.T.)].
References
- 1.Freeman B.M., Univers J., Fisher R.K.. et al. (2017) Testosterone replacement attenuates intimal hyperplasia development in an androgen deficient model of vascular injury. J. Surg. Res. 207, 53–62 10.1016/j.jss.2016.08.016 [DOI] [PubMed] [Google Scholar]
- 2.Comeglio P., Cellai I., Filippi S.. et al. (2016) Differential effects of testosterone and estradiol on clitoral function: an experimental study in rats. J. Sex Med. 13, 1858–1871 10.1016/j.jsxm.2016.10.007 [DOI] [PubMed] [Google Scholar]
- 3.Wu X., Gu Y. and Li L. (2017) The anti-hyperplasia, anti-oxidative and anti-inflammatory properties of Qing Ye Dan and swertiamarin in testosterone-induced benign prostatic hyperplasia in rats. Toxicol. Lett. 265, 9–16 10.1016/j.toxlet.2016.11.011 [DOI] [PubMed] [Google Scholar]
- 4.Zhang H., Shi L., Ren G.Q.. et al. (2016) Dihydrotestosterone modulates endothelial progenitor cell function via RhoA/ROCK pathway. Am. J. Transl. Res. 8, 4300–4309 [PMC free article] [PubMed] [Google Scholar]
- 5.Olsen J.R., Azeem W., Hellem M.R.. et al. (2016) Context dependent regulatory patterns of the androgen receptor and androgen receptor target genes. BMC Cancer 16, 377. 10.1186/s12885-016-2453-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toocheck C., Clister T., Shupe J.. et al. (2016) Mouse spermatogenesis requires classical and nonclassical testosterone signaling. Biol. Reprod. 94, 11. 10.1095/biolreprod.115.132068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roshan M.H., Tambo A. and Pace N.P. (2016) The role of testosterone in colorectal carcinoma: pathomechanisms and open questions. EPMA J. 7, 22. 10.1186/s13167-016-0071-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pihlajamaa P., Sahu B. and Janne O.A. (2015) Determinants of receptor- and tissue-specific actions in androgen signaling. Endocr. Rev. 36, 357–384 10.1210/er.2015-1034 [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto A.M. (2013) Testosterone administration in older men. Endocrinol. Metab. Clin. North Am. 42, 271–286 10.1016/j.ecl.2013.02.011 [DOI] [PubMed] [Google Scholar]
- 10.Werner R. and Holterhus P.M. (2014) Androgen action. Endocr. Dev. 27, 28–40 [DOI] [PubMed] [Google Scholar]
- 11.Bryce A.H. and Antonarakis E.S. (2016) Androgen receptor splice variant 7 in castration-resistant prostate cancer: clinical considerations. Int. J. Urol. 23, 646–653 10.1111/iju.13134 [DOI] [PubMed] [Google Scholar]
- 12.Zhang L., Wu S., Ruan Y.. et al. (2011) Testosterone suppresses oxidative stress via androgen receptor-independent pathway in murine cardiomyocytes. Mol. Med. Rep. 4, 1183–1188 [DOI] [PubMed] [Google Scholar]
- 13.Torres-Estay V., Carreno D.V., San Francisco I.F.. et al. (2015) Androgen receptor in human endothelial cells. J. Endocrinol. 224, R131–R137 10.1530/JOE-14-0611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopes R.A., Neves K.B., Pestana C.R.. et al. (2014) Testosterone induces apoptosis in vascular smooth muscle cells via extrinsic apoptotic pathway with mitochondria-generated reactive oxygen species involvement. Am. J. Physiol. Heart Circ. Physiol. 306, H1485–H1494 10.1152/ajpheart.00809.2013 [DOI] [PubMed] [Google Scholar]
- 15.Yu S., Xia S., Yang D.. et al. (2013) Androgen receptor in human prostate cancer-associated fibroblasts promotes prostate cancer epithelial cell growth and invasion. Med. Oncol. 30, 674. 10.1007/s12032-013-0674-9 [DOI] [PubMed] [Google Scholar]
- 16.Lai J.J., Lai K.P., Chuang K.H.. et al. (2009) Monocyte/macrophage androgen receptor suppresses cutaneous wound healing in mice by enhancing local TNF-alpha expression. J. Clin. Invest. 119, 3739–3751 10.1172/JCI39335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khetawat G., Faraday N., Nealen M.L.. et al. (2000) Human megakaryocytes and platelets contain the estrogen receptor beta and androgen receptor (AR): testosterone regulates AR expression. Blood 95, 2289–2296 [PubMed] [Google Scholar]
