Abstract
In the United States in 2013, nearly 500,000 bicyclists were injured and required emergency department care. The objectives of this study were to describe the types of injuries which urban bicyclists sustain, to analyze the number and type of surgeries required, and to better delineate the services providing care. This is an observational study of injured bicyclists presenting to a Level I trauma center between February 2012 and August 2014. Most data were collected within 24 hours of injury and included demographics, narrative description of the incident, results of initial imaging studies, Injury Severity Score, admission status, length of stay, surgical procedure, and admitting and discharging service. A total of 706 injured bicyclists were included in the study, and 187 bicyclists (26.4%) required hospital admission. Of those admitted, 69 (36.8%) required surgery. There was no difference in gender between those who required surgery and those who did not (P = 0.781). Those who required surgery were older (mean age 39.1 vs 34.1, P = 0.003). Patients requiring surgery had higher Abbreviated Injury Scores for head (P ≤ 0.001), face (P ≤ 0.001), abdomen (P = 0.012), and extremity (P ≤ 0.001) and higher mean Injury Severity Scores (12.6 vs 3.7, P < 0.001). Sixty-nine patients required surgery and were brought to the operating room 82 times for 89 distinct procedures. Lower extremity injuries were the reason for 43 (48.3%) procedures, upper extremity injuries for 14 (15.7%), and facial injuries for 15 (16.9%). Orthopedic surgery performed 50 (56.2%) procedures, followed by plastic surgery (15 procedures; 16.8%). Trauma surgeons performed five (5.6%) procedures in four patients. The majority of admitted patients were admitted and discharged by the trauma service (70.1%, 56.7%, respectively) followed by the orthopedics service (13.9%, 19.8%, respectively). Injured bicyclists represent a unique subset of trauma patients. Orthopedic surgeons are most commonly involved in their operative management and rarely are the operative skills of a general traumatologist required. From a resource perspective, it is more efficient to direct the inpatient care of bicyclists with single-system trauma to the appropriate surgical subspecialty service soon after appropriate initial evaluation and treatment by the trauma service.
In the united states in 2013, an estimated 494,430 bicyclists required emergency department care due to injury; 800 bicyclists died that year as a result of trauma.1 A variety of injuries contribute to hospital admission and determine the need for surgery. Pedacyclist deaths accounted for 2 per cent of all motor vehicle traffic fatalities in 2013. The majority of these fatalities occurred in urban areas (68%).2 In New York City in 2013, there were 3884 bicyclist collisions with motor vehicles, resulting in 12 fatalities.3
Although there are a number of case series describing handlebar injuries in the pediatric population, data on injuries sustained by the adult bicyclist community and the subsequent surgeries required are more limited and less detailed.4, 5 In addition, there is little data as to the distribution of these cases among the various surgical services.
Our hypothesis was that the majority of injuries sustained by bicyclists are bony fractures requiring primarily orthopedic surgical procedures and postoperative management. The objectives of this study were to describe the types of injuries that urban bicyclists sustain, to analyze the number and type of surgeries required, and to better delineate the surgical services providing that care.
Material and Methods
This study was an observational study of injured bicyclists presenting to Bellevue Hospital Center (BHC). BHC is a Level I regional trauma center whose primary catchment area is southern Manhattan and western Brooklyn. Data collection was performed at BHC between February 1, 2012 and August 31, 2014, excluding a three-month interruption (October 29, 2012 through February 7, 2013), when clinical services were interrupted due to Hurricane Sandy.
Most data were collected within 24 hours of injury for all bicyclists presenting to the BHC Emergency Department (ED). The study included both admitted and nonadmitted patients. Collected variables included demographics, narrative description of the incident, results of initial FAST (focused assessment with sonography in trauma) and CT imaging studies, Abbreviated Injury Score (AIS), Injury Severity Score (ISS), admission status, hospital length of stay (LOS), surgical procedure, disposition, and mortality. Admitting and discharging services of record were also identified. For all injuries requiring operative intervention, the procedures performed and the surgical services involved were recorded. Bedside tracheostomies and percutaneous endoscopic gastrostomies were excluded from the list of operative procedures.
