Abstract
Background
Like other complex psychosocial interventions, mindfulness-based treatments comprise various modality-specific components as well as nonspecific therapeutic ingredients that collectively contribute to efficacy. Consequently, the isolated effects of mindfulness strategies per se remain unclear.
Methods
Using a randomized double-blind design, we compared the isolated effects of 11-minutes of “supervised” mindfulness instruction against a closely matched active control (relaxation) on subjective, physiological, and behavioral indices of maladaptive alcohol responding in drinkers at risk of harm from alcohol use (n = 68). Simple follow-up instructions on strategy use were provided, but practice was unsupervised and not formally monitored.
Results
Both groups showed acute reductions in craving after training, although a trend group x time interaction (P = .056) suggested that this reduction was greater in the relaxation group (d = 0.722 P < .001) compared with the mindfulness group (d = 0.317, P = .004). Furthermore, upregulation of parasympathetic activity was found after relaxation (d = 0.562; P < .001) but not mindfulness instructions (d = 0.08; P > .1; group x time interaction: P = .009). By contrast, only the mindfulness group showed a reduction in past-week alcohol consumption at 7-day follow-up (-9.31 units, d = 0.593, P < .001), whereas no significant reduction was seen in the relaxation group (-3.00 units, d = 0.268, P > .1; group x time interaction: P = .026).
Conclusion
Very brief mindfulness practice can significantly reduce alcohol consumption among at-risk drinkers, even with minimal encouragement to use this strategy outside of the experimental context. The effects on consumption may therefore represent a lower bound of efficacy of “ultra-brief” mindfulness instructions in hazardous drinkers, at least at short follow-up intervals.
Keywords: mindfulness, alcohol, craving, relaxation
Significance Statement
We examine the isolated effects of simple mindfulness instructions in people at risk of harm from alcohol consumption (“at-risk drinkers”). A single brief session of mindfulness resulted in significant reductions in alcohol consumption compared with a carefully matched relaxation control condition at 1-week follow-up. These findings suggest that even “ultra-brief” experience with mindfulness can have measurable and potentially clinically meaningful effects in at-risk drinkers.
Introduction
Alcohol use disorder (AUD) causes inestimable personal suffering and contributes significantly to the global disease burden (Whiteford et al., 2013). However, AUD represents a clinical endpoint that is influenced by numerous environmental, developmental, and neurobiological factors (e.g., Schuckit, 1994; Slutske, 2005; Walsh et al., 2017). The transition to more severe alcohol problems is generally preceded by patterns of heavy drinking, which might not cross the severity threshold for AUD but are nonetheless associated with elevated risk of various negative outcomes for the individual, their social networks, and society more broadly (NICE, 2010). From a public health perspective therefore, these at-risk drinkers are an important group for whom innovative brief psychosocial interventions are needed (Whitlock et al., 2004; NICE, 2010).
In recent years, many innovations in behavioral science have occurred at the interface between Eastern and Western scientific psychology in the form of “mind-body” treatments (Grossman et al., 2004). There has been particular interest in mindfulness-based interventions for a range of psychiatric and physical health conditions (Gotink et al., 2015), which has been mirrored by enormous public interest in these approaches (Shonin and Van Gordon, 2015). Marlatt and colleagues (e.g., Leigh et al., 2005; Marlatt and Marques, 1977) were among the first to advance the idea that techniques based on Eastern contemplative traditions could usefully be incorporated into formal psychological treatments for addiction. Since the publication of this early theoretical and clinical case material, more than 30 randomized controlled trials of mindfulness-based interventions in substance-using populations have been published (reviewed in Li et al., 2017). These studies suggest that, compared with alternative treatments, mindfulness-based treatments are superior on a variety of substance-use related outcomes.
Mindfulness refers to a heightened moment-to-moment awareness of the processes and contents of the mind, without judgement or clinging (Mikulas, 2011). As such, this process is antithetical to the fixation upon and elaboration of desire states that characterize addictions (May et al., 2004). Craving is the quintessential desire state associated with problematic drug use and is activated by external cues (cue-induced craving), as well as operating as a background state (tonic craving) signalling varying degrees of deprivation (Sayette, 2016). Given the proposed association between craving (and negative affect) and relapse (Sinha and Li, 2007), most existing psychosocial (e.g., cognitive behavioral therapy) and pharmacological treatments (e.g., replacement therapies) for drug and alcohol problems directly aim to downregulate the intensity of cue-induced or tonic craving, or both. Many psychosocial treatments for alcohol and substance use problems, such as cognitive behavioral therapy, consist of “emotion regulation” procedures that explicitly aim to reduce the occurrence and/or intensity of craving. Theoretically, these procedures derive from the idea that maladaptive behaviors are proceeded by undesirable cognitive and affective states (e.g., craving and drug-related thoughts), and reductions in the intensity/occurrence of these states is responsible for behavior change (Beck et al., 2001). Relaxation is a prototypical emotion regulation strategy, which is commonly employed in psychosocial AUD treatments to reduce physiological arousal associated with craving, negative affect, or stress (Spada, 2012).
Notably, mindfulness-based approaches do not aim to dispel or otherwise alter craving or related thoughts and feelings. Instead, these approaches emphasise nonjudgementally attending to the arising of craving, its intensification, and gradual diminution, followed by further arising (e.g., “urge surfing,” Bowen and Marlatt, 2009). By deliberating on these subjective experiences nonjudgementally, the individual learns about their usual tendency to respond reflexively to urges. They also learn that they can apply nonreactive observation to urges that normally activate automatized action tendencies (compulsions). As such, one proposal is that mindfulness-based treatments enable the link between craving, affect, and behavior to become increasingly conscious and under the control of intention (Brewer et al., 2013), leading to an uncoupling between drug-taking and automatic motivational tendencies (Ostafin et al., 2012; see also Garland et al., 2014) and craving (Brewer et al., 2011; Elwafi et al., 2013). Other clinical trials suggest that, despite not directly aiming to reduce craving, reductions in craving are nonetheless observed following mindfulness-based treatments (e.g., Bowen et al., 2009; Davis et al., 2014; Garland et al., 2016; see Li et al., 2017 for other examples). Laboratory experiments have also shown acute reductions in craving following mindfulness in smokers, although this effect is most robust when mindfulness strategies are compared with inactive control strategies (see Serfaty et al., 2017). Alternatively, some laboratory studies have shown that, relative to active control strategies (e.g., distraction or reappraisal), brief mindfulness-like strategies result in increased (Szasz et al., 2012), or limited reductions in, cue-induced craving (Murphy and McKillop, 2014). As such, the mechanistic relationship between mindfulness treatment, craving, and drug use is complex and remains to be resolved (although see Witkiewitz and Bowen, 2010 for a well-powered moderated-mediation analysis involving mindfulness-based relapse prevention vs treatment as usual and craving, depression, and substance use).
While an evidence base that supports the use of mindfulness-based therapies for AUD (e.g., mindfulness-based relapse prevention, acceptance and commitment therapy, dialectical behavior therapy) is developing apace (Grant et al., 2015; Lee et al., 2015; Li et al., 2017; Rösner et al., 2015), few well-controlled laboratory studies have been performed that parse the specific, isolated effects of specific mindfulness strategies (Levin et al., 2012). Such studies have different aims to those of clinical trials of mindfulness therapies, which involve complex treatment packages, containing numerous individual therapeutic procedures (Craig et al., 2008). It is therefore difficult to isolate the contribution of individual therapeutic elements and determine their impact on overall efficacy using RCT designs (Levin et al., 2012). Although recent developments in clinical trial design allow common addiction treatment elements to be studied in relative isolation and in simple combinations (Schlam et al., 2016), RCTs are expensive and cumbersome. An alternative approach has therefore been to study specific, isolated psychosocial treatment elements in highly controlled laboratory settings. The aims of such studies are closely aligned to those of pharmacological dose-finding studies (e.g., McCabe et al., 2009), namely to achieve maximum levels of experimental control to establish a proof-of-concept prior to RCTs designed to establish clinical utility. Moreover, such laboratory experimental studies allow a flexible, fine-grained, and highly efficient assessment of specific therapeutic strategies on mechanistically important substance-use indicators, which might be logistically difficult to assess in clinical trials (e.g., cue-induced craving) or raise ethical issues in treatment seekers (e.g., use of an alcohol “taste test”).