- 18.McCrohon J.A., Death A.K., Nakhla S.. et al. (2000) Androgen receptor expression is greater in macrophages from male than from female donors. A sex difference with implications for atherogenesis. Circulation 101, 224–226 10.1161/01.CIR.101.3.224 [DOI] [PubMed] [Google Scholar]
- 19.Liu P.Y., Death A.K. and Handelsman D.J. (2003) Androgens and cardiovascular disease. Endocr. Rev. 24, 313–340 10.1210/er.2003-0005 [DOI] [PubMed] [Google Scholar]
- 20.Wen Q., Cheng C.Y. and Liu Y.X. (2016) Development, function and fate of fetal Leydig cells. Semin. Cell Dev. Biol. 59, 89–98 10.1016/j.semcdb.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sa E.Q., Sa F.C., Guedes A.D.. et al. (2009) [Serum testosterone and cardiovascular disease in men]. Arq. Bras. Endocrinol. Metabol. 53, 915–922 10.1590/S0004-27302009000800004 [DOI] [PubMed] [Google Scholar]
- 22.Burger H.G. (2002) Androgen production in women. Fertil. Steril. 77, Suppl 4S3–S35 10.1016/S0015-0282(02)02985-0 [DOI] [PubMed] [Google Scholar]
- 23.Clark B.J. and Stocco D.M. (1996) StAR-A tissue specific acute mediator of steroidogenesis. Trends Endocrinol. Metab. 7, 227–233 10.1016/S1043-2760(96)00114-2 [DOI] [PubMed] [Google Scholar]
- 24.Winters S.J., Takahashi J. and Troen P. (1999) Secretion of testosterone and its delta4 precursor steroids into spermatic vein blood in men with varicocele-associated infertility. J. Clin. Endocrinol. Metab. 84, 997–1001 [DOI] [PubMed] [Google Scholar]
- 25.Heinlein C.A. and Chang C. (2002) The roles of androgen receptors and androgen-binding proteins in nongenomic androgen actions. Mol. Endocrinol. 16, 2181–2187 10.1210/me.2002-0070 [DOI] [PubMed] [Google Scholar]
- 26.Oettel M. (2004) The endocrine pharmacology of testosterone therapy in men. Naturwissenschaften 91, 66–76 10.1007/s00114-003-0494-4 [DOI] [PubMed] [Google Scholar]
- 27.Chignalia A.Z., Oliveira M.A., Debbas V.. et al. (2015) Testosterone induces leucocyte migration by NADPH oxidase-driven ROS- and COX2-dependent mechanisms. Clin. Sci. (Lond.) 129, 39–48 10.1042/CS20140548 [DOI] [PubMed] [Google Scholar]
- 28.Jones T.H., Arver S., Behre H.M.. et al. (2011) Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 study). Diabetes Care 34, 828–837 10.2337/dc10-1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bassil N., Alkaade S. and Morley J.E. (2009) The benefits and risks of testosterone replacement therapy: a review. Ther. Clin. Risk Manag. 5, 427–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tostes R.C., Carneiro F.S., Carvalho M.H.. et al. (2016) Reactive oxygen species: players in the cardiovascular effects of testosterone. Am. J. Physiol. Regul. Integr. Comp. Physiol. 310, R1–R14 10.1152/ajpregu.00392.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Basaria S. (2010) Androgen abuse in athletes: detection and consequences. J. Clin. Endocrinol. Metab. 95, 1533–1543 10.1210/jc.2009-1579 [DOI] [PubMed] [Google Scholar]
- 32.Bagatell C.J. and Bremner W.J. (1996) Androgens in men–uses and abuses. N. Engl. J. Med. 334, 707–714 10.1056/NEJM199603143341107 [DOI] [PubMed] [Google Scholar]
- 33.Leening M.J., Ferket B.S., Steyerberg E.W.. et al. (2014) Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ 349, g5992. 10.1136/bmj.g5992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khaw K.T., Dowsett M., Folkerd E.. et al. (2007) Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study. Circulation 116, 2694–2701 10.1161/CIRCULATIONAHA.107.719005 [DOI] [PubMed] [Google Scholar]
- 35.Malkin C.J., Pugh P.J., Morris P.D.. et al. (2010) Low serum testosterone and increased mortality in men with coronary heart disease. Heart 96, 1821–1825 10.1136/hrt.2010.195412 [DOI] [PubMed] [Google Scholar]