The details of the incident were elicited from patients when they were alert and able to answer questions. Verbal informed consent was obtained prior to study inclusion. Injuries were recorded and AIS and ISS variables were calculated after official radiology imaging reports were finalized. Hospital LOS, surgery, and disposition data were gathered from the electronic medical record.
Data were analyzed using STATA version 13.0 statistical software (StataCorp LP, College Station, TX). When applicable, Pearson’s chi-squared, Fischer’s exact, or independent Student’s t tests were performed, with P < 0.05 representing statistical significance. Both the New York University School of Medicine and the BHC institutional review boards approved this study. Funding was provided by a Highway Safety Grant from the State of New York Governor’s Traffic Safety Committee.
Results
A total of 706 injured bicyclists were evaluated at BHC during the study period. Five hundred and thirteen patients (72.6%) were treated and released from the ED, while 187 bicyclists (26.4%) were admitted (Table 1). Of the 513 treated and released, 425 (82.8%) were brought in by emergency medical services, while 185 (97.8%) of those requiring admission were brought in by emergency medical services. Of those admitted, 69 (36.8%) required surgery.
Table 1.
Demographics, Mechanisms of Injury, Imaging Studies, and Injury Scores of Bicyclists
| Categories | Surgery (n = 69) | No Surgery (n = 637) | P |
|---|---|---|---|
| Gender | |||
| Male | 56 (81.2) | 508 (79.7) | 0.781 |
| Age | |||
| Mean (SD) | 39.1 (16.3) | 34.1 (13.5) | 0.003 |
| Min, max | 6, 82 | 3, 78 | |
| <18 | 1 (1.4) | 39 (6.1) | 0.002 |
| 18–64 years old | 60 (87.0) | 580 (91.1) | |
| ≥65 | 8 (11.6) | 18 (2.8) | |
| Incident description* | |||
| Versus pedestrian | 1 (1.4) | 27 (4.3) | 0.484 |
| Versus other cyclist | 1 (1.4) | 28 (4.4) | |
| Versus motor vehicle | 44 (63.8) | 405 (64.0) | |
| Fall from bike | 22 (31.9) | 167 (26.4) | |
| Other | 1 (1.4) | 9 (0.9) | |
| FAST results† | |||
| Negative | 44 (69.8) | 285 (48.0) | 0.002 |
| Positive | 1 (1.6) | 2 (0.3) | |
| Equivocal | 0 (0) | 4 (0.7) | |
| Not performed | 18 (28.6) | 303 (51.0) | |
| Head CT performed | 36 (52.2) | 304 (47.7) | 0.482 |
| C-spine performed | 39 (56.5) | 269 (42.2) | 0.023 |
| Chest CT performed | 20 (29.0) | 83 (13.0) | <0.001 |
| Abdomen/pelvis CT performed | 27 (39.1) | 95 (14.9) | <0.001 |
| Admission status | |||
| Admitted | 69 (100.0) | 118 (18.5) | <0.001 |
| Discharged | 0 (0) | 518 (81.3) | |
| Died in ED | 0 (0) | 1 (0.2) | |
| Head AIS | |||
| AIS = 0 | 53 (76.8) | 585 (91.8) | <0.001 |
| AIS ≥ 1 | 16 (23.2) | 52 (8.2) | |
| Face AIS | |||
| AIS = 0 | 45 (65.2) | 559 (87.8) | <0.001 |
| AIS ≥ 1 | 24 (34.8) | 78 (12.2) | |
| Chest AIS | |||
| AIS = 0 | 65 (94.2) | 617 (96.9) | 0.281 |
| AIS ≥ 1 | 4 (5.8) | 20 (3.1) | |
| Abdominal AIS | |||
