Abstract
Context:
The effect of unilateral cryotherapy-facilitated rehabilitation exercise on involved-limb quadriceps function and limb symmetry in individuals with quadriceps dysfunction after anterior cruciate ligament reconstruction (ACLR) remains unclear.
Objective:
To measure the effect of a 2-week unilateral cryotherapy-facilitated quadriceps-strengthening program on knee-extension strength and quadriceps central activation ratio (CAR) in participants with ACLR.
Design:
Controlled laboratory study.
Setting:
Laboratory.
Patients or Other Participants:
A total of 10 volunteers with unilateral ACLR (1 man, 9 women; age = 21.0 ± 2.8 years, height = 164.6 ± 5.0 cm, mass = 64.0 ± 6.1 kg, body mass index = 23.7 ± 2.7 kg/m2) and 10 healthy volunteers serving as control participants (1 man, 9 women; age = 20.8 ± 2.5 years, height = 169.1 ± 6.2 cm, mass = 61.1 ± 6.4 kg, body mass index = 21.4 ± 2.3 kg/m2) participated.
Intervention(s):
Participants with ACLR completed a 2-week unilateral cryotherapy-facilitated quadriceps-strengthening intervention.
Main Outcome Measure(s):
Bilateral normalized knee-extension maximal voluntary isometric contraction (MVIC) torque (Nm/kg) and quadriceps CAR (%) were assessed preintervention and postintervention. Limb symmetry index (LSI) was calculated at preintervention and postintervention testing. Preintervention between-groups differences in unilateral quadriceps function and LSI were evaluated using independent-samples t tests. Preintervention-to-postintervention differences in quadriceps function were evaluated using paired-samples t tests. Cohen d effect sizes (95% confidence interval [CI]) were calculated for each comparison.
Results:
Preintervention between-groups comparisons revealed less knee-extension MVIC torque and quadriceps CAR for the ACLR limb (MVIC: P = .01, Cohen d = −1.31 [95% CI = −2.28, −0.34]; CAR: P = .004, Cohen d = −1.48 [95% CI = −2.47, −0.49]) and uninvolved limb (MVIC: P = .03, Cohen d = −1.05 [95% CI = −1.99, −0.11]; CAR: P = .01, Cohen d = −1.27 [95% CI = −2.23, −0.31]) but not for the LSI (MVIC: P = .46, Cohen d = −0.34 [95% CI = −1.22, 0.54]; CAR: P = .60, Cohen d = 0.24 [95% CI = −0.64, 1.12]). In the ACLR group, participants had improved knee-extension MVIC torque in the involved limb (P = .04, Cohen d = 0.32 [95% CI = −0.56, 1.20]) and uninvolved limb (P = .03, Cohen d = 0.29 [95% CI = −0.59, 1.17]); however, the improvement in quadriceps CAR was limited to the involved limb (P = .02, Cohen d = 1.16 [95% CI = 0.21, 2.11]). We observed no change in the LSI with the intervention for knee-extension MVIC torque (P = .74, Cohen d = 0.09 [95% CI = −0.79, 0.97]) or quadriceps CAR (P = .61, Cohen d = 0.26 [95% CI = −0.62, 1.14]).
Conclusions:
Two weeks of cryotherapy-facilitated exercise may improve involved-limb quadriceps function while preserving between-limbs symmetry in patients with a history of ACLR.
Key Words: disinhibitory modalities, quadriceps strength, quadriceps central activation ratio, limb symmetry index, cross-education
Key Points
A 2-week cryotherapy-facilitated strengthening program may improve involved-limb quadriceps function and preserve between-limbs symmetry in patients with a history of anterior cruciate ligament reconstruction.
Clinicians should consider using this approach when treating patients with persistent quadriceps weakness during recovery from anterior cruciate ligament reconstruction.
Quadriceps weakness and activation failure commonly persist beyond the return to physical activity after anterior cruciate ligament reconstruction (ACLR) because of a number of underlying factors, including muscle atrophy1 and persistent muscle inhibition.2 Despite this concerning clinical finding, many individuals successfully return to recreational and competitive physical activity after ACLR.3,4 Unfortunately, whereas functional status may not be affected by persistent quadriceps dysfunction (weakness and activation failure), individuals who return to physical activity are more likely to experience a subsequent traumatic knee injury within the first 5 years,5,6 as well as symptoms or radiographic evidence of osteoarthritis within the first 2 decades after ACLR.7 Suboptimal quadriceps function after ACLR has been consistently shown to be related to a variety of lower extremity kinematic8 and kinetic variables,8,9 reduced overall movement quality,10 and poor patient-reported knee function after ACLR.11 The relationship among quadriceps dysfunction, altered lower extremity movement patterns, and poor patient-reported outcomes may help to describe a potential rationale for the alarming rates of reduced quality of life,12 subsequent knee-joint injury,6 and long-term joint degeneration after ACLR.10
Limb symmetry has been consistently identified as an important clinical indicator of optimal lower extremity function when applied to muscle strength, functional performance, and lower extremity biomechanics.2,13,14 Measures such as the limb symmetry index (LSI) provide clinicians and researchers with a straightforward way of assessing impairments and improvements in functional measures, especially when preinjury or normative information is unavailable. Using the uninjured or contralateral limb for comparison can give a within-patient or within-participant guide to what may be considered normal levels of function14; however, these measures may be biased because unilateral joint trauma can negatively affect the contralateral or uninvolved side despite the lack of structural damage.15 This phenomenon is clinically important because it indicates that the contralateral or uninvolved limb may not be a valid surrogate for preinjury or optimal muscle function. Instead, researchers15−17 recently highlighted the importance of promoting unilateral strength in the involved limb while maintaining limb symmetry throughout rehabilitation.