Two laboratory studies testing the specific and isolated effects of brief mindfulness strategies in at-risk drinkers have been published recently. These showed either a highly circumscribed and limited differential effect of mindfulness (i.e., changes in state mindfulness immediately following mindfulness relative to a word-count matched relaxation condition; Vinci et al., 2014) or superior efficacy of a control strategy (distraction) on craving and craving-related distress relative to mindfulness (Murphy and MacKillop, 2014). However, while these and other laboratory experimental studies are informative, they have some limitations. These include lack of experimenter blinding, limited matching of conditions or nonoptimal controls, limited use of theoretically appropriate outcomes, and use of research participants whose alcohol/drug-use patterns are unlikely to be habitual (see Serfaty et al., 2017). As such, it remains to be established whether brief mindfulness instructions can have effects that endure beyond a laboratory training session and affect consumption behavior in drug-/alcohol-using populations, including at-risk drinkers.
Efficacy alone is not sufficient to establish the clinical utility of psychosocial interventions for AUD. Such treatments also need to have high levels of compliance, uptake, and cost effectiveness. These factors likely explain the preference among service providers and users for brief alcohol interventions (Bertholet et al., 2005). However, it is generally accepted that mindfulness is a form of cognitive training requiring sustained and disciplined practice, and as such, the conjunction of the terms “brief” and “mindfulness” may seem oxymoronic. However, Bowen and Marlatt (2009) reported promising effects of just 11 minutes of mindfulness instructions on smoking behavior over the course of a 7-day follow-up. Given those findings, and the limitations in previous experimental research on mindfulness in drug- and alcohol-using populations (noted above), it remains important to determine whether a minimal dose of mindfulness is effective in changing drinking outcomes in the short term (≤7 days). Evidence of post-acute benefits of brief mindfulness strategies might have clinical importance, encouraging the use of such strategies early in treatment, with the potential to improve self-efficacy and treatment motivation and retention.
In the current study, we aimed to address the limitations of previous laboratory studies of mindfulness in drug and alcohol users by comparing the effects of a brief set of mindfulness instructions with well-matched, active control instructions in participants with elevated risk of alcohol-related harms. The control strategy in this case consisted of relaxation instructions specifically designed to downregulate craving by reducing arousal. The mindfulness instructions, on the other hand, emphasized ongoing attention to internal experiences without attempting to change these. We describe these strategy instructions as ultra-brief because of their brevity relative to instructions typically used in mindfulness-based treatments (typically >10 hours; e.g., Bowen et al., 2014).
Methods
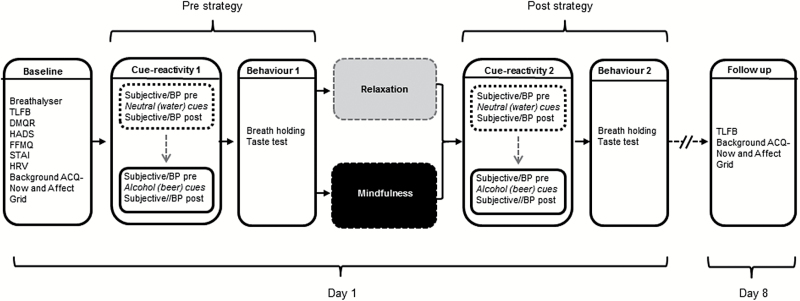
University College London Ethics Committee provided ethical approval for this study. A double-blind, randomized controlled design was used to assess the effects of mindfulness and relaxation on cue reactivity and drinking behavior. Following telephone screening, participants attended the study center (day 1), followed by remote 1-week follow-up (on day 8; Figure 1). Participants were blind to group and study hypotheses. Experimenters were blind to treatment allocation (see below).
Figure 1.
Experimental protocol for the within-session (day 1) assessments and follow-up (day 8) procedures.
Participants
Participants (n=68; n=34 women) were heavy drinkers but otherwise healthy. They provided written, informed consent and met the following inclusion criteria: fluency in English; age 18 to 50 years; preference for beer; hazardous drinking indicated by a score of ≥8 on the Alcohol Use Disorder Identification Test (AUDIT; Babor et al., 2001), and pre-2016 thresholds for risky drinking in the UK (≥14 or ≥21 units/week for men and women respectively; 8 g ethanol/unit). Participants who self-declared the presence of current mental health problems or substance/alcohol use disorder or historical treatment seeking for these conditions were excluded. Note, the AUDIT was only used to screen-in rather than screen-out participants with high scores.
Those self-declaring any respiratory difficulties were also excluded (see below). Of n=241 screened individuals, n=92 were eligible, and n=68 attended the scheduled experimental session. The majority were students (n=54; 79.5%) with similar numbers of students per group (χ2(1)=1.439, P>.1). Participants received £20 compensation.
Based on an effect size from similar work (ηp2=0.13; Beadman et al., 2015; G*Power3, Faul et al., 2007), a minimum n≥22 was sufficient to detect a significant (α=0.05) time x group interaction. However, given the uncertainty about effect magnitude for some indices used here, a conservative small-medium sized effect (f=0.175) was assumed, yielding a sample size estimate of n=68 (α=0.05; 1-β=0.80).
Measures
Physiological Indices of Cue-Reactivity and Strategy Response
Psychophysiological indices are markers of treatment response, indexing changes in cue-reactivity (Kamboj et al., 2011, 2012). Here, systolic blood pressure (BP; BM40 XL, Beurer UK Limited) was used as an index of cue-associated physiological arousal and sampled immediately after the cue-reactivity procedures for neutral and alcohol cues (see below; Sinha et al., 2009). Diastolic BP values are also reported. Heart rate variability (HRV) was used as a marker of autonomic functioning before and during strategy-use and was acquired using an electrocardiogram (ECG) device with a sampling rate of 1 kHz (Bodyguard 2, Firstbeat Technologies). HRV was quantified using the mean square of successive inter-beat differences (RMSSD), which reflects self-regulation capacity and underlying parasympathetic influence on cardiac activity. RMSSD is particularly appropriate for short duration measurements, as used here (Task Force of The European Society of Cardiology, 1996).
ECG electrodes were attached below the right collarbone and left ribcage at the start of the experiment to allow stabilization. Event markers corresponded to the start and end of a 5-minute baseline period prior to cue exposure, and the last 5-minute period of mindfulness/relaxation. Data were analyzed offline (Kubios; Tarvainen et al., 2014).
Alcohol-Related Measures
The AUDIT (Babor et al., 2001) assessed hazardous/harmful drinking. Previous week consumption was assessed using a 7-day Timeline Follow-Back (TLFB; Sobell and Sobell, 1992), and UK government guidelines were used to determine binge-drinking frequency (≥6 or ≥8 units of alcohol ≥once/week for women and men, respectively). The Drinking Motives Questionnaire-Revised (DMQR) was used to assess high-risk drinking motives (coping and self-enhancement; Cooper, 1994).
Episodic craving was assessed using the 12-item Alcohol Craving Questionnaire (ACQ; Singleton et al., 1994) either in the context of the cue reactivity procedure (i.e., phasic or cue-induced craving) or in the absence of cues (i.e., tonic or background craving; see Tiffany and Wray, 2012, for discussion of the distinction of these 2 types of craving). In both cases, instructions were to rate the items according to how participants felt “right now.” Mean values for the 12 items of the ACQ are reported here.