- 36.Zarotsky V., Huang M.Y., Carman W.. et al. (2014) Systematic literature review of the risk factors, comorbidities, and consequences of hypogonadism in men. Andrology 2, 819–834 10.1111/andr.274 [DOI] [PubMed] [Google Scholar]
- 37.English K.M., Mandour O., Steeds R.P.. et al. (2000) Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur. Heart J. 21, 890–894 10.1053/euhj.1999.1873 [DOI] [PubMed] [Google Scholar]
- 38.Hiort O. and Ahmed S.F. (2014) Understanding differences and disorders of sex development. Foreword. Endocr. Dev. 27, VII–VIII 10.1159/issn.1421-7082 [DOI] [PubMed] [Google Scholar]
- 39.Foradori C.D., Weiser M.J. and Handa R.J. (2008) Non-genomic actions of androgens. Front. Neuroendocrinol. 29, 169–181 10.1016/j.yfrne.2007.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grino P.B., Griffin J.E. and Wilson J.D. (1990) Testosterone at high concentrations interacts with the human androgen receptor similarly to dihydrotestosterone. Endocrinology 126, 1165–1172 10.1210/endo-126-2-1165 [DOI] [PubMed] [Google Scholar]
- 41.Bennett N.C., Gardiner R.A., Hooper J.D.. et al. (2010) Molecular cell biology of androgen receptor signalling. Int. J. Biochem. Cell Biol. 42, 813–827 10.1016/j.biocel.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 42.Pietri E., Conteduca V., Andreis D.. et al. (2016) Androgen receptor signaling pathways as a target for breast cancer treatment. Endocr. Relat. Cancer 23, R485–R498 10.1530/ERC-16-0190 [DOI] [PubMed] [Google Scholar]
- 43.Li J. and Al-Azzawi F. (2009) Mechanism of androgen receptor action. Maturitas 63, 142–148 10.1016/j.maturitas.2009.03.008 [DOI] [PubMed] [Google Scholar]
- 44.Nicoll R., Howard J.M. and Henein M.Y. (2015) A review of the effect of diet on cardiovascular calcification. Int. J. Mol. Sci. 16, 8861–8883 10.3390/ijms16048861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Makaryus A.N., Sison C., Kohansieh M.. et al. (2014) Implications of gender difference in coronary calcification as assessed by CT coronary angiography. Clin. Med. Insights Cardiol. 8, Suppl 451–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhu D., Hadoke P.W., Wu J.. et al. (2016) Ablation of the androgen receptor from vascular smooth muscle cells demonstrates a role for testosterone in vascular calcification. Sci. Rep. 6, 24807. 10.1038/srep24807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Son B.K., Kozaki K., Iijima K.. et al. (2007) Gas6/Axl-PI3K/Akt pathway plays a central role in the effect of statins on inorganic phosphate-induced calcification of vascular smooth muscle cells. Eur. J. Pharmacol. 556, 1–8 10.1016/j.ejphar.2006.09.070 [DOI] [PubMed] [Google Scholar]
- 48.Melaragno M.G., Cavet M.E., Yan C.. et al. (2004) Gas6 inhibits apoptosis in vascular smooth muscle: role of Axl kinase and Akt. J. Mol. Cell Cardiol. 37, 881–887 10.1016/j.yjmcc.2004.06.018 [DOI] [PubMed] [Google Scholar]
- 49.Son B.K., Akishita M., Iijima K.. et al. (2010) Androgen receptor-dependent transactivation of growth arrest-specific gene 6 mediates inhibitory effects of testosterone on vascular calcification. J. Biol. Chem. 285, 7537–7544 10.1074/jbc.M109.055087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen Y.Q., Zhao J., Jin C.W.. et al. (2016) Testosterone delays vascular smooth muscle cell senescence and inhibits collagen synthesis via the Gas6/Axl signaling pathway. Age (Dordr.) 38, 60. 10.1007/s11357-016-9910-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spada M., Kasper D., Pagliardini V.. et al. (2017) Metabolic progression to clinical phenotype in classic Fabry disease. Ital. J. Pediatr. 43, 1. 10.1186/s13052-016-0320-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shen J.S., Meng X.L., Wight-Carter M.. et al. (2015) Blocking hyperactive androgen receptor signaling ameliorates cardiac and renal hypertrophy in Fabry mice. Hum. Mol. Genet. 24, 3181–3191 10.1093/hmg/ddv070 [DOI] [PubMed] [Google Scholar]