Several intervention strategies have been suggested to successfully treat persistent quadriceps dysfunction after ACLR. Whereas these strategies are diverse, investigators have provided strong support for using disinhibitory modalities,18 such as cryotherapy,19 transcutaneous electrical nerve stimulation,20 and neuromuscular electrical stimulation,17 in conjunction with quadriceps-strengthening exercises to optimize rehabilitation outcomes. Theoretically, using disinhibitory modalities enables the clinician to treat the underlying source of muscle dysfunction at the level of the central nervous system. Addressing the underlying source of inhibition using a disinhibitory modality may provide a short treatment window (30−90 minutes21−24) during a rehabilitation session throughout which the effect of rehabilitation-based strengthening exercises on quadriceps function may be maximized.18,25 This strategy has been shown to induce clinically meaningful improvements in knee-extension strength,19,26 quadriceps activation,19,26 and lower extremity biomechanics17 over 2- to 4-week interventions; however, the effect of this intervention style on limb symmetry in quadriceps function among individuals with a history of ACLR has not been established. Researchers have clearly shown a positive contralateral effect, known as a crossover effect, of involved or uninvolved limb strength or functional status among healthy individuals,16 as well as those with a history of knee-joint injury.20,27 Despite this information, it remains unclear if using a disinhibitory modality, such as cryotherapy, would amplify the crossover effect and promote improvements in involved-limb quadriceps function while maintaining optimal limb symmetry in those experiencing persistent quadriceps dysfunction after ACLR. Therefore, the primary purpose of our study was to measure the effect of a 2-week, unilateral, cryotherapy-facilitated quadriceps-strengthening program on between-limbs symmetry of knee-extension strength and quadriceps central activation ratio (CAR) in participants with ACLR. We hypothesized that, whereas involved- and uninvolved-limb quadriceps function would improve over the intervention, limb symmetry would not change. The secondary purpose of our study was to compare unilateral measures of quadriceps CAR and knee-extension strength and limb symmetry preintervention between those with ACLR and healthy matched control participants. We hypothesized that, whereas limb symmetry would not differ between groups, the involved and uninvolved limbs of participants with ACLR would have less knee-extension strength and a lower quadriceps CAR than control participants.
METHODS
Participants
Ten participants with a history of ACLR and 10 healthy matched individuals serving as control participants enrolled in this study. Participants were matched based on sex, age (±1 year), and physical activity level (Tegner Activity Scale ± 1 level). Volunteers were included if they were considered physically active as defined by Garber et al,28 free of gross functional limitation, and free of substantial knee-joint pain (visual analog scale [VAS] ≤1.0 cm) that would prohibit them from completing a strength assessment. Participants were included in the ACLR group if they had a history of primary, unilateral ACLR after which they had been cleared by a medical professional to return to unrestricted physical activity. We recruited volunteers from a university community; therefore, we used no consistent criteria for clearance across the ACLR group. In addition, no participant had either a substantial lower extremity injury (excluding the anterior cruciate ligament injury) that resulted in altered functional status for 12 months before testing or a history of lower extremity surgery, excluding the ACLR. Demographic information for both groups is provided in Table 1. All assessments were completed over a period of no more than 20 days. All participants provided written consent, and the study was approved by the University of Miami Institutional Review Board for Medical Sciences.
Table 1. .
Participant Demographics and Knee-Related Function
| Characteristic |
Group |
t18 Value |
P Value |
|
| Anterior Cruciate Ligament Reconstruction (n = 10) |
Control (n = 10) |
|||
| Sex | 1 man, 9 women | 1 man, 9 women | NA | NA |
| Graft source | 5 bone-patellar tendon-bone autograft, 5 semitendinosus | NA | NA | NA |
| Mean ± SD |
||||
| Age, y | 21.0 ± 2.8 | 20.8 ± 2.5 | 0.16 | .88 |
| Height, cm | 164.6 ± 5.0 | 169.1 ± 6.2 | −1.82 | .09 |
| Mass, kg | 64.0 ± 6.1 | 61.1 ± 6.4 | −0.48 | .64 |
| Body mass index, kg/m2 | 23.7 ± 2.7 | 21.4 ± 2.3 | 0.63 | .54 |
| Months since surgery, mean ± SD | 27.9 ± 16.6 | NA | NA | NA |
| Tegner Activity Scale score (range, 0−10) | 6.6 ± 1.1 | 7.3 ± 1.6 | −1.49 | .15 |
| Visual analog scale for knee pain, cm (range, 0−10) | 0.1 ± 0.2 | 0.0 ± 0.1 | 1.60 | .13 |
Abbreviation: NA, not applicable.
Preintervention Testing Procedures
All participants completed the International Knee Documentation Committee Form, the Tegner Activity Scale, and the VAS for knee pain during the 24 hours before testing. Next, they completed a bilateral assessment of quadriceps function, including knee-extension strength and voluntary quadriceps activation.