| AIS = 0 | 63 (91.3) | 622 (97.6) | 0.012 |
| AIS ≥ 1 | 6 (8.7) | 15 (2.4) | |
| Extremity AIS | |||
| AIS = 0 | 22 (31.9) | 497 (78.0) | <0.001 |
| AIS ≥ 1 | 47 (68.1) | 140 (22.0) | |
| External AIS | |||
| AIS = 0 | 8 (11.6) | 85 (13.3) | 0.851 |
| AIS ≥ 1 | 61 (88.4) | 552 (86.7) | |
| ISS | |||
| Mean (SD) | 12.6 (9.0) | 3.7 (5.8) | <0.001 |
| Min, max | 1, 45 | 0, 50 | |
| No injuries, 0 | 0 (0) | 57 (8.9) | <0.001 |
| 1–8 | 18 (26.1) | 481 (75.5) | |
| 9–15 | 36 (52.2) | 69 (10.8) | |
| 16–24 | 5 (7.2) | 19 (3.0) | |
| ≥25 | 10 (14.5) | 11 (1.7) | |
| Hospital length of stay‡ | |||
| Mean (SD) | 8.09 (11.52) | 3.21 (5.84) | <0.001 |
| Min, max | 1, 66 | 0,38 | |
| Median | 4 | 1 | |
| Died | 0 (0) | 3 (0.5) | 1.000 |
| Disposition | |||
| Home | 55 (79.7) | 619 (97.2) | <0.001 |
| Rehab | 14 (20.3) | 10 (1.6) | |
| Other | 0 (0) | 8 (1.3) | |
SD, standard deviation; C-spine, cervical-spine; AIS, anatomic injury severity; min, minimum; max, maximum.
Four unknowns removed from the “no surgery” column.
Forty-three unknowns removed from “no surgery” column, six unknowns removed from “surgery” column.
Only includes those who were admitted, surgery, n = 69; non surgery, n = 118.
There was no difference in gender composition between those who required surgery and those who did not (P =0.781) (Table 1). Those who required surgery were older with a mean age of 39.1 years (vs 34.1 years, P = 0.003); 11.6 per cent were 65 years of age or older. There was no difference in injury mechanism between the two groups (P = 0.484). Those who required surgery were more likely to have a FAST examination (P = 0.002) and CT imaging studies of the C-spine, chest, and abdomen/pelvis (P = 0.023, P ≤ <0.001, P ≤ 0.001, respectively). Patients requiring surgery had higher AIS scores for head (P ≤ 0.001), face (P ≤ 0.001), abdomen (P =0.012), and extremity (P ≤ 0.001) categories and higher mean ISS (12.6 vs 3.7, P < 0.001). Of admitted patients, those requiring surgery had longer mean LOS (8.1 vs 3.2 days, P < 0.001) and were more likely to require intensive care unit admission (20.3% vs 3.0%, P < 0.001.)
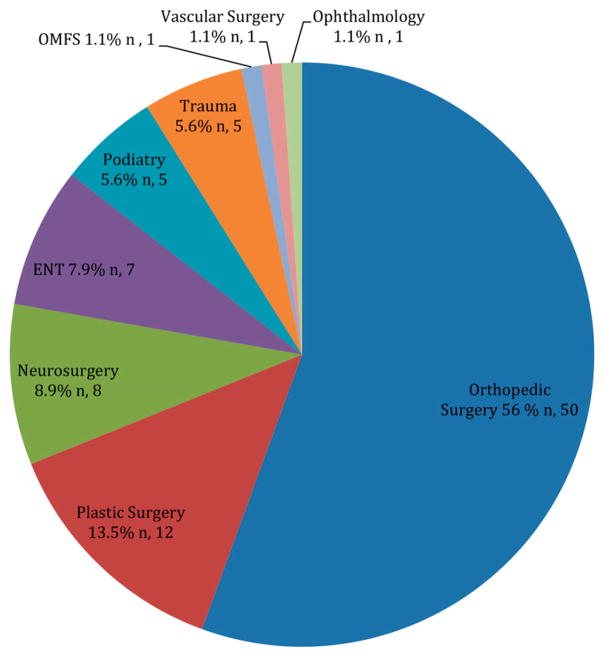
A total of 69 patients required surgery and were brought to the operating room 82 times for 89 distinct procedures (Table 2). Anatomically, lower extremity injuries were the reason for 43 (48.3%) procedures, upper extremity injuries for 14 (15.7%) procedures, and facial injuries for 15 (16.9%) procedures. Orthopedic surgery performed 50 (56.2%) of the procedures, followed by plastic surgery, which performed 15 procedures (16.8%) (Fig. 1). Fourteen of the orthopedic procedures involved the femur whereas 12 involved the tibia. Trauma surgeons performed five (5.6%) operative procedures in four patients: three exploratory laparotomies, one bilateral gluteal fasciotomy, and one upper extremity wound exploration and repair.