Affect
The Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith, 1983) identifies abnormal levels of anxiety and depression, with 7 items related to each construct. The State-Trait Anxiety Inventory (STAI; Spielberger, 2010) was also used to assess trait anxiety. Affective state (valence and arousal) was assessed using the affect grid (Russel et al., 1989), a 2-dimensional, 9 x 9 matrix, with valence anchors of “extremely unpleasant” (score=1; left side of grid) and “extremely pleasant” (score=9; right side of grid) and arousal anchors of “extremely highly aroused” (score=9; top of grid) and “extreme sleepiness” (score= 1; bottom of grid). A single cross is placed in one of the 81 boxes to simultaneously indicate current valence and arousal. The middle square (score of 5) corresponded to neutral valence and arousal. Arousal and valence were assessed over 2 timescales: acutely in the context of the cue reactivity procedure (cue-induced arousal/valence, day 1) and longer term (day 1 baseline to day 8 follow-up) reflecting background affect (i.e., in the absence of cues).
Mindfulness and Relaxation
Trait mindfulness was assessed using the Five Facet Mindfulness Questionnaire (Baer et al., 2008). Immediately after the mindfulness or relaxation strategy, state mindfulness was assessed with the Toronto Mindfulness Scale (TMS) and state relaxation-tension using a 9-point single-item measure (“absolutely no tension” to “extremely tense;” Vinci et al., 2014).
Manipulation Checks
The Credibility/Expectancy Questionnaire was adapted from the original measure (Devilly and Borkovec, 2000) and referred to beliefs about whether the allocated strategy might help the participant reduce their drinking. A manipulation check (Rood et al., 2012; Murphy and MacKillop, 2014) was adapted for this study and included 6 true/false questions (e.g., “I was instructed to allow my craving to stay as it is without trying to change it;” “I was instructed to breathe calmly in order to reduce my craving”). Strategy use during the 7-day follow-up period was assessed remotely on day 8 (“how many days have you practiced the technique during this week?” and “for how long (minutes) on average have you practiced each day”). Finally, participants were asked about the extent to which they were “fully engaged” with the strategy during the previous week (5-point scale: 1= “not at all,” 3=”somewhat;” 5= “completely”).
In Vivo Cue-Reactivity Procedure
Reactivity was assayed for identical quantities of chilled water (“neutral”) and chilled beer (“alcohol”) in identical beer glasses. Water preceded alcohol cues to avoid carry-over effects (Sayette et al., 2010). The reactivity procedure was conducted at 2 time points: before (cue reactivity 1) and after (cue reactivity 2) strategy use (see Figure 1 for timeline of measures). The instructions on interacting with cues were the same for all participants and were delivered as a standardized audio (~2 minutes) via headphones. Participants were asked to notice sensory qualities and any thoughts that occurred while interacting with cues. Participants were then instructed to imagine taking a sip of the drink, noticing accompanying sensations and urges. BP, craving (ACQ-now), and affect (affect grid) were assessed after exposure to each type of cue before and after strategy use.
Beer Taste-Test
Participants were instructed to drink as much/as little of 275 mL chilled beer (Becks Blue, alcohol-free) as required to provide accurate taste ratings (below; Field and Eastwood, 2005). Alcohol-free beer was used to avoid pharmacological interference with mindfulness/relaxation. Although we concealed our intention (to avoid pharmacological effects of alcohol), this “deception” was necessary to preserve the integrity of the experimental manipulations.
Participants rated the beer on 4 sensory continua to conceal the objective of this test (Field and Eastwood, 2005). This task along with the breath holding task (see below) were undertaken prior to (behavior 1) and after (behavior 2) mindfulness or relaxation strategies (see Figure 1 for timing of behavior 1 and 2 measures).
Breath-Holding
The duration of breath-holding is a behavioural measure of distress tolerance, which may be related to (the effects of) mindfulness (Lotan et al., 2013). Participants held their breath for as long as possible after a full, normal exhalation (Sütterlin et al., 2013). To ensure compliance, participants wore a nose clip and were monitored. Timing (seconds) stopped when participants took their first inhalation.
Mindfulness and Relaxation Strategies
Strategy instructions were recorded in a sound-attenuated environment (same male actor for both sets of instructions). Doctoral trainees in clinical psychology (n=10) with academic and clinical training in mindfulness rated both recordings (10-point scale) on the extent to which the instructions were consistent with their respective aims (to encourage either mindfulness or relaxation in response to craving). Both strategies scored highly: mindfulness=9.60±0.70; relaxation=8.90±0.74. Strategy instructions were well matched in terms of duration, number of words (mindfulness: 1581; relaxation:1595 words for 4 phases; see below), number of smoking- and craving-related words, and language complexity (Flesch-Kincaid grade level 8).
Participants received strategy instructions according to a randomization code, balanced for gender (www.random.org), which was concealed from the experimenters. The audio instructions were stored on separate USB devices retained by the study supervisors and accessed individually for each participant, along with a sealed envelope, containing experimenter-concealed follow-up practice instructions printed on a credit-card sized flashcard.
During the session, participants were administered instructions from one of the USB devices according to randomization code. Headphone audio volume was fixed to prevent sound leakage and inadvertent breaking of the experimenter blind.Instructions involved 4 phases: introduction (30 seconds), explanation of strategy (3 minutes), preliminary experiential practice (4 minutes), and main strategy practice (7 minutes). The introduction explained the aim of the upcoming strategy and was identical for both strategies. During the explanation of strategy, the relaxation group was told, for example, that craving intensity can be reduced by “softening the muscles...and calming and unwinding the mind…releasing tension in your body” and that relaxation enabled transformation of sensations into more calming, less unpleasant experiences. It was also emphasized that this was a way of gaining control over craving.
By contrast, mindfulness instructions did not include any mention of reduced craving or of controlling, transforming, or regulating internal experience. It was clarified that the aim was not to simply relax, but to be alert and attentive. The emphasis was on “open monitoring” of experience and particularly on “aware[ness] of feelings and bodily sensations” and to “experience craving in a different way.” Participants were told that by noticing bodily sensations they could “experience them as temporary events in the body,” helping the participant to “tolerate [bodily sensations] without acting on them.” To minimize expectancy effects relating to the increasing popularity and public discussion of complementary medicine approaches, no mention of the term “mindfulness” (or “relaxation”) was made in any experimental or recruitment material.
After the explanations, participants provided ratings of credibility and expectancy for their assigned strategy. They then briefly practiced their assigned strategy (preliminary experiential practice) and then undertook the strategy proper (main strategy practice). In contrast to the explanation, which involved a simple description of the strategies, the preliminary and main strategy practice involved active participation in the strategy. As such, during preliminary practice, participants in the mindfulness group were first instructed on breath and body awareness. They were then instructed to notice alcohol-related urges; to focus their attention on these feelings in the body and to “tell yourself [for example], I feel my craving in my abdomen [or chest etc.].” In contrast, relaxation involved instructions to “calm your body” in response to urges; to “loosen and ‘untense’ that region” and to “tell yourself, ‘I am managing my craving by calming my abdomen [or chest, etc.]’.” Mindfulness participants were also instructed to notice “the exact sensations” in their body and encouraged to consider the accompanying sensory qualities. Relaxation participants were instructed to breathe slowly and deeply and to “release tension” upon exhaling.
The main mindfulness practice reiterated and expanded upon these instructions, with additional instructions to be “open hearted and non-reactive as you notice the [craving] sensations...[letting] go of the tendency to want things to be different.” Instructions to “notice” and “focus” on urges “as they come and go” and that “these feelings can be accepted and tolerated rather than acted upon” were also included and repeated. The main relaxation instructions emphasized ease and comfort and “releas[ing] any stiffness in your muscles” in response to craving sensations. They also included instructions to loosen muscles and to respond to any unwanted feelings with feelings of calmness. Full instruction scripts are available from the authors.
At the end of day 1, participants were asked to practice their assigned strategy for 15 min/d over the next 7 days, referring to the flashcard reminder instructions they received in a sealed envelope. These stated, “Remember that if/when you experience craving or urge to drink alcohol, you can refrain from it by using the strategies you have been taught.” The mindfulness reminder card additionally contained instructions to “Notice and observe your thoughts and physiological reactions nonjudgementally as they arise. Allow them to be there and let them go.” In contrast, the relaxation card stated “Take a few deep breaths and release any tension in your body as it arises. Allow your muscles to feel more and more calm.”
