Abstract
Context:
Diminished hip-abductor strength has been suggested to increase the risk of noncontact lateral ankle sprains.
Objective:
To determine prospectively whether baseline hip-abductor strength predicts future noncontact lateral ankle sprains in competitive male soccer players.
Design:
Prospective cohort study.
Setting:
Athletic training facilities and various athletic fields.
Patients or Other Participants:
Two hundred ten competitive male soccer players.
Main Outcome Measure(s):
Before the start of the sport season, isometric hip-abductor strength was measured bilaterally using a handheld dynamometer. Any previous history of ankle sprain, body mass index, age, height, and weight were documented. During the sport season (30 weeks), ankle injury status was recorded by team medical providers. Injured athletes were further classified based on the mechanism of injury. Only data from injured athletes who sustained noncontact lateral ankle sprains were used for analysis. Postseason, logistic regression was used to determine whether baseline hip strength predicted future noncontact lateral ankle sprains. A receiver operating characteristic curve was constructed for hip strength to determine the cutoff value for distinguishing between high-risk and low-risk outcomes.
Results:
A total of 25 noncontact lateral ankle sprains were confirmed, for an overall annual incidence of 11.9%. Baseline hip-abductor strength was lower in injured players than in uninjured players (P = .008). Logistic regression indicated that impaired hip-abductor strength increased the future injury risk (odds ratio = 1.10 [95% confidence interval = 1.02, 1.18], P = .010). The strength cutoff to define high risk was ≤33.8% body weight, as determined by receiver operating characteristic curve analysis. For athletes classified as high risk, the probability of injury increased from 11.9% to 26.7%.
Conclusions:
Reduced isometric hip-abductor strength predisposed competitive male soccer players to noncontact lateral ankle sprains.
Key Words: inversion ankle sprain, noncontact injury, ankle-sprain prevention, hip abductor
Key Points
Reduced hip strength (≤33.8% body weight) more than doubled the risk of noncontact lateral ankle sprains in male soccer players.
Among players classified as high risk, the probability of injury increased from 11.9% to 26.7%.
Ankle sprains are among the most common musculoskeletal injuries observed in competitive athletes.1,2 Lateral (or inversion) ankle sprains are observed most frequently, followed by syndesmotic (high) and deltoid (medial) ankle sprains.2 Basketball, football, and soccer are associated with the highest percentages of ankle sprains (41%, 9%, and 8%, respectively), as these sports expose the ankle to increased angular and rotational strain from repetitive running, cutting, and jumping.3 In addition, males between 15 and 24 years of age have substantially higher ankle sprain rates compared with their female counterparts.3 Based on a 2014 systematic review and meta-analysis2 of 181 prospective epidemiologic studies, the prevalence of ankle sprains was 11.9%, but the prevalence of lateral ankle sprains was 15.3%.
From an injury-prevention standpoint, noncontact lateral ankle sprains (or those arising from an athlete's inherent movement patterns) are of primary interest. Contact ankle sprains (or those arising from an external perturbation such as player contact) are theoretically less preventable. In separate reviews, Martin et al (2013)4 and McGovern and Martin (2016)5 acknowledged that the following risk factors have generally been accepted as increasing the risk of future lateral ankle sprains: history of previous ankle sprain, limited ankle-dorsiflexion range of motion, lack of static and dynamic warmup before activity, increased talar curvature, failure to use an external ankle support prophylactically, poor proprioception, and impaired balance.
Authors6–8 of cross-sectional studies have reported that persons who have experienced an ankle sprain exhibit hip weakness. However, a limitation of such studies is that cause-and-effect relationships cannot be determined. Nonetheless, hip weakness (particularly in the abductors) has been shown to contribute to poor balance and compensatory neuromuscular adaptations at the ankle (ie, elevated inversion moments and increased activation and earlier onset of the ankle evertors). As such, it has been proposed that hip-abductor weakness may increase one's risk for lateral ankle sprain.9,10 This premise was supported by Leetun et al,11 who reported that athletes who sustained a lower extremity injury (ie, an event that occurred during athletic participation and required medical attention) were weaker in hip abduction and hip external rotation compared with their uninjured counterparts. Conversely, in a prospective study, McHugh et al12 concluded that the strength of the hip abductors, hip flexors, or hip adductors did not predict the future risk of noncontact lateral ankle sprain. However, McHugh et al12 examined a combined-sex cohort and evaluated athletes in multiple sports (basketball, football, gymnastics, soccer), making it difficult to ascertain the conditions (if any) under which hip strength predicted future noncontact lateral ankle sprain.
The primary aim of our study was to prospectively determine whether reduced baseline hip strength (specifically in hip abduction) predicted future noncontact lateral ankle sprains. In contrast to McHugh et al,12 we sought to address this question in a more homogeneous population (male soccer players) because this group is considered to be at high risk for ankle sprains.13 A secondary aim of the study was to determine the cutoff for baseline hip-abduction strength that would allow us to predict future noncontact lateral ankle sprains with high sensitivity and specificity.