Assessment of Quadriceps Function.
Knee-extension strength was measured as the maximal voluntary isometric contraction (MVIC) of knee-extension torque using a multimodal dynamometer (System 4; Biodex Medical Systems, Inc, Shirley, NY). Participants completed 2 submaximal and 2 maximal isometric knee-extension practice trials at 90° of knee flexion. After no less than 3 minutes of rest, participants completed 2 knee-extension MVIC trials. They rested for 1 minute between trials. The investigator (A.R.K.) gave oral cues on contraction form throughout the testing trials. A successful trial was one in which the participant achieved a 2-second plateau representing the MVIC.29 Trials with substantial torque inconsistency or poor data quality were discarded, and a supplemental trial was collected. Torque inconsistency was considered to be a greater than 5% difference between trials, whereas poor data quality was defined as occurring in any trial in which a torque plateau of at least 200 milliseconds was not achieved. Given a limitation in study design, the average number of trials required to achieve 2 acceptable trials was not recorded. Knee-extension MVIC torque was normalized to body mass (Nm/kg).
Quadriceps CAR was measured via the superimposed-burst technique during the knee-extension MVIC trials.30,31 During each trial, a 100-millisecond train of 10 square-wave pulses (intensity of 125 V, pulse duration of 600 μ, and frequency of 100 pulses per second) of electrical stimulation was manually delivered to the quadriceps using a dual-output square-pulse stimulator (model S88; Grass-Telefactor, West Warwick, RI).29 This stimulus produced an increase in torque known as a superimposed burst, which we compared with the MVIC torque to permit calculation of the quadriceps CAR (Equation 1)32:
where TMVIC is the MVIC torque and TSIB is the superimposed burst torque.
Limb Symmetry Index.
An LSI was calculated for normalized knee-extension MVIC torque and quadriceps CAR at the preintervention and postintervention time points.33 In the ACLR group, LSI was calculated as follows (Equation 2):
In the control group, LSI was calculated as follows (Equation 3):
In both cases, an LSI of 100% indicated perfect symmetry between limbs for a given measure.
Cryotherapy-Facilitated Quadriceps-Strengthening Intervention
Participants in the ACLR group completed a 2-week, unilateral, cryotherapy-facilitated quadriceps-strengthening intervention focused on the involved limb. The program consisted of 4 supervised and 10 home-based exercise sessions, for a total of 14 exercise sessions.19,34 In all cases, the first day of the intervention was scheduled as a supervised exercise session to ensure proper technique for both supervised and home-based exercise sessions. After completing the initial supervised exercise session, participants were scheduled for 3 more supervised exercise sessions over the following 13 days. On all days when participants did not complete a supervised exercise session, we instructed them to complete a home-based exercise session, totaling 14 exercise sessions over the 2-week intervention period.
In a typical exercise session, participants started with a 20-minute application of cryotherapy treatment to the knee joint (approximately 1.5 L of crushed ice applied to the anterior and posterior aspects of the knee joint) followed by lower extremity muscle stretching, progressive strengthening exercises, and balance training.19 These sessions lasted approximately 1 hour (Table 2). All supervised exercise sessions were overseen by 1 of 2 certified athletic trainers (C.M.K., A.R.K.) who each had at least 4 years of clinical experience. Both clinicians discussed participant exercise progression after each supervised session to ensure consistency in the treatment protocol. The number of repetitions and resistance used for each supervised and home-based exercise were progressed by the athletic trainers based on perceived difficulty and participant-reported fatigue throughout the supervised sessions.34 Daily home treatments were monitored using a treatment log, which was reviewed at each supervised exercise session. All participants in the ACLR group attended a minimum of 3 supervised sessions and completed a minimum of 8 home-based exercise sessions.
Table 2. .
Exercises Included in Supervised and Home-Based Exercise Sessions for Participants With Anterior Cruciate Ligament Reconstruction
| Exercise |
Exercise Session |
|
| Supervised |
Home Based |
|
| Cryotherapy treatment | Included | Included |
| Thigh-muscle stretching | Included | Included |
| Quadriceps sets | Included | Included |
| Resisted straight-leg raises | Included | Included |
| Single-legged calf raises | Included | Included |
| Resisted leg press | Included | Not included |
| Resisted knee flexion | Included | Not included |
| Lunges with dumbbells | Included | Included |
| Lateral step-downs with dumbbells | Included | Not included |
| Wall squats with medicine ball | Included | Not included |
| Unstable single-legged balance | Included | Not included |
Postintervention Testing Procedures
Participants in the ACLR group returned for follow-up testing no later than 2 days after completing the intervention program. All testing procedures from the preintervention testing session were repeated in identical order during the postintervention testing session.
Statistical Analysis
Descriptive information and patient-reported outcome measures were compared between groups using independent-samples t tests. Preintervention between-groups differences in normalized knee-extension MVIC torque and quadriceps CAR, as well as LSI for both measures, were evaluated using independent-samples t tests. Postintervention data from the ACLR group were also compared with data from the control group using independent-samples t tests to reevaluate between-groups differences after the 2-week intervention. For all comparisons, the involved limb in the ACLR group was compared with the poorer-performing limb in the control group, whereas the uninvolved limb in the ACLR group was compared with the better-performing limb in the control group.