Procedure
Participants responded to online adverts on general and research-oriented sites (Gumtree, Experimatch, Call for participants, and a university-administered recruitment system), which contained a link to a web-based screening questionnaire that participants completed to declare whether they met inclusion/exclusion criteria.
To reduce expectancy effects related to one or the other strategy prior to day 1, participants remained blind to the specific study aims and design. On the day 1, generic information relevant to both strategies was provided. Specifically, study information described the experiment as involving brief strategies that may be helpful for managing craving experiences. Given that only broad aims of the experiment were disclosed, a degree of concealment was involved, which, on balance, was deemed essential to protect study integrity.
The sequence of tasks on day 1 and 8 is outlined in Figure 1. Upon arrival, physiological equipment (BP cuff and ECG electrodes and device) was attached, followed by a ~10-minute habituation and stabilization period. Participants were breathalyzed (Lion 500, Lion Instruments) to ensure compliance with instructions to refrain from alcohol on the testing day (all participants provided readings of 0.00) and then completed baseline questionnaires (TLFB, DMQR, HADS, Five Facet Mindfulness Questionnaire, STAI, background ACQ-Now, and background affect grid), with baseline HRV data acquired simultaneously. This was followed by the in vivo cue reactivity procedure for water, and then beer cues, followed by the beer taste-test and breath-holding (prestrategy phase; Figure 1).
Participants then listened to strategy instructions, immediately followed by completion of poststrategy manipulation checks (TMS, relaxation state questionnaire, true/false manipulation check) followed by a second in vivo cue reactivity procedure with water and beer cues and a second beer taste- and breath-holding test (poststrategy phase; Figure 1). At the end of the session participants were given the sealed envelope containing follow-up strategy instructions.
Participants completed follow-up assessments on day 8 by following a link to an online survey tool. Participants repeated the TLFB (previous 7 days), the ACQ-Now, and affect grid. These latter assessments (and those at baseline on day 1) were not conducted in the context of any cue reactivity instructions and hence can be assumed to reflect background-craving and affect. Finally, on day 8, participants completed questions regarding strategy-use over the previous 7 days.
Statistical Analysis
All data are presented as means ± SD (or SEM, where indicated in figures), percentages, or counts. Data were examined for skewness and outliers both statistically (Kolmogorov-Smirnov tests) and graphically. Where skewness was not corrected by transformation (questions regarding 7-day strategy practice), nonparametric (Mann-Whitney) tests were used. Outliers (>upper quartile + 1.5*IQR; Field, 2013) were winsorized (replacement with the highest nonoutlier for affect grid values or 1+ highest nonoutlier for all other variables). Sensitivity analysis confirmed the same statistical pattern of findings without outlier replacement.
The groups were compared on demographic characteristics, trait measures, baseline drinking behavior, and subjectively rated dependent variables, using independent samples t tests. Other data were analyzed using mixed time x cue type x group ANOVAs. The time factor involved 2 timeframes depending on the dependent variable: within session and longer term (baseline to follow-up).
Pearson’s r is reported for correlations. Diagnostics of multiple regression (exploring the effects of group, strategy practice, expectancy, and credibility on drinking) revealed no violation of the assumptions, indicating ordinary least squares was appropriate for parameter estimation.
The significance level was 0.05 and all reported tests were 2-tailed; all posthoc tests were Bonferroni corrected. Within-group effect sizes were calculated based on t and r values of within-subjects tests (Dunlap et al., 1996). Missing data points (recording failures due to technical issues) were missing completely at random (Little’s test: χ2(776) = 210.23, P > 0.1) and are indicated by deviations in the expected degrees of freedom in some of the analyses described below.
Results
Sample Characteristics
There were no group differences on demographic, mood, or alcohol consumption variables (Table 1; t values ≤1.50; P values > .1; ethnicity: χ2(1) = 2.138, P > .1). Frequency of alcohol consumption (AUDIT item 1) was matched (n = 20: 2–3 times/wk; n = 14 ≥4 times/wk in past month in both groups), as was binge drinking frequency. HADS scores for the whole sample were similar to normative UK values for depression (normative mean for depression: 3.68 + 3.07; see Crawford et al., 2001) but somewhat elevated for anxiety (cf normative mean for anxiety 6.14 + 3.76). Nonetheless, the relatively low scores on the HADS (Table 1) in this sample is consistent with exclusion of participants with significant levels of common psychiatric symptoms.
Table 1.
Demographic and psychometric characteristics of participants in the Relaxation and mindfulness groups
| Relaxation control (n = 34) | Mindfulness (n = 34) | |
|---|---|---|
| Demographic | ||
| Women (n; %) | 17 (50%) | 17 (50%) |
| Age (y) | 23.09 (4.98) | 24.60 (6.77) |
| Education (y) | 15.47 (1.48) | 15.53 (1.69) |
| Non-Caucasian (n; %) | 10 (29.4%) | 5 (14.7%) |
| Mood | ||
| HADS (depression) | 3.91 (2.77) | 3.65 (3.56) |
| HADS (anxiety) | 8.09 (3.86) | 7.41 (4.55) |
| STAI | 45.65 (12.68) | 41.38 (11.98) |
| Arousal baselinea | 4.71 (1.79) | 4.55 (1.72) |
| Valence baselinea | 6.35 (1.25) | 6.48 (0.91) |
| Alcohol (baseline) | ||
| AUDIT | 17.21 (4.61) | 16.41 (5.00) |
| TLFB | 23.94 (11.71) | 27.66 (16.95) |
| ACQ-Nowa | 4.03 (0.81) | 3.70 (1.00) |
| Binge drinking/wk | 1.65 (1.04) | 1.68 (1.25) |
Except for sex and ethnicity, all values are mean ± SD.
aBaseline assessments in the absence of cues.
TLFB, number of alcohol units (1 unit = 8 g pure alcohol) consumed over the previous 7 days.
All differences = ns (P > .1).
All dfs = 66 except arousal and valence, df = 58.
The groups did not differ on DMQR drinking motives (F(3,198) = 0.356, P > .1), and both groups showed the same rank order of motives on the DMQR: social (3.84 ± 0.77) ≈ enhancement (3.50 ± 0.82) >coping (2.61 ± 1.01) >conformity (1.73 ± 0.81). High levels of enhancement motives in particular are consistent with the intention to recruit at-risk drinkers (Kuntsche et al., 2005).
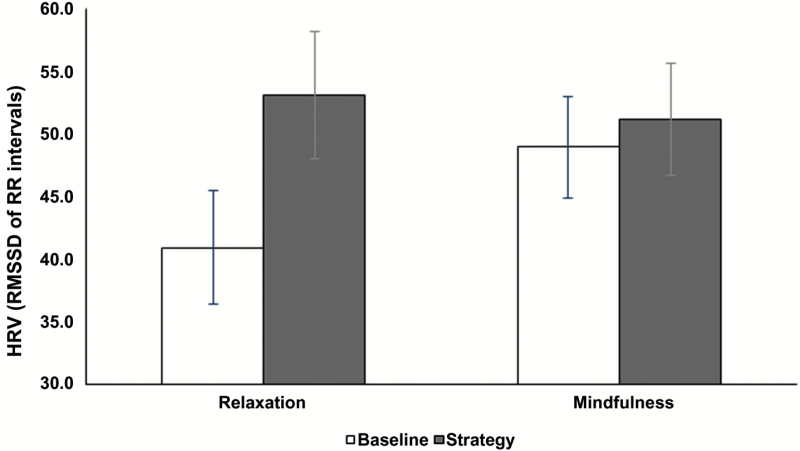
General Strategy Effects
Relaxation and mindfulness did not differ in credibility or expectancy of efficacy, and participants provided equivalent ratings on understanding of strategy instructions (P values > .1). Poststrategy state mindfulness was not significantly higher in the mindfulness group (t(65) = 1.363, P >.1; Table 2), nor did state relaxation-tension differ statistically between groups (t(65) = 1.351, P >.1; Table 2). However, parasympathetic activity indexed using HRV during the strategy showed a significant main effect of time (F(1, 57) = 14.973, P <.001, = 0.208), subsumed by a significant time x group interaction (F(1, 57) = 7.266, P <.01, = 0.113; Figure 2). This reflected an increase in HRV during relaxation (mean(Diff) = 12.24 ± 2.79 ms; d = 0.562; P <.001) but not during mindfulness (mean(Diff) = 2.19 ± 2.48 ms; d = 0.08; P >.1).
