Abstract
Background
The development of spontaneous kidney transplant tolerance has been associated with numerous B cell-related immune alterations. We have previously shown that tolerant recipients exhibit reduced B cell receptor (BCR) signalling and higher IL-10 production than healthy volunteers. However, it is unclear whether CD4+T cells from tolerant recipients also display an antiinflammatory profile that could contribute to graft maintenance.
Methods
CD4+T cells were isolated from kidney transplant recipients who were identified as being tolerant recipients, patients with chronic-rejection or healthy volunteers. CD4+T cells from the 3 groups were compared in terms of their gene expression profile, phenotype and functionally upon activation.
Results
Gene expression analysis of transcription factors and signalling proteins, in addition to surface proteins expression and cytokine production, revealed that tolerant recipients possessed fewer Th17 cells and exhibited reduced Th17 responses, relative to patients with chronic rejection or healthy volunteers. Furthermore, impaired TCR signalling and altered cytokine cooperation by monocytes contributed to the development of Th17 cells in tolerant recipients.
Conclusions
These data suggest that defective proinflammatory Th17 responses may contribute to the prolonged graft survival and stable graft function, which is observed in tolerant recipients in the absence of immunosuppressive agents.
Introduction
Kidney transplantation is the gold-standard therapeutic option for treating end-stage renal diseases but the benefits of this approach are limited by graft rejection. The ideal scenario following transplantation is the development of clinical “operational tolerance”, whereby the allograft is stably maintained and functions normally in the absence of immunosuppression1–3. However, this is a rare event, which seldom occurs in kidney transplant recipients.
The development of operational tolerance has been associated with the maintenance of B cell numbers and an increased expression of B cell-related genes4–7. However, the role of other lymphocyte subsets in the development of operational tolerance remains unclear. In 2006, Louis et al, compared the phenotype of peripheral blood mononuclear cells (PBMC) between i) tolerant renal transplant recipients; ii) recipients with chronic-rejection or stable graft function under immunosuppression; and iii) healthy individuals8. No significant difference in terms of percentages of T cells, proliferation or cytokine production between groups was observed8. The authors demonstrated that recipients with chronic-rejection possessed significantly fewer peripheral CD25hiCD4+T cells than tolerant recipients and healthy individuals, suggesting that patients with chronic-rejection had a deficit in regulatory T cells, as tolerant recipients displayed a similar profile to healthy individuals. Conversely, no significant differences were observed in the relative ratios of T cell subsets, proliferation or cytokine production between the groups analysed8. In 2007, Brouard et al, proceeded to identify peripheral biomarkers for operational tolerance9. By comparing the gene expression profiles of 75 renal-transplant patients, it was demonstrated that genes characterizing proinflammatory Th1/Th2 responses such as TNF-α, IL-4 and IL-10 were consistently reduced in tolerant recipients, compared to patients with chronic-rejection9. Furthermore, 90% of known proinflammatory cytokines were also reduced, whereas FOXP3 expression was increased in tolerant patients, compared to patients with chronic-rejection9. The authors highlighted that their tolerant patients did not display clinical evidence of immune-incompetency, corroborating a previous study in which patients were evaluated for IFN-γ responses in vitro after influenza vaccination10. However, in the latter study, a trend was observed for tolerant recipients to exhibit inferior immune-responses, relative to patients under immunosuppression or healthy volunteers. However, this finding did not reach statistical significance, possibly due to the low number of tolerant patients analysed (n=4)10.
We reported that CD4+T cells from tolerant recipients exhibited hyporesponsiveness to donor antigens and a higher ratio of FoxP3/α-1,2-mannosidase gene expression compared to patients with chronic-rejection4. In addition, we recently demonstrated that CD4+T cells from tolerant recipients were defective in their ability to produce IL-2 and IL-4 following TCR activation, relative to healthy volunteers11. Furthermore, we showed a tendency for B cells from tolerant recipients to be hyporesponsive, compared to cells isolated from healthy volunteers11,12. As such, we hypothesized that CD4+T cells from tolerant recipient would exhibit reduced effector responses compared to patients with chronic-rejection and healthy volunteers. T cell responses from a cohort of tolerant renal transplant recipients were compared with age/gender-matched healthy volunteers and patients with chronic-rejection. The data presented demonstrate that tolerant patients possess fewer Th17 cells and exhibit reduced TCR signalling, compared to healthy controls and patients with chronic-rejection. Together, these results suggest that a decrease in Th17 cell frequency/response and a consequential reduction in IL-17 production in tolerant patients may contribute to prolonged allograft survival.
Materials and Methods
Patients
Peripheral blood samples were acquired from renal transplant recipients and healthy volunteers as part of the Genetic Analysis & Monitoring of Biomarker of Immunological Tolerance (GAMBIT) study with informed consent and ethical approval (Institute of Child Health/Great Ormond Street Hospital; REC: 09/H0713/12) in accordance with the principles of the Declarations of Helsinki. Tolerant recipients (n=17) were defined as having a functionally stable transplanted kidney without immunosuppression for more than 1 year. Patients with chronic-rejection (n=32) were defined as kidney transplant recipients with graft dysfunction, despite adequate immunosuppression, with a recent biopsy showing signs of immunologically driven chronic-rejection in accordance with the BANFF Criteria13. Healthy controls (n=12) were volunteers who were age and gender matched to renal transplant patients. Patient characteristics are described in Table 1. PBMCs were isolated by Ficoll-Hypaque (PAA, Buckinghamshire, UK) density gradient centrifugation in a blinded manner and cryopreserved prior to batch analysis.