We used paired-samples t tests to compare preintervention and postintervention normalized knee-extension MVIC torque, quadriceps CAR, and LSI in the involved and uninvolved limbs of the ACLR group. In addition, Cohen d effect sizes and associated 95% confidence intervals (CIs; Cohen d ± 95% CI) were calculated for each comparison using the pooled standard deviation between groups or time points. The Cohen d effect sizes were interpreted as weak (<0.2), small (0.21−0.39), medium (0.4−0.7), or large (>0.7). We set the α level a priori at ≤.05. Statistical analyses were performed using SPSS (version 22.0; IBM Corp, Armonk, NY). Effect sizes and 95% CIs were calculated using Excel (version 2010; Microsoft Corp, Redmond, WA).
RESULTS
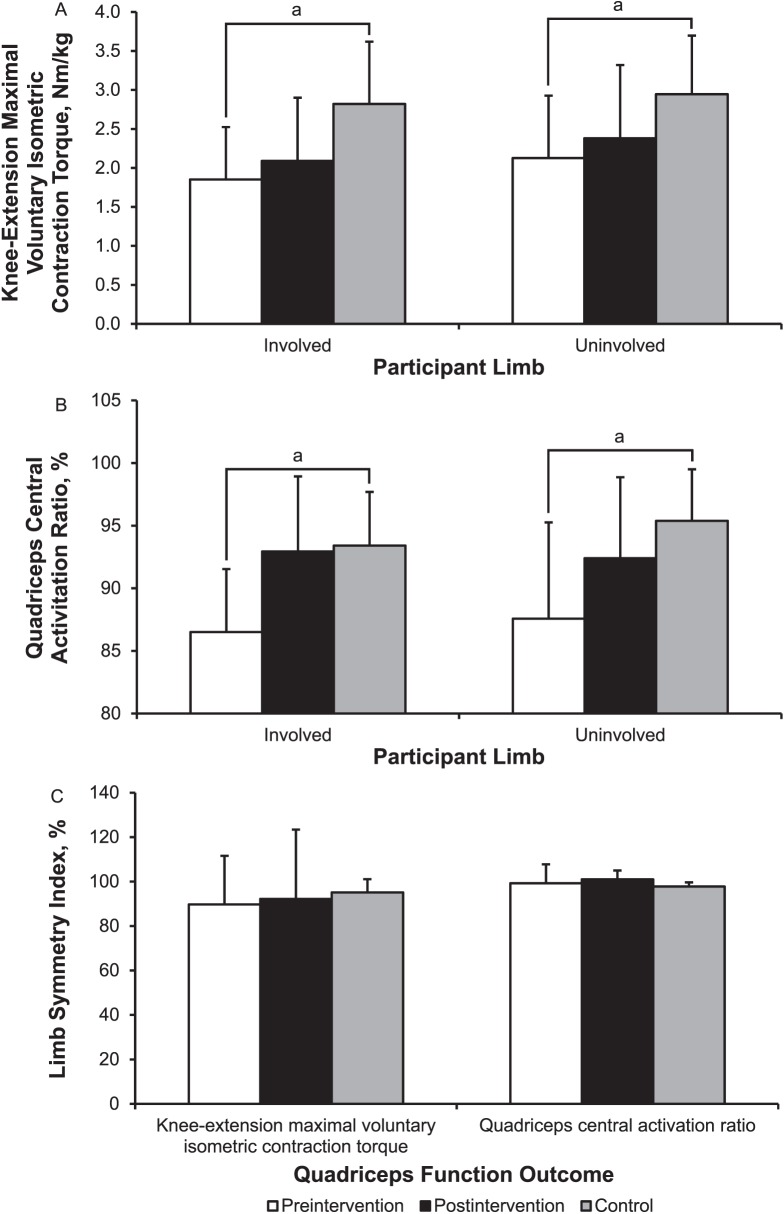
During the intervention, no participant was excluded because of lack of compliance, and no participant was lost to follow-up. Comparisons between the control and ACLR groups during the preintervention period (Figure 1 and Table 3) revealed less knee-extension MVIC torque and quadriceps CAR in the ACLR-involved limb than in the poorer-performing control limb (MVIC: P = .01, Cohen d = −1.31 [95% CI = −2.28, −0.34]; CAR: P = .004, Cohen d = −1.48 [95% CI = −2.47, −0.49]) and in the uninvolved ACLR limb than in the better-performing control limb (MVIC: P = .03, Cohen d = −1.05 [95% CI = −1.99, −0.11]; CAR: P = .01, Cohen d = −1.27 [95% CI = −2.23, −0.31]). When comparing LSI between groups, we observed no differences for either knee-extension MVIC torque (P = .46, Cohen d = −0.34 [95% CI = −1.22, 0.54]) or quadriceps CAR (P = .60, Cohen d = 0.24 [95% CI = −0.64, 1.12]).
Figure 1. .
Preintervention and postintervention comparison of the involved and uninvolved limbs. A, Knee-extension maximal voluntary isometric contraction torque. B, Quadriceps central activation ratio. C, Limb symmetry index for both measures between individuals with a history of anterior cruciate ligament reconstruction and matched control participants. a Indicates difference between the preintervention anterior cruciate ligament reconstruction and the control groups (P ≤ .05).