- 53.Ikeda Y., Aihara K., Sato T.. et al. (2005) Androgen receptor gene knockout male mice exhibit impaired cardiac growth and exacerbation of angiotensin II-induced cardiac fibrosis. J. Biol. Chem. 280, 29661–29666 10.1074/jbc.M411694200 [DOI] [PubMed] [Google Scholar]
- 54.An W.F., Germain A.R., Bishop J.A., Nag P.P., Metkar S, Ketterman J.. et al. (2010) Discovery of potent and highly selective inhibitors of GSK3b. Probe reports from the NIH molecular libraries program (Internet). Ed Bethesda and the National Center for Biotechnology Information, USA [Google Scholar]
- 55.Duran J., Oyarce C., Pavez M.. et al. (2016) GSK-3beta/NFAT signaling is involved in testosterone-induced cardiac myocyte hypertrophy. PLoS One 11, e0168255. 10.1371/journal.pone.0168255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naik J.S., Osmond J.M., Walker B.R.. et al. (2016) Hydrogen sulfide-induced vasodilation mediated by endothelial TRPV4 channels. Am. J. Physiol. Heart Circ. Physiol. 311, H1437–H1444 10.1152/ajpheart.00465.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bucci M., Mirone V., Di Lorenzo A.. et al. (2009) Hydrogen sulphide is involved in testosterone vascular effect. Eur. Urol. 56, 378–383 10.1016/j.eururo.2008.05.014 [DOI] [PubMed] [Google Scholar]
- 58.Brancaleone V., Vellecco V., Matassa D.S.. et al. (2015) Crucial role of androgen receptor in vascular H2S biosynthesis induced by testosterone. Br. J. Pharmacol. 172, 1505–1515 10.1111/bph.12740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mustafa A.K., Sikka G., Gazi S.K.. et al. (2011) Hydrogen sulfide as endothelium-derived hyperpolarizing factor sulfhydrates potassium channels. Circ. Res. 109, 1259–1268 10.1161/CIRCRESAHA.111.240242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhao K., Li S., Wu L.. et al. (2014) Hydrogen sulfide represses androgen receptor transactivation by targeting at the second zinc finger module. J. Biol. Chem. 289, 20824–20835 10.1074/jbc.M114.559518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mishra, J.S. Hankins, G.D. and Kumar, S. (2016) Testosterone downregulates angiotensin II type-2 receptor via androgen receptor-mediated ERK1/2 MAP kinase pathway in rat aorta. J. Renin Angiotensin Aldosterone Syst. 17, pii: 1470320316674875 10.1177/1470320316674875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gray G.D., Smith E.R. and Davidson J.M. (1980) Hormonal regulation of penile erection in castrated male rats. Physiol. Behav. 24, 463–468 10.1016/0031-9384(80)90237-1 [DOI] [PubMed] [Google Scholar]
- 63.Mills T.M., Stopper V.S. and Wiedmeier V.T. (1994) Effects of castration and androgen replacement on the hemodynamics of penile erection in the rat. Biol. Reprod. 51, 234–238 10.1095/biolreprod51.2.234 [DOI] [PubMed] [Google Scholar]
- 64.Consensus Conference NIH. (1993) Impotence. NIH Consensus Development Panel on Impotence. J. Am. Med. Assoc. 270, 83–90 10.1001/jama.1993.03510010089036 [DOI] [PubMed] [Google Scholar]
- 65.Celik O. and Yucel S. (2013) Testosterone replacement therapy: should it be performed in erectile dysfunction?. Nephrourol. Mon. 5, 858–861 10.5812/numonthly.11523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alves-Lopes R., Neves K.B., Silva M.B., Olivon V.C., Ruginsk S.G., Antunes-Rodrigues J.. et al. (2016) Functional and structural changes in internal pudendal arteries underlie erectile dysfunction induced by androgen deprivation. Asian J. Androl., Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schultheiss D., Badalyan R., Pilatz A.. et al. (2003) Androgen and estrogen receptors in the human corpus cavernosum penis: immunohistochemical and cell culture results. World J. Urol. 21, 320–324 10.1007/s00345-003-0371-y [DOI] [PubMed] [Google Scholar]