Table 2.
Number of Surgical Procedures Which Injured Bicyclists Required by Anatomic Region and Service
| Anatomic Region | Total Number of Procedures (n = 89) | Service |
|---|---|---|
| Head | 7 | Neurosurgery |
| Spine | 1 | Neurosurgery |
| Face | 15 | Plastics, OMFS, ENT, ophthalmology |
| Chest | 1 | Vascular surgery |
| Abdomen | 3 | Trauma |
| Pelvis/acetabulum | 5 | Ortho, trauma |
| Upper extremity | 14 | |
| Clavicle | 1 | Ortho |
| Upper arm | 3 | Ortho, trauma |
| Elbow | 2 | Ortho |
| Ortho | ||
| Radius | 2 | Ortho |
| Radius + ulnar | 4 | Ortho |
| Hand | 2 | Ortho, plastics |
| Lower extremity | 43 | |
| Femur | ||
| Femoral neck | 5 | Ortho |
| Femoral shaft | 5 | Ortho |
| Intertrochanteric | 4 | Ortho |
| Knee | 2 | Ortho |
| General lower extremity | 5 | Ortho, plastics |
| Tibia | 12 | Ortho |
| Ankle | 4 | Ortho |
| Foot | 6 | Podiatry, plastics |
Fig. 1.
The specialty services that performed surgery on injured bicyclists. ENT, ear, nose, and throat.
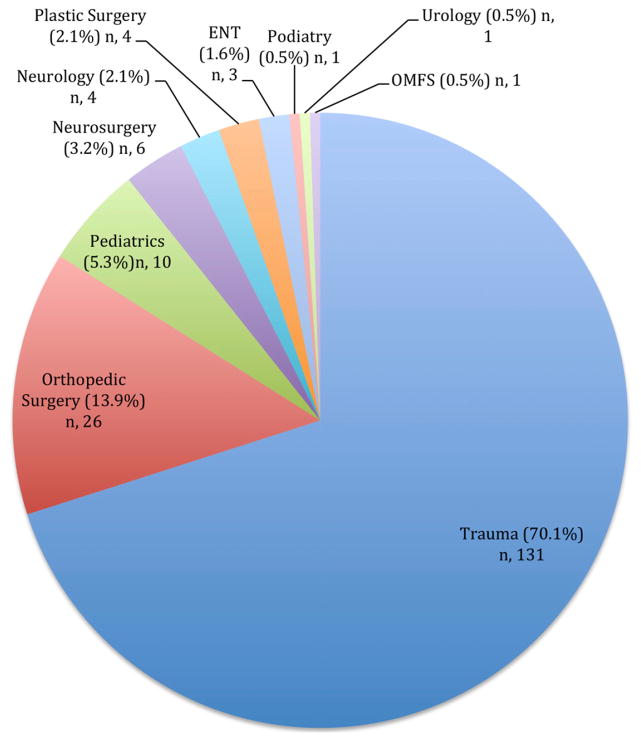
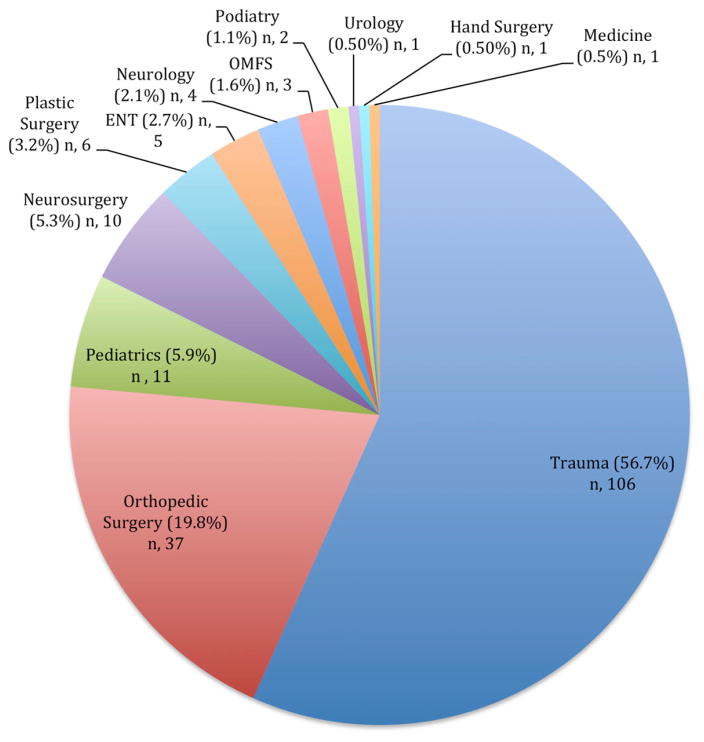
The majority of admitted patients were admitted by the trauma surgery service (70.1%) followed by the orthopedic surgery service (13.9%) (Fig. 2). The majority of patients were discharged from the hospital from the trauma surgery service (56.7%), followed by the orthopedic surgery service (19.8%) (Fig. 3).
Fig. 2.
The specialty services to which injured bicyclists were admitted. ENT, ear, nose, and throat.
Fig. 3.
The specialty services from which injured bicyclists were discharged. ENT, ear, nose, and throat.
Discussion
Injured bicyclists represent a unique subset of blunt trauma patients. Perhaps the most significant distinction between bicyclist injuries and pedestrian injuries by motor vehicles is the body region involved. A study of 203 nonfatal collisions in northern Sweden demonstrated that pedestrians experienced more severe injuries of the head and neck (38%), thorax (40%), and abdomen/pelvis (50%), while bicyclists sustained more major extremity injuries (70%).6
