Abstract
The American College of Academic International Medicine (ACAIM) represents a group of clinicians who seek to promote clinical, educational, and scientific collaboration in the area of Academic International Medicine (AIM) to address health care disparities and improve patient care and outcomes globally. Significant health care delivery and quality gaps persist between high-income countries (HICs) and low-and-middle-income countries (LMICs). International Medical Programs (IMPs) are an important mechanism for addressing these inequalities. IMPs are international partnerships that primarily use education and training-based interventions to build sustainable clinical capacity. Within this overall context, a comprehensive framework for IMPs (CFIMPs) is needed to assist HICs and LMICs navigate the development of IMPs. The aim of this consensus statement is to highlight best practices and engage the global community in ACAIM's mission. Through this work, we highlight key aspects of IMPs including: (1) the structure; (2) core principles for successful and ethical development; (3) information technology; (4) medical education and training; (5) research and scientific investigation; and (6) program durability. The ultimate goal of current initiatives is to create a foundation upon which ACAIM and other organizations can begin to formalize a truly global network of clinical education/training and care delivery sites, with long-term sustainability as the primary pillar of international inter-institutional collaborations.
Key Words: Academic International Medicine, comprehensive framework for international medical programs, International Medical Programs, The American College of Academic International Medicine
FOREWORD
The American College of Academic International Medicine represents clinicians from every specialty and from every discipline of the health sciences. Our membership includes practitioners from around the world. The following consensus statement is intended to represent the physician voice to and from every field of medicine.
INTRODUCTION
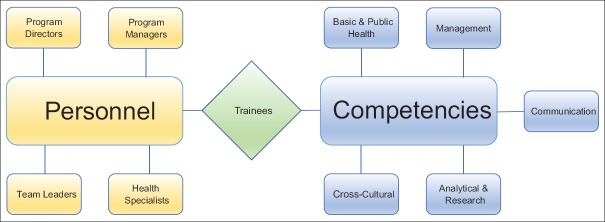
Significant disparities in health care delivery persist between high-income countries (HICs) and low-and-middle-income countries (LMICs). International Medical Programs (IMPs) are an important mechanism of American medical outreach to address these inequalities. IMPs are international partnerships that use primarily education and training-based interventions, broadly defined in this consensus as Academic International Medicine (AIM), to build local clinical capacity in low-resource settings [Figure 1]. Professional and ethical frameworks for research-based international medical partnerships and participation in short-term international training experiences exist;[1,2,3] however, few guidelines are available to support the design, development, and wider adoption of IMPs. In practice, IMPs face a variety of challenges including, but not limited to, lack of sustainability; inconsistent funding and resources; poorly defined structure; and non-specific long-term goals and/or deliverables. When several HICs collaborate, poor interinstitutional coordination can result in confusion, misallocation, and maldistribution of limited resources.[4]
Figure 1.
Definitions of Academic International Medicine and International Medical Programs
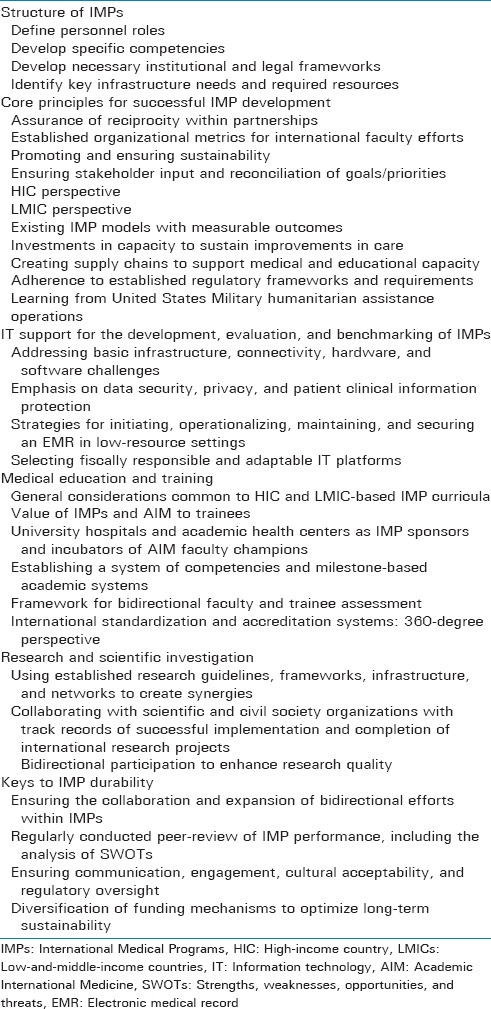
This consensus statement outlines key issues and core principles, identified during the 2017 AIM Congress by the leadership of American College of Academic International Medicine (ACAIM). Here we introduce the Comprehensive Framework for International Medical Programs (CFIMPs) with the goal to promote and improve access to quality medical care globally. The CFIMPs [Table 1] highlights key aspects of IMPs including: (1) structure; (2) core principles for ethical development; (3) information technology; (4) medical education and training; (5) research and scientific investigation; and (6) program durability.
Table 1.
Outline of the American College of Academic International Medicine Comprehensive Framework for International Medical Programs (CFIMPs)
RATIONALE FOR INTERNATIONAL MEDICAL PROGRAMS
Institutions across the United States (US) have worked diligently to advance medicine worldwide through the prism of bidirectional development. In LMICs, there is growing demand for the attainment of enhanced quality of patient care, including standardized practices, clinical protocols, and technological implementations. There is a growing need to invest in access and outcome-based policies to enhance local health care infrastructure, workforce, and capacity in resource-limited settings.[5]
It is difficult to improve health systems without first ensuring that basic infrastructure and resources are present. Paul Farmer has referred to these needs as the “four S's” of “staff, stuff, space, and systems.”[6,7,8] IMPs are instrumental in supplying knowledge, technology, and effective care to people living in regions with limited health care resources and/or care delivery platforms. Moreover, IMPs provide personnel and logistics to support sustainable efforts in partner communities while facilitating the translation of current concepts and medical advances into improved clinical outcomes. For clarity, IMPs are not “global health” (GH) programs where public health experts focus on the performance of research in LMICs. In this context, the objective of IMPs is to work in tandem with GH researchers to ensure the optimization of structure and function of clinical enterprises, supporting the provision of high-quality, timely and affordable care. At the same time, IMPs should strive to ensure safe and well-structured environments for medical education and training.[9,10] These core concepts serve as the rationale to advance IMP bidirectional exchange, where participants of low-resource countries are able to engage in education and training opportunities in high-resource settings.
THE STRUCTURE OF INTERNATIONAL MEDICAL PROGRAMS
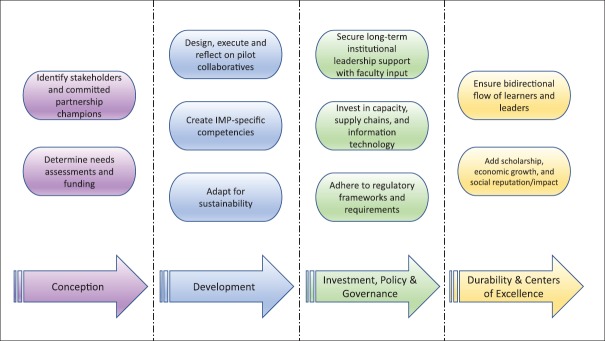
There are four main personnel roles in IMPs: program directors, program managers, team leaders, and health specialists.[11] Program directors oversee all IMP operations, champion collaborative vision, and set administrative, educational/training, and research goals. Program managers are responsible for day-to-day operations, regulatory and compliance documentation, and facilitate the interaction between trainees and the clinical/academic environment. Team leaders directly supervise trainees during patient care. Health specialists serve as short- or long-term advisors, program officers, or consultants. Together these roles provide complimentary personnel for successful IMPs structuring [Figure 2].