- 68.Babica P., Zurabian R., Kumar E.R.. et al. (2016) Methoxychlor and vinclozolin induce rapid changes in intercellular and intracellular signaling in liver progenitor cells. Toxicol. Sci. 153, 174–185 10.1093/toxsci/kfw114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Losel R.M., Falkenstein E., Feuring M.. et al. (2003) Nongenomic steroid action: controversies, questions, and answers. Physiol. Rev. 83, 965–1016 10.1152/physrev.00003.2003 [DOI] [PubMed] [Google Scholar]
- 70.Kurokawa J., Kodama M., Clancy C.E.. et al. (2016) Sex hormonal regulation of cardiac ion channels in drug-induced QT syndromes. Pharmacol. Ther. 168, 23–28 10.1016/j.pharmthera.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Michels G. and Hoppe U.C. (2008) Rapid actions of androgens. Front. Neuroendocrinol. 29, 182–198 10.1016/j.yfrne.2007.08.004 [DOI] [PubMed] [Google Scholar]
- 72.Dent J.R., Fletcher D.K. and McGuigan M.R. (2012) Evidence for a non-genomic action of testosterone in skeletal muscle which may improve athletic performance: implications for the female athlete. J. Sports Sci. Med. 11, 363–370 [PMC free article] [PubMed] [Google Scholar]
- 73.Dupree K. and Dobs A. (2004) Osteopenia and male hypogonadism. Rev. Urol. 6, Suppl 6S30–S34 [PMC free article] [PubMed] [Google Scholar]
- 74.Lieberherr M. and Grosse B. (1994) Androgens increase intracellular calcium concentration and inositol 1,4,5-trisphosphate and diacylglycerol formation via a pertussis toxin-sensitive G-protein. J. Biol. Chem. 269, 7217–7223 [PubMed] [Google Scholar]
- 75.Wunderlich F., Benten W.P., Lieberherr M.. et al. (2002) Testosterone signaling in T cells and macrophages. Steroids 67, 535–538 10.1016/S0039-128X(01)00175-1 [DOI] [PubMed] [Google Scholar]
- 76.Yildirim E. and Erol K. (2011) The effects of testosterone on isolated sheep coronary artery. Anadolu Kardiyol. Derg. 11, 343–350 [DOI] [PubMed] [Google Scholar]
- 77.Podlasek C.A., Mulhall J., Davies K.. et al. (2016) Translational perspective on the role of testosterone in sexual function and dysfunction. J. Sex Med. 13, 1183–1198 10.1016/j.jsxm.2016.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yu J., Akishita M., Eto M.. et al. (2012) Src kinase-mediates androgen receptor-dependent non-genomic activation of signaling cascade leading to endothelial nitric oxide synthase. Biochem. Biophys. Res. Commun. 424, 538–543 10.1016/j.bbrc.2012.06.151 [DOI] [PubMed] [Google Scholar]
- 79.Yu J., Akishita M., Eto M.. et al. (2010) Androgen receptor-dependent activation of endothelial nitric oxide synthase in vascular endothelial cells: role of phosphatidylinositol 3-kinase/akt pathway. Endocrinology 151, 1822–1828 10.1210/en.2009-1048 [DOI] [PubMed] [Google Scholar]
- 80.Campelo A.E., Cutini P.H. and Massheimer V.L. (2012) Cellular actions of testosterone in vascular cells: mechanism independent of aromatization to estradiol. Steroids 77, 1033–1040 10.1016/j.steroids.2012.05.008 [DOI] [PubMed] [Google Scholar]
- 81.Ma R., Jiang S.S., Cheng X.M.. et al. (2009) [Testosterone at physiological level inhibits PGF2alpha-induced increase in intracellular Ca2+ in cultured vascular smooth muscle cells]. Zhonghua Nan Ke Xue 15, 326–330 [PubMed] [Google Scholar]
