Abstract
Background
The present study aimed to describe a new safe and economical technique for medial patellofemoral ligament (MPFL) reconstruction with satisfactory clinical outcomes, and present the results of a four-year follow-up.
Material/Methods
Thirty-two patients with recurrent patella dislocation, who underwent MPFL reconstruction with two semi-patellar tunnels and hardware-free patellar fixation between 2011 and 2013, were included in the study. Patella stability was tested by an apprehension test preoperatively and at follow-up. Knee function was evaluated using the Kujala score, Lysholm score, and Crosby-Insall grading system. Patellar congruence angle and patellar tilt angle were measured using an axial computed tomography scan. Furthermore, objective feelings of patients and complications were recorded.
Results
Thirty knees (30 patients) were followed for a minimum of 48 months. The apprehension test was positive in all patients preoperatively, but negative at follow-up. Kujala and Lysholm scores increased from 58.9±9.6 to 92.0±4.8 (p<0.001) and 53.3±5.6 to 91.6±3.5 (p<0.001), respectively, at the last follow-up. Seventeen patients were graded as excellent and 13 were graded as good by the Crosby-Insall grading system. The patellar congruence angle and patellar tilt angle also improved significantly. No patient experienced patellar re-dislocation, subluxation, or patella fracture. Most patients (93%) were satisfied with the surgery.
Conclusions
MPFL reconstruction with two semi-patellar tunnels and hardware-free patellar fixation was described and the study observations indicated it was a safe and economical surgical procedure for recurrent patella dislocation with satisfactory results. It could be an alternative surgery method for patients with patella recurrent dislocation.
MeSH Keywords: Patella, Patellar Dislocation, Patellofemoral Joint
Background
The medial patellofemoral ligament (MPFL), which contributes 60% of soft tissue force restraint to lateral patella translation, plays an important role in patella stability [1]. MPFL has been found to be ruptured or injured during patella lateral dislocation, a finding supported by magnetic resonance imaging (MRI) studies and anatomic research [2,3]. The conservative treatment of patella dislocation can result in high re-dislocation occurrence rates, poor treatment effects, and patellofemoral osteoarthritis [4–6]. Therefore, MPFL reconstruction has become the preferred treatment, especially for patients with recurrent patella dislocation who have normal bony anatomy and alignment [7–11].
The understanding of the anatomy and function of MPFL has developed over time [1,12–14]. Kang et al. [13] did a series of research studies on the anatomy of the MPFL and proposed the concept of two functional bundles of the MPFL: an inferior straight bundle and a superior oblique bundle. In addition, Wang et al. [15] did a retrospective study and showed that patients treated with anatomical double-bundle MPFL reconstruction had better clinically and radiologically outcomes than patients treated with single-bundle isometric reconstruction.
A number of articles have described techniques of MPFL reconstruction, with variations based on the various methods used for patella fixation. Common fixations are suture anchor fixation, interference screw fixation and bone tunnel fixation [16–20]. Two suture anchors or interference screws are used in the patellar fixation, which adds substantial cost. Bone tunnel fixation is more economical with no screw application but with serious complications such as patella fracture [16,17]. Thus we developed MPFL reconstruction with two semi-patellar tunnels and hardware-free patellar fixation for safety and cost-savings for patients.
The purpose of the present study was to describe the new surgical procedure, present its preliminary results, and discuss the feasibility of its clinical application. Significantly improved subjective clinical outcomes and radiological improvements, including Kujala and Lysholm scores, patella tilt angle, and patella congruence angle, were hypothesized.
Material and Methods
Study design and patients
The study was a prospective, noncomparative, and interventional case series. Thirty-two consecutive patients with recurrent patella dislocation, who underwent isolated MPFL reconstruction from June 2011 to March 2013, were included in this study.
The inclusion criterion for isolated MPFL reconstruction was symptomatic patients who had experienced at least two episodes of patella dislocation and failed a course of conservative treatment (at least three months); and MPFL rupture was shown in MRI. The exclusion criteria for isolated MPFL reconstruction were as follows: osteoarthritis > grade 1 according to Kellgren and Lawrence [21]; focal cartilage defects > grade 3 according to Outerbridge [22]; trochlear dysplasia > grade B according to Dejour [23]; tibial tuberosity-trochlear groove distance (TT-TG) >20 mm [24]; patellar height: Insall–Salvati index >1.2 [25]; Q-angle >20° [26]; and knee cruciate ligaments and medial collateral ligament injury.