METHODS
Participants
Male players from Isfahan competitive soccer clubs (ie, members of the premier soccer club league) were invited to participate in this study. Players represented different age categories (junior, high junior, and adult; ages 14–34 years). Players who had sustained any lower extremity injury over the past 6 months or had any history of knee surgery were excluded from participation. Of the 234 players initially contacted, 210 consented to participate, and provided written informed consent. This study was approved by the Institutional Review Board at the University of Isfahan.
We estimated that 12% to 15% of the players would sustain a noncontact lateral ankle sprain over the course of a single season.2 Results from simulation experiments concerning the number of events (or less common outcome) suggested that a minimum of 10 events per predictor (preferably greater) would be needed to build a valid logistic model.14,15 Our predictor of interest was hip-abductor strength, so we estimated that we would need at least 10 cases (or injured athletes) for adequate power. Assuming an injury rate of 12%, we aimed to recruit at least 100 players. To account for dropouts, misdiagnoses, and a potentially lower injury rate, we sought to recruit at least 200 players.
Injury Surveillance
Players were followed over the course of a single season (30 weeks). In total, 10 teams (at different sites) and 10 team physicians were involved in the study. On average, athletes participated in 30 games during the course of the season and 8 soccer practices per week.
An ankle sprain was defined as noncontact if it was sustained without direct contact (from another player or object) to the lower extremity, upper extremity, or trunk. All other ankle sprains were deemed to be from contact. Physical examination by the team physician confirmed all ankle sprains (specifically whether lateral, medial, or syndesmotic) immediately after injury, and patient recall (ie, interviewing) within 48 hours of injury was used to determine the injury mechanism (ie, noncontact versus contact). Only noncontact lateral ankle sprains that necessitated absence from physical activity for at least 1 week (which was mandatory owing to professional soccer club policies) were analyzed, and only a single ankle sprain per player was counted. If a second sprain occurred during the course of the season, only the first was used for analysis.
Hip-Strength Assessment
Before the start of the sport season, bilateral isometric hip-abductor strength was assessed using a handheld dynamometer (model Commander Power Track II; JTECH Medical Industries, Salt Lake City, UT). Players were tested in the side-lying position on a treatment table with the pelvis stabilized by a research assistant. The hip was abducted to 30°, and the dynamometer pad was placed 10 cm proximal to the lateral femoral epicondyle. The participant then abducted the hip with maximum effort into the dynamometer pad for 5 seconds against manual resistance.16–18 Three repetitions were performed, and the average value was used for analysis. Strength measures were normalized to body weight (BW) and expressed as a percentage using the following formula: 100 × (kg strength)/(kg BW).19–22 Normalization increases the validity of strength measures, as the potential for body-size confounding is eliminated.21,22 We elected to exponentiate BW by a factor of 1 (although exponential factors ranging from 0.45 to 0.76 are generally advised for force)19–22 to simplify clinical interpretation.
In total, 17 graduate students in the program of sports science were selected to serve as strength testers. Each tester completed a training session and reliability testing, which consisted of testing 5 participants on 2 occasions (same day, 30 minutes apart). Intrarater and interrater reliability were calculated using an intraclass correlation coefficient (ICC; 3,3) absolute-agreement model.23 This equated to a 2-way mixed model (as the same raters tested all participants and were representative of the population) with average measures (as the reliability was based on the mean of 3 trials) and absolute agreement. The 10 raters with the highest intrarater reliability were selected to obtain the hip-strength measurements for the study participants. Average ICC values for intrarater and interrater reliability were 0.95 to 0.99 and 0.71, respectively. The measurement error of the strength scores was calculated using the standard error of measurement (SEM; SD√[1 − ICC]).24 Standard error values for intrarater and interrater reliability were 1.1 to 2.0 and 5.8, respectively.
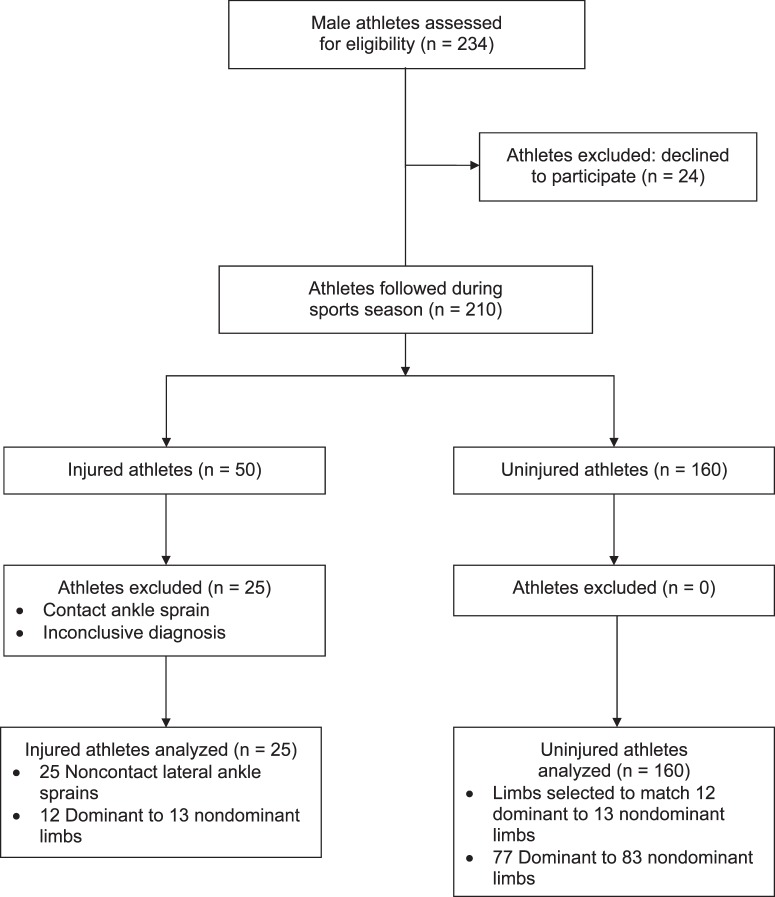
Bilateral hip-abductor strength was measured preseason (ie, before the start of the 30-week sport season). Testing was conducted on a player's day off from practice to minimize fatigue. For the injured players, the hip strength of the injured limb was used for analysis. For the uninjured players, the tested limb was selected so that the dominant-to-nondominant limb ratio was equivalent to that observed in the injured group.18,25 The dominant limb was defined as the preferred limb to kick a ball.26 In total, 25 noncontact lateral ankle sprains (1 injury per player) occurred. Specifically, 12 injuries were sustained to the dominant limb, and 13 injuries were sustained to the nondominant limb. This equated to a 12 : 13 dominant-to-nondominant limb ratio. We maintained the same 12 : 13 ratio in the uninjured group by randomly selecting 77 dominant limbs and 83 nondominant limbs (n = 160) for analysis (Figure 1). Only a single limb was tested per participant.