Table 2.
Group by Time Effects for Subjective Valence and Arousal Immediately before (Cue Reactivity 1) and after (Cue Reactivity 2) Cue Reactivity Procedures for Neutral (Water) and Alcohol (Beer) Cues
| Relaxation | Mindfulness | |||
|---|---|---|---|---|
| Cue reactivity 1 | Cue reactivity 2 | Cue reactivity 1 | Cue reactivity 2 | |
| Valence a | ||||
| Neutral | 5.97 (1.33) | 6.07 (1.23) | 6.45 (1.02) | 6.28 (1.58) |
| Alcohol | 6.07 (1.55) | 5.60 (1.69) | 6.24 (1.53) | 6.38 (1.37) |
| Arousal b,c | ||||
| Neutral | 5.17 (1.88) | 4.40 (1.94) | 5.07 (1.71) | 4.80 (1.57) |
| Alcohol | 5.63 (2.11) | 4.83 (2.10) | 5.55 (1.79) | 5.14 (1.36) |
| Prestrategy | Poststrategy | Prestrategy | Poststrategy | |
| BHT | 32.66 (12.05) | 33.13 (10.95) | 31.61 (10.63) | 33.73 (11.38) |
| Taste testb | 50.45 (23.75) | 42.38 (16.98) | 58.34 (34.81) | 55.56 (37.38) |
| TMS | 30.48 (6.22) | 32.59 (6.41) | ||
| Tension | 3.00 (1.73) | 3.65 (2.60) | ||
| Follow-up | Follow-up | |||
| Practice | ||||
| Days/wk | 3.73 (1.77) | 3.35 (1.87) | ||
| Min/d | 9.02 (4.00) | 8.38 (3.48) | ||
| Engagement | 3.30 (0.92) | 3.35 (0.73) | ||
Abbreviations: BHT, breath holding test; TMS, Toronto Mindfulness Scale.
aThree-way (cue type x time x group) interaction.
bMain effect of time.
cMain effect of cue type (see text).
Figure 2.
Group x time effect on mean (±SEM) heart rate variability (RMSSD) for relaxation and mindfulness at baseline (open bars) and during (filled gray bars) relaxation or mindfulness (see details on Bonferroni corrected posthoc tests in text).
There were no group effects or time x group interaction (P values >.1) on distress tolerance (breath-holding time), although participants showed a trend toward longer breath-holding times after (i.e., at the behavior 2 time point) compared with before strategy instructions (behavior 1 time point; F(1,64) = 3.911, P =.052; Table 2).
At follow-up there were no group differences in the number of days of strategy practice, duration of practice per occasion, or level of engagement during practice (Table 2; P values >.1).
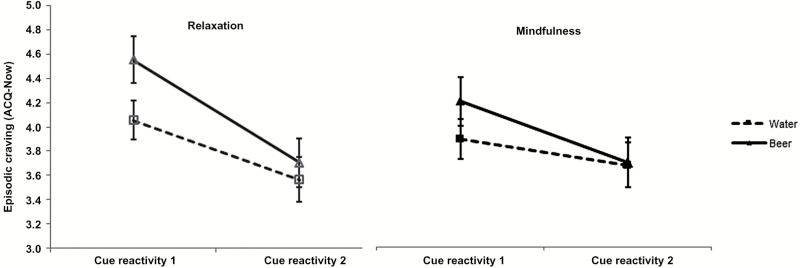
Acute Strategy Effects on Cue Reactivity
Subjective cue-induced craving (ACQ-Now) showed main effects for cue type (water, beer; F(1,62) = 21.94, P <.001, = 0.261) and time (cue reactivity 1, cue reactivity 2; F(1,62) = 38.272, P <.001, = 0.382), along with a cue-type x time interaction (F(1,62) = 17.214, P <.01, = 0.217). The latter reflected larger decreases in alcohol craving from pre- to poststrategy in response to in vivo beer cues (d = 0.574, P <.001) relative to in vivo water cues (d = 0.357, P <.001) in both groups (Figure 3). There was also a trend-level time x group interaction (F(1,62) = 3.805, P =.056, = 0.058), reflecting steeper reductions in ACQ-Now scores in the relaxation group (d = 0.722, P <.001) relative to the mindfulness group (d = 0.317, P =.004).
Figure 3.
Mean (±SEM) cue-induced craving during cue reactivity procedure in response to neutral (water; squares) and alcohol (beer; triangles) cues pre- and post-relaxation and mindfulness.
Affect grid valence (pleasantness) ratings showed no significant main effects or 2-way interactions (F values ≤1.926, P >.1). However, there was a significant 3-way interaction (F(1,57) = 4.768, P =.033, = 0.077), which appeared to reflect a greater reduction in cue-induced pleasantness during beer cue reactivity (cue-reactivity 1 to cue-reactivity 2; d = 0.274) but not during water reactivity (d < 0.1) in the relaxation group (Table 2). However, the relevant Bonferroni corrected posthoc test was not significant (P >.1).
Arousal ratings from the affect grid showed a main effect of cue type, with higher levels of arousal to alcohol cues relative to neutral cues (F(1,57) = 13.284, P =.001, = 0.189). In addition, there was a main effect of time (F(1, 57) = 7.513, P =.008, = 0.116), reflecting an overall reduction in arousal from pre- to poststrategy in both groups (Table 2). However, there were no 2- or 3-way interactions (F values ≤ 1.135, P >.1). In addition, there were no main effects or interactions on systolic (F values ≤2.590, P >.1) or diastolic BP (F values ≤2.651, P >.1).
Longer Term Effects on Background Craving and Affect
ACQ-Now scores reflecting craving in the absence of the structured cue reactivity procedure (i.e., background-craving) showed a reduction from the baseline to follow-up assessment time points (F(1,66) = 54.564, P <.001, = 0.453) but no main or interaction effects involving group (F ≤ 2.883, P >.094). There were also no main effects or interactions on the longer term assessments of pleasantness and arousal (F values ≤ 2.476, P >.1).
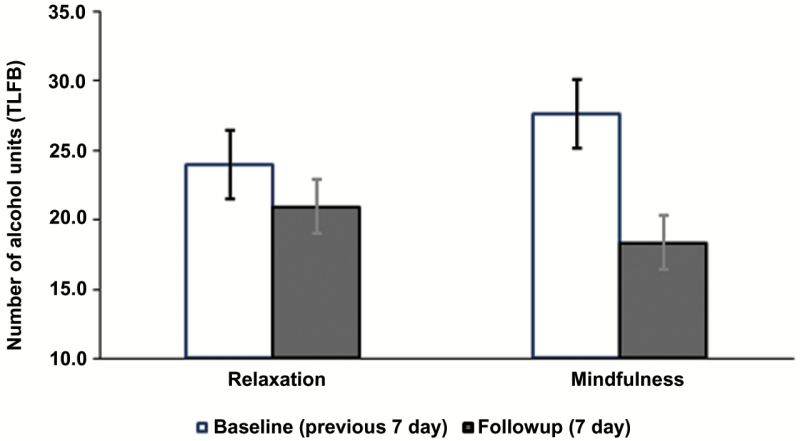
Acute and Longer Term Effects on Alcohol Consumption
There was only a main effect of time on within-session drinking during the beer taste-test (F(1, 65) = 4.551, P =.036, = 0.065; Table 2) and no effects involving group (F values < 2.44, P >.1). There was also a main effect of time (baseline, follow-up; F(1,66) = 19.699, P <.001, = 0.230) on the TLFB assessment of previous 7-day drinking. Critically, however, this was qualified by a time x group interaction (F(1,66) = 5.175, P =.026, P =.037, = 0.073). As can be seen in Figure 4, the interaction reflected a larger reduction in previous 7-day alcohol consumption from baseline to follow-up in the mindfulness group (-9.31 units or 74.5 g of pure alcohol; P <.001, d = 0.593) relative to the relaxation group (-3.00 units or 24 g of alcohol, P >.1, d = 0.268). The change in taste test consumption was not correlated with alcohol consumption at follow up (TLFB) in either group (r values ≤0.22, P >.1).