Patellofemoral cartilage condition was observed by arthroscopy. Trochlear morphology and TT-TG distance were measured on computed tomography (CT) scan. Q-angle and patellar height were evaluated by weight-bearing anterior-posterior and lateral views of knee x-ray radiographs, respectively. Kujala and Lysholm scores and apprehension test were also used to evaluate the patients before surgery [4,27].
Informed consents were obtained from all individual participants included in the study. All of the methods were approved by the local ethics committee.
Surgery technique
The surgeries were completed by one experienced senior surgeon. Autologous semi-tendinosus tendon was harvested and divided longitudinally into two equal grafts. Then the two grafts were folded from the middle point and the four free ends were whip stitched together about 25 mm with No. 1 Ethicon nonabsorbable sutures (Figure 1).
Figure 1.
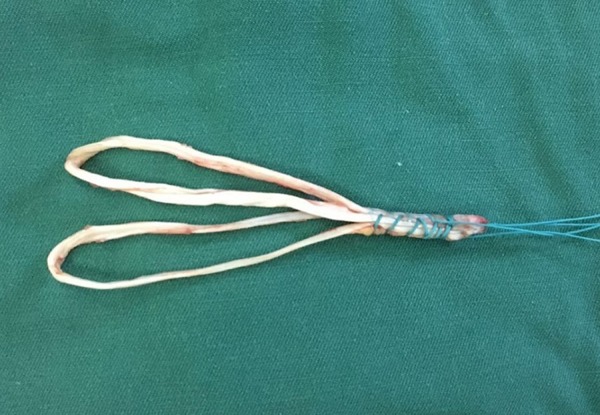
The preparation of the autografts.
A guide pin with 2.0-mm diameter with an eyelet was inserted from the site superoposterior to the medial femoral epicondyle and distal to the adductor tubercle to the lateral cortex of the femur [28,29]. Then a longitudinal skin incision with length to 10 mm was made over the femoral insertion site and subcutaneous tissue was dissected to expose the cortical bone. A femoral tunnel of a depth of 25 mm was drilled over the guide pin by a cannulated reamer with a diameter of 7 mm. The whip stitched portions of the two grafts were pulled into the femoral tunnel by their No. 1 Ethicon nonabsorbable sutures and guide pin. After adjustment, the whip stitched portions of the grafts were fixed with a bioabsorbable interference screw measuring 6×10 mm2, with the sutures in the femoral tunnel under tension.
A longitudinal incision was made from the upper inner corner to the center of the medial edge of the patella. Two folded ends of the grafts were pulled out to the medial patella margin through the subcutaneous fascial layers (Figure 2). Subsequently, the folded ends were separated for the double-bundle of MPFL and were passed through by two No. 2 nonabsorbable Fiberwire. A guide pin with 2.0-mm diameter was transversely inserted from the midpoint of the medial edge of the patella to the lateral border. A semi-patellar tunnel with a length of 20 mm was drilled by a cannulated reamer with a diameter of 4.0 mm under the guidance of the guide pin. After that, one folded end was pulled into the semi-patellar tunnel. A guide pin with 2.0-mm diameter was inserted from the upper inner corner of the patella to the lateral border transversely. A 20-mm long semi-patellar tunnel and another folded end were pulled into the tunnel by the same procedures.
Figure 2.

The two autografts were separated for double-bundle MPFL reconstruction.
After pulling guide pins out of the patella, the grafts were fixed temporarily using two hemostats clamping the ends of Fiberwire sutures on the lateral side of the patella. The graft tension and patella tracking were assessed by arthroscopy and physical examination in the flexion at 0–60° of the knee. The four ends of the two No. 2 Fiberwire nonabsorbable sutures over the lateral bone bridge were fastened for fixation when tensing the folded ends of the grafts in 30° of knee flexion. Because biomechanical studies have shown that the MPFL has its maximal length and restraint against patella lateralization in 30° of flexion [12]. At last, routine wound closure was performed. The schematic diagram for the reconstruction is shown in Figure 3.
Figure 3.