Table 1.
Clinical data of tolerant kidney transplant recipients, patients with chronic-rejection and healthy volunteers.
| Patient Data | Healthy Control | Tolerant | Chronic Rejection |
|---|---|---|---|
| Number of patients | 12 | 17 | 32 |
| Male | 10 | 14 | 22 |
| Female | 2 | 3 | 10 |
| Donor (Living/Deceased) | - | (9/8) | (11/21) |
| Age in years [mean (range)] | 48.0 (23-72) | 50.2 (22-77) | 44.3 (18-72) |
| Recipient age at Transpl [mean (range)] | - | 31.3 (11-56) | 34.9 (11-62) |
| Years immunosuppression free [mean (range)] | - | 6.1 (1-23) | - |
| HLA mismatches per group | |||
| Number of patients with no mismatches | - | 6 | 0 |
| Number of patients with HLA (A or B) mismatches | - | 2 | 2 |
| Number of patients with HLA (A and B) mismatches | - | 1 | 7 |
| Number of patients with HLA (A + DR) mismatches | - | 0 | 3 |
| Number of patients with HLA (B + DR) mismatches | - | 0 | 3 |
| Number of patients with HLA (A, B, DR) mismatches | - | 7 | 14 |
| Missing data | - | 1 | 3 |
| Immunosuppressive Regime | |||
| CNI | - | - | 1 |
| MMF | - | - | 1 |
| CNI + MMF | - | - | 6 |
| CNI + Aza | - | - | 2 |
| CNI + Steroid | - | - | 4 |
| MMF + Steroids | - | - | 1 |
| CNI + MMF + Steroids | - | - | 14 |
| CNI + Aza + Steroids | - | - | 3 |
| Donor-specific antibodies | |||
| No DSA | - | 14 | 16 |
| DSA Class I | - | 2 | 6 |
| DSA Class II | - | 1 | 4 |
| DSA Class I and II | - | 0 | 5 |
| Missing data | 0 | 1 | |
| Renal Function Parameters | |||
| Creatinine (mmols/L) [mean±SD] | - | 116.4±38.5 | 224.9±92.1 |
| eGFR (mL/min/1.73m2) [mean±SD] | - | 64.9±20.1 | 32.8±14.1 |
| Cell Count | |||
| Lymphocytes count x 109 [mean±SD] | 2.18±0.4 | 2.07±1.2 | 1.42±0.9 |
CNI, Calcineurin inhibitor (Cyclosporine or Tacrolimus). Aza, azathioprine. MMF, mycophenolate mofetil. DSA: donor-specific antibodies. eGFR: estimated glomerular filtration rate. SD: standard deviation.
Gene expression analysis
Peripheral blood was drawn into Tempus Blood RNA Tubes (Life Technologies, Paisley, UK), and stored at -20°C. RNA was isolated using the Tempus Spin RNA Isolation kit and cDNA was subsequently synthesized using TaqMan Reverse Transcription Reagents (both Life Technologies, Paisley, UK). Expression of target genes was measured by quantitative real-time PCR platform (qPCR; Fluidigm BioMark) (South San Francisco, CA) where 3 endogenous reference genes were used, as previously described14.
Flow cytometry
3x106 PBMCs were stained with Live/Dead Aqua (Life Technologies) and antibodies specific for the following human markers: anti-CD3-PercP-Cy5.5 (eBioscience), anti-CD20-Brillian Violet (BV)421 (eBioscience), anti-CD4-AlexaFluor700/PercP-Cy5.5 (eBioscience), anti-CD8-APC (eBioscience), anti-CD25-PE (BD), anti-CD14- AlexaFluor647 (BioLegend), anti-CD16-PE (eBioscience), anti-CXCR3-FITC (BioLegend), anti-CCR4-PECy-7 (BioLegend), anti-CCR6-BV605 (BioLegend) anti-CD161-BV421 (BioLegend), anti-CD45RA APCy-7 (BioLegend), anti-HLA-DR PECy7 (eBioscience), anti-CD80 CCR6-BV650 (BioLegend), CD86-FITC (Invitrogen) and CD163-APC/Cy7 (BioLegend) for 30min at 4°C. Cells were acquired on an LSR-Fortessa (BD) with consistent application settings, internal assay-control, fluorescence minus ones (FMO) control, isotype controls and/or biological control. Data was analysed using FlowJo (Tree Star, Inc. OR, USA) with gating strategies provided in the supplemental material.
Monocyte and CD4+T cell isolation and cultures
Monocytes and CD4+T cells were isolated using CD14 Microbeads and the untouched CD4+T cell Isolation Kit II, respectively (both Miltenyi-Biotec, Cologne, Germany). Representative purities are shown in Figure S1. Cells were cultured in X-VIVO (Lonza, Bazel, Switzerland) supplemented with 10% of human serum (BioSera, Nuaille, France), 2mM L-glutamine and 100U/mL penicillin/streptomycin (both Life Technologies). Monocytes were cultured in the presence or absence of LPS (50μg/mL) for 48h. CD4+T cells and monocytes were then cocultured at a 2:1 ratio in the presence or absence of soluble αCD3 (10ng/mL) (eBioscience) for 72h. Cytokine production was measured by cytometric bead array (CBA) with FCAP Array Software v3.0 (BD).
T cell activation
CD4+T cells were isolated using the human CD4+T cell Isolation Kit II (Miltenyi-Biotec) and activated with αCD3/CD28 beads (1:2 bead:cell ratio; Life Technologies). CD25 and CD69 expression was assessed by flow cytometry and cytokine production was measured by CBA 24h and 72h postactivation, respectively.