Table 3. .
Group Statistics for Preintervention and Postintervention Primary Outcome Measures (Mean ± SD)
| Outcome Measure |
Group |
|||||
| Anterior Cruciate Ligament Reconstruction |
Control |
|||||
| Involved Limb |
Uninvolved Limb |
Limb Symmetry Index |
Nondominant Limb |
Dominant Limb |
Limb Symmetry Index |
|
| Knee-extension maximal voluntary isometric contraction torque, Nm/kg | ||||||
| Preintervention | 1.85 ± 0.67 | 2.13 ± 0.80 | 89.76 ± 21.85 | 2.82 ± 0.80 | 2.95 ± 0.75 | 95.14 ± 5.96 |
| Postintervention | 2.09 ± 0.81 | 2.38 ± 0.94 | 92.21 ± 31.22 | NA | NA | NA |
| Quadriceps central activation ratio, % | ||||||
| Preintervention | 86.51 ± 5.03 | 87.58 ± 7.68 | 99.27 ± 8.50 | 93.41 ± 4.29 | 95.38 ± 4.12 | 97.80 ± 1.87 |
| Postintervention | 92.94 ± 5.99 | 92.39 ± 6.47 | 100.70 ± 4.01 | NA | NA | NA |
| International Knee Documentation Committee score | ||||||
| Preintervention | 85.29 ± 11.81a | 99.43 ± 1.46 | ||||
| Postintervention | 87.01 ± 11.34a | NA | NA | |||
Abbreviation: NA, not applicable.
Indicates preintervention between-groups difference (P ≤ .05).
For postintervention between-groups comparisons (Figure 1 and Table 3), we observed no difference in knee-extension MVIC torque or quadriceps CAR between the ACLR-involved limb and the poorer-performing control limb (MVIC: P = .06, Cohen d = −0.98 [95% CI = −1.90, −0.06]; CAR: P = .84, Cohen d = −0.09 [95% CI = −0.97, 0.79]) or between the uninvolved ACLR limb and the better-performing control limb (MVIC: P = .15, Cohen d = −0.67 [95% CI = −1.57, 0.23]; CAR: P = .23, Cohen d = −0.55 [95% CI = −1.44, 0.34]). When comparing LSI between groups, we observed no differences between groups for either knee-extension MVIC torque (P = .77, Cohen d = −0.13 [95% CI = −1.01, 0.75]) or quadriceps CAR (P = .06, Cohen d = 0.22 [95% CI = −0.66, 1.10]).
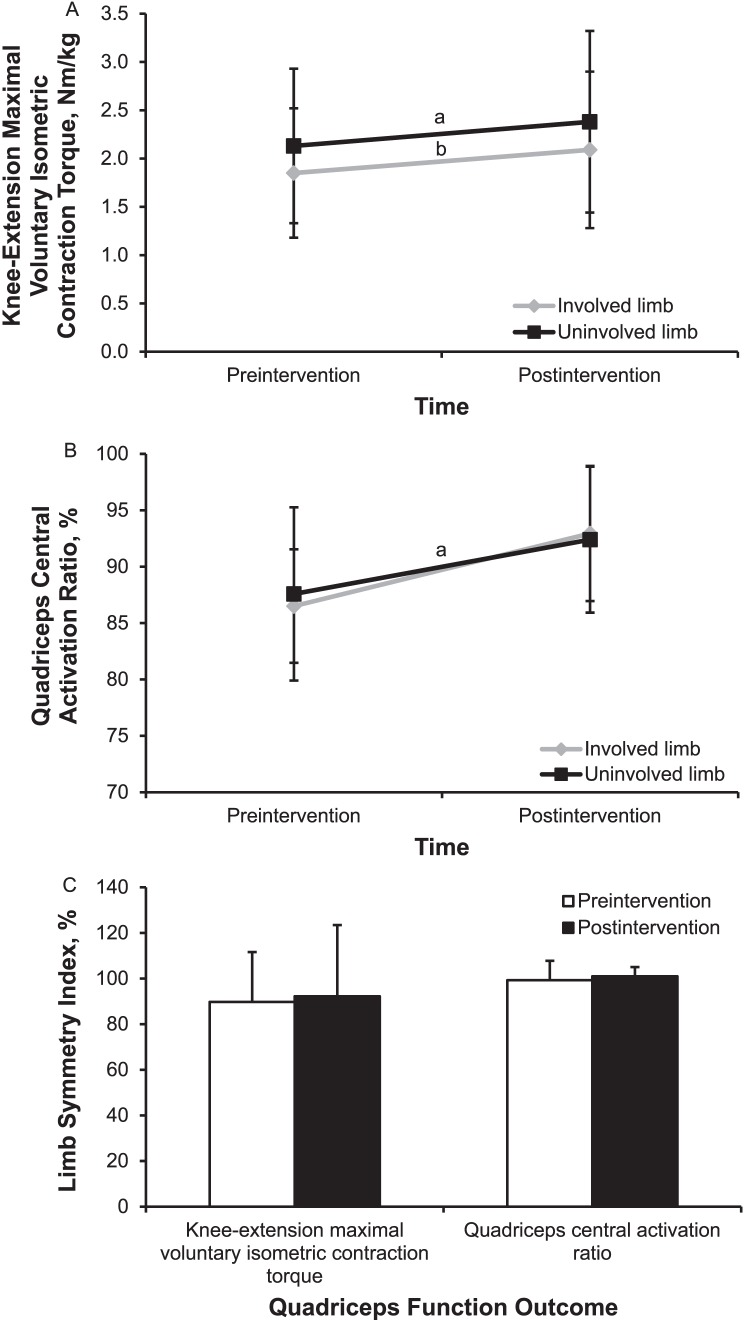
Involved-limb (P = .04, Cohen d = 0.32 [95% CI = −0.56, 1.20]) and uninvolved-limb (P = .03, Cohen d = 0.29 [95% CI = −0.59, 1.17]) knee-extension MVIC torque improved over the intervention in the ACLR group (Figure 2); however, improvement in quadriceps CAR was limited to the involved limb (P = .02, Cohen d = 1.16 [95% CI = 0.21, 2.11]). We observed no change in LSI over the intervention for knee-extension MVIC torque (P = .74, Cohen d = 0.09 [95% CI = −0.79, 0.97]) or quadriceps CAR (P = .61, Cohen d = 0.26 [95% CI = −0.62, 1.14]).