- 82.Francomano D., Fattorini G., Gianfrilli D.. et al. (2016) Acute endothelial response to testosterone gel administration in men with severe hypogonadism and its relationship to androgen receptor polymorphism: a pilot study. J. Endocrinol. Invest. 39, 265–271 10.1007/s40618-015-0325-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pi M., Kapoor K., Wu Y.. et al. (2015) Structural and functional evidence for testosterone activation of GPRC6A in peripheral tissues. Mol. Endocrinol. 29, 1759–1773 10.1210/me.2015-1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Clemmensen C., Smajilovic S., Wellendorph P.. et al. (2014) The GPCR, class C, group 6, subtype A (GPRC6A) receptor: from cloning to physiological function. Br. J. Pharmacol. 171, 1129–1141 10.1111/bph.12365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pi M. and Quarles L.D. (2012) Multiligand specificity and wide tissue expression of GPRC6A reveals new endocrine networks. Endocrinology 153, 2062–2069 10.1210/en.2011-2117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bulldan A., Dietze R., Shihan M.. et al. (2016) Non-classical testosterone signaling mediated through ZIP9 stimulates claudin expression and tight junction formation in Sertoli cells. Cell Signal. 28, 1075–1085 10.1016/j.cellsig.2016.04.015 [DOI] [PubMed] [Google Scholar]
- 87.Thomas P., Pang Y., Dong J.. et al. (2014) Identification and characterization of membrane androgen receptors in the ZIP9 zinc transporter subfamily: II. Role of human ZIP9 in testosterone-induced prostate and breast cancer cell apoptosis. Endocrinology 155, 4250–4265 10.1210/en.2014-1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Asuthkar S., Velpula K.K., Elustondo P.A.. et al. (2015) TRPM8 channel as a novel molecular target in androgen-regulated prostate cancer cells. Oncotarget 6, 17221–17236 10.18632/oncotarget.3948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang L. and Barritt G.J. (2004) Evidence that TRPM8 is an androgen-dependent Ca2+ channel required for the survival of prostate cancer cells. Cancer Res. 64, 8365–8373 10.1158/0008-5472.CAN-04-2146 [DOI] [PubMed] [Google Scholar]
- 90.Asuthkar S., Elustondo P.A., Demirkhanyan L.. et al. (2015) The TRPM8 protein is a testosterone receptor: I. Biochemical evidence for direct TRPM8-testosterone interactions. J. Biol. Chem. 290, 2659–2669 10.1074/jbc.M114.610824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Harno E., Edwards G., Geraghty A.R.. et al. (2008) Evidence for the presence of GPRC6A receptors in rat mesenteric arteries. Cell Calcium 44, 210–219 10.1016/j.ceca.2007.11.011 [DOI] [PubMed] [Google Scholar]
- 92.Pi M., Parrill A.L. and Quarles L.D. (2010) GPRC6A mediates the non-genomic effects of steroids. J. Biol. Chem. 285, 39953–39964 10.1074/jbc.M110.158063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Montezano A.C., Tsiropoulou S., Dulak-Lis M.. et al. (2015) Redox signaling, Nox5 and vascular remodeling in hypertension. Curr. Opin. Nephrol. Hypertens. 24, 425–433 10.1097/MNH.0000000000000153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chignalia A.Z., Schuldt E.Z., Camargo L.L.. et al. (2012) Testosterone induces vascular smooth muscle cell migration by NADPH oxidase and c-Src-dependent pathways. Hypertension 59, 1263–1271 10.1161/HYPERTENSIONAHA.111.180620 [DOI] [PubMed] [Google Scholar]
- 95.Panday A., Sahoo M.K., Osorio D.. et al. (2015) NADPH oxidases: an overview from structure to innate immunity-associated pathologies. Cell. Mol. Immunol. 12, 5–23 10.1038/cmi.2014.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ko E., Choi H., Kim B.. et al. (2014) Testosterone stimulates Duox1 activity through GPRC6A in skin keratinocytes. J. Biol. Chem. 289, 28835–28845 10.1074/jbc.M114.583450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pi M., Faber P., Ekema G.. et al. (2005) Identification of a novel extracellular cation-sensing G-protein-coupled receptor. J. Biol. Chem. 280, 40201–40209 10.1074/jbc.M505186200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pi M., Chen L., Huang M.Z.. et al. (2008) GPRC6A null mice exhibit osteopenia, feminization and metabolic syndrome. PLoS One 3, e3858. 