Figure 2.
International Medical Program structure organized by personnel needs and competencies. Trainees are integral to the model as they supply an expanded work force that can advance to a personnel role. Trainees also shape and are educated via the competencies. Partnerships should designate and create site-specific structure for sustainability and academic validity[11]
Core competencies fall into five general categories: (1) basic and public health skills, (2) management skills, (3) communication skills, (4) cross-cultural skills, and (5) analytical and research skills Figures 2 and 3.[11,12]
Figure 3.
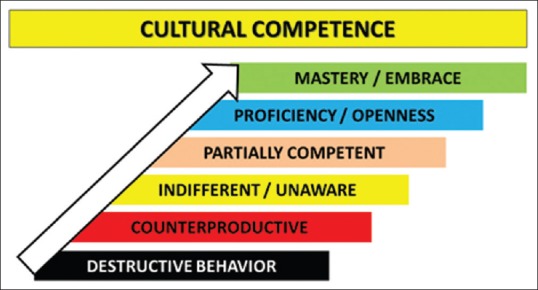
The continuum of cultural competence. International Medical Programs should strive to embrace bi-directional mastery within each domain[12]
Basic and public health skills are subdivided into public health, disease control, and prevention competencies.[13] Intuitively, appropriate technical expertise and sound understanding of the epidemiology and pathology of diseases can help achieve project outcomes.
Management skills are subdivided into financial, human resource, administration, and contact-related competencies. IMP personnel must be adept at policy formulation, planning and development, and multidisciplinary team building as these are critical management skills.[11]
Communication skills are subdivided into negotiations, mentoring, conflict resolution, and advocacy competencies. Other important communication skills include English language fluency, sufficient proficiency in pertinent site-specific languages, as well as technical/specialist consultation or advisory skills.[11,14]
Cross-cultural skills are essential to IMP work and include the ability to communicate effectively with people from different socioeconomic, ethnic, and cultural backgrounds.[15,16] In LMICs, clinicians must be able to work independently in complex social and cultural settings with extremely limited resources and high poverty levels. IMP personnel should be able to adapt to diverse educational and cultural backgrounds, and interface effectively with both public and private sectors while exhibiting culturally sensitive professional standards of conduct.
Finally, IMP personnel should possess fundamental analytical and research skills (including research ethics) in accordance with international standards and guidelines.[11] They need to develop necessary institutional and legal frameworks and identify key infrastructure needs and required resources. For each of the above competencies, IMPs should aim to achieve mastery of cultural competence and integration [Figure 3].[12] The ethnocentrism-ethnorelativism continuum of intercultural sensitivity as it pertains to the current discussion is presented in Figure 4.[17]
Figure 4.
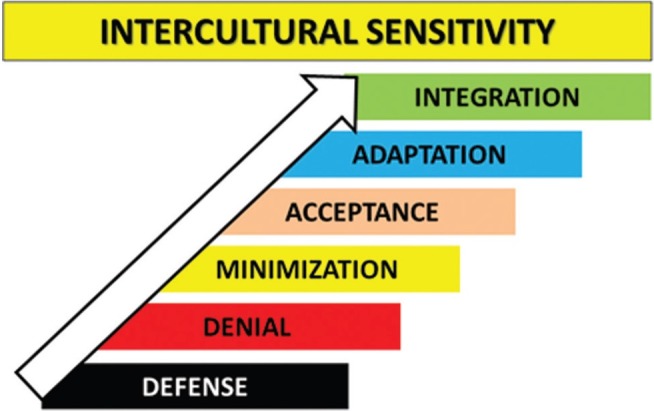
The continuum of intercultural sensitivity. International Medical Programs should embrace bidirectional ethnorelativism[17]
CORE PRINCIPLES FOR SUCCESSFUL DEVELOPMENT OF INTERNATIONAL MEDICAL PROGRAMS
AIM serves an important role in both HIC and LMIC health systems.[18] An effective AIM approach is to develop or work within partnerships built on shared goals and objectives as the platform for international exchange. Considerable time and effort is required to build the level of trust; mutual understanding and experience needed to achieve transparent and productive relationships; and the understanding of needs, aims, and mechanisms.[19] Reciprocal benefits and liabilities should be thoughtfully examined and clearly communicated. This investment of faculty time and effort should be quantified using organized metrics to ensure successful development of IMPs. Although partnerships involved in each IMP will be unique in their aims and applications, some general themes apply. The following are several commonly encountered perspectives presented as a platform for discussion as part of the CFIMPs.
PROMOTING SUSTAINABILITY: AVOIDING THE “VOLUNTOURISM” TRAP
IMPs must be thoughtfully designed and implemented to achieve measurable institutional and societal benefit. The term “voluntourism” has been used to describe the practice, whereby travelers from HICs participate in voluntary work within LMICs.[20,21] While this form of medical outreach is genuinely motivated by a desire to help others, it may easily be perceived as a self-serving “vacation”, unregulated skills acquisition, or pseudo-academic activity to enhance one's professional resume. The lack of proper organizational framework or supervision also puts into question the integrity of such unstructured medical trips. Short-term “volunteer vacations,” “drive-by humanitarianism,” and “parachute medicine” rarely have sustainable impact on the host environment and raise ethical and moral concerns about international medical outreach in general.[10,20,22,23,24,25]
Promoting sustainability involves short-, intermediate-, and long-term commitments (e.g., dedication to consistent presence), bidirectional exchange of personnel and trainees with reciprocal agreements (i.e., starting student/resident electives with memoranda of understanding, consideration of international faculty appointments, etc.), operational/logistical support, and the development of IMP champions on both sides. Joint needs analysis, with dissemination and implementation of corresponding plans, are both critical to successful IMP outcomes. The benchmarking process should include periodic assessments of goals, highlighting achievements and addressing failures, anticipating emerging target areas of focus, and securing financial and personnel support.[26,27]
HIGH-INCOME COUNTRY PERSPECTIVE
From an organizational perspective, participation in IMPs supports HIC institutional excellence by enhancing national and international impact. IMP participation also serves to attract high-quality trainees and faculty. It has been suggested that future physicians cannot serve impoverished communities effectively without first understanding the structural forces that contribute to societal inequalities.[6] International rotations have grown exponentially over the last decade, and well-structured programs influence trainee choices in undergraduate and graduate medical education and fellowship.[9] International electives provide rich learning opportunities to demonstrate professionalism, practice-based learning, and system-based practice (SBP), competencies challenging to teach in a homogeneous learning environment.[28] Despite evidence that international clinical electives can be educationally and professionally beneficial to both high-resource and low-resource country trainees, participation remains challenging for American residents.[29] Only 59% of residency programs offer international clinical rotations to residents, and as few as 10% of residents participate when such opportunities are available.[30] Students participating in IMPs develop improved cultural sensitivity, clinical and communication skills, resource utilization, and are more likely to work in underserved areas upon training completion.[31,32] Faculty serving in LMICs are better prepared to model and teach important skills not otherwise obtainable at home. The institutional benefit of LMIC work includes more patient-centered clinical care, improved community relations, and potential for “reverse innovation” to improve health-care quality through exposure to new ideas and processes that are effective in other systems.[18,33,34]
Although AIM training is not regulated by the Accreditation Council for Graduate Medical Education (ACGME) certification requirement, the ACGME competency-based assessment requirements may provide an important framework for IMP-based education.[35] AIM training programs should incorporate common goals for clinical care oversight and faculty development.[36,37] Published clinical practice models may provide a template for collaboration in this domain.[38,39]
LOW-AND-MIDDLE-INCOME COUNTRY PERSPECTIVE
IMPs are founded on mutual, bidirectional benefit. This may include any combination of personnel, physical resources, electronic reference access, didactic opportunities, research collaboration, educational exchanges, or formal mentorship.[40,41] Care must be taken to ensure that HIC learners do not impede LMIC learner education by diverting resources, cases, or procedures. Conversely, LMIC learners should benefit from short-term rotations in HICs, encouraging the exchange and import of skills, ideas, and perspectives needed to become the leaders of advancement or change in their home countries. When accepting reciprocal LMIC learners, IMPs should encourage policies that discourage the “brain-drain” phenomenon. It is counterproductive when LMIC students and medical personnel travel to HICs to pursue alternative training and upon completion settle in the HICs rather than returning home with their valuable knowledge and skill set.[42]