Figure 4.
Alcohol consumption: mean (±SEM) number of “units” of alcohol (1 unit = 8 g pure alcohol) consumed in the previous 7 days using the timeline followback (TLFB) procedure.
When group, practice, credibility, and expectancy along with their interactions were entered into a multiple regression model, group was the only significant predictor of TLFB-change scores (β = 6.45, SE = 2.89, P =.028).
Discussion
In this study, we examined the acute and longer term effects of ultra-brief mindfulness training on cue reactivity, affect, autonomic activity, and alcohol consumption in at-risk drinkers. Participants rated mindfulness and the control relaxation strategies as equivalently credible, had similar expectancies regarding beneficial effects, and practiced each strategy to a similar extent across the 7-day follow-up. Bearing this equivalence in mind, our primary finding was that despite the brevity of strategy instructions, the mindfulness group, but not the relaxation group, showed significant reductions in alcohol consumption (reductions of 9.31 units or 74.5g vs 3 units or 24 g of pure alcohol, respectively). On the other hand, the relaxation group showed significantly increased HRV in line with increased parasympathetic (or reduced sympathetic) influence on cardiac activity during strategy use (Sakakibara et al., 1994), and a trend-level interaction suggested larger generalized reductions in craving in the relaxation group. Descriptively, the 3-way interaction on affect-valence also appeared to reflect the effect of relaxation on alcohol cue-induced pleasantness, although the relevant Bonferonni corrected posthoc test was not significant.
The apparently distinct effects of mindfulness and relaxation are consistent with the proposal that these techniques have different psychological and physiological mechanisms of action (Dunn et al., 1999). The more limited effects of mindfulness on evaluative aspects of cue reactivity are consistent with instructions to not control or evaluate subjective experiences of craving. In contrast, other lab-based mindfulness studies (particularly in smokers) have demonstrated a larger downregulation of craving following brief mindfulness instructions. However, these effects have generally been observed when mindfulness was compared with an inactive control condition (see review by Serfaty et al., 2017).
In addition, the absence of an effect on autonomic functioning (assessed via HRV) during mindfulness is consistent with the idea that any relaxation response following mindfulness instructions might have been offset by accompanying effortful mental activity, especially when instructions such as those used here explicitly describe the anticipated mindful state as one of alertness rather than relaxation (Lumma et al., 2015). By contrast, the ostensible increase in parasympathetic activity and relatively large reduction in cue-elicited craving in the relaxation group is consistent with instructions related to arousal reduction (Hoffman et al., 1982), which are in turn consistent with the general treatment goals of therapies that aim to downregulate the intensity of affective states (i.e., cognitive/behavioral therapies). Although the effect of relaxation on craving was >2-fold larger than mindfulness, the posthoc effects should be treated with caution until replicated, as they were based on a trend-level interaction (P =.056). Nonetheless, these effects are broadly in line with recent findings in smokers (Beadman et al., 2015) and heavy drinkers (Murphy and MacKillop, 2014) showing that use of emotion regulation strategies (reappraisal and distraction respectively), but not mindfulness-like strategies, result in immediate reductions in craving. In addition, the effects on parasympathetic activity and craving vs drinking behavior may reflect differing time courses of action of relaxation and mindfulness, respectively. There were no between-group differences in acute (taste-test) drinking, and taste-test quantities did not correlate with longer-term (TLFB) drinking. Therefore, the effects of mindfulness on alcohol consumption may be time dependent, only emerging after a delay. Future research should include a reassessment of subjective and physiological cue reactivity and acute drinking behavior (taste test) measures to determine the longer-term effects of mindfulness/relaxation on these important outcomes.
As well as their obvious clinical implications, studies that examine changes in drug-use following mindfulness may be especially informative based on theoretical consideration (Levin et al., 2012). Of the recent relevant laboratory studies that examine both drug/alcohol use behavior and intensity of internal subjective states (Bowen and Marlatt, 2009; Rogojanski et al., 2011; Ostafin et al., 2012; Murphy and MacKillop, 2014; Ruscio et al., 2016), we are aware of only one study that showed a clear reduction in consumption (smoking) following brief mindfulness instructions compared with control (Bowen and Marlatt, 2009). However, despite being an important early demonstration of positive effects of brief mindfulness instructions on drug use, that study has some limitations. For example, subjects appeared to be very light smokers and hence may not have shown the high level of automaticity in relation to smoking behavior which is assumed to be a primary target of mindfulness interventions (see below). In addition, expectancy and other important potential confounds were not controlled for. By applying a number of methodological improvements (use of a carefully matched active control, randomized, double-blind allocation, expectancy and credibility assessment), we believe that the current study provides strong evidence for a reduction in drug/alcohol-use behavior following very brief mindfulness training. Comparisons between 2 active psychosocial interventions rarely yield significant differences (Wampold and Imel, 2015), underscoring the strength of the current findings.
Importantly, the effects were demonstrated in a clinically relevant, albeit non-treatment-seeking group of drinkers at risk of harm from alcohol. From an experimental perspective in fact, the presence of high levels of consumption and/or elevated indices of dependence may be particularly important when studying the effects of mindfulness in the laboratory. Specifically, lighter, social, or episodic drinkers/drug-users are likely to have a limited reward-learning history, and since mindfulness is proposed to act through a weakening of the influence of automatic processes on behavior (Ostafin, 2015), it is possible that the neurobiological substrate upon which mindfulness would act is absent in lighter users. The most appropriate participants to test the effects of mindfulness on behavior may therefore be those with drug/alcohol dependence, with compulsive patterns of use (Bowen et al., 2014). However, laboratory studies must balance this issue with the need to maintain high levels of internal validity, which can be compromised through the recruitment of more severely affected drug/alcohol users, especially due to extraneous variability arising from psychiatric comorbidity.
We recognize that there are a number of limitations of the current study. Firstly, since the current study did not investigate a dose-response relationship, we cannot claim to have established a minimally effective dose of mindfulness, but simply identified a very short training duration that produces reductions in alcohol consumption. Secondly, students were overrepresented in our sample, which may limit the generalizability of our findings. Relatedly, the effects may have been affected by chronicity of at-risk drinking, but onset/duration of such drinking was not assessed. Such assessments, along with a more complete diagnostic workup of participants, would have provided a clearer indication of the relevance of the findings to clinical populations (especially those with AUD). As it stands, our method for screening out participants on the basis of self-declared AUD was probably inadequate to this goal, and it is likely that our sample contained participants with at least mild AUD. On the other hand, we deliberately kept the assessment procedure as simple and brief as possible in this study, because the between-groups differences were expected to be subtle, and more extensive assessment of alcohol-related difficulties (e.g., structured diagnostic assessment) raised a concern that differential effects between mindfulness and an active comparator would have been obscured (Kypri et al., 2007).
Thirdly, strategy use was not actively promoted in the days after the experimental session, and compliance was measured relatively crudely. Frequent assessment of strategy use, along with salient prompts to use the strategy, may have provided us with higher reliability data to examine the relationship between strategy practice and reduction in drinking. On the other hand, given the lack of prompts, the effects of mindfulness observed here may represent a lower bound of those expected in a clinical situation, where between-session practice is actively promoted. This is highly encouraging for the development of brief mindfulness interventions in people at risk of AUD.
It should also be reiterated that our description of a dissociation between craving and behavioral outcomes in the 2 strategy groups was based on a statistical trend for the relevant interaction. Therefore, these findings should be interpreted with caution until replicated. However, the >2-fold larger effect size (in craving reduction) in the relaxation group suggests that this may be a clinically relevant finding. Indeed, beneficial effects of very brief relaxation training on craving have been noted in smokers (Limsanon and Kalayasiri, 2015). Beyond replication of the current findings, future research in at-risk drinkers should also examine the specific effects of relaxation in its own right.