Figure 2. .
Preintervention to postintervention comparison of involved limb and uninvolved limb. A, Knee-extension maximal voluntary isometric contraction torque. B, Quadriceps central activation ratio. C, Limb symmetry index for both measures among individuals with a history of anterior cruciate ligament reconstruction. a Indicates difference between preintervention and postintervention measures in the involved limb (P ≤ .05). b Indicates difference between preintervention and postintervention measures in the uninvolved limb (P ≤ .05).
DISCUSSION
Return to preinjury levels of knee-extension strength and quadriceps central activation, as well as nearly complete limb symmetry, have been highlighted as important factors for determining when to allow patients to return to physical activity after ACLR.14,15 Commonly, clinicians use the uninvolved limb as a stable comparison for the involved limb during rehabilitation after ACLR; however, our findings indicated that limb symmetry alone may not provide comprehensive information about restoration of involved-limb quadriceps function before the return to unrestricted physical activity (Figure 1). Whereas restoring involved-limb knee-extension strength and quadriceps central activation and maintaining optimal limb symmetry (>90.0%) may represent important clinical goals,35 continued efforts must be made to address persistent quadriceps dysfunction if the goal is a return to preinjury status.
The ACLR group displayed reduced bilateral knee-extension strength and quadriceps activation compared with the control group despite no measurable between-groups difference in limb symmetry for either measure (Figure 1). Anterior cruciate ligament reconstruction negatively affected quadriceps function in the involved and uninvolved limbs compared with the matched control limbs, which is consistent with several reports2,36,37 in this clinical population. These observations highlight an interesting and potentially challenging disconnect between a common clinical criterion, limb symmetry, used to measure improvement from rehabilitation after ACLR and the actual functional status of the individual. Whereas the potential limitations of symmetry as a measure have been described, our findings further the understanding that comparing unilateral knee-extension strength and quadriceps activation with preinjury levels,38 population-based norms,39 or patient-centered cutoff scores15,40 may add value to the LSI. Restoring limb symmetry for knee-extension strength and quadriceps activation, coupled with a return to normal involved-limb quadriceps function, may promote an optimal outcome for individuals after ACLR.
A 2-week program of focused quadriceps-strengthening exercise coupled with cryotherapy application as a disinhibitory modality has been shown19 to result in clinically important increases in involved knee-extension strength and quadriceps central activation in individuals experiencing persistent quadriceps dysfunction after ACLR; however, the effect on limb symmetry has not been investigated in this population. Based on the design of our study, we do not know whether using cryotherapy before exercise amplified the effect of the intervention.19 Results reported in the literature have supported the relative effectiveness of this intervention compared with strengthening alone in a population with ACLR, but without a direct comparison between interventions, the relative effect on measures of unilateral quadriceps function, such as LSI, remains unclear. Yet based on our findings, a disinhibitory modality in concert with focused strengthening exercises improved knee-extension strength and quadriceps central activation while maintaining nearly normal limb symmetry (90.0%) over a 2-week intervention (Figure 2).35 These findings are notable because the intervention resulted in bilateral improvement in the function of both quadriceps despite the cryotherapy application and most of the strengthening exercises being limited to the involved limb (Table 2). A positive crossover effect of involved-limb rehabilitation exercise on contralateral muscle function has been reported16; however, the magnitude of improvement from a relatively short-duration intervention (2 weeks) highlights the potential clinical utility of unilateral involved-limb quadriceps-strengthening exercises in concert with cryotherapy to facilitate a return to normal quadriceps function after ACLR.
Researchers investigating the immediate and short-term effects of disinhibitory modalities alone or coupled with strengthening exercises have reported similar phenomena of improved knee-extension strength18 and facilitation of voluntary activation,18,19 indicating that this approach to treatment may improve muscle function through reduced inhibitory signaling41 rather than the peripheral muscle hypertrophy associated with longer-duration strength-training interventions. Further investigation into the effects of a prolonged strengthening intervention, including disinhibitory modalities on quadriceps function or broader measures of lower extremity function, is an essential next step to improve the clinical applicability of our findings.