Retention programs with financial and sociopolitical incentives are key to promoting the development of local expertise.[40,43] Programs that expand local capacity should be supported by all stakeholders, including governments. An example is the human resources in health program run by the Rwandan Ministry of Health and supported by the Clinton Health Access Initiative. Highlights include long-term (i.e., 1-year) HIC faculty commitment to help develop Rwandan faculty and a gradual phasing out of HIC faculty as Rwandan trainees gradually move into full-time faculty positions to ensure program sustainability.[44,45] Similarly, the Afya Bora (Swahili for “Better Health”) Consortium, formed in response to the need for qualified health care leaders, consists of five Africa-US partnerships in Botswana, Kenya, Uganda, Tanzania, and Cameroon.[46] The consortium works to develop a powerful collaboration by merging and consolidating education, training, and research experiences and resources. A focused mission prepares future global leaders for careers in health care settings to leverage governmental and nongovernmental organizations (NGOs) to transform health care delivery systems to better serve the citizens of LMICs.[46]
INVESTMENTS IN CAPACITY TO SUSTAIN IMPROVEMENTS IN CARE
Education is most effective as a tool for change if it addresses not only “what” to do differently but also “how” and “why” to do it. IMPs should consider the totality of structural, socioeconomic, and institutional resources, along with the barriers that impact clinical change processes when designing and implementing interventions. Achieving sustainable improvements in clinical care require that programs also address specific intervention and initiative implementation within the existing LMIC service structure and systems. Workforce, quality assurance, and research capacity must be addressed in addition to clinical skills training. Importantly, material resources to sustain or measure the impact of desired changes strengthen the ability of partners in LMICs to translate education and training into improved downstream processes and health outcomes.
CREATING SUPPLY CHAINS TO SUPPORT MEDICAL AND EDUCATIONAL CAPACITY
Needs assessments performed before IMP initiation ensure that plans and supply chains are appropriate and sustainable. Ideally, IMPs can leverage available equipment and maintenance contracts from existing local organizations. Basic supplies may be locally available, but it is critical to ensure that ample resources to sustain improvements are in place to support patient care and subsequent education and training initiatives. When selecting locations, the understanding of the low-resource site equipment and infrastructure landscape is advantageous. Donated supplies that fit the needs assessments and are compatible with locally available components are crucially important. ACAIM does not advocate the use of expired supplies, and any reuse of supplies must be made on a case-by-case basis as determined by the inter-institutional collaborative agreement. Moreover, all stakeholders need to agree on supply quality standards to maximize care safety and efficacy. For most IMPs, logistical issues are common and usually addressable within the context of local cultural, local social, and economic considerations. However, advanced planning and care ensures that local custom requirements and pathways are well understood before shipping so that recipients are able to receive and use donated items without undue expense.
ADHERENCE TO ESTABLISHED REGULATORY FRAMEWORKS AND REQUIREMENTS
The most pernicious variety of “voluntourism” exists when private placement organizations promote and elevate HIC volunteers in expert roles while discounting LMIC health workers with relevant training, superior skills, and contextual knowledge.[47] Even highly experienced clinicians need to develop cultural and SBP competencies to practice safely and effectively in new environments. It is critical that medical students, residents, and other unlicensed participants do not engage in unsupervised medical activities and/or perform procedures that they are not permitted to perform in their home countries.[24] Within this broader context, IMPs may help ensure that adequately licensed, prepared, and motivated participants adhere to regulatory frameworks (local and international), medicolegal implications, and clinical practice standards relevant to their proposed activities. Particularly, when trainees from HICs are (or may become) involved in direct patient care decisions in LMICs, the HIC institution has a duty to provide adequate predeparture training, supervision, and oversight. Rules and regulations (including credentialing) are predetermined and agreed upon by all participants to prevent health care outside professional scope and training. This requires that HIC institutions recognize and support the involvement of dedicated faculty in the process.
Minimum accreditation standards are urgently needed to help facilitate safe and effective IMP development. Professional hospital and training program accreditation organizations such as the Joint Commission International are well placed to lead in this domain.[48] ACAIM members may make visits to accrediting partners with the expressed purpose of cooperation and bidirectional information sharing. Among our near-term goals, a dedicated ACAIM taskforce will develop and maintain an edited resource guide to assist institutions from HICs and LMICs with milestones, regulatory frameworks, and requirements.
LEARNING FROM UNITED STATES MILITARY HUMANITARIAN ASSISTANCE OPERATIONS
The US military frequently engages in global humanitarian aid and consequently can offer significant knowledge and experience in this domain. Historically, it was noted that the Department of Defense humanitarian assistance program achieved improved outcome-based measures of effectiveness by utilizing medical after-action reports, analyses of lessons learned, and expert-based feedback on internationally accepted standards in humanitarian assistance.[49,50] Coordinated efforts were subsequently made to disseminate emergency management experiences in the following content areas: (1) planning of regional/global collaboration with public–private cooperation; (2) international humanitarian action; (3) coordination of leadership; (4) ethics in disaster management; (5) resilience management; (6) training programs and exercises; (7) human resources; (8) communication; and (9) civil-military cooperation.[51] Global medical humanitarian efforts generally lag behind the military, and thus, there are many clinical and operational experiences that can help shape IMP development.
Military personnel undergo specialized preparation that is potentially relevant to IMP leadership. One example is diplomacy training that exists for military physicians who deploy internationally.[52] Core concepts range from understanding governance and international cooperation to practical challenges in collaborative research and capacity building. Finally, academic institutions can draw parallels between IMP and military deployments among their faculty members, especially in terms of approaches to accounting for clinical productivity and deployment-related logistics.
INFORMATION TECHNOLOGY SUPPORT FOR THE DEVELOPMENT, EVALUATION, AND BENCHMARKING OF INTERNATIONAL MEDICAL PROGRAMS
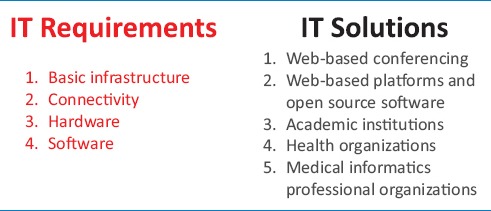
In LMICs, information technology (IT) challenges are pervasive. Opportunities for improvement can be found in the following areas: (1) basic infrastructure (e.g., electricity availability and reliability); (2) connectivity (e.g., data sharing, internet access, wireless, and wide area network); (3) hardware (e.g., computers, tablets, servers, printers, backup technology, peripherals, and interface devices); and (4) software (e.g., EMR systems, patient photographs, and disease progression picture archival).[53,54] A critical emphasis needs to be placed on ensuring data security, privacy, and appropriate mechanisms to protect patient clinical information.