Changes in drinking behavior were not biochemically verified here, and future studies may seek to employ remote alcohol monitoring (e.g., continuous alcohol monitoring technologies), which is ideally suited to short-timeframe assessments and participants for whom liver enzyme tests may not serve as sensitive or specific indices of problematic drinking. If such monitoring were combined with remote assessment of craving, this would also enable an objective assessment (or verification) of recent drinking in relation to craving assessment, allowing more sophisticated modelling of the change process. Overall, our study did not make any specific attempt (and was not designed) to delineate the detailed mechanistic processes that may be responsible for mindfulness’s effects on behavior change. It could be argued, for example, that our mindfulness instructions might have additionally encouraged reappraisal of craving sensations and that our observed effects were secondary to this form of emotion regulation (Garland et al., 2014).
Finally, while we made efforts to ensure blinding to strategy condition, we did not test the integrity of the blind for participants or experimenters. Relatedly, we did not determine whether participants had previous experience of mindfulness or relaxation, which could have affected their response to these strategies and unblinded them to condition allocation upon exposure to the instructions. While expectancy effects might have been introduced by including questions about meditation experience during the screening/assessment phase of the experiment, retrospective assessment of experience (at the end of the follow-up) would have allowed us to factor this variable into the interpretation of our findings.
To summarize, we found that ultra-brief in-session mindfulness instruction plus similarly brief instructions for out-of-session practice was associated with a robust decrease in alcohol consumption over the course of a week. The alternative, the control relaxation strategy, was associated with increased parasympathetic activity during strategy use, and, based on a trend-level interaction, potentially larger acute reductions in craving. The findings suggest that participants can be easily and rapidly trained in mindfulness, and this may therefore be a useful adjunctive strategy in brief interventions for excessive drinking.
Funding
This work was supported by individual funds awarded to D.I. and S.S. by the Research Department of Clinical, Educational and Health Psychology, University College London.
Statement of Interest
None.
Acknowledgments
The authors thank Sharinjeet Dhiman for administrative support.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. (2001) The alcohol use disorders identification test. Guidelines for use in primary care. Geneva: World Health Organization: Department of Mental Health and Substance Dependence. [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JMG. (2008) Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment 15:329–342. [DOI] [PubMed] [Google Scholar]
- Beadman M, Das RK, Freeman TP, Scragg P, West R, Kamboj SK. (2015) A comparison of emotion regulation strategies in response to craving cognitions: effects on smoking behaviour, craving and affect in dependent smokers. Behav Res Ther 69:29–39. [DOI] [PubMed] [Google Scholar]
- Beck AT, Wright FD, Newman CF, Liese BS. (2001) Cognitive therapy of substance abuse. New York: Guilford Press. [PubMed] [Google Scholar]
- Bertholet N, Daeppen J-B, Wietlisbach V, Fleming M, Burnand B. (2005) Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Int Med 165:986–995. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, … and Marlatt A. (2009) Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse 30:295– 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. (2009) Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychol Addictive Behav 23:666–671. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Carroll HA, Harrop E, Collins SE, Lustyk MK. (2014) Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry 71:547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Drobes DJ, Unrod M, Heckman BW, Oliver JA, Roetzheim R, Karver SB, Small BJ (2011) Varenicline effects on craving, cue reactivity, and smoking reward. Psychopharmacology 218:391–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Minnix-Cotton CA, Byrne SA, Kober H, Weinstein AJ. (2011) Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend 119:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Elwafi HM, Davis JH. (2013) Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychol Addict Behav 27:366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. (1994) Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess 6:117. [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. (2008) Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford JR, Henry JD, Crombie C, Taylor EP. (2001) Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol 40:429–434. [DOI] [PubMed] [Google Scholar]
- Davis JM, Manley AR, Goldberg SB, Smith SS, Jorenby DE. (2014) Randomized trial comparing mindfulness training for smokers to a matched control. J Subst Abuse Treat 47:213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. (2000) Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 31:73–86. [DOI] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. (1996) Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Method 1:170. [Google Scholar]
- Dunn BR, Hartigan JA, Mikulas WL. (1999) Concentration and mindfulness meditations: unique forms of consciousness? Appl Psychophysiol Biofeedback 24:147–165. [DOI] [PubMed] [Google Scholar]
- Elwafi HM, Witkiewitz K, Mallik S, Thornhill TA, IV, Brewer JA. (2013) Mindfulness training for smoking cessation: moderation of the relationship between craving and cigarette use. Drug Alcohol Depend 130:222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A- G, Buchner A. (2007) G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Research Meth 39:175–191. [DOI] [PubMed] [Google Scholar]
- Ferguson SG, Shiffman S. (2009) The relevance and treatment of cue-induced cravings in tobacco dependence. J Subst Abuse Treat 36:235–243. [DOI] [PubMed] [Google Scholar]
- Field A. (2013) Discovering statistics using IBM SPSS statistics. Sage Publications. [Google Scholar]
- Field M, Eastwood B. (2005) Experimental manipulation of attentional bias increases the motivation to drink alcohol. Psychopharmacology 183:350–357. [DOI] [PubMed] [Google Scholar]
- Garland E, Froeliger B, Howard M. (2014) Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Front Psychiatry 4:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. (2016) Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav Res Ther 77:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotink RA, Chu P, Busschbach JJ, Benson H, Fricchione GL, Hunink MM. (2015) Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PloS One 10:e0124344. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Grant S, Hempel S, Colaiaco B, Motala A, Shanman RM, Booth M, Dudley W, Sorbero ME. (2015) Mindfulness-based relapse prevention for substance use disorders: a systematic review. Santa Monica: National Defense Research Institute, RAND Corporation. Available at http://www.rand.org/pubs/research_reports/RR1031.html. Accessed January 1, 2017. [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. (2004) Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res 57:35–43. [DOI] [PubMed] [Google Scholar]
- Hoffman JW, Benson H, Arns PA, Stainbrook GL, Landsberg G, Young JB, Gill A. (1982) Reduced sympathetic nervous system responsivity associated with the relaxation response. Science 215:190–192. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1982) An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry 4:33–47. [DOI] [PubMed] [Google Scholar]
- Kamboj SK, Massey-Chase R, Rodney L, Das R, Almahdi B, Curran HV, Morgan CJ. (2011) Changes in cue reactivity and attentional bias following experimental cue exposure and response prevention: a laboratory study of the effects of D-cycloserine in heavy drinkers. Psychopharmacology 217:25–37. [DOI] [PubMed] [Google Scholar]
- Kamboj SK, Joye A, Das RK, Gibson AJ, Morgan CJ, Curran HV. (2012) Cue exposure and response prevention with heavy smokers: a laboratory-based randomised placebo-controlled trial examining the effects of D-cycloserine on cue reactivity and attentional bias. Psychopharmacology 221:273–284. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. (2005) Why do young people drink? A review of drinking motives. Clin Psychology Rev 25:841–861. [DOI] [PubMed] [Google Scholar]
- Kypri K, Langley JD, Saunders JB, Cashell‐Smith ML. (2007) Assessment may conceal therapeutic benefit: findings from a randomized controlled trial for hazardous drinking. Addiction 102:62–70. [DOI] [PubMed] [Google Scholar]
- Lee EB, An W, Levin ME, Twohig MP. (2015) An initial meta-analysis of Acceptance and Commitment Therapy for treating substance use disorders. Drug Alcohol Depend 155:1–7. [DOI] [PubMed] [Google Scholar]