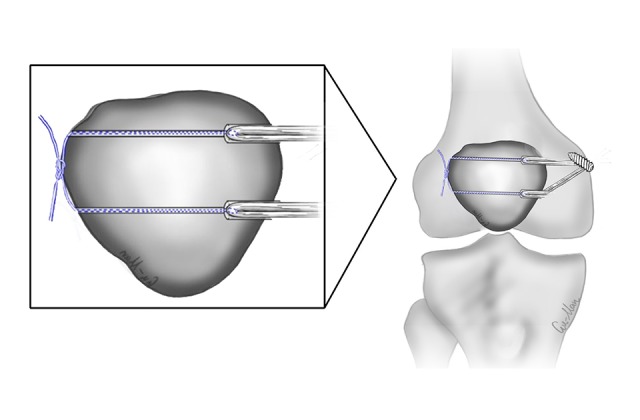
The schematic diagram of the MPFL reconstruction.
Postoperative care
The knee was immobilized for one week in an extended position. On the second day postoperatively, leg raising and quadriceps isometric strength exercises were started. At one week after surgery, a gradual range of motion was initiated with a hinged brace. Four week postoperatively, 90° of knee flexion was achieved. At six weeks after surgery, the brace was removed. Six weeks after surgery, full weight-bearing was allowed without a crutch. Three months after the surgery, the patients returned to performing normal daily activities. Contact sports were permitted six months after the surgery.
Clinical assessments
Knee function was evaluated using Kujala score, Lysholm scores and Crosby-Insall grading system [30]. Physical examinations were assessed using the apprehension test for lateral stability of the patella. Re-dislocation and fracture cases were also recorded. In addition, knee joint CT scans with 30° of knee flexion were performed to measure patella tilt angle and patella congruence angle preoperatively, six months postoperatively and annually thereafter. The subjective feelings of patients were recorded using questionnaire forms in the last follow-up. These values were recorded to the nearest 0.1.
Statistical analysis
The statistical analysis was performed using SPSS version 21.0 (SPSS, IL, USA). The preoperative and the most recent data from clinical and radiologic assessments were compared using the paired Student t-test. The level of significance was set at p<0.05. The results were expressed as mean ± standard deviation.
Results
Two patients who underwent the procedure were unavailable for follow-up for more than 24 months (could not be connected via their telephone numbers), thereby leaving 30 patients (30 knees) in the study (10 males and 20 females). The average age was 25 years (range 16–35 years). The average follow-up time was 55 months (range 48–63 months). The basic patient characteristics are shown in Table 1.
Table 1.
Patient characteristics.
| Variable | N | Mean ±SD |
|---|---|---|
| Sex (M/F) | 10/20 | |
| Side (L/R) | 14/16 | |
| Cause of dislocation (trauma/others) | 11/19 | |
| Age for surgery (year) | 25.0±6.9 | |
| Height (cm) | 163.0±7.6 | |
| Weight (kg) | 52.9±8.3 | |
| Month from first dislocation | 18.9±14.1 | |
| Q-angle (degrees) | 11.7±2.1 | |
| Insall-Salvati index | 1.0±0.1 | |
| Sulcus angle (degrees) | 136.7±6.7 | |
| TT-TG distance (mm) | 14.3±2.7 | |
| Follow-up month | 55.1±4.9 |
TT-TG distance – tibial tuberosity–trochlear groove distance.
At the last follow-up, the Kujala score increased from 58.9±9.6 to 92.0±4.8 (p<0.001) and the Lysholm score increased from 53.3±5.6 to 91.6±3.5 (p<0.001). According to the Crosby-Insall grading system, 17 patients were graded as excellent and 13 as good. The apprehension test was positive in all patients preoperatively, but negative at follow-up. No patient experienced patella re-dislocation or subluxation in the follow-up. No case of patella fracture was reported. The patellar congruence angle (41.9±8.6° to 5.8±7.3°, p<0.001) and the patellar tilt angle (32.3±8.6° to 12.8±3.4°, p<0.001) also improved significantly (Table 2). Most patients (93%) were satisfied with the surgery (Table 3).
Table 2.
Radiological and functional evaluations at the latest follow-up.
| Measurement | Preoperative | Latest follow-up | P value |
|---|---|---|---|
| PCA | 41.9±8.6 | 5.8±7.3 | <0.001 |
| PTA | 32.3±8.6 | 12.8±3.4 | <0.001 |
| Kujala score | 58.9±9.6 | 92±4.8 | <0.001 |
| Lysholm score | 53.3±5.6 | 91.6±3.5 | <0.001 |
PCA – patellar congruence angle; PTA – patellar tilt angle.