Strategic IT investments facilitate effective communication, which is critical to effective IMP operations. For example, implementing technology to support web-based conferencing may have great value.[55,56,57] Partnerships for initiating, operationalizing, maintaining, and securing an EMR in LMICs may seem daunting, but experience and technological advances suggest otherwise.[58] Web-based platforms and open-source software are available and may help defray costs associated with initiating and maintaining EMR systems in LMICs.[59] With decreasing costs, greater performance and reliability, and a smaller device footprint-storage capacity ratio, the reality of providing and supporting some type of inexpensive and adaptable IT platform is integral to contemporary IMP efforts. Important considerations regarding the design and implementation of IT and information management solutions are presented in Table 2.
Table 2.
Information technology requirements and solutions for successful international medical information management programs
MEDICAL EDUCATION AND TRAINING
Trainee IMP participation has increased steadily over the past 3 decades. In 1984, 6% of graduating US medical students took part in international health electives; this number has increased significantly since then, with medical students self-reporting GH experiences on the Association of American Medical Colleges Graduate Questionnaire in the range of 20-30%.[60] Despite growing interest, most trainees are unable to participate in IMPs.[30] This may represent a missed opportunity since the value of educational involvement in AIM can be substantial for trainees. International learning experiences may be empowering and the highlight of one's training.[61,62] Moreover, many trainees report a heightened sense of social responsibility, improved cultural sensitivity, and improved clinical and communication skills following IMP participation. Nearly 95% say it increased the likelihood they would volunteer with low-resource populations in the future.[31,32,63,64] Despite evidence that international clinical electives can be educationally and professionally beneficial to both HIC and LMIC trainees, bidirectionality remains challenging to secure. Even when logistically feasible, elective rotations can be inconsistently structured.[29] It is critical that participating trainees experience first hand the health-care needs of the international community in an organized and consistent manner.
AIM provides unique knowledge and competencies that are currently underrepresented in medical education. For example, it expands trainees' immigrant health knowledge, particularly in socioeconomically disadvantaged communities.[33] Trainees must be prepared for these knowledge and competency needs prior to an AIM experience. Ideally, predeparture preparation for trainees participating in international electives includes both classroom and immersive experiential components.[36] Among program directors who reported resident participation in international rotations (approximately 73%), only 15.4% reported predeparture training specific to working abroad. In addition, only 47% of responders knew if liability insurance covered the residents' work, while 31% were not covered and 22% were unaware of coverage. Furthermore, only 45% of the international rotation sites had been evaluated for safety by a faculty member.[36] Targeted predeparture training, dedicated faculty supervision, professional liability insurance agreements, and site-specific safety vetting are essential parts of the CFIMPs. Multiple solutions to the issues described above have been proposed. Aforementioned published practice and curriculum models may be of benefit,[38,39] and bidirectional faculty development may be optimized using universally available web-based resources.[37]
The global society is becoming increasingly interconnected. IMPs provide experiential education and opportunities for professional development while allowing trainees to contribute as global citizens. Participants attain valuable knowledge and skills, including cultural competence.[65] Structured exposure to technology-limited practice settings sharpens history and physical examination skills, encouraging more efficient resource utilization. Trainees may also become more familiar with unusual or advanced disease processes and gain functional plasticity (i.e., operational SBP skills) by learning how to navigate very different health care systems [Figure 5].
Figure 5.
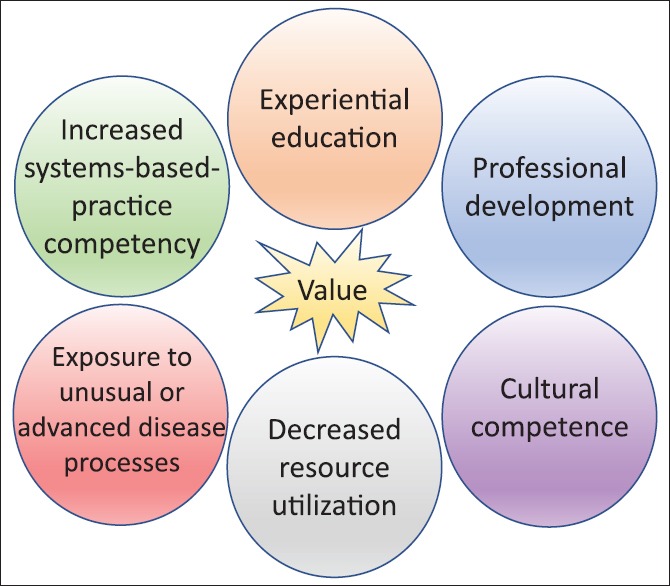
The value of International Medical Programs and Academic International Medicine to trainees
Clinical care, education, and research are the traditional pillars of academic medical practice. Through their leadership in these domains, teaching hospitals help establish and maintain best practices and standards of care. IMPs seek to incorporate these state-of-the-art processes and practices across their international partnerships through the development of AIM faculty champions. Such institutional AIM champions must effectively integrate local and global health delivery plans with their departmental and college leadership while being mindful of organizational strategic alignments and plans.[70,71,72]
IMP-BASED MEDICAL TRAINING: ESTABLISHING COMPETENCIES AND MILESTONES
Trainees participating in IMPs can fulfill ACGME competencies of patient care, professionalism, practice-based learning and improvement, interpersonal and communication skills, medical knowledge, and SBP. SBP is perhaps the most gradual of the ACGME competencies to master because it requires good understanding of different health care systems, knowledge of safety and quality principles, and the ability to successfully navigate health care economics. By requiring the participant to engage in a complex operational system intended to continually improve organizational performance and resource-utilization, IMPs uniquely augment a trainee's ACGME specialty-specific achievement of SBP milestones.[66] ACAIM aspires to create appropriate AIM milestones to assist trainees in their professional development, across various specialties, and more importantly with the valuable input and participation of both LMIC and HIC faculty members.
FRAMEWORK FOR BIDIRECTIONAL FACULTY AND TRAINEE ASSESSMENT
Program assessments should occur before, during, and after IMP rotations, incorporating bidirectional trainee and faculty feedback. Assessment tools developed collaboratively with international faculty should take into account environment-specific cultural norms.[67] It is important for trainees to perform planned self-assessment, focusing primarily on general ACGME competencies and milestones. Trainees may also receive assessments specific to their IMP-based educational experience (i.e., patient care versus research). ACAIM will create a task force to examine a collaborative framework that guides bidirectional faculty and trainee assessment.
INTERNATIONAL STANDARDIZATION AND ACCREDITATION SYSTEMS: 360-DEGREE PERSPECTIVE
Physician competency expectations can vary widely between countries. Practice prerequisites ensure that care of consistent quality is delivered.[18] In 2004, the WHO and World Federation for Medical Education partnered to develop accreditation standards for basic medical education.[68] This partnership contributed to better clinical training and improved standardized test performance across a broad range of settings. The ACGME has also expanded its global presence with the ACGME-International. This new entity has received a positive reception from international medical students, and many countries have adopted its standardized accreditation systems.[69] ACAIM will utilize a multidisciplinary consensus group to promote thoughtful standardization, accreditation, and harmonization of metrics with existing organizations. Strategic IMP-centric ACAIM planning initiatives are highlighted in Figure 6.
Figure 6.