Th17 differentiation
CD4+T cells were activated with anti-CD3/CD28 beads (1:5 bead:cell ratio) and cultured in X-VIVO supplemented with 4ng/mL IL-1β, 20ng/mL IL-6, 5ng/mL IL-23, 5ng/mL TGF-β 10μg/mL anti-IL-4 and 10μg/ml anti-IFN-γ (all from R&D Systems) for 72h. For Th17 differentiation in the presence of ERK inhibitor, CD4+T cells were activated in the presence or absence of 0.1μg/mL ERK inhibitor (UO126, Tocris Bioscience) (where the inhibitor or DMSO carrier was resupplemented after 36h). Cytokines were analysed at the end of culture by CBA (BD).
ERK activation and western blot
CD4+T cells were activated with 5μg/mL plate bound CD3/28 (R&D) in a 96 U-bottom plate (5x104 cells/well) for 10min at 37°C. Cell pellets were lysed with ice-cold RIPA buffer (Thermo Fisher Scientific) containing protease inhibitors 1X (Calbiochem). Samples were electrophoresed on 10% SDS polyacrylamide gels and transferred to nitrocellulose membranes. Membranes were incubated with phospho-p44/42 MAPK (Erk1/2; Thr202/Tyr204; #9101, Cell Signalling) or p44/42 MAPK (Erk1/2; #9102, Cell Signalling) overnight at 4°C. Proteins were detected with chemiluminescence detection reagents (BIORAD) after HRP-conjugated secondary antibody incubation using ImageQuant LASS4000 mini and quantified with ImageQuant TL software (GE Healthcare Life Science).
Statistical analysis
Statistical tests were performed using Prism 7 software (GraphPad). For all data in graphs summary lines depict mean ± standard error of the mean (SEM) and all individual values are also shown. Nonparametric variables between groups were compared using Kruskal-Wallis tests. Repeated Measurement (RM) 2-way ANOVA was used to compare 2 related variables between groups. Pearson correlation test was used to calculate r and p value between TCR signalling and IL-17 production. Posthoc tests are reported in figure legends. Statistical significance is denoted as follows: *p<0.05, **p<0.01, *** p<0.001 and **** p<0.0001.
Results
Tolerant kidney transplant recipients display a reduced Th17 lineage compartment compared to healthy controls and patients with chronic-rejection
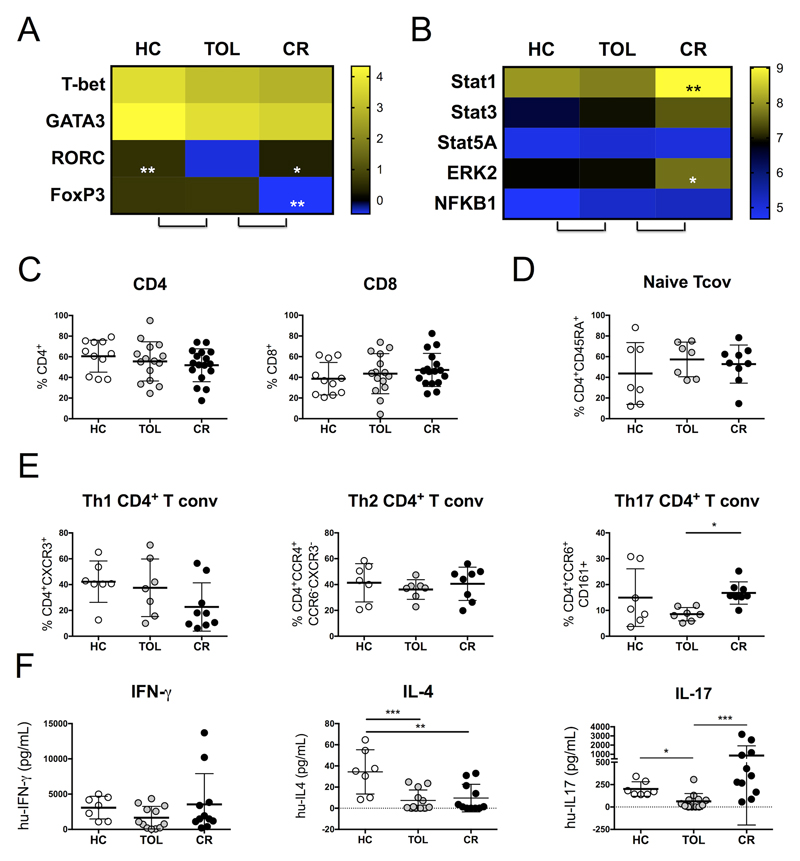
To identify differences in T cell responses between healthy volunteers, tolerant patients and patients with chronic-rejection (Table 1), peripheral blood samples were compared where the expression of T helper(Th) pathway-associated transcription factors and signalling proteins was assessed. FOXP3 expression was significantly reduced in patients with chronic-rejection, as previously reported8,9 (Figure 1A, Figure S2). Conversely, no differences were observed in T bet or GATA3 expression between the 3 groups analysed. Interestingly, RAR-related orphan receptor C (RORC) was expressed at lower levels in tolerant recipients compared to patients with chronic-rejection and healthy controls, suggesting a correlation between a reduced Th17 compartment and transplant tolerance (Figure 1A). Gene expression analyses of signalling proteins revealed a significantly lower expression of STAT1 and ERK2 in tolerant recipients, compared to patients with chronic-rejection (Figure 1B). Moreover, STAT1, STAT3 and ERK2 were also expressed at lower levels in healthy controls, compared to patients with chronic-rejection. Conversely, no significant differences were observed in the expression of these genes between healthy volunteers and tolerant recipients (Figure S2). STAT5A and NFKB1 expression was similar between the 3 groups analysed (Figure 1B).