Multiple factors determine which patients require admission. An epidemiologic study by Rivara et al.7 demonstrated that the most important predictor of admission to the hospital was injury severity, as measured by ISS greater than eight. Age is an important contributor to injury severity and subsequent admission. Kroyer8 showed an increase in fatality proportions for struck bicyclists beginning in the 45 to 54 age group. Scheiman et al.9 studied older adults over 65 years of age and showed a 34 per cent admission rate, two times that of patients under 65 years of age. As per Rivara et al., other significant risk factors for admission were male gender, age under 12 years, and self-reported speed under 15 mph.
Our study’s aim was to look beyond admission statistics and determine risk factors for surgical need. There is little in the literature describing the qualities of injured bicyclists who require surgery. Overall, 9.8 per cent of our patient population required surgery, representing over a third of admitted patients. Those requiring surgery were older, although injury mechanisms did not play a role; collisions with motor vehicles did not contribute to a greater proportion of patients requiring surgery. Rivara et al. showed that collision with a motor vehicle increases the risk of severe injury by 3.6-fold but did not delineate surgical need.
As mentioned, the most common region requiring surgery after bicyclist injury is the lower extremity. Our population’s injury pattern is consistent with the literature, across many different patient populations. Rosenkranz and Sheridan10 studied 222 admitted adult injured bicyclists and found that 174 sustained orthopedic fractures while 78 had facial fractures. In a study by Selbst et al.11 of children seen in the ED with bicycle injuries, 33 per cent of injuries were to the lower extremity, 31 per cent to the head and neck, and 21 per cent to the upper extremities.