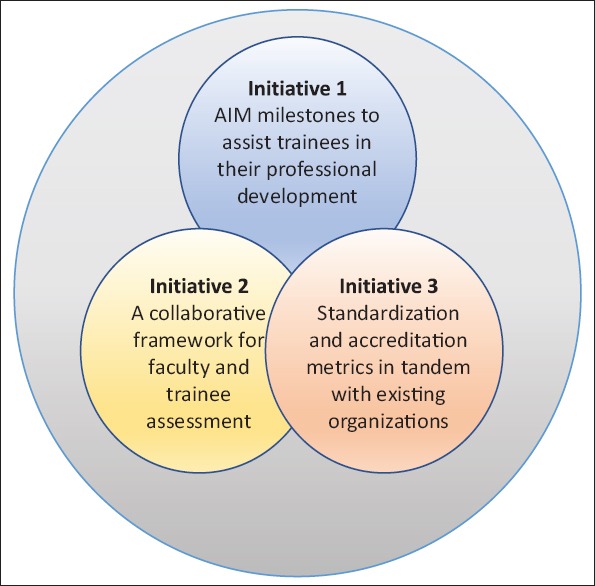
American College of Academic International Medicine International Medical Program strategic planning initiatives
RESEARCH AND SCIENTIFIC INVESTIGATION
Research and analytical skills are among the core competencies of international health workers.[11] Reasons to engage in AIM or GH research begin with data needs for regional, national, and global population health indicators.[73] Currently, the quality and reliability of captured data can be highly variable.[37] Some countries do not have institutional review boards (IRB), informed consent processes, or systems for patient protection in research.[37] IMPs may participate in research to: (1) improve study quality; (2) teach study design methodologies, (3) develop informed consent procedures and/or IRBs, (4) enhance population access to clinical studies, (5) increase sample size, (6) decrease study completion times, and (7) improve research proposal competitiveness.[37] Collaborations may be based on local, virtual, or hybrid presence. Beyond study design, IMP personnel may serve as advisors, co-investigators, or assist with statistical analyses, manuscript or grant writing, and publishing.[37]
Researchers should utilize appropriate guidelines for the reporting of health-care research as outlined by the Enhancing the Quality and Transparency of Health Research Network.[74] In addition, the Guidelines for Accurate and Transparent Health Estimates Reporting were created to define best practices for documenting studies that report on global health outcomes.[74] Although compliance with these guidelines is not an absolute indicator of study quality, it does ensure that key information is available so that an informed reader can judge the study's quality and use results appropriately.[73]
RESEARCH AND CIVIL SOCIETY ORGANIZATIONS
When conducting international research, investigators are encouraged to engage with local civil society organizations (CSOs). Common in LMICs, CSOs are nonprofit organizations that aim to enhance the well-being and prosperity across communities. Motivated to protect and empower the vulnerable, CSOs work in areas such as community development, service provision, advocacy, activism, and research.[75] Of note, research and advocacy are among the main CSO health sector functions, along with service provision, social welfare and support activities. They are at the forefront of supporting innovations intended to solve challenging issues facing local communities. IMP–CSO partnerships are important to ensuring that research efforts help improve the well-being of involved communities.[75] CSOs are able to constructively impact research agendas by providing appropriate contextual framework for both governments and researchers.[75] Conversely, they can disrupt scientific endeavors if they deem scientific premises invalid or harmful to the local communities, as occurred when ACT UP Paris successfully campaigned to halt the anti-HIV Tenofovir trials (Gilead Sciences, Inc.) in Cambodia and Cameroon.[76,77]
CSOs come in five types: (1) NGOs, (2) community-based organizations, (3) faith-based organizations, (4) voluntary health organizations, and (5) networks.[75] NGOs work outside direct government control and can be local, national, or international.[78] Community-based organizations draw membership from the communities they serve.[75] Faith-based organizations draw the purpose of their work from a particular religious belief and may work through local centers of faith.[75] Volunteer health organizations often focus on a specific disease or syndrome (e.g., diabetes or hypertension) and promote research and trial participation, treatment access, and aid for the afflicted. Finally, networks are groups comprised of various organizations and individuals that converge around common issues.[75]
CSOs may assist research through advocacy with policy-makers and various funding sources. They may function as a community interface and may be an access point to vulnerable or stigmatized communities (e.g. refugees).[75] Furthermore, many CSOs are research-focused and contain experienced biomedical and social scientists, representing an often underutilized resource for collaboration on areas such as epidemiology, social sciences, product development, knowledge translation, health services, and policy research.[75] Finally, CSOs are critical when determining if proposed research is in the best interests of the local communities, ensuring respect toward their views and rights.[75]
KEYS TO IMP DURABILITY
We highlight 16 keys to navigating successful international partnerships to ensure durability [Table 3].[25]
Table 3.
Key concepts important to developing successful IMPs and ensuring program durability (adapted from John et al.[25])
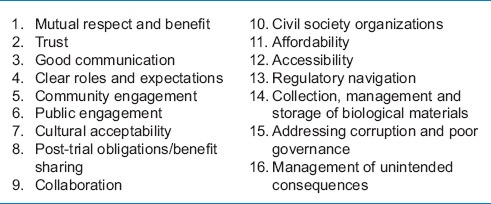
The inclusion of international collaborators as colleagues will promote reciprocal long-term relationships.[25] Conversely, paternalistic attitudes (e.g., “I know what's good for you”) will impede progress.[25] Transparency, frequent communication, sharing a common vision, early definition of clear roles and expectations, and planning for future studies with site primary investigators can facilitate mutual trust.[25] Moreover, maintaining humility, power differential awareness, collaborative action, and accountability is critical for durable efforts.[79]
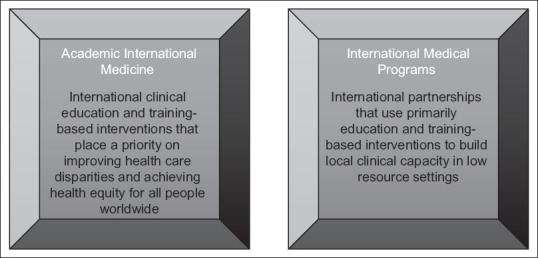
The authors of this ACAIM consensus thus present a model for IMP viability [Figure 7]. Collaborators will navigate viability phases from conception to durability in a time frame dependent on the experience/commitment of the participants and the resources available. During the conception phase, collaborators will identify stakeholders and determine needs assessments and funding sources. This will be critical to ensure bidirectional accountability, supervision, and financial resource allocation. During the second phase of development, collaborators will design, execute and reflect on pilot experiences. This will lead to the creation and refinement of IMP-specific competencies and sustainability. During the third phase of investment, policy and governance, collaborators will secure long-term institutional support; create investments in capacity, supply chains and information technology; and adhere to regulatory requirements to ensure continued promulgation with institutional leaders in the proper framework. During the final phase of durability and centers of excellence, collaborators will ensure bidirectional flow of learners and leaders and add scholarship opportunities (i.e., peer-reviewed publications, scientific presentations), economic growth (i.e. grant funding, donations), and social reputation/impact (i.e. positive community outcomes, global community public relations). The authors encourage thoughtful establishment of site-specific IMP viability with the above model.
Figure 7.
Key factors critical to International Medical Program viability. Each of the color-coded phases may take between 1-2 years to complete
Community engagement is essential for high quality, effective, and ethical IMP conduct.[80,81] It serves to facilitate better understanding, permission, mutual ownership, and organizational legitimacy. Public engagement is a bidirectional process that provides individuals with trustworthy information (e.g., radio, newspapers, television, social media, schools, churches, etc.) on key policy issues. It then elicits input, and integrates it into decision-making and social action.[80] The prioritization of IMP efforts toward ensuring cultural acceptability of a proposed project and its seamless integration in a culturally inclusive manner is critical to successfully managing any potential unintended consequences.