Figure 1. .
Overview of study design and selection of limbs for analysis. Limbs for uninjured participants were selected to match the ratio of dominant to nondominant limbs in the injured group.
Statistical Analysis
Players' baseline characteristics stratified by postseason injury status were compared using independent t tests (age, height, weight, body mass index [BMI], and hip-abductor strength) and χ2 tests (history of a previous ankle sprain of any type during the past 2 years). Logistic regression was used to determine the risk factors that predicted a future noncontact lateral ankle sprain. Potential risk factors were as follows: age, height, weight, BMI, hip-abductor strength, and ankle sprain during the past 2 years. All factors were entered into a logistic model using a multivariate stepwise approach and entry criteria of P < .1. Once a preliminary model was developed, we then checked for confounders by comparing the adjusted odds ratio (OR) and unadjusted OR with the inclusion of each factor. Any variable that caused at least a 5% increase in the OR was deemed a confounder and added to our final model. As a proxy for model fit, we reported the Nagelkerke R2 (as opposed to an alternative such as the Cox and Snell R2) because it is adjusted to achieve a maximum value of 1, thereby simplifying interpretation.27
A receiver operating characteristic (ROC) curve was constructed for hip-abductor strength to determine (1) the overall discriminative accuracy for predicting noncontact lateral ankle sprains and (2) the cutoff value for distinguishing between a positive test (high risk) and a negative test (low risk).28 The overall accuracy was assessed by evaluating the area under the curve (AUC), which ranged from 0 to 1 (with 0.5 equating to no better than chance alone and 1 indicating perfect accuracy).28 The cutoff point for the strength measure was selected by extrapolating the value on the ROC curve that maximized the sum of sensitivity and specificity (ie, the Youden Index).28,29 Players with a score greater than or equal to the cutoff were classified as high risk (positive test), and players with a score less than the cutoff were classified as low risk (negative test). For the selected cutoff point, the corresponding sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive posttest probability, and negative posttest probability were reported.30–32 In brief, sensitivity represents the percentage of cases within the injured cohort correctly identified as sustaining a noncontact lateral ankle sprain using the cutoff, whereas specificity represents the percentage of cases within the uninjured cohort correctly identified as not sustaining a noncontact lateral ankle sprain using the cutoff. The positive likelihood ratio represents how likely injured players are to have a positive test compared with uninjured players, whereas the negative likelihood ratio represents how likely injured players are to have a negative test compared with uninjured players. Finally, the positive posttest probability represents the probability of future injury given a positive preseason strength test, and the negative posttest probability represents the probability of future injury given a negative preseason strength test.
For all analyses, SPSS (version 22.0; IBM Corp, Armonk, NY) was used. MedCalc (version 13.1.2; MedCalc Software, Ostend, Belgium) was used to calculate 95% confidence intervals (CIs) for the sensitivity, specificity, and positive and negative likelihood ratios. Two-tailed P values less than .05 were deemed statistically significant.
RESULTS
Of the 210 players originally enrolled in the study, 25 were removed from the final analyses as they sustained a contact ankle sprain or had an inconclusive diagnosis (Figure 1). Given that the purpose of this study was to evaluate ankle sprains resulting from a noncontact mechanism, we eliminated all ankle sprains resulting from a contact (n = 21) or inconclusive mechanism (n = 4).18,33,34 Baseline descriptive data for the remaining 185 males are provided in Table 1.
Table 1. .