Figure 1. Tolerant kidney transplant recipients exhibit a reduced Th17 lineage compared to healthy controls and patients with chronic-rejection.
(A) Peripheral blood cell gene expression analysis of transcription factors Tbet, GATA3, RORC and FOXP3 and (B) signalling proteins STAT1, STAT3, STAT5A, ERK2 and NFKB1 from tolerant recipients were compared to healthy volunteers and patients with chronic-rejection. (C) The percentage of CD4 and CD8 was measured in peripheral blood CD3+ cells from transplant recipients and healthy volunteers. (D) The percentage of CD45RA+ naive CD4+T cells and (E) Th1, Th2 and Th17 conventional CD4+T cells was measured in the peripheral blood from patients and healthy volunteers. (F) IFN-γ, IL-4 and IL-17 production by 2x105 CD4+T cells from patients and healthy volunteers was measured by CBA after 72h of anti-CD3/28 activation (1:2 bead:cell ratio). Statistical significance was determined using Kruskal-Wallis ANOVAs with Dunn’s multiple comparison tests and is denoted as follows: ****=P<0.0001, ***=P<0.001, **=P<0.01 and *=P<0.05.
We next analysed the phenotype and relative frequencies of T cell subtypes (Figure S3). No differences were observed in the percentage of CD4+ or CD8+T cells between the 3 groups analysed (Figure 1C), nor in the percentage of CD4+CD45RA+ naïve T cells (Figure 1D). This suggested that the reduced RORC gene expression observed in tolerant recipients was not due to a higher proportion of naïve T cells in circulation15. The relative ratio of Th1, Th2 and Th17 cells in the conventional effector memory T cell compartment was then assessed where Th1 were defined as CXCR3+16, Th2 were CCR4+CXCR3-CCR6-16 and Th17 were CCR6+CD161+17, respectively (Figure S3). We observed that the proportion of Th17 cells was significantly lower in tolerant recipients compared to patients with chronic-rejection, further suggesting a link between a reduced Th17 compartment and tolerance (Figure 1E).
To investigate the function of the patient-derived Th effector cells, total CD4+T cells were stimulated with CD3/CD28 beads for 72h and production of IFNγ, IL-4 and IL-17 was measured by CBA. The amount of IL-17 produced by CD4+T cells from tolerant patients was lower than CD4+T cells from patients with chronic-rejection and healthy volunteers (Figure 1F). IL-4 production was also significantly reduced in tolerant recipients compared to healthy volunteers, as previously shown11. Expression of activation markers CD25 and CD69 in CD4+T cells was analysed to assess whether the decrease in cytokines secreted by CD4+T cells from tolerant patients was due to a defect in T cell activation but no significant differences were observed (Figure S4). Together, these data demonstrate that tolerant recipients have a reduced peripheral Th17 compartment compared to healthy volunteers and patients with chronic-rejection.
Reduced IL-6 production characterized monocytes from tolerant recipients
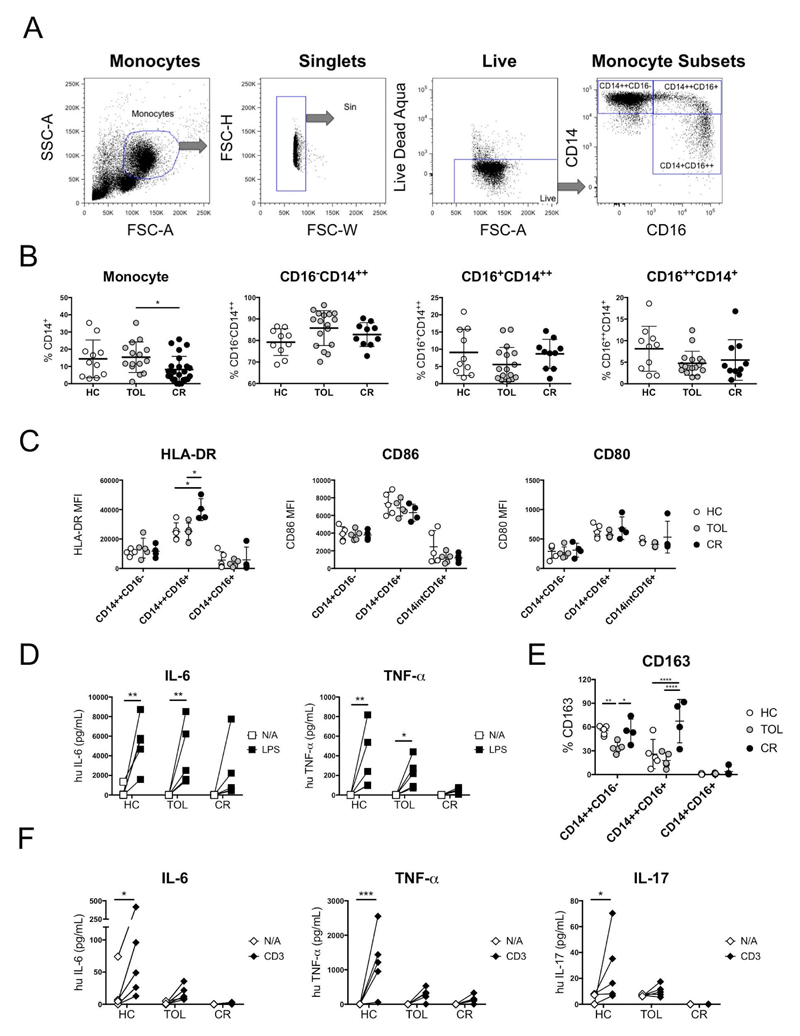
To establish the possible mechanisms behind these observations, we investigated whether modulating microenvironmental factors, such as local proinflammatory cytokines, influenced the differentiation of Th17 cells. Monocytes have been shown to be important for the differentiation of Th17 cells due to their capacity to produce IL-6, IL-1β and TNF-α18. We compared the proportion of classical (CD14++CD16), intermediate (CD14++CD16+; proinflammatory) and non-classical (CD14+CD16++) monocyte subsets19 between patients and healthy volunteers (Figure 2A). The proportion of total monocytes was lower in patients with chronic-rejection compared to tolerant recipients, but not significantly different compared to healthy volunteers (Figure 2B). CD14++CD16+ monocytes from patients with chronic-rejection expressed higher levels of the activation marker HLA-DR, relative to tolerant patients and healthy volunteers (Figure 2C), although no differences were observed in the expression of other activation markers (CD80/CD86) or in any of the other monocyte subsets analysed.