Two-way processes that strengthen the capacity and collaboration between public and private sectors in low resource settings create sustainable science and technology infrastructure.[80] Furthermore, access to knowledge and technology must be affordable and accessible, both being ethical concepts rooted in the notion of equity.[80]
CONCLUSIONS
Global connectivity is growing at an exponential rate. This manuscript outlines the CFIMP as well as key steps for fostering successful international collaboration within the proposed framework. As an US representation for the AIM community, ACAIM's goal is to help create a platform that will foster the creation and durability of high quality, viable IMPs. It is our hope that such IMPs will help facilitate closer inter-institutional, interdisciplinary, cross-cultural, and bidirectional collaborations. We also believe that it is the model of shared governance and shared responsibility that will produce the most optimal long-term results for both US-based participants and their international counterparts around the globe. We invite all health-care providers to share their knowledge and commitment with us. This, in turn, will allow the AIM community to create, disseminate, and implement the necessary knowledge, experience, innovation, understanding, and reproducibility across existing and new IMPs.
CONSENSUS TEAM LEADERSHIP CONTACT INFORMATION
Manish Garg, MD, FAAEM, President-Elect of ACAIM, Professor and Senior Associate Residency Program Director, Temple University Hospital Department of Emergency Medicine, Director of Global Medicine at Lewis Katz School of Medicine at Temple University, Philadelphia, PA; E-mail: Manish. Garg@tuhs.temple.edu; Twitter: @TheGargFather
Gregory Peck, DO, FACS, Member, ACAIM Board of Governors, Associate Director of Acute Care Surgery Fellowship, Associate Director of Trauma, Rutgers– Robert Wood Johnson Medical School, New Brunswick, NJ; E-mail: peckgr@rwjms.rutgers.edu; Twitter: @DrGregoryPeck; Facebook: @RUglobalsurgery
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This consensus statement is being published across all ACAIM-sponsored periodicals (International Journal of Critical Illness and Injury Science and International Journal of Academic Medicine) as requested by the combined ACAIM Boards of Governors and Directors as well as the Multidisciplinary Consensus Group on IMPs. Justifications for parallel publication of this important material include wider dissemination of knowledge and significant differences in readership distribution of both periodicals. The parallel publication of this document has been approved by editors of both journals and by all co-authors of this scholarly work.
Members of the Multidisciplinary Consensus Group on International Medical Programs included (complete alphabetical list): Bonnie Arquilla (Brooklyn, NY); Harry L. Anderson III (Ann Arbor, MI); Christina Bloem (Brooklyn, NY); Jordan Kapper (Bethlehem, PA); Silvana Dal Ponte (Porto Alegre, Brazil); Paula Ferrada (Richmond, VA); Sagar C. Galwankar (Tampa, FL); Ramon E. Gist (New York, NY); Vicente H. Gracias (New Brunswick, NJ); Weidun Alan Guo (Buffalo, NY); Bhakti Hansoti (Baltimore, MD), Ricardo Izurieta (Tampa, FL), Marian McDonald (Allentown, PA), Alaa-Eldin A. Mira (Bethlehem, PA), Sudip Nanda (Bethlehem, PA); Chinenye O. Nwachuku (Bethlehem, PA); Benedict Nwomeh (Columbus, OH); Thomas J. Papadimos (Toledo, OH); Gregory L. Peck (New Brunswick, NJ); Scott Plantz (Tampa, FL); Richard P. Sharpe (Phillipsburg, NJ); Ziad C. Sifri (Newark, NJ); Sari Soghoian (New York, NY); Stanislaw P. Stawicki (Bethlehem, PA); and Mamta Swaroop (Chicago, IL).
The authors would also like to acknowledge the following individuals for their support during the consensus planning and drafting process: Charles H. Cook (Boston, MA); Susan D. Moffatt-Bruce (Columbus, OH); Mayur Narayan (New York, NY); James P. Orlando (Bethlehem, PA); Kiran C. Patel (Tampa, FL).
REFERENCES
- 1.Larkan F, Uduma O, Lawal SA, van Bavel B. Developing a framework for successful research partnerships in global health. Global Health. 2016;12:17. doi: 10.1186/s12992-016-0152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crump JA, Sugarman J. Working Group on Ethics Guidelines for Global Health Training (WEIGHT). Ethics and best practice guidelines for training experiences in global health. Am J Trop Med Hyg. 2010;83:1178–82. doi: 10.4269/ajtmh.2010.10-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhutta ZA. Ethics in international health research: A perspective from the developing world. Bull World Health Organ. 2002;80:114–20. [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson HL, 3rd, Arquilla B, Firstenberg MS, Garg M, Galwankar SC, Gracias VH, et al. Mission statement of the American College of Academic International Medicine. Int J Crit Illn Inj Sci. 2017;7:3–7. doi: 10.4103/IJCIIS.IJCIIS_13_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philibert I. International medical education outreach: Benefits for US medical education and practice: An interview with Joseph Kolars, MD. J Grad Med Educ. 2009;1:162–3. doi: 10.4300/01.01.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drobac P, Morse M. Medical education and global health equity. AMA J Ethics. 2016;18:702–9. doi: 10.1001/journalofethics.2016.18.7.medu1-1607. [DOI] [PubMed] [Google Scholar]
- 7.Farmer P. Diary. Vol. 36. London, England: London Review of Books; 2014. pp. 38–9. [Google Scholar]
- 8.Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA, et al. Global access to surgical care: A modelling study. Lancet Glob Health. 2015;3:e316–23. doi: 10.1016/S2214-109X(15)70115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P, et al. Global health in medical education: A call for more training and opportunities. Acad Med. 2007;82:226–30. doi: 10.1097/ACM.0b013e3180305cf9. [DOI] [PubMed] [Google Scholar]
- 10.Hanson L, Harms S, Plamondon K. Undergraduate international medical electives: Some ethical and pedagogical considerations. J Stud Int Educ. 2011;15:171–85. [Google Scholar]
- 11.Akbar H, Hill PS, Rotem A, Riley ID, Zwi AB, Marks GC, et al. Identifying competencies for Australian health professionals working in international health. Asia Pac J Public Health. 2005;17:99–103. doi: 10.1177/101053950501700207. [DOI] [PubMed] [Google Scholar]
- 12.Cross TL. Toward a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children who are Severely Emotionally Disturbed. Washington, DC: Georgetown University Child Development Center; 1989. [Google Scholar]
- 13.Aschengrau A, Seage GR. Essentials of Epidemiology in Public Health. Burlington, MA: Jones & Bartlett Publishers; 2013. [Google Scholar]
- 14.Fulmer HS, Adams AC, Deuschle KW. Medical student training in international cross-cultural medicine. J Med Educ. 1963;38:920–31. [PubMed] [Google Scholar]
- 15.Johnson JP, Lenartowicz T, Apud S. Cross-cultural competence in international business: Toward a definition and a model. J Int Bus Stud. 2006;37:525–43. [Google Scholar]
- 16.Le Roux J. Effective educators are culturally competent communicators. Intercult Educ. 2002;13:37–48. [Google Scholar]
- 17.Bennett MJ. Developmental Model of Intercultural Sensitivity. Hoboken, NJ: Wiley Online Library; 1998. [Google Scholar]