Baseline Characteristics of Male Soccer Players (N = 185) Stratified by Postinjury Status
| Variable |
Injured Players (n = 25) |
Uninjured Players (n = 160) |
||||
| Mean ± SD |
Minimum |
Maximum |
Mean ± SD |
Minimum |
Maximum |
|
| Age, ya | 20.9 ± 5.9 | 14.0 | 34.0 | 19.6 ± 5.1 | 13.0 | 32.0 |
| Height, ma | 1.78 ± 0.06 | 1.67 | 1.90 | 1.78 ± 0.08 | 1.50 | 1.95 |
| Mass, kga | 71.6 ± 7.1 | 57.0 | 82.0 | 68.6 ± 10.3 | 37.0 | 90.0 |
| Body mass index, kg/m2b | 22.5 ± 1.1 | 19.5 | 24.8 | 21.6 ± 2.0 | 13.6 | 24.8 |
| Hip-abductor strength, % body weight | ||||||
| Dominant limb | 27.0 ± 5.5 | 27.0 | 48.2 | 40.6 ± 6.7 | 25.8 | 58.8 |
| Nondominant limb | 35.9 ± 5.7 | 26.0 | 48.9 | 38.9 ± 6.6 | 15.6 | 61.3 |
| Adjustedc | 35.7 ± 5.6 | 26.0 | 48.2 | 39.5 ± 6.6 | 23.0 | 61.3 |
| Previous ankle sprain?, n (%)d | ||||||
| Yes (n = 36) | 8 (22.2) | 28 (77.8) | ||||
| No (n = 149) | 17 (11.4) | 132 (88.6) | ||||
No main effect for injury was observed (all P > .15).
Injured players demonstrated higher values than uninjured players (P = .002).
Injured players demonstrated lower values than uninjured players (P = .008). Values used for final analysis after controlling for limb dominance.
No association with injury status was observed (P = .09).
Injury Incidence
A total of 45 lateral ankle sprains (contact and noncontact combined) were sustained over the course of the season by 45 players. Twenty-five (56%) of the lateral ankle sprain injuries that occurred were noncontact, and the remaining 20 (44%) were contact. The annual incidence of noncontact lateral ankle sprains for males was 11.9% (25 of 210 players). Athletes with a previous ankle sprain had a reinjury rate of 22.2% (8 of 36 players). In contrast, athletes with no history of ankle sprain had an initial injury rate of 11.4% (17 of 149 players).
Baseline Characteristics
Preliminary analysis indicated the dominant limb was stronger than the nondominant limb for all athletes combined (40.1% BW ± 6.6% BW versus 38.5% BW ± 6.6% BW, respectively; P < .001). As such, we controlled for limb dominance, as previously described, and the resulting values are displayed in Table 1. Results from independent t tests (comparing injured versus uninjured male players) were nonsignificant for age (P = .242), height (P = .785), and mass (P = .154; Table 1). However, for hip-abductor strength, injured players were weaker (P = .008) than uninjured players (Table 1). In addition, injured players had a higher BMI compared with uninjured players (P = .002; Table 1). Chi-square analysis indicated no association between injury status and a history of ankle sprain (P = .089).
Regression Analysis
The logistic model produced using a stepwise approach is shown in Table 2. Subsequent checks for confounders resulted in no changes in our model. That is, forced entry of each of the potential risk factors into the model did not affect the OR at our threshold of 5%. The inclusion of BMI decreased the OR for hip strength by 1.8%. The inclusion of BW decreased the OR for hip strength by 0.9%. The inclusion of a history of prior ankle sprain increased the OR for hip strength by 0.9%. Therefore, our final model for predicting noncontact lateral ankle sprains was univariate (ie, included only hip-abductor strength). Reduced hip-abductor strength was associated with an increased risk of noncontact lateral ankle sprains (OR = 1.10 [95% CI = 1.02, 1.18], P = .010; Table 2). Stated alternatively, the odds of sustaining a noncontact lateral ankle sprain were increased by 10% for each 1-unit decrease in hip-abductor strength (expressed as % BW). The model explained 7.1% of the variation in injury status (based on the Nagelkerke R2) using hip-abductor strength alone as a predictor.
Table 2. .
Final Logistic Regression Model for Predicting Noncontact Lateral Ankle Sprains in Male Players
| Predictor |
Odds Ratio (95% Confidence Interval) |
P Value |
Nagelkerke R2 |
| Hip-abductor strength, % body weight | 1.10 (1.02, 1.18) | .01a | 7.1% |
Difference (P < .05).