Figure 2. Reduced IL-6 production contributes to impaired Th17 polarization in tolerant recipients.
(A) Representative dot plots and (B) total percentage of CD14, CD14++CD16-, CD14++CD16+ and CD14+CD16++ monocytes in peripheral blood samples from patients and healthy volunteers. Statistical significance was determined using Kruskal-Wallis ANOVAs with Dunn’s multiple comparison tests. (C) HLA-DR, CD86 and CD80 MFI were measured in monocyte subsets from patients and healthy volunteers. Statistical significance was determined using Repeated Measurement (RM) 2-Way ANOVAs with Sidak’s multiple comparison tests. (D) IL-6 and TNF-α production by 1.25x105 monocytes isolated from patients and healthy volunteers was measured after LPS activation (50ng/ml). Statistical significance was determined using RM 2-Way ANOVAs with Sidak’s multiple comparison tests. (E) CD163 expression was measured in monocyte subsets from patients and healthy volunteers. Statistical significance was determined using RM 2-Way ANOVAs with Sidak’s multiple comparison tests. (F) IL-6, TNF-α and IL-17 production was measured in cocultures consisting of 5x104 CD4+T cells and 2.5x104 monocytes in the presence or absence of soluble 10ng/mL anti-CD3, using cells isolated from patients and healthy volunteers. Statistical significance was determined using RM 2-Way ANOVAs with Sidak’s multiple comparison tests. Statistical significance is denoted as follows: ****=P<0.0001, ***=P<0.001, **=P<0.01 and *=P<0.05.
Before investigating the capacity of monocytes to induce IL-17+ cells, we assessed the response of monocytes to lipopolysaccharide (LPS) activation to control for their capacity to secrete IL-6 and TNF-α. Monocytes from tolerant recipients secreted both IL-6 and TNF-α after activation, whereas monocytes from patients with chronic-rejection did not respond (Figure 2D, Figure S1). This was likely due to the effects of the immunosuppressive drugs which have been shown to influence lymphocyte subset distribution14 and decrease IL-6 production by monocytes20. As antithymocyte globulin (ATG) and steroid treatment have been shown to induce expression of CD163, we next analysed the expression of this marker on monocytes21. CD163 was expressed at higher levels on proinflammatory monocytes from patients with chronic-rejection, compared to tolerant recipients (Figure 2E), suggesting that the immunosuppressive treatment in patients with chronic-rejection could affect monocyte responses.
To investigate whether monocytes from tolerant recipients were defective in their ability to polarize CD4+T cells towards a Th17 phenotype, we next performed cocultures of these cells, in the presence of anti-CD3 to activate the T cells, and measured the production of IL-6, TNF-α and IL-17 by CBA (Figure 2F, Figure S1). IL-6, TNF-α and IL-17 levels were significantly decreased in cocultures containing tolerant patient-derived cells, compared to cocultures containing cells from healthy volunteers (Figure 2F). Conversely, monocytes from patients with chronic-rejection did not respond. Overall, these results suggest that impaired cytokine production in the cross-talk between monocytes and T cells from tolerant patients may contribute to a reduced Th17 skewing in these patients.