Table 3.
Subjective feeling questionnaire at the latest follow-up.
| Question | Yes number | % |
|---|---|---|
| Are you satisfied with the outcome of the surgery? | 28 | 93 |
| Did the surgery improve your symptoms obviously? | 30 | 100 |
| Would you recommend this procedure to others? | 22 | 73 |
| Have you had a recurrence of your symptoms? | 0 | 0 |
| Have you resumed sport/maximal activities? | 21 | 70 |
| Do you feel anxious for patella re-dislocation after surgery? | 5 | 16 |
| Do you feel pain or uncomfortable in patella? | 1 | 3 |
| Do you feel pain or uncomfortable in the femur (place around interference screw)? | 2 | 7 |
| Do you feel pain or uncomfortable in the tibia (location where autografts were harvested)? | 2 | 7 |
| Compared with the contralateral knee, do you feel difficult in knee rotation, extension and flexion? | 1 | 3 |
Discussion
The present study showed that anatomical MPFL reconstruction with two semi-patellar tunnels and hardware-free fixation was a safe technique to treat patients with recurrent patella dislocation, which yielded satisfactory results. Thirty patients were involved in the study and achieved good clinical results at a mean follow-up of 55 months. The Kujala score was 92±4.8, Lysholm score was 91.6±3.5, patellar congruence angle was 5.8±7.3°, and patellar tilt angle was 12.8±3.4° at the last follow-up. In addition, no patient experienced patella re-dislocation or subluxation. No case of patella fracture was reported. Most patients (93%) were satisfied with the surgery.
Two semi-patellar tunnels with 20 mm length were drilled under the guidance of the guide pin and filled with folded grafts, which had several advantages. Compared with bone tunnel fixation, semi-patellar tunnels caused less bone loss and were easy to control when drilling. Also, the risk of patella fracture decreased [16,17]. Compared with the suture anchor and interference screw fixation, the technique used in this study was not restricted by the diameter of the screws because metal screws were not used. In addition, postoperative complications such as postoperative pain caused by interference screws and anchor screws occurs frequently [31]. Hence, a lack of application of screws for patellar fixation in this study could result in fewer complications, as well as being less costly.
In a study reported by Hinterwimmer et al. [16], 19 patients received MPFL reconstruction with bone tunnel fixation and had follow-up at a mean of 16±3 months; 89% of the patients were either satisfied or very satisfied with the overall outcome. The mean Kujala score was 92±7 (range 69–100), and the median Tegner scale was 5 (range 3–7). Two patients could not flex the knee beyond 90° at six weeks postoperatively and one other patient suffered a displaced fracture three months postoperatively. In the study reported by Enderlein et al. [17], 224 patients received MPFL reconstruction with bone tunnel fixation and had follow-up from 12 to 60 months; the Kujala score improved from 62.5 to 80.4. Among them, seven patients (4.6%) had a re-dislocation, and 39% of patients experienced one or more episodes of subjective patellar instability. Song et al. [19] reported MPFL reconstruction with suture anchors fixation. Twenty patients had follow-up with a mean of 34.5 months, Kujala score was 90.9±4.5, and Lysholm score was 90.9±5.9 at the last follow-up. The Kujala score and Lysholm score in this study were comparable or even superior to those in other studies reporting on the results of anatomical MPFL reconstruction. No patient in our study experienced patella re-dislocation or subluxation. No complication such as patella dislocation was reported. Thus, MPFL reconstruction in this study can be considered a safe surgical method.
The limitations of our study included the small sample size and a mid-term follow-up. A longer follow-up with a larger patient cohort is necessary to confirm the effectiveness and safety of this technique. Also, control groups are needed in the future to show the efficacy and superiority of the presented technique clinically. However, the main aim of this study was to describe a new technique for anatomical MPFL reconstruction and present its clinical results. The technique was thought to have several advantages compared with the current techniques, especially for safety and cost-saving.