Our study had limitations. The frequency of treatment during the intervention may be atypical compared with some health care environments. Whereas this was meant to maximize the effect of the intervention over a short period, the structure of the intervention may not be generalizable to the broader population. Our participants were young, physically active individuals who had already reestablished limb symmetry for knee-extension strength and quadriceps activation after ACLR. Based on previous investigations,2,40 many individuals experience persistent asymmetry along with quadriceps dysfunction after ACLR, in which case our findings may not be directly applicable. In addition, we limited the outcome variables to measures of quadriceps function. Although these outcome measures have been shown to be related to patient-reported function and more general lower extremity function, translation to more functional measures of lower extremity performance is essential to maximize the generalizability of our findings. Lastly, our participants were predominantly female, which may have affected our results. Given our findings, it remains unclear if sex affects quadriceps strengthening after ACLR.
CONCLUSIONS
Participants with a history of ACLR may display acceptable limb symmetry while experiencing persistent reductions in knee-extension strength and quadriceps central activation compared with healthy matched individuals. Two weeks of focused strengthening of the involved limb facilitated by the disinhibitory effects of cryotherapy may improve involved-limb quadriceps function while preserving between-limbs symmetry. Clinicians should consider this approach when treating individuals experiencing persistent quadriceps weakness during recuperation from ACLR.
REFERENCES
- 1. Kuenze CM, Blemker SS, Hart JM. . Quadriceps function relates to muscle size following ACL reconstruction. J Orthop Res. 2016; 34 9: 1656– 1662. [DOI] [PubMed] [Google Scholar]
- 2. Kuenze CM, Hertel J, Weltman A, Diduch D, Saliba SA, Hart JM. . Persistent neuromuscular and corticomotor quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train. 2015; 50 3: 303– 312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. . Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014; 48 21: 1543– 1552. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. . Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015; 43 4: 848– 856. [DOI] [PubMed] [Google Scholar]
- 5. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. . Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012; 22 2: 116– 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. . Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014; 42 7: 1567– 1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Luc B, Gribble PA, Pietrosimone BG. . Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014; 49 6: 806– 819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lewek M, Rudolph K, Axe M, Snyder-Mackler L. . The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002; 17 1: 56– 63. [DOI] [PubMed] [Google Scholar]
- 9. Blackburn JT, Pietrosimone B, Harkey MS, Luc BA, Pamukoff DN. . Quadriceps function and gait kinetics after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2016; 48 9: 1664– 1670. [DOI] [PubMed] [Google Scholar]
- 10. Kuenze CM, Foot N, Saliba SA, Hart JM. . Drop-landing performance and knee-extension strength after anterior cruciate ligament reconstruction. J Athl Train. 2015; 50 6: 596– 602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lepley LK. . Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction: a review of the current literature. Sports Health. 2015; 7 3: 231– 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barenius B, Nordlander M, Ponzer S, Tidermark J, Eriksson K. . Quality of life and clinical outcome after anterior cruciate ligament reconstruction using patellar tendon graft or quadrupled semitendinosus graft: an 8-year follow-up of a randomized controlled trial. Am J Sports Med. 2010; 38 8: 1533– 1541. [DOI] [PubMed] [Google Scholar]
- 13. Ericsson YB, Roos EM, Frobell RB. . Lower extremity performance following ACL rehabilitation in the KANON-trial: impact of reconstruction and predictive value at 2 and 5 years. Br J Sports Med. 2013; 47 15: 980– 985. [DOI] [PubMed] [Google Scholar]
- 14. Palmieri-Smith RM, Lepley LK. . Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015; 43 7: 1662– 1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kuenze C, Hertel J, Saliba S, Diduch DR, Weltman A, Hart JM. . Clinical thresholds for quadriceps assessment after anterior cruciate ligament reconstruction. J Sport Rehabil. 2015; 24 1: 36– 46. [DOI] [PubMed] [Google Scholar]
- 16. Lepley LK, Palmieri-Smith RM. . Cross-education strength and activation after eccentric exercise. J Athl Train. 2014; 49 5: 582– 589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lepley LK, Wojtys EM, Palmieri-Smith RM. . Combination of eccentric exercise and neuromuscular electrical stimulation to improve biomechanical limb symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2015; 30 7: 738– 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harkey MS, Gribble PA, Pietrosimone BG. . Disinhibitory interventions and voluntary quadriceps activation: a systematic review. J Athl Train. 2014; 49 3: 411– 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hart JM, Kuenze CM, Diduch DR, Ingersoll CD. . Quadriceps muscle function after rehabilitation with cryotherapy in patients with anterior cruciate ligament reconstruction. J Athl Train. 2014; 49 6: 733– 739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pietrosimone BG, Saliba SA, Hart JM, Hertel J, Ingersoll CD. . Contralateral effects of disinhibitory TENS on quadriceps function in people with knee osteoarthritis following unilateral treatment. N Am J Sports Phys Ther. 2010; 5 3: 111– 121. [PMC free article] [PubMed] [Google Scholar]