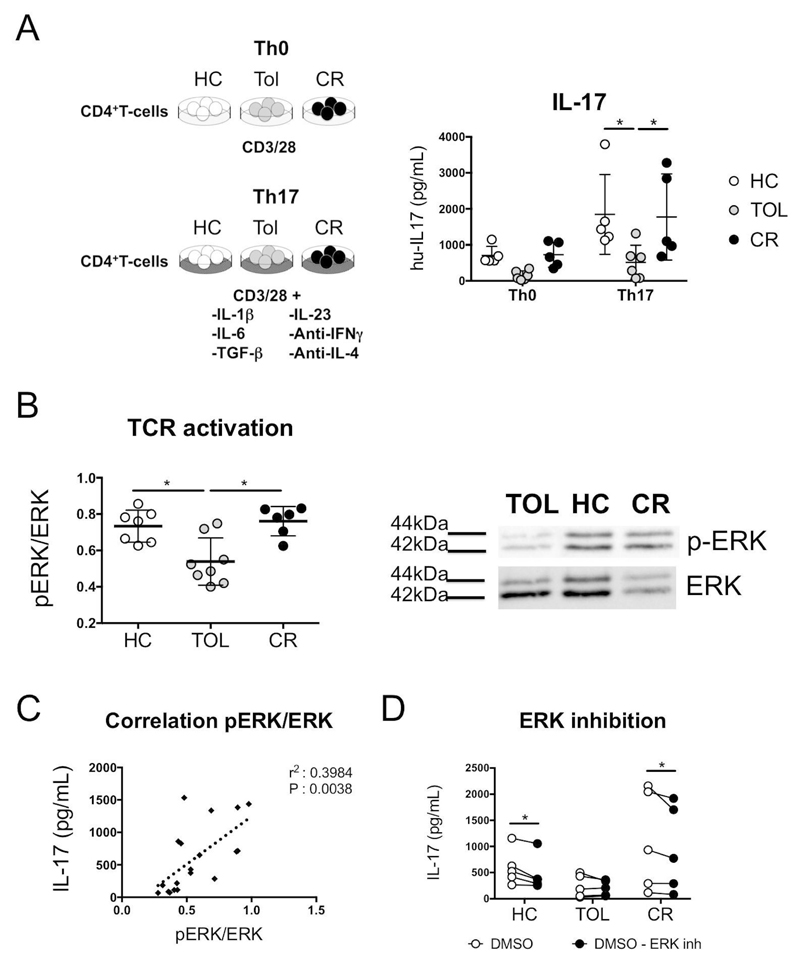
Reduced TCR activation contributes to impaired Th17 polarization in tolerant recipients
Having confirmed the effect of extrinsic factors in the induction of the Th17 lineage, we next assessed the intrinsic capacity of T cells to polarize into Th17 cells. CD4+T cells from patients and healthy volunteers were stimulated in vitro using a Th17 differentiation cocktail (Figure 3A). Despite the presence of all the necessary elements to induce Th17 differentiation, T cells from tolerant recipients displayed a resistance to skew towards a Th17 phenotype, relative to healthy controls and patients with chronic-rejection (Figure 3A). This implied a potential and specific intrinsic defect in T cell from tolerant recipients.
Figure 3. Reduced TCR activation contributes to impaired Th17 polarization in tolerant recipients.
(A) IL-17 produced by 2x105 CD4+T cells from patients and healthy volunteers was measured following anti-CD3/28 activation (1:2 bead:cell ratio) in the presence or absence of a Th17 polarization cocktail (4ng/mL IL-1β, 20ng/mL IL-6, 5ng/mL IL-23, 5ng/mL TGF-β, 10μg/mL αIFN-γ and 10μg/mL αIL-4). Statistical significance was determined using RM 2-Way ANOVAs with Tukey’s multiple comparison tests. (B) ERK phosphorylation was measured in CD4+T cells following activation with 5ug/mL plate bound anti-CD3/28 for 10min via western blot. Statistical significance was determined using Kruskal-Wallis ANOVAs with Dunn’s multiple comparison tests. (C) The correlation between ERK phosphorylation and IL-17 production was assessed using a Pearson correlation test to determine statistical significance. (D) IL-17 produced by CD4+T cells activated with anti-CD3/28 (1:5 bead:cell ratio) in a Th17 polarization cocktail in the presence of ERK inhibitor (100ng/ml) or carrier DMSO was measured. Statistical significance was determined using RM 2-Way ANOVAs with Fisher’s multiple comparison tests. Statistical significance is denoted as follows: **=P<0.01 and *=P<0.05.
Previous studies have shown that blockade of ERK activation in T cells inhibits Th17 cell development in mice and human22. Furthermore, we have demonstrated that phosphorylation of ERK is impaired in B cells from these tolerant recipients, following BCR activation11. As such, we next analysed whether the phosphorylation state of ERK in CD4+T cells differed between the 3 groups, after TCR activation. Reduced ERK phosphorylation was observed in CD4+T cells from tolerant recipients, compared to healthy controls and patients with chronic-rejection (Figure 3B, Figure S5). Furthermore, a positive correlation was observed between ERK phosphorylation and IL-17 production (Figure 3C). To further investigate these findings, we cultured CD4+T cells under Th17 skewing conditions in the presence of a specific ERK-inhibitor. We found that inhibition of ERK phosphorylation reduced IL-17 secretion (Figure 3D), whilst production of a 3rd party cytokine (IL-2) was unaffected (Figure S6). Together, these data suggest that the reduced frequency of circulating Th17 cells in tolerant recipient could be attributed to an impaired intrinsic Th17 polarization capacity.
Discussion
We describe for the first time that tolerant patients exhibit impaired Th17 responses after CD3/28 activation and reduced TCR signalling compared to healthy controls and patients with chronic-rejection. We also demonstrated that the reduction in TCR signalling in tolerant recipients was linked with a decrease in IL-17 production by CD4+T cells. Furthermore, reduced IL-6 and TNF-α production by monocytes, upon coculture with CD4+T cells, may also contribute to the reduction in Th17 responses observed in tolerant recipients.