10.1371/journal.pone.0003858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lopes R.A., Neves K.B. and Carneiro F.S. (2012) Tostes R.C.Testosterone and vascular function in aging. Front. Physiol. 3, 89. 10.3389/fphys.2012.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cheung K.K., Lau E.S., So W.Y.. et al. (2016) Low testosterone and clinical outcomes in Chinese men with type 2 diabetes mellitus - Hong Kong Diabetes Registry. Diabetes Res. Clin. Pract. 123, 97–105 10.1016/j.diabres.2016.11.012 [DOI] [PubMed] [Google Scholar]
- 101.Sonmez A., Haymana C., Bolu E.. et al. (2011) Metabolic syndrome and the effect of testosterone treatment in young men with congenital hypogonadotropic hypogonadism. Eur. J. Endocrinol. 164, 759–764 10.1530/EJE-10-0951 [DOI] [PubMed] [Google Scholar]
- 102.Gururani K., Jose J. and George P.V. (2016) Testosterone as a marker of coronary artery disease severity in middle aged males. Indian Heart J. 68, Suppl 3S16–S20 10.1016/j.ihj.2016.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Morgentaler A., Miner M.M., Caliber M.. et al. (2015) Testosterone therapy and cardiovascular risk: advances and controversies. Mayo Clin. Proc. 90, 224–251 10.1016/j.mayocp.2014.10.011 [DOI] [PubMed] [Google Scholar]
- 104.Basaria S., Coviello A.D., Travison T.G.. et al. (2010) Adverse events associated with testosterone administration. N. Engl. J. Med. 363, 109–122 10.1056/NEJMoa1000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Corona G., Maseroli E., Rastrelli G.. et al. (2014) Cardiovascular risk associated with testosterone-boosting medications: a systematic review and meta-analysis. Expert Opin. Drug Saf. 13, 1327–1351 10.1517/14740338.2014.950653 [DOI] [PubMed] [Google Scholar]
- 106.Borst S.E., Shuster J.J., Zou B.. et al. (2014) Cardiovascular risks and elevation of serum DHT vary by route of testosterone administration: a systematic review and meta-analysis. BMC Med. 12, 211. 10.1186/s12916-014-0211-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Muraleedharan V., Marsh H., Kapoor D.. et al. (2013) Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur. J. Endocrinol. 169, 725–733 10.1530/EJE-13-0321 [DOI] [PubMed] [Google Scholar]
- 108.Rech C.M., Clapauch R., de Souza M.. et al. (2016) Low testosterone levels are associated with endothelial dysfunction in oophorectomized early postmenopausal women. Eur. J. Endocrinol. 174, 297–306 10.1530/EJE-15-0878 [DOI] [PubMed] [Google Scholar]
- 109.Akishita M., Hashimoto M., Ohike Y.. et al. (2007) Low testosterone level is an independent determinant of endothelial dysfunction in men. Hypertens. Res. 30, 1029–1034 10.1291/hypres.30.1029 [DOI] [PubMed] [Google Scholar]
- 110.Bordallo J., Cantabrana B., Suarez L.. et al. (2011) Testosterone inhibits cAMP-phosphodiesterases in heart extracts from rats and increases cAMP levels in isolated left atria. Pharmacology 87, 155–160 10.1159/000324172 [DOI] [PubMed] [Google Scholar]
- 111.Nguyen C.T., Aaronson A., Morrissey R.P.. et al. (2011) Myths and truths of growth hormone and testosterone therapy in heart failure. Expert Rev. Cardiovasc. Ther. 9, 711–720 10.1586/erc.11.25 [DOI] [PubMed] [Google Scholar]
- 112.Cheetham T.C., An J.J., Jacobsen S.J., Niu F., Sidney S. and Quesenberry C.P. (2017) Van Den Eeden S.K.Association of testosterone replacement with cardiovascular outcomes among men with androgen deficiency. JAMA Intern. Med. 177, 491–499 [DOI] [PubMed] [Google Scholar]
- 113.Nettleship J.E., Jones T.H., Channer K.S.. et al. (2007) Physiological testosterone replacement therapy attenuates fatty streak formation and improves high-density lipoprotein cholesterol in the Tfm mouse: an effect that is independent of the classic androgen receptor. Circulation 116, 2427–2434 10.1161/CIRCULATIONAHA.107.708768 [DOI] [PubMed] [Google Scholar]