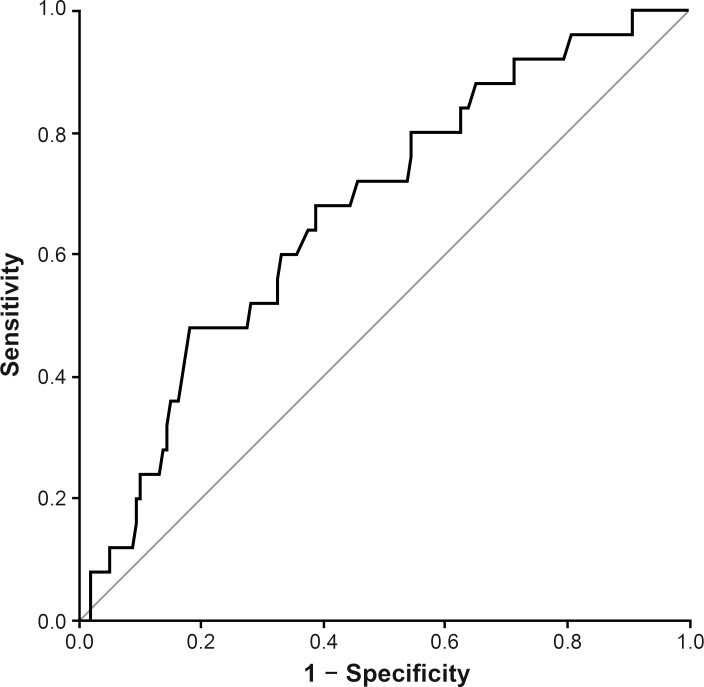
Receiver Operating Characteristic Curve Analysis
The ROC analysis (Figure 2, Table 3) indicated that the preseason hip-abductor strength test independently distinguished between players who later sustained a noncontact lateral ankle sprain and those who remained uninjured better than chance alone (AUC = 0.67 [95% CI = 0.56, 0.78], P = .006). In other words, 67% of athletes were correctly classified. Given that the predictive capacity of the curve was adequate (ie, better than chance alone), a cutoff was subsequently established to identify players at high injury risk: hip-abductor strength ≤33.8% BW (Table 3). A cutoff of 33.8% of BW corresponded with a sensitivity of 48% (95% CI = 28, 69), specificity of 82% (95% CI = 75, 88), positive likelihood ratio of 2.7 (95% CI = 1.6, 4.5), and negative likelihood ratio of 0.64 (95% CI = 0.43, 0.93).
Figure 2. .
Receiver operator characteristic curve used to calculate the area under the curve and optimal cutoff for hip-abductor strength.
Table 3. .
Predictive Capacity of Baseline Hip-Abductor Strength for Predicting Noncontact Lateral Ankle Sprains in Male Players
| Receiver Operating Characteristic Curve Analysis Variable |
Value |
| Cutoff, % body weight | 33.8 |
| Area under the curve (95% CI)a | 0.67 (0.56, 0.78) |
| Sensitivity, % (95% CI) | 48 (28, 69) |
| Specificity, % (95% CI) | 82 (75, 88) |
| Positive likelihood ratio (95% CI) | 2.7 (1.6, 4.5) |
| Negative likelihood ratio (95% CI) | 0.64 (0.43, 0.93) |
| Positive posttest probability, % | 26.7 |
| Negative posttest probability, % | 8.0 |
Abbreviation: CI, confidence interval.
Indicates difference (P < .05).
DISCUSSION
The purpose of our study was to prospectively determine if baseline hip-abductor strength predicted future noncontact lateral ankle sprains in male soccer players over the course of a single season. The findings indicate that a significant relationship existed between baseline hip strength and future noncontact lateral ankle sprain status. Specifically, increased hip strength had a protective effect against future injury (or diminished strength increased injury risk). It should be noted that our primary goal was to evaluate the predictive ability of hip-abductor strength. Although we considered other risk factors (ie, age, height, weight, BMI, previous ankle sprain), our study was by no means comprehensive, as we did not consider all possible risk factors (ie, other strength measurements, balance, strength asymmetries, range of motion). Therefore, our results represent only a small aspect of what is likely a complex interaction among baseline anthropometric measurements, strength measurements, injury history, anatomical morphology, neurologic function, and other factors.
Authors6–8 of cross-sectional studies have reported that persons who have experienced an ankle sprain exhibit hip weakness. Based on our results, hip-abduction weakness directly increases the risk of a future ankle sprain above what would be expected from a previous sprain. When we controlled for a previous history of ankle sprain (regardless of mechanism), our findings remained unchanged. That is, the OR for hip strength was increased by less than 1%: injury status = hip strength (OR = 1.11 [95% CI = 1.03, 1.19], P = .007) + prior ankle sprain (OR = 1.22 [95% CI = 0.95, 1.56], P = .12); Nagelkerke R2 = 9.3%.
Our results contrast with those of McHugh et al,12 who reported that hip-abduction strength had no influence on future noncontact lateral ankle sprains. Based on a power analysis,35 the present study had 83.4% power to detect a difference in means at the .05 level. In contrast, McHugh et al12 had 13.9% power to detect a difference in means at the .05 level. Therefore, the McHugh et al study was likely underpowered to detect an effect of hip strength on injury status. It should be noted that we reported a total of 25 noncontact lateral ankle sprains (in 210 players) over a single season (1-year incidence rate = 11.9%), whereas McHugh et al reported a total of 20 noncontact lateral ankle sprains (in 169 players) over 2 seasons (1-year incidence rate = 5.9%).12 The 5.9% incidence rate of McHugh et al (who investigated high school athletes) is comparable with that previously reported for amateur soccer players (Henry et al,36 2016, 6.7%). The 11.9% incidence rate in our study (of competitive male soccer players) is comparable with that reported for professional male soccer players (Fousekis et al,37 2012, 17%). Our injury rate of 11.9% included only participants with noncontact lateral ankle sprains and was lower than that established by Fousekis et al, who did not differentiate by injury location. Nonetheless, hip strength may only predict future injury in soccer players at the competitive level.