Previous studies have demonstrated a close relationship between Th17 cells and allograft rejection. In 2010, Deteix et al, investigated how the polarization of CD4+T cell infiltrates in allografts influenced the course of clinical chronic-rejection23. Eleven renal allografts were explanted from recipients with terminal chronic active rejection and T cell subsets were identified in the tissues. Expression of Th-17-associated cytokines (IL-17 and IL-21) was higher in grafts which were rejected in < 8 years, compared to grafts which survived > 8 years. Conversely, the antiinflammatory cytokine IL-10 was expressed at higher levels in grafts that were rejected slower. An analysis of master regulator transcription factors revealed that FOXP3 and GATA-3 were expressed at higher levels in grafts that survived longer whilst RORC2 was expressed more in grafts that were rejected faster. These results demonstrated that a reduced proportion of Th17 cells was associated with prolonged graft survival. In our manuscript, we observe Th17 defective responses in patients with long-term graft acceptance in the absence of immunosuppression. A year later, Chung et al, investigated the relationship between cellular infiltration into allograft tissues and the severity of allograft dysfunction in acute T cell mediated rejection24. They found that Th17 cell infiltration was significantly associated with allograft function and the severity of tissue injury24. These authors proceeded to assess effect of calcineurin inhibitors in Th1/Th2/Th17 responses and observed in vitro and in vivo that tacrolimus suppressed Th1 and Th2, but not Th17 responses25. Our results showed a trend for patients with chronic-rejection to have fewer circulating CXCR3+Th1 cells than healthy volunteers and tolerant recipients, as well as a reduction in the production of IL-4, compared to healthy volunteers. These results could be explained, at least in part, by the fact that the immunosuppressive treatment in patients with chronic-rejection affected their Th1 and Th2 cells, but not Th17 cells.
Monocytes from tolerant recipients can produce some IL-6 and TNFα after LPS activation but in co-culture with activated T cells this production was deficient, as well as that of IL-17. We do not have enough data to dissect whether the reduced cytokine production in the cocultures is fundamental for the Th17 defect observed, as this polarization was also reduced in the presence of an optimal differentiation cocktail. We also observed that monocytes from CR patients secreted negligible levels of TNF-α and IL-6, relative to monocytes from tolerant patients, upon LPS-mediated activation; as previously shown this could be due to steroid treatment in these26.
We have previously demonstrated that B cells from tolerant patients have a reduced ERK phosphorylation state in B cells following CD40-mediated activation, compared to healthy volunteers11. The results presented in this manuscript suggest that reduced ERK signaling may influence the development and polarization of Th17 cells, as previously reported22, and that consequently, Th17 polarization and cell-responses may be limited in tolerant recipients. Combined with our previous observations of reduced B cell responses in tolerant patients11, these findings depict that an antiinflammatory environment may contribute to long-term graft acceptance. Thus, we have provided novel evidence that an incomplete Th17 pathway integrity could contribute to the tolerant state.
The question of whether the responses that we have evidenced are naturally occurring before immunosuppression withdrawal or whether these responses are the result of a modified graft-host is currently difficult to answer. Our data raise a more important question of whether tolerant recipients are donor-specific unresponsive or they could be somewhat immune-deficient. Clinically, most of the tolerant recipients maintain good graft function in the absence of immunosuppression, but no evidence of increased infections or cancer have been described for this population. An estimated 10-year patient survival after the establishment of operational tolerance of 90% (95% CI: 75–96), has recently been described27. Clearly, the putative immune-defect allows them to maintain good graft function and not succumb to other immune-pathologies, but currently, we do not have any evidence to strongly discern between donor-specific tolerance or immune-deficient responses.
In summary, we have provided novel evidence that an incomplete Th17 pathway integrity could contribute to human transplantation tolerance; whether this implies an immune-deficient state or not is now open for debate.
Supplementary Material
Funding
EN-L was funded by a scholarship from CONICYT Bicentennial Becas-Chile, Chile. The authors acknowledge financial support from the Medical Research Council (MRC) (grants G0801537/ID: 88245 and MRC Centre for Transplantation, – MRC grant no. MR/J006742/1) and Guy’s and St Thomas’ Charity (grants R080530 and R090782). The research was funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy's and St Thomas' NHS Foundation Trust and King's College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. GL, and MPH-F have received funding from the European Union, Seventh Framework Programme [FP7/2007–2013], under grant agreement no HEALTH-F5– 2010–260687: The ONE Study. SC, PM and MPHF received funding from FP7-HEALTH-2012-INNOVATION-1 project number 305147: BIO-DrIM. GAMBIT Consortium collaborators provided patient samples and detailed clinical information. We would like to thank all GAMBIT patients and healthy volunteers for their participation in the project.
Abbreviations
- ANOVA
Analysis of variance
- Aza
Azathioprine
- BCR
B cell receptor
- CD
Cluster of differentiation
- CNI
Calcineurin inhibitor
- DSA
Donor-specific antibodies
- ERK1/2
Extracellular Signal-Regulated Kinases 1 and 2
- GAMBIT
Genetic Analysis & Monitoring of Biomarker of Immunological Tolerance
- HRP
Horseradish peroxidase
- LPS
Lipopolysaccharide
- MEK
Mitogen-Activated Protein Kinase Kinase
- MMF
Mycophenolate mofetil
- PBMC
Peripheral blood mononuclear cell
- RORC
RAR-related orphan receptor C
- RM
Repeated measurements
- TCR
T cell receptor
Footnotes
Disclosure
The authors declare no conflicts of interest.