- 18.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–58. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 19.Wall AE. Ethics for International Medicine: A Practical Guide for Aid Workers in Developing Countries. Lebanon, NH: University Press of New England; 2012. [Google Scholar]
- 20.McLennan S. Medical voluntourism in Honduras: ‘Helping’ the poor? Prog Dev Stud. 2014;14:163–79. [Google Scholar]
- 21.Snyder J, Dharamsi S, Crooks VA. Fly-by medical care: Conceptualizing the global and local social responsibilities of medical tourists and physician voluntourists. Global Health. 2011;7:6. doi: 10.1186/1744-8603-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.deVries CR, Price RR. Global Surgery and Public Health: A New Paradigm. Sudbury, MA: Jones & Bartlett Publishers; 2012. [Google Scholar]
- 23.Dupuis CC. Humanitarian missions in the third world: a polite dissent. Plastic and reconstructive surgery. 2004;113:433. doi: 10.1097/01.PRS.0000097680.73556.A3. [DOI] [PubMed] [Google Scholar]
- 24.Lasker JN. Hoping to Help: The Promises and Pitfalls of Global Health Volunteering. Ithaca, NY: Cornell University Press; 2016. [Google Scholar]
- 25.John CC, Ayodo G, Musoke P. Successful global health research partnerships: What makes them work? Am J Trop Med Hyg. 2016;94:5–7. doi: 10.4269/ajtmh.15-0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bao J, Rodriguez DC, Paina L, Ozawa S, Bennett S. Monitoring and evaluating the transition of large-scale programs in global health. Glob Health Sci Pract. 2015;3:591–605. doi: 10.9745/GHSP-D-15-00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Firestone R, Rowe CJ, Modi SN, Sievers D. The effectiveness of social marketing in global health: A systematic review. Health Policy Plan. 2017;32:110–24. doi: 10.1093/heapol/czw088. [DOI] [PubMed] [Google Scholar]
- 28.Gladding S, Zink T, Howard C, Campagna A, Slusher T, John C, et al. International electives at the university of minnesota global pediatric residency program: Opportunities for education in all accreditation council for graduate medical education competencies. Acad Pediatr. 2012;12:245–50. doi: 10.1016/j.acap.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Monroe-Wise A, Kibore M, Kiarie J, Nduati R, Mburu J, Drake FT, et al. The clinical education partnership initiative: An innovative approach to global health education. BMC Med Educ. 2014;14:1043. doi: 10.1186/s12909-014-0246-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McKinley DW, Williams SR, Norcini JJ, Anderson MB. International exchange programs and U.S. medical schools. Acad Med. 2008;83:S53–7. doi: 10.1097/ACM.0b013e318183e351. [DOI] [PubMed] [Google Scholar]
- 31.Haq C, Rothenberg D, Gjerde C, Bobula J, Wilson C, Bickley L, et al. New world views: Preparing physicians in training for global health work. Fam Med. 2000;32:566–72. [PubMed] [Google Scholar]
- 32.Ramsey AH, Haq C, Gjerde CL, Rothenberg D. Career influence of an international health experience during medical school. Fam Med. 2004;36:412–6. [PubMed] [Google Scholar]
- 33.Bjorklund AB, Cook BA, Hendel-Paterson BR, Walker PF, Stauffer WM, Boulware DR, et al. Impact of global health residency training on medical knowledge of immigrant health. Am J Trop Med Hyg. 2011;85:405–8. doi: 10.4269/ajtmh.2011.10-0732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Syed SB, Dadwal V, Rutter P, Storr J, Hightower JD, Gooden R, et al. Developed-developing country partnerships: Benefits to developed countries? Global Health. 2012;8:17. doi: 10.1186/1744-8603-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zink T, Solberg E. Development of a global health curriculum for family medicine based on ACGME competencies. Teach Learn Med. 2014;26:174–83. doi: 10.1080/10401334.2014.883987. [DOI] [PubMed] [Google Scholar]
- 36.Morris SC, Schroeder ED. Emergency medicine resident rotations abroad: Current status and next steps. West J Emerg Med. 2016;17:63–5. doi: 10.5811/westjem.2015.11.28159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alagappan K, Schafermeyer R, Holliman CJ, Iserson K, Sheridan IA, Kapur GB, et al. International emergency medicine and the role for academic emergency medicine. Acad Emerg Med. 2007;14:451–6. doi: 10.1197/j.aem.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 38.Thomas HA, Binder LS, Chapman DM, Kramer DA, LaMantia J, Perina DG, et al. The 2003 model of the clinical practice of emergency medicine: The 2005 update. Acad Emerg Med. 2006;13:1070–3. doi: 10.1197/j.aem.2006.06.045. [DOI] [PubMed] [Google Scholar]
- 39.Hockberger RS, Binder LS, Chisholm CD, Cushman JT, Hayden SR, Sklar DP, et al. The model of the clinical practice of emergency medicine: A 2-year update. Ann Emerg Med. 2005;45:659–74. doi: 10.1016/j.annemergmed.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 40.Ng-Kamstra JS, Greenberg SL, Abdullah F, Amado V, Anderson GA, Cossa M, et al. Global surgery 2030: A roadmap for high income country actors. BMJ Glob Health. 2016;1:e000011. doi: 10.1136/bmjgh-2015-000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kraeker C, Chandler C. “We learn from them, they learn from us”: Global health experiences and host perceptions of visiting health care professionals. Acad Med. 2013;88:483–7. doi: 10.1097/ACM.0b013e3182857b8a. [DOI] [PubMed] [Google Scholar]
- 42.Wernick B, Wojda TR, Wallner A, Yanagawa F, Firstenberg MS, Papadimos TJ, et al. Brain drain in academic medicine: Dealing with personnel departures and loss of talent. Int J Acad Med. 2016;2:68. [Google Scholar]
- 43.Riviello R, Ozgediz D, Hsia RY, Azzie G, Newton M, Tarpley J, et al. Role of collaborative academic partnerships in surgical training, education, and provision. World J Surg. 2010;34:459–65. doi: 10.1007/s00268-009-0360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Binagwaho A, Kyamanywa P, Farmer PE, Nuthulaganti T, Umubyeyi B, Nyemazi JP, et al. The human resources for health program in Rwanda – A new partnership. N Engl J Med. 2013;369:2054–9. doi: 10.1056/NEJMsr1302176. [DOI] [PubMed] [Google Scholar]
- 45.Ndenga E, Uwizeye G, Thomson DR, Uwitonze E, Mubiligi J, Hedt-Gauthier BL, et al. Assessing the twinning model in the Rwandan Human Resources for Health Program: Goal setting, satisfaction and perceived skill transfer. Global Health. 2016;12:4. doi: 10.1186/s12992-016-0141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ousman K, Polomano RC, Seloilwe E, Odero T, Tarimo E, Mashalla YJ, et al. Interprofessional fellowship training for emerging global health leaders in Africa to improve HIV prevention and care: The afya bora consortium. J Assoc Nurses AIDS Care. 2016;27:331–43. doi: 10.1016/j.jana.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sullivan N. International clinical volunteering in tanzania: A postcolonial analysis of a global health business. Glob Public Health. 2017:1–15. doi: 10.1080/17441692.2017.1346695. [DOI] [PubMed] [Google Scholar]
- 48.Joint Commission International, Joint Commission on Accreditation of Health care Organizations. Joint Commission International Accreditation Standards for Hospitals. Joint Commission Resources. 2002 [Google Scholar]
- 49.Reaves EJ, Schor KW, Burkle FM., Jr Implementation of evidence-based humanitarian programs in military-led missions: Part I. Qualitative gap analysis of current military and international aid programs. Disaster Med Public Health Prep. 2008;2:230–6. doi: 10.1097/DMP.0b013e31818d3c80. [DOI] [PubMed] [Google Scholar]