In our study, orthopedic surgeons represented the surgical specialists whose services were most frequently required in the operative care of injured bicyclists representing over half of all surgeries performed. The most common site of fracture requiring surgical fixation was the femur, followed by the tibia. In the national database study by Lustenberger et al.,12 which listed the injuries sustained in bicycle accidents, regardless of intervention, the lower leg (i.e., tibia/fibula) was the most commonly fractured location (13.8% of all bicycle-related injuries) followed by the femur (7.7%). A study by Karbakhsh-Davari13 et al., which looked at injured bicyclists requiring more than 24 hours admission in a hospital found that of 170 patients, 86 (50.6%) required surgery. Of those requiring surgery, 40.7 per cent underwent closed reduction without internal fixation and 39.5 per cent underwent open reduction and internal fixation. Scheiman’s9 study of injured bicyclists over 65 found that 38.5 per cent had fractures: 51 per cent were upper extremity, 19.6 per cent were upper leg and hip, and 13.8 per cent were knee and lower leg. Muthucumaru et al.5 studied 196 children admitted for bicycle injuries and found that 33.2 per cent had upper extremity fractures, whereas 5.6 per cent had lower extremity fractures. This also may explain why the Scheiman study had a high percentage of upper extremity injuries as it included patients regardless of emergency room disposition.
Facial fractures and associated injuries were common and required a variety of subspecialty services, including otolaryngology, oromaxillofacial surgery (OMFS), plastic surgery, and ophthalmology. A study by Boffano et al.,14 which looked at maxillofacial injuries in the Netherlands over 10 years found that 11.4 per cent of OMFS fractures were secondary to bicycle-related injuries, and that orthopedic injuries were the most common concomitant injury in this setting. Yamamoto et al.15 broke down bicycling-related maxillofacial fractures and found that the most common fracture location was the mandible, followed by the midface. Similar to the Boffano study, 23 per cent of these patients required orthopedic follow-up for concomitant injuries. Among their patient population of 305 patients with 307 facial fractures, 23.1 per cent required open reduction, while 26.4 per cent required maxillo-mandibular fixation.
Considering that the majority of injuries sustained by bicyclists in our study involved the extremities and face, as opposed to the abdomen or chest, it is not surprising that the operative role of the general traumatologist is exceedingly small. In our study, only five patients required general trauma surgery for operative care of acute injuries; of these, only three represented exploratory laparotomies (one of which was negative), while two were skin and soft tissue procedures. These findings are consistent with the literature. In the Karbakhsh-Davari13 study, two of the 86 patients requiring surgery were operated on by general traumatologists. Lustenberger et al.12 looked at 12,429 injured bicyclists in the national trauma database and found that while 34.9 per cent had extremity fractures, only 6.6 per cent had intra-abdominal injuries.
In our study, the great majority of patients who were admitted were placed on the trauma service. Although many were triaged to other subspecialties, most were still under the care of the trauma service at the time of discharge. The role of the traumatologist in the care of the injured bicyclist is predominantly a non-operative one, providing the initial assessment and care and subsequently serving as care coordinator alongside the subspecialists. From a resource perspective, it may be more efficient to direct the in-patient care of patients with single-system trauma to the appropriate surgical subspecialty service soon after appropriate initial evaluation and treatment by the trauma service. More complex injured patients, including the elderly, or those with multisystem trauma should remain on the trauma service as they may benefit from the traumatologist’s expertise. This study was not designed to compare outcomes between service-specific admissions.
This study has several strengths. Data were collected prospectively and the dataset captured all injured bicyclists, regardless of admission status. The study took place in an urban environment, as do the majority of bicycle collisions in the United States.
There are several limitations to the study. This study only includes bicyclists who were injured within the catchment area of BHC, and therefore represents only a single institution’s experience. Our data are not generalizable to injured bicyclists in other areas of NYC. Our population is also limited to those who were injured enough to require hospital care, and excludes those who were injured but did not seek ED evaluation and those declared dead at the scene. In addition, the in-house operative management and service designation represent the routine and protocols of a single hospital. Although this study may comment on resource utilization, it was not designed to address outcome differences based on admitting service.