- Leigh J, Bowen S, Marlatt GA. (2005) Spirituality, mindfulness and substance abuse. Addict Behav 30:1335–1341. [DOI] [PubMed] [Google Scholar]
- Levin ME, Hildebrandt MJ, Lillis J, Hayes SC. (2012) The impact of treatment components suggested by the psychological flexibility model: a meta-analysis of laboratory-based component studies. Behav Ther 43:741–756. [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, Lazar M. (2017) Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J Subst Abuse Treat 75:62–96. [DOI] [PubMed] [Google Scholar]
- Limsanon T, Kalayasiri R. (2015) Preliminary effects of progressive muscle relaxation on cigarette craving and withdrawal symptoms in experienced smokers in acute cigarette abstinence: a randomized controlled trial. Behav Ther 46:166–176. [DOI] [PubMed] [Google Scholar]
- Lotan G, Tanay G, Bernstein A. (2013) Mindfulness and distress tolerance: relations in a mindfulness preventive intervention. Int J Cogn Ther 6:371–385. [Google Scholar]
- Lumma A-L, Kok BE, Singer T. (2015) Is meditation always relaxing? Investigating heart rate, heart rate variability, experienced effort and likeability during training of three types of meditation. Int J Psychophysiol 97:38–45. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Marques J K. (1977). Meditation, self-control, and alcohol use. In: Behavioral self-management: strategies, techniques, and outcomes (Stuart Richard B., ed). New York: Brunner/ Mazel. [Google Scholar]
- May J, Andrade J, Panabokke N, Kavanagh D. (2004) Images of desire: cognitive models of craving. Memory 12:447–461. [DOI] [PubMed] [Google Scholar]
- McCabe C, Cowen PJ, Harmer CJ. (2009) NK1 receptor antagonism and the neural processing of emotional information in healthy volunteers. Int J Neuropsychopharmacol 12:1261–1274. [DOI] [PubMed] [Google Scholar]
- Mermelstein LC, Garske JP. (2015) A brief mindfulness intervention for college student binge drinkers: a pilot study. Psychol Addict Behav 29:259–269. [DOI] [PubMed] [Google Scholar]
- Mikulas WL. (2011) Mindfulness: significant common confusions. Mindfulness 2:1–7. [Google Scholar]
- Murphy CM, MacKillop J. (2014) Mindfulness as a strategy for coping with cue‐elicited cravings for alcohol: an experimental examination. Alcohol Clin Exp Res 38:1134–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE (2010) Alcohol use disorders: preventing the development of hazardous and harmful drinking. NICE Public Health Guidance 24:1–96. [Google Scholar]
- Ostafin BD. (2015) Taming the wild elephant: mindfulness and its role in overcoming automatic mental processes. In: Handbook of mindfulness and self-regulation, pp 47–63. Springer. [Google Scholar]
- Ostafin BD, Bauer C, Myxter P. (2012) Mindfulness decouples the relation between automatic alcohol motivation and heavy drinking. J Soc Clin Psychol 31:729. [Google Scholar]
- Rogojanski J, Vettese LC, Antony MM. (2011) Coping with cigarette cravings: comparison of suppression versus mindfulness-based strategies. Mindfulness 2:14–26. [Google Scholar]
- Rood L, Roelofs J, Bögels SM, Arntz A. (2012) The effects of experimentally induced rumination, positive reappraisal, acceptance, and distancing when thinking about a stressful event on affect states in adolescents. J Abn Child Psychol 40:73–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rösner S, Willutzki R, Zgierska A. (2015) Mindfulness‐based interventions for substance use disorders. The Cochrane Library. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AC, Muench C, Brede E, Waters AJ. (2016) Effect of brief mindfulness practice on self-reported affect, craving, and smoking: a pilot randomized controlled trial using ecological momentary assessment. Nicotine Tob Res 18:64–73. [DOI] [PubMed] [Google Scholar]
- Russel JA, Weiss A, Mendelsohn GA. (1989) Affect grid: a single-item scale of pleasure and arousal. J Person Soc Psychol 57:493–502. [Google Scholar]
- Sakakibara M, Takeuchi S, Hayano J. (1994) Effect of relaxation training on cardiac parasympathetic tone. Psychophysiology 31:223–228. [DOI] [PubMed] [Google Scholar]
- Sayette MA. (2016) The role of craving in substance use disorders: theoretical and methodological issues. Ann Rev Clin Psychol 12:407–433. [DOI] [PubMed] [Google Scholar]
- Sayette MA, Griffin KM, Sayers WM. (2010) Counterbalancing in smoking cue research: a critical analysis. Nicotine Tob Res:ntq159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlam TR, Fiore MC, Smith SS, Fraser D, Bolt DM, Collins LM, … and Loh WY. (2016) Comparative effectiveness of intervention components for producing long‐term abstinence from smoking: a factorial screening experiment. Addiction 111:142–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA. (1994) Low level of response to alcohol as a predictor of future alcoholism. Am J Psychiatry 151:184–189. [DOI] [PubMed] [Google Scholar]
- Serfaty S, Gale G, Beadman M, Froeliger B, Kamboj SK. (2017) Mindfulness, acceptance and defusion strategies in smokers: a systematic review of laboratory studies. Mindfulness. Accessed on July 17, 2017. doi 10.1007/s12671-017-0767-1 [In press]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonin E, Van Gordon W. (2015) Practical recommendations for teaching mindfulness effectively. Mindfulness 6:952–955. [Google Scholar]
- Singleton E, Henningfield J, Tiffany S. (1994) Alcohol craving questionnaire: ACQ-Now: background and administration manual. Baltimore: NIDA Addiction Research Centre. [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz KM. (2009) Enhanced negative emotion and alcohol craving, and altered physiological responses following stress and cue exposure in alcohol dependent individuals. Neuropsychopharmacology 34:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Li C-S R. (2007) Imaging stress-and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug Alc Rev 26:25–31. [DOI] [PubMed] [Google Scholar]
- Slutske WS. (2005) Alcohol use disorders among US college students and their non–college-attending peers. JAMA Psychiatry 62:321–327. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. (1992) Timeline follow-back. In: Measuring alcohol consumption, pp 41–72. Springer. [Google Scholar]
- Spada M. (2012) Overcoming problem drinking. Hachette UK. [Google Scholar]
- Spielberger CD. (2010) Test anxiety inventory. Wiley Online Library. [Google Scholar]
- Sütterlin S, Schroijen M, Constantinou E, Smets E, Van den Bergh O, Van Diest I. (2013) Breath holding duration as a measure of distress tolerance: examining its relation to measures of executive control. Front Psychol 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szasz PL, Szentagotai A, Hofmann SG. (2012) Effects of emotion regulation strategies on smoking craving, attentional bias, and task persistence. Behav Res Ther 50:333–340. [DOI] [PubMed] [Google Scholar]
- Tarvainen MP, Niskanen J-P, Lipponen JA, Ranta-Aho PO, Karjalainen PA. (2014) Kubios HRV–heart rate variability analysis software. Comput Methods Programs Biomed 113:210–220. [DOI] [PubMed] [Google Scholar]
- Task Force of The European Society of Cardiology (1996) Heart rate variability standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17:354–381. [PubMed] [Google Scholar]
- Tiffany ST, Wray JM. (2012) The clinical significance of drug craving. Ann N Y Acad Sci 1248: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treanor M. (2011) The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clin Psych Rev 31:617–625. [DOI] [PubMed] [Google Scholar]
- Vinci C, Peltier M, Shah S, Kinsaul J, Waldo K, McVay M, Copeland A. (2014) Effects of a brief mindfulness intervention on negative affect and urge to drink among college student drinkers. Behav Research Ther 59:82–93. [DOI] [PubMed] [Google Scholar]
- Walsh K, Das RK, Kamboj SK. (2017) The subjective response to nitrous oxide is a potential pharmaco-endophenotype for alcohol use disorder: a preliminary study with heavy drinkers. Int J Neuropsychopharmacol 20:346–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold BE, Imel ZE. (2015) The great psychotherapy debate: the evidence for what makes psychotherapy work. Routledge. [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N. (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet 382:1575–1586. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. (2004) Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US Preventive Services Task Force. Ann Int Med 140:557–568. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. (2010) Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol 78:362–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, Hsu SH. (2013. a) Mindfulness-based relapse prevention for substance craving. Addict Behav 38:1563–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Lustyk MKB, Bowen S. (2013. b) Retraining the addicted brain: a review of hypothesized neurobiological mechanisms of mindfulness-based relapse prevention. Psychol Addict Behav 27:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. (1983) The hospital anxiety and depression scale. Acta Psychiat Scand 67:361–370. [DOI] [PubMed] [Google Scholar]