The findings from the current study suggest that, as hip-abductor strength decreases, injury risk increases (even when controlling for previous injury, as previously discussed). A possible mechanism for this finding considers the role of the hip abductors in maintaining postural stability. Persons with hip-abductor weakness exhibit (1) decreased medial-lateral postural stability9,10 and (2) increased activation and earlier onset of the ankle evertors in an effort to prevent excessive ankle inversion.9,10 Therefore, impaired hip strength may expose the ankle to injury by reducing postural control, which results in compensatory neuromuscular adaptions at the ankle.
As noted earlier, the derived values for the positive and negative likelihood ratios were used to calculate the probability of noncontact lateral ankle sprains given a positive (high risk) or negative (low risk) preseason hip-strength value (Table 3).31,32 Players classified as high risk based on their preseason hip-abductor strength had their probability of noncontact lateral ankle sprain increase from 11.9% to 26.7%. Players classified as low risk based on their preseason hip abductor strength had their probability of noncontact lateral ankle sprain decrease from 11.9% to 8.0%. It should be mentioned that the aforementioned values were derived using a preinjury risk of 11.9%, or the annual incidence rate of noncontact lateral ankle sprains in the current study.
It also bears mentioning that we derived an athlete's classification of high versus low risk using the ROC curve (Figure 2) by extrapolating the point that maximized the sum of sensitivity and specificity (33.8% BW, sensitivity = 48 [95% CI = 28, 69], specificity = 82 [95% CI = 75, 88]; Table 3).28,29 This means that our preseason strength test detected 48% of injured athletes (true positives) and 82% of uninjured athletes (true negatives). This then implies that 52% of injured athletes will remain undetected (false-negatives) and 18% of uninjured athletes will be incorrectly identified as injured (false-positives). In summary, these numbers suggest that an athlete who tests positive is probably correctly identified as likely to sustain a future injury (as the rate of false positives is low at 18%), whereas an athlete who tests negative will be less certain of his or her future injury status (as the rate of false-negatives is high at 52%). Although we could have selected a different cutoff value (to increase sensitivity and thereby lower the rate of false-negatives), this would have reduced specificity (for example, the cutoff corresponding to 80% sensitivity had 45% specificity). Therefore, we gave equal weighting to sensitivity and specificity by selecting the cutoff value that maximized their sum. The numeric cutoff of 33.8% of BW is comparable with the cutoff previously established18 for predicting noncontact anterior cruciate ligament injuries (35.4% of BW, sensitivity = 87 [95% CI = 60, 98], specificity = 65 [95% CI = 60, 69]), further supporting the concept that diminished hip strength increases the lower extremity injury risk.
A major limitation of sensitivity and specificity values is that they cannot be used to identify the probability of injury (given a positive or negative preseason strength test). As such, to enhance the clinical application of our study, we computed likelihood ratios, which were then used to compute the probability of injury. The positive and negative likelihood ratios were 2.7 and 0.64, respectively. A positive likelihood ratio of 2.7 means that an injured athlete is 2.7 times more likely to have a positive preseason strength test than an uninjured athlete. The higher this value, the more useful the test is in predicting injury. A negative likelihood ratio of 0.64 means that an injured athlete is 0.64 times as likely to have a negative preseason strength test than an uninjured athlete. The smaller this value, the more useful the test is in predicting lack of injury. Stated alternatively, uninjured athletes are 1.6 times more likely to have a negative preseason strength test compared with injured athletes. Generally speaking, positive likelihood ratios >10 significantly increase the probability of the condition, whereas negative likelihood ratios <0.1 significantly decrease the probability of the condition.31 Our positive and negative likelihood ratios of 2.7 and 0.64, respectively, were small, suggesting that hip strength alone is not an appropriate predictor of noncontact lateral ankle sprains. In addition, our OR of 1.10 was smaller than those ORs computed from other studies of ankle-sprain risk factors: power output (OR = 9.20),36 balance (OR = 2.33),36 BW (OR = 5.72),37 BMI (OR = 8.16),37 ankle-strength asymmetries (OR = 8.88),37 and previous ankle injury (OR = 1.83).38
It should be acknowledged that our logistic model as a whole explained only 7.1% of the variation in injury status (Table 2), and the accuracy of our model was only 67% (AUC, Table 3). Therefore, reduced hip strength is only 1 of several potential risk factors, such as lower limb power output,36 impaired balance,36 increased BW,37 increased BMI,12,37 ankle eccentric strength asymmetries of the dorsiflexors and plantar flexors,37 and previous injury,12,38 that should be considered when assessing an athlete's risk of noncontact lateral ankle sprain. Including BMI and previous injury in our model (in addition to hip strength) would have increased the Nagelkerke R2 from 7.1% to 11.4%. However, because both variables were eliminated when we performed stepwise regression (with a liberal entry criteria of P < .1; Table 2) and neither BMI nor prior injury was a confounder, we elected to report our final model as univariate (with hip-abductor strength alone).