Conclusions
Anatomical double-bundle MPFL reconstruction with two semi-patellar tunnels and hardware-free fixation was found to be a safe and economical method. Clinical and radiographic outcomes were satisfactory, which indicated it could be an alternative surgery for patients with patella recurrent dislocation.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Aragão JA, Reis FP, de Vasconcelos DP, et al. Metric measurements and attachments levels of the medial patellofemoral ligament: An anatomical study in cadavers. Clinics. 2008;63:541–44. doi: 10.1590/S1807-59322008000400021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nomura E. Classification of lesions of the medial patellofemoral ligament in patellar dislocation. Int Orthop. 1999;23:260–63. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanders TG, Morrison WB, Singleton BA, et al. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25(6):957–62. doi: 10.1097/00004728-200111000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Camanho GL, Viegas AC, Bitar AC. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–25. doi: 10.1016/j.arthro.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Kang HJ, Wang F, Chen BC, et al. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):325–31. doi: 10.1007/s00167-012-2020-8. [DOI] [PubMed] [Google Scholar]
- 6.Nomura E, Inoue M. Second-look athroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthritis Cartilage. 2005;13(11):1029–36. doi: 10.1016/j.joca.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Fisher B, Nyland J, Brand E, Curtin B. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation: A systematic review including rehabilitation and return-to-sports efficacy. Arthroscopy. 2010;26(10):1384–94. doi: 10.1016/j.arthro.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Zhou JW, Wang CH, Ji G. A minimally invasive medial patellofemoral ligament arthroscopic reconstruction. Eur J Orthop Surg Traumatol. 2014;24:225–30. doi: 10.1007/s00590-012-1162-1. [DOI] [PubMed] [Google Scholar]
- 9.Mackay ND, Smith NA, Parsons N, et al. Medial patellofemoral ligament reconstruction for patellar dislocation: A systematic review. Orthop J Sports Med. 2014;2(8):1–7. doi: 10.1177/2325967114544021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35(11):1851–38. doi: 10.1177/0363546507306161. [DOI] [PubMed] [Google Scholar]
- 11.Lording T, Heimstra L, Fink C, Getgood A. Strategies for reconstruction of the medial patellofemoral ligament. Operative Techniques in Sports Medicine. 2015;23(2):87–94. [Google Scholar]
- 12.Amis AA, Firer P, Mountney J. Anatomy and biomechanics of the medical patellofemoral ligament: Review. Knee. 2003;10:215–20. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 13.Panagiotopoulos E, Strzlczyk P, Herrmann M. Cadaveric study on static medial patellar stabilizers the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Tarthrosc. 2006;14:7–12. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 14.Kang HJ, Wang F, Chen BC, et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1511–16. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 15.Wang C, Ma L, Zhou J, et al. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013;37:617–24. doi: 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinterwimmer S, Imhoff AB, Minzlaff P. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: Technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc. 2013;21:2147–54. doi: 10.1007/s00167-013-2498-8. [DOI] [PubMed] [Google Scholar]
- 17.Enderlein D, Nielsen T, Christiansen SE, et al. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2458–64. doi: 10.1007/s00167-014-3164-5. [DOI] [PubMed] [Google Scholar]
- 18.Panni AS, Alam M, Cerciello S, et al. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39:2647–55. doi: 10.1177/0363546511420079. [DOI] [PubMed] [Google Scholar]
- 19.Song SY, Kim IS, Chang HG, et al. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2431–37. doi: 10.1007/s00167-013-2730-6. [DOI] [PubMed] [Google Scholar]
- 20.Schottle PB, Hensler D, Imhoff AB. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18:147–51. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 21.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–57. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 23.Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(1):45–54. [PubMed] [Google Scholar]
- 24.Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity-trochlear groove distance; A comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–4. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 26.Hvid I, Andersen LI, Schmidt H. Chondromalacia patellae: The relation to abnormal patellofemoral joint mechanics. Acta Orthop Scand. 1981;52(6):661–66. doi: 10.3109/17453678108992164. [DOI] [PubMed] [Google Scholar]
- 27.Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–63. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 28.Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13:510–15. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 29.Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–4. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 30.Crosby EB, Insall J. Recurrent dislocation of the patella, relation of treatment to osteoarthritis. J Bone Joint Surg Am. 1976;58A:9–13. [PubMed] [Google Scholar]
- 31.Shah JN, Howard JS, Flanigan DC, et al. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–23. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]