- 114.Nettleship J.E., Jones R.D., Channer K.S.. et al. (2009) Testosterone and coronary artery disease. Front. Horm. Res. 37, 91–107 10.1159/000176047 [DOI] [PubMed] [Google Scholar]
- 115.Saad F., Gooren L.J., Haider A.. et al. (2008) A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J. Androl. 29, 102–105 10.2164/jandrol.107.002774 [DOI] [PubMed] [Google Scholar]
- 116.Svartberg J., von Muhlen D., Mathiesen E.. et al. (2006) Low testosterone levels are associated with carotid atherosclerosis in men. J. Intern. Med. 259, 576–582 10.1111/j.1365-2796.2006.01637.x [DOI] [PubMed] [Google Scholar]
- 117.Muller M., van den Beld A.W., Bots M.L.. et al. (2004) Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation 109, 2074–2079 10.1161/01.CIR.0000125854.51637.06 [DOI] [PubMed] [Google Scholar]
- 118.Reckelhoff J.F. (2005) Sex steroids, cardiovascular disease, and hypertension: unanswered questions and some speculations. Hypertension 45, 170–174 10.1161/01.HYP.0000151825.36598.36 [DOI] [PubMed] [Google Scholar]
- 119.Reckelhoff J.F., Yanes L.L., Iliescu R.. et al. (2005) Testosterone supplementation in aging men and women: possible impact on cardiovascular-renal disease. Am. J. Physiol. Renal. Physiol. 289, F941–F948 10.1152/ajprenal.00034.2005 [DOI] [PubMed] [Google Scholar]
- 120.Quan A., Chakravarty S., Chen J.K.. et al. (2004) Androgens augment proximal tubule transport. Am. J. Physiol. Renal. Physiol. 287, F452–F459 10.1152/ajprenal.00188.2003 [DOI] [PubMed] [Google Scholar]
- 121.Fortepiani L.A. and Reckelhoff J.F. (2005) Role of oxidative stress in the sex differences in blood pressure in spontaneously hypertensive rats. J. Hypertens 23, 801–805 10.1097/01.hjh.0000163149.05083.13 [DOI] [PubMed] [Google Scholar]
- 122.Choobineh H., Sadighi Gilani M.A., Pasalar P.. et al. (2016) The effects of testosterone on oxidative stress markers in mice with spinal cord injuries. Int. J. Fertil. Steril. 10, 87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Christakou C.D. and Diamanti-Kandarakis E. (2008) Role of androgen excess on metabolic aberrations and cardiovascular risk in women with polycystic ovary syndrome. Womens Health (Lond.) 4, 583–594 10.2217/17455057.4.6.583 [DOI] [PubMed] [Google Scholar]
- 124.de Groot P.C., Dekkers O.M., Romijn J.A.. et al. (2011) PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum. Reprod. Update 17, 495–500 10.1093/humupd/dmr001 [DOI] [PubMed] [Google Scholar]
- 125.Page-Wilson G., Goulart A.C. and Rexrode K.M. (2009) Interrelation between sex hormones and plasma sex hormone-binding globulin and hemoglobin A1c in healthy postmenopausal women. Metab. Syndr. Relat. Disord. 7, 249–254 10.1089/met.2008.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Eendebak R.J., Huhtaniemi I.T., Pye S.R.. et al. (2016) The androgen receptor gene CAG repeat in relation to 4-year changes in androgen-sensitive endpoints in community-dwelling older European men. Eur. J. Endocrinol. 175, 583–593 10.1530/EJE-16-0447 [DOI] [PubMed] [Google Scholar]
- 127.Tirabassi G., Cignarelli A., Perrini S.. et al. (2015) Influence of CAG repeat polymorphism on the targets of testosterone action. Int. J. Endocrinol. 2015, 298107. 10.1155/2015/298107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pi M., Parrill A.L. and Quarles L.D. (2010) GPRC6A mediates the non-genomic effects of steroids. J. Biol. Chem. 285, 39953–39964 10.1074/jbc.M110.158063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chignalia A.Z., Schuldt E.Z., Camargo L.L.. et al. (2012) Testosterone induces vascular smooth muscle cell migration by NADPH oxidase and c-Src-dependent pathways. Hypertension 59, 1263–1271 10.1161/HYPERTENSIONAHA.111.180620 [DOI] [PubMed] [Google Scholar]