To the best of our knowledge, this is the first prospective study to establish a link between preseason hip strength and future noncontact lateral ankle sprain. However, this is not the first prospective study to link impaired hip strength with future lower extremity injury. Authors of previous prospective studies have reported that decreased hip strength increased the risk of noncontact anterior cruciate ligament injury,18 hip-adductor strain,39 low back pain,40 medial tibial pain (ie, shin splints),25 patellofemoral pain,41 and general lower extremity injuries.11,42 The implications of increasing hip strength are multifaceted in terms of benefiting the entire lower extremity and potentially reducing the risk of injury distally (such as at the ankle), proximally (such as at the low back), and in regions between (such as at the knee).
Limitations
Several limitations to our study need to be acknowledged. First, our results are based on hip-strength measures acquired using a handheld dynamometer, rendering our strength cutoffs inappropriate for other instruments. Second, we selected only a single cutoff value for hip-abduction strength. As such, our cutoff value only distinguished between low-risk and high-risk players (we did not include a moderate-risk group). Third, although our athletes had comparable heights, we did not account for possible differences in leg length, which may have affected our force results (ie, longer limbs have increased leverage and thereby increased potential for force production). Fourth, because we did not evaluate the strength of other muscles, it is difficult for us to ascertain if hip-abductor strength alone contributed the most to injury risk or whether this simply represented generalized weakness in the lower extremity. Fifth, even though we controlled for a history of ankle sprain (any type), we did so for only a 2-year period. Thus, our findings may have differed had we been able to obtain more extensive injury histories. However, adjusting for prior injury (even though for only a 2-year history) did not affect our results, so we would expect similar findings using an extensive injury history. Sixth, our athletes participated in 30 games and 240 practices, on average, during the present study, but we did not directly measure athletes' exposure. Therefore, some players may have been at greater risk of injury simply due to more practice time (as opposed to impaired hip strength). Seventh, our OR of 1.10 for the hip was lower than risk factors established in prior studies. However, this was the only significant predictor of injury in our study, even after adjusting for well-established risk factors such as previous ankle sprain. Finally, we can only conclude that reduced preseason hip-abductor strength predicted future noncontact lateral ankle sprains in male soccer players at the professional level. As a result, our findings may not be applicable to other sports or female athletes.
CONCLUSIONS
Baseline isometric hip-abductor strength (measured using a handheld dynamometer) predicted future noncontact lateral ankle sprains in competitive male soccer players. On average, the odds of sustaining a noncontact lateral ankle sprain increased by 10% for each 1-unit decrease in hip-abductor strength (expressed as % BW). The hip-abductor–strength cutoff established to identify players at high risk was ≤33.8% BW. For players classified as high risk, the probability of injury increased from 11.9% to 26.7%. Based on our findings, it may be useful to evaluate isometric hip-abductor strength as part of clinical interventions or screening procedures (or both) because reduced hip strength predisposed competitive male soccer players to future noncontact lateral ankle sprains.
REFERENCES
- 1. Kaminski TW, Hertel J, Amendola N, et al. . National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013; 48 4: 528– 545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. . The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014; 44 1: 123– 140. [DOI] [PubMed] [Google Scholar]
- 3. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr.. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010; 92 13: 2279– 2284. [DOI] [PubMed] [Google Scholar]
- 4. Martin RL, Davenport TE, Paulseth S, et al. . Ankle stability and movement coordination impairments: ankle ligament sprains. J Orthop Sports Phys Ther. 2013; 43 9: A1– A40. [DOI] [PubMed] [Google Scholar]
- 5. McGovern RP, Martin RL. . Managing ankle ligament sprains and tears: current opinion. Open Access J Sports Med. 2016; 7: 33– 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Friel K, McLean N, Myers C, Caceres M. . Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006; 41 1: 74– 78. [PMC free article] [PubMed] [Google Scholar]
- 7. Nicholas JA, Strizak AM, Veras G. . A study of thigh muscle weakness in different pathological states of the lower extremity. Am J Sports Med. 1976; 4 6: 241– 248. [DOI] [PubMed] [Google Scholar]
- 8. Hubbard TJ, Kramer LC, Denegar CR, Hertel J. . Contributing factors to chronic ankle instability. Foot Ankle Int. 2007; 28 3: 343– 354. [DOI] [PubMed] [Google Scholar]
- 9. Lee SP, Powers CM. . Individuals with diminished hip abductor muscle strength exhibit altered ankle biomechanics and neuromuscular activation during unipedal balance tasks. Gait Posture. 2014; 39 3: 933– 938. [DOI] [PubMed] [Google Scholar]
- 10. Lee SP, Powers C. . Fatigue of the hip abductors results in increased medial-lateral center of pressure excursion and altered peroneus longus activation during a unipedal landing task. Clin Biomech (Bristol, Avon). 2013; 28 5: 524– 529. [DOI] [PubMed] [Google Scholar]