- 21. Hopkins J, Ingersoll CD, Edwards J, Klootwyk TE. . Cryotherapy and transcutaneous electric neuromuscular stimulation decrease arthrogenic muscle inhibition of the vastus medialis after knee joint effusion. J Athl Train. 2002; 37 1: 25– 31. [PMC free article] [PubMed] [Google Scholar]
- 22. Hopkins JT. . Knee joint effusion and cryotherapy alter lower chain kinetics and muscle activity. J Athl Train. 2006; 41 2: 177– 184. [PMC free article] [PubMed] [Google Scholar]
- 23. Pietrosimone BG, Hart JM, Saliba SA, Hertel J, Ingersoll CD. . Immediate effects of transcutaneous electrical nerve stimulation and focal knee joint cooling on quadriceps activation. Med Sci Sports Exerc. 2009; 41 6: 1175– 1181. [DOI] [PubMed] [Google Scholar]
- 24. Pietrosimone BG, Ingersoll CD. . Focal knee joint cooling increases the quadriceps central activation ratio. J Sports Sci. 2009; 27 8: 873– 879. [DOI] [PubMed] [Google Scholar]
- 25. Kuenze C, Hart JM. . Cryotherapy to treat persistent muscle weakness after joint injury. Phys Sportsmed. 2010; 38 3: 38– 44. [DOI] [PubMed] [Google Scholar]
- 26. Hart JM, Kuenze CM, Pietrosimone BG, Ingersoll CD. . Quadriceps function in anterior cruciate ligament-deficient knees exercising with transcutaneous electrical nerve stimulation and cryotherapy: a randomized controlled study. Clin Rehabil. 2012; 26 11: 974– 981. [DOI] [PubMed] [Google Scholar]
- 27. Koutras G, Pappas E, Terzidis IP. . Crossover training effects of three different rehabilitation programs after arthroscopic meniscectomy. Int J Sports Med. 2009; 30 2: 144– 149. [DOI] [PubMed] [Google Scholar]
- 28. Garber CE, Blissmer B, Deschenes MR, et al. . American College of Sports Medicine. American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults. Guidance for prescribing exercise. Med Sci Sports Exerc. 2011; 43 7: 1334– 1359. [DOI] [PubMed] [Google Scholar]
- 29. Roberts D, Kuenze C, Saliba S, Hart JM. . Accessory muscle activation during the superimposed burst technique. J Electromyogr Kinesiol. 2012; 22 4: 540– 545. [DOI] [PubMed] [Google Scholar]
- 30. Hart JM, Fritz JM, Kerrigan DC, Saliba EN, Gansneder BM, Ingersoll CD. . Quadriceps inhibition after repetitive lumbar extension exercise in persons with a history of low back pain. J Athl Train. 2006; 41 3: 264– 269. [PMC free article] [PubMed] [Google Scholar]
- 31. Snyder-Mackler L, De Luca PF, Williams PR, Eastlack ME, Bartolozzi AR III.. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994; 76 4: 555– 560. [DOI] [PubMed] [Google Scholar]
- 32. Kent-Braun JA, Le Blanc R. . Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996; 19 7: 861– 869. [DOI] [PubMed] [Google Scholar]
- 33. Juris PM, Phillips EM, Dalpe C, Edwards C, Gotlin RS, Kane DJ. . A dynamic test of lower extremity function following anterior cruciate ligament reconstruction and rehabilitation. J Orthop Sports Phys Ther. 1997; 26 4: 184– 191. [DOI] [PubMed] [Google Scholar]
- 34. Kuenze C, Eltoukhy M, Kelly A, Kim CY. . Impact of quadriceps strengthening on response to fatiguing exercise following ACL reconstruction. J Sci Med Sport. 2017; 20 1: 6– 11. [DOI] [PubMed] [Google Scholar]
- 35. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. . Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007; 87 3: 337– 349. [DOI] [PubMed] [Google Scholar]
- 36. Lepley LK, Palmieri-Smith RM. . Quadriceps strength, muscle activation failure, and patient-reported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: a cross-sectional study. J Orthop Sports Phys Ther. 2015; 45 12: 1017– 1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lepley AS, Ericksen HM, Sohn DH, Pietrosimone BG. . Contributions of neural excitability and voluntary activation to quadriceps muscle strength following anterior cruciate ligament reconstruction. Knee. 2014; 21 3: 736– 742. [DOI] [PubMed] [Google Scholar]
- 38. Lepley AS, Gribble PA, Thomas AC, Tevald MA, Sohn DH, Pietrosimone BG. . Quadriceps neural alterations in anterior cruciate ligament reconstructed patients: a 6-month longitudinal investigation. Scand J Med Sci Sports. 2015; 25 6: 828– 839. [DOI] [PubMed] [Google Scholar]
- 39. Leyva A, Balachandran A, Signorile JF. . Lower-body torque and power declines across six decades in three hundred fifty-seven men and women: a cross-sectional study with normative values. J Strength Cond Res. 2016; 30 1: 141– 158. [DOI] [PubMed] [Google Scholar]
- 40. Pietrosimone B, Lepley AS, Harkey MS, et al. . Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc. 2016; 48 9: 1671– 1677. [DOI] [PubMed] [Google Scholar]
- 41. Hart JM, Bessette M, Choi L, Hogan MV, Diduch D. . Sensory response following knee joint damage in rabbits. BMC Musculoskelet Disord. 2014; 15: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]