Conclusions
Injured bicyclists represent a unique subset of trauma patients who sustain predominantly lower extremity fractures followed by upper extremity and facial bony injuries. Most patients with bicycle injuries are admitted to the trauma surgery service, although orthopedic surgeons are most commonly involved in the operative management and only rarely are the operative skills of a general traumatologist required. Likely, effective inpatient resource utilization would be aided by admitting single-system injured bicyclists directly to operative surgical subspecialty services once cleared by a traumatologist.
Acknowledgments
The State of New York Governor’s Traffic Safety Committee provided funding support.
References
- 1.Centers for Disease Control and Prevention. [Accessed July 11, 2015];Web-based Injury Statistics Query and Reporting System (WISQARS) Available at: http://www.cdc.gov/injury/wisqars/
- 2. [Accessed July 11, 2015];Traffic Safety Facts Data. 2013 Available at: http://www.nrd.nhtsa.dot.gov/Pubs/812151.pdf.
- 3. [Accessed February 9, 2016];Bicycle Crash Data. 2013 Available at: http://www.nyc.gov/html/dot/downloads/pdf/2013-bicycle-crash-data-report.pdf.
- 4.Karaman I, Karaman A, Aslan M, et al. A hidden danger of childhood trauma: bicycle handlebar injuries. Surg Today. 2009;39:572–4. doi: 10.1007/s00595-008-3931-3. [DOI] [PubMed] [Google Scholar]
- 5.Muthucumaru M, Keys C, Kimber C, et al. Trend of severe abdominal injuries from bicycle accidents in children: a preventable condition. J Paediatr Child Health. 2011;48:259–62. doi: 10.1111/j.1440-1754.2011.02233.x. [DOI] [PubMed] [Google Scholar]
- 6.Oman M, Fredriksson R, Bylund P, et al. Analysis of the mechanism of injury in non-fatal vehicle-to-pedestrian and vehicle-to-bicyclist frontal crashes in Sweden. Int J Inj Contr Saf Promot. 2015;23:405–12. doi: 10.1080/17457300.2015.1047869. [DOI] [PubMed] [Google Scholar]
- 7.Rivara F, Thompson D, Thompson R. Epidemiology of bicycle injuries and risk factors for serious injury. Inj Prev. 2015;21:47–51. doi: 10.1136/injprev-00002-0038rep. [DOI] [PubMed] [Google Scholar]
- 8.Kröyer H. The relation between speed environment, age and injury outcome for bicyclists struck by a motorized vehicle—a comparison with pedestrians. Accid Anal Prev. 2015;76:57–63. doi: 10.1016/j.aap.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 9.Scheiman S, Moghaddas H, Björnstig U, et al. Bicycle injury events among older adults in Northern Sweden: a 10-year population based study. Accid Anal Prev. 2010;42:758–63. doi: 10.1016/j.aap.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Rosenkranz K, Sheridan R. Trauma to adult bicyclists: a growing problem in the urban environment. Injury. 2003;34:825–9. doi: 10.1016/s0020-1383(02)00389-3. [DOI] [PubMed] [Google Scholar]
- 11.Selbst S, Alexander D, Ruddy R. Bicycle-related injuries. Am J Dis Child. 1987;141:140–4. doi: 10.1001/archpedi.1987.04460020030021. [DOI] [PubMed] [Google Scholar]
- 12.Lustenberger T, Inaba K, Talving P, et al. Bicyclists injured by automobiles: relationship of age to injury type and severity—a national trauma database analysis. J Trauma. 2010;69:1120–5. doi: 10.1097/TA.0b013e3181d0f68b. [DOI] [PubMed] [Google Scholar]
- 13.Karbakhsh-Davari M, Khaji A, Salimi J. Bicycle-related injuries in Tehran. Arch Iran Med. 2008;11:94–7. [PubMed] [Google Scholar]
- 14.Boffano P, Roccia F, Gallesio C, et al. Bicycle-related maxillofacial injuries: a double-center study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:275–80. doi: 10.1016/j.oooo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto K, Matsusue Y, Horita S, et al. Maxillofacial fractures sustained in bicycle accidents. J Oral Maxillofac Surg. 2011;69:155–60. doi: 10.1016/j.joms.2010.12.028. [DOI] [PubMed] [Google Scholar]