- 11. Leetun DT, Ireland ML, Willson JD, et al. . Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004; 36 6: 926– 934. [DOI] [PubMed] [Google Scholar]
- 12. McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. . Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006; 34 3: 464– 470. [DOI] [PubMed] [Google Scholar]
- 13. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. . A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007; 37 1: 73– 94. [DOI] [PubMed] [Google Scholar]
- 14. Bagley SC, White H, Golomb BA. . Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol. 2001; 54 10: 979– 985. [DOI] [PubMed] [Google Scholar]
- 15. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. . A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49 12: 1373– 1379. [DOI] [PubMed] [Google Scholar]
- 16. Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. . The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2012; 42 1: 22– 29. [DOI] [PubMed] [Google Scholar]
- 17. Ireland ML, Willson JD, Ballantyne BT, Davis IM. . Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003; 33 11: 671– 676. [DOI] [PubMed] [Google Scholar]
- 18. Khayambashi K, Ghoddosi N, Straub RK, Powers CM. . Hip muscle strength predicts noncontact anterior cruciate ligament injury in male and female athletes: a prospective study. Am J Sports Med. 2016; 44 2: 355– 361. [DOI] [PubMed] [Google Scholar]
- 19. Jaric S. . Role of body size in the relation between muscle strength and movement performance. Exerc Sport Sci Rev. 2003; 31 1: 8– 12. [DOI] [PubMed] [Google Scholar]
- 20. Folland JP, Mc Cauley TM, Williams AG. . Allometric scaling of strength measurements to body size. Eur J Appl Physiol. 2008; 102 6: 739– 745. [DOI] [PubMed] [Google Scholar]
- 21. Jaric S. . Muscle strength testing: use of normalisation for body size. Sports Med. 2002; 32 10: 615– 631. [DOI] [PubMed] [Google Scholar]
- 22. Bazett-Jones DM, Cobb SC, Joshi MN, Cashin SE, Earl JE. . Normalizing hip muscle strength: establishing body-size-independent measurements. Arch Phys Med Rehabil. 2011; 92 1: 76– 82. [DOI] [PubMed] [Google Scholar]
- 23. Shrout PE, Fleiss JL. . Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86 2: 420– 428. [DOI] [PubMed] [Google Scholar]
- 24. Weir JP. . Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005; 19 1: 231– 240. [DOI] [PubMed] [Google Scholar]
- 25. Verrelst R, Willems TM, De Clercq D, Roosen P, Goossens L, Witvrouw E. . The role of hip abductor and external rotator muscle strength in the development of exertional medial tibial pain: a prospective study. Br J Sports Med. 2014; 48 21: 1564– 1569. [DOI] [PubMed] [Google Scholar]
- 26. Peters M. . Footedness: asymmetries in foot preference and skill and neuropsychological assessment of foot movement. Psychol Bull. 1988; 103 2: 179– 192. [DOI] [PubMed] [Google Scholar]
- 27. Bewick V, Cheek L, Ball J. . Statistics review 14: logistic regression. Crit Care. 2005; 9 1: 112– 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Akobeng AK. . Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007; 96 5: 644– 647. [DOI] [PubMed] [Google Scholar]
- 29. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. . Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. 2008; 50 3: 419– 430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Akobeng AK. . Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr. 2007; 96 3: 338– 341. [DOI] [PubMed] [Google Scholar]
- 31. Akobeng AK. . Understanding diagnostic tests 2: likelihood ratios, pre- and post-test probabilities and their use in clinical practice. Acta Paediatr. 2007; 96 4: 487– 491. [DOI] [PubMed] [Google Scholar]
- 32. Deeks JJ, Altman DG. . Diagnostic tests 4: likelihood ratios. BMJ. 2004; 329 7458: 168– 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dingenen B, Malfait B, Nijs S, et al. . Postural stability during single-leg stance: a preliminary evaluation of noncontact lower extremity injury risk. J Orthop Sports Phys Ther. 2016; 46 8: 650– 657. [DOI] [PubMed] [Google Scholar]
- 34. Krosshaug T, Steffen K, Kristianslund E, et al. . The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: a prospective cohort study of 710 athletes. Am J Sports Med. 2016; 44 4: 874– 883. [DOI] [PubMed] [Google Scholar]
- 35. Faul F, Erdfelder E, Lang AG, Buchner A. . G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39 2: 175– 191. [DOI] [PubMed] [Google Scholar]
- 36. Henry T, Evans K, Snodgrass SJ, Miller A, Callister R. . Risk factors for noncontact ankle injuries in amateur male soccer players: a prospective cohort study. Clin J Sport Med. 2016; 26 3: 251– 258. [DOI] [PubMed] [Google Scholar]
- 37. Fousekis K, Tsepis E, Vagenas G. . Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012; 40 8: 1842– 1850. [DOI] [PubMed] [Google Scholar]
- 38. Kofotolis ND, Kellis E, Vlachopoulos SP. . Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med. 2007; 35 3: 458– 466. [DOI] [PubMed] [Google Scholar]
- 39. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. . The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001; 29 2: 124– 128. [DOI] [PubMed] [Google Scholar]
- 40. Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, DePrince M. . Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001; 80 8: 572– 577. [DOI] [PubMed] [Google Scholar]
- 41. Finnoff JT, Hall MM, Kyle K, Krause DA, Lai J, Smith J. . Hip strength and knee pain in high school runners: a prospective study. PM R. 2011; 3 9: 792– 801. [DOI] [PubMed] [Google Scholar]
- 42. Nadler SF, Malanga GA, Solomon JL, Feinberg JH, Foye PM, Park YI. . The relationship between lower extremity injury and the hip abductor to extensor strength ratio in collegiate athletes. J Back Musculoskelet Rehabil. 2002; 16 4: 153– 158. [DOI] [PubMed] [Google Scholar]