- 50.Reaves EJ, Schor KW, Burkle FM., Jr Implementation of evidence-based humanitarian programs in military-led missions: Part II. The impact assessment model. Disaster Med Public Health Prep. 2008;2:237–44. doi: 10.1097/DMP.0b013e31818d4510. [DOI] [PubMed] [Google Scholar]
- 51.Adini B, Ohana A, Furman E, Ringel R, Golan Y, Fleshler E, et al. Learning lessons in emergency management: The 4th International Conference on Health care System Preparedness and Response to Emergencies and Disasters. Disaster Mil Med. 2016;2:16. doi: 10.1186/s40696-016-0026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Katz R, Blazes D, Bae J, Puntambekar N, Perdue CL, Fischer J, et al. Global health diplomacy training for military medical researchers. Mil Med. 2014;179:364–9. doi: 10.7205/MILMED-D-13-00389. [DOI] [PubMed] [Google Scholar]
- 53.Jawhari B, Ludwick D, Keenan L, Zakus D, Hayward R. Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review. BMC Med Inform Decis Mak. 2016;16:116. doi: 10.1186/s12911-016-0354-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fritz F, Tilahun B, Dugas M. Success criteria for electronic medical record implementations in low-resource settings: A systematic review. J Am Med Inform Assoc. 2015;22:479–88. doi: 10.1093/jamia/ocu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wong A, Vohra R, Ruha AM, Koutsogiannis Z, Graeme K, Dargan PI, et al. The global educational toxicology uniting project (GETUP): An analysis of the first year of a novel toxicology education project. J Med Toxicol. 2015;11:295–300. doi: 10.1007/s13181-015-0479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pereira BM, Calderan TR, Silva MT, Silva AC, Marttos AC, Jr, Fraga GP, et al. Initial experience at a university teaching hospital from using telemedicine to promote education through video conferencing. Sao Paulo Med J. 2012;130:32–6. doi: 10.1590/S1516-31802012000100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mars M. Building the capacity to build capacity in e-health in Sub-Saharan Africa: The KwaZulu-Natal experience. Telemed J E Health. 2012;18:32–7. doi: 10.1089/tmj.2011.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moucheraud C, Schwitters A, Boudreaux C, Giles D, Kilmarx PH, Ntolo N, et al. Sustainability of health information systems: A three-country qualitative study in Southern Africa. BMC Health Serv Res. 2017;17:23. doi: 10.1186/s12913-016-1971-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolfe BA, Mamlin BW, Biondich PG, Fraser HS, Jazayeri D, Allen C, et al. The OpenMRS system: Collaborating toward an open source EMR for developing countries. AMIA Annu Symp Proc. 2006;2006:1146. [PMC free article] [PubMed] [Google Scholar]
- 60.Bazemore AW, Henein M, Goldenhar LM, Szaflarski M, Lindsell CJ, Diller P, et al. The effect of offering international health training opportunities on family medicine residency recruiting. Fam Med. 2007;39:255–60. [PubMed] [Google Scholar]
- 61.Purnell CA. Operation smile and the guwahati comprehensive cleft care center: Multidisciplinary global activism in plastic surgery. Plast Surg Nurs. 2016;36:180–1. doi: 10.1097/PSN.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 62.Purnell CA. Operation smile and the guwahati comprehensive cleft care center: Multidisciplinary global activism in plastic surgery. Plast Surg Nurs. 2014;34:181–2. doi: 10.1097/PSN.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 63.Campbell A, Sherman R, Magee WP. The role of humanitarian missions in modern surgical training. Plast Reconstr Surg. 2010;126:295–302. doi: 10.1097/PRS.0b013e3181dab618. [DOI] [PubMed] [Google Scholar]
- 64.Campbell A, Sullivan M, Sherman R, Magee WP. The medical mission and modern cultural competency training. J Am Coll Surg. 2011;212:124–9. doi: 10.1016/j.jamcollsurg.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 65.Coupet S. International health electives: Strengthening graduate medical education. J Am Osteopath Assoc. 2012;112:800–4. [PubMed] [Google Scholar]
- 66.Hayward AS, Jacquet GA, Sanson T, Mowafi H, Hansoti B. Academic affairs and global health: How global health electives can accelerate progress towards ACGME milestones. Int J Emerg Med. 2015;8:45. doi: 10.1186/s12245-015-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Arora G, Condurache T, Batra M, Butteris SM, Downs T, Garfunkel L, et al. Miles away milestones: A Framework for assessment of pediatric residents during global health rotations. Acad Pediatr. 2017;17:577–9. doi: 10.1016/j.acap.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 68.Karle H. Executive Council, World Federation for Medical Education. International recognition of basic medical education programmes. Med Educ. 2008;42:12–7. doi: 10.1111/j.1365-2923.2007.02907.x. [DOI] [PubMed] [Google Scholar]
- 69.Ibrahim H, Abdel-Razig S, Nair SC. Medical students' perceptions of international accreditation. Int J Med Educ. 2015;6:121–4. doi: 10.5116/ijme.5610.3116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 71.World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: Global policy recommendations. World Health Organization. 2010 [PubMed] [Google Scholar]
- 72.Redwood-Campbell L, Pakes B, Rouleau K, MacDonald CJ, Arya N, Purkey E, et al. Developing a curriculum framework for global health in family medicine: emerging principles, competencies, and educational approaches. BMC Medical Education. 2011;11:46. doi: 10.1186/1472-6920-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet. 2016;388:e19–23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 74.The_EQUATOR_Network. Enhancing Quality and Transparency of Health Research. 2017. [Last accessed on 2017 Oct 11]. Available from: http://www.equator-network.org/
- 75.Bhan A, Singh JA, Upshur RE, Singer PA, Daar AS. Grand challenges in global health: Engaging civil society organizations in biomedical research in developing countries. PLoS Med. 2007;4:e272. doi: 10.1371/journal.pmed.0040272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh JA, Mills EJ. The abandoned trials of pre-exposure prophylaxis for HIV: What went wrong? PLoS Med. 2005;2:E234. doi: 10.1371/journal.pmed.0020234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mills EJ, Singh S, Singh JA, Orbinski JJ, Warren M, Upshur RE, et al. Designing research in vulnerable populations: Lessons from HIV prevention trials that stopped early. BMJ. 2005;331:1403–6. doi: 10.1136/bmj.331.7529.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Delisle H, Roberts JH, Munro M, Jones L, Gyorkos TW. The role of NGOs in global health research for development. Health Res Policy Syst. 2005;3:3. doi: 10.1186/1478-4505-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kohrt BA, Marienfeld CB, Panter-Brick C, Tsai AC, Wainberg ML. Global mental health: Five areas for value-driven training innovation. Acad Psychiatry. 2016;40:650–8. doi: 10.1007/s40596-016-0504-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Berndtson K, Daid T, Tracy CS, Bhan A, Cohen ER, Upshur RE, et al. Grand challenges in global health: Ethical, social, and cultural issues based on key informant perspectives. PLoS Med. 2007;4:e268. doi: 10.1371/journal.pmed.0040268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pang T. Commentary on ‘reflections and recommendations on research ethics in developing countries’ by S.R. Benatar. Soc Sci Med. 2002;54:1145–6. doi: 10.1016/s0277-9536(01)00329-x. [DOI] [PubMed] [Google Scholar]