References
- 1.Turka LA, Lechler RI. Towards the identification of biomarkers of transplantation tolerance. Nat Rev Immunol. 2009;9(7):521–526. doi: 10.1038/nri2568. [DOI] [PubMed] [Google Scholar]
- 2.Lechler RI, Sykes M, Thomson AW, Turka LA. Organ transplantation--how much of the promise has been realized? Nat Med. 2005;11(6):605–613. doi: 10.1038/nm1251. [DOI] [PubMed] [Google Scholar]
- 3.Orlando G, Hematti P, Stratta RJ, et al. Clinical operational tolerance after renal transplantation: current status and future challenges. Ann Surg. 2010;252(6):915–928. doi: 10.1097/SLA.0b013e3181f3efb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sagoo P, Perucha E, Sawitzki B, et al. Development of a cross-platform biomarker signature to detect renal transplant tolerance in humans. J Clin Invest. 2010;120(6):1848–1861. doi: 10.1172/JCI39922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newell KA, Asare A, Kirk AD, et al. Identification of a B cell signature associated with renal transplant tolerance in humans. J Clin Invest. 2010;120(6):1836–1847. doi: 10.1172/JCI39933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva HM, Takenaka MCS, Moraes-Vieira PMM, et al. Preserving the B-cell compartment favors operational tolerance in human renal transplantation. Mol Med. 2012;18:733–743. doi: 10.2119/molmed.2011.00281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pallier A, Hillion S, Danger R, et al. Patients with drug-free long-term graft function display increased numbers of peripheral B cells with a memory and inhibitory phenotype. Kidney International. 2010;78(5):503–513. doi: 10.1038/ki.2010.162. [DOI] [PubMed] [Google Scholar]
- 8.Louis S, Braudeau C, Giral M, et al. Contrasting CD25hiCD4+T cells/FOXP3 patterns in chronic rejection and operational drug-free tolerance. Transplantation. 2006;81(3):398–407. doi: 10.1097/01.tp.0000203166.44968.86. [DOI] [PubMed] [Google Scholar]
- 9.Brouard S, Mansfield E, Braud C, et al. Identification of a peripheral blood transcriptional biomarker panel associated with operational renal allograft tolerance. Proc Natl Acad Sci USA. 2007;104(39):15448–15453. doi: 10.1073/pnas.0705834104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ballet C, Roussey-Kesler G, Aubin JT, et al. Humoral and cellular responses to influenza vaccination in human recipients naturally tolerant to a kidney allograft. Am J Transplant. 2006;6(11):2796–2801. doi: 10.1111/j.1600-6143.2006.01533.x. [DOI] [PubMed] [Google Scholar]
- 11.Nova-Lamperti E, Chana P, Mobillo P, et al. Increased CD40 ligation and reduced BCR signalling leads to higher IL-10 production in B cells from tolerant kidney transplant patients. Transplantation. 2017;101(3):541–547. doi: 10.1097/TP.0000000000001341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nova-Lamperti E, Fanelli G, Becker PD, et al. IL-10-produced by human transitional B-cells down-regulates CD86 expression on B-cells leading to inhibition of CD4+T-cell responses. Sci Rep. 2016;6 doi: 10.1038/srep20044. 20044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haas M, Sis B, Racusen LC, et al. Banff 2013 meeting report: inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. 2014;14(2):272–283. doi: 10.1111/ajt.12590. [DOI] [PubMed] [Google Scholar]
- 14.Rebollo-Mesa I, Nova-Lamperti E, Mobillo P, et al. Biomarkers of tolerance in kidney transplantation: are we predicting tolerance or response to immunosuppressive treatment? Am J Transplant. 2016;16(12):3443–3457. doi: 10.1111/ajt.13932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Z, O’Shea JJ. Regulation of IL-17 production in human lymphocytes. Cytokine. 2008;41(2):71–78. doi: 10.1016/j.cyto.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sallusto F, Lenig D, Mackay CR, Lanzavecchia A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J Exp Med. 1998;187(6):875–883. doi: 10.1084/jem.187.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cosmi L, De Palma R, Santarlasci V, et al. Human interleukin 17-producing cells originate from a CD161+CD4+ T cell precursor. J Exp Med. 2008;205(8):1903–1916. doi: 10.1084/jem.20080397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng Y, Sun L, Jiang T, Zhang D, He D, Nie H. TNFα promotes Th17 cell differentiation through IL-6 and IL-1β produced by monocytes in rheumatoid arthritis. J Immunol Res. 2014;2014 doi: 10.1155/2014/385352. 385352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11(11):762–774. doi: 10.1038/nri3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dieleman LA, Beagley KW, Elson CO. The effect of immunosuppressive agents on monocyte generation and cytokine expression. Inflamm Bowel Dis. 1995;1(4):266–275. doi: 10.1097/00054725-199512000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Sekerkova A, Krepsova E, Brabcova E, et al. CD14+CD16+ and CD14+CD163+ monocyte subpopulations in kidney allograft transplantation. BMC Immunol. 2014;15(1):4. doi: 10.1186/1471-2172-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mele F, Basso C, Leoni C, et al. ERK phosphorylation and miR-181a expression modulate activation of human memory TH17 cells. Nature Communications. 2015;6:6431. doi: 10.1038/ncomms7431. [DOI] [PubMed] [Google Scholar]
- 23.Deteix C, Attuil-Audenis V, Duthey A, et al. Intragraft Th17 infiltrate promotes lymphoid neogenesis and hastens clinical chronic rejection. J Immunol. 2010;184(9):5344–5351. doi: 10.4049/jimmunol.0902999. [DOI] [PubMed] [Google Scholar]
- 24.Chung BH, Oh HJ, Piao SG, et al. Higher infiltration by Th17 cells compared with regulatory T cells is associated with severe acute T-cell-mediated graft rejection. Exp Mol Med. 2011;43(11):630–637. doi: 10.3858/emm.2011.43.11.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung BH, Kim K-W, Kim B-M, et al. Dysregulation of Th17 cells during the early post-transplant period in patients under calcineurin inhibitor based immunosuppression. PLoS ONE. 2012;7(7):e42011. doi: 10.1371/journal.pone.0042011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cepika AM, Bendelja K, Vergles JM, Malenica B, Kapitanovic S, Gagro A. Monocyte response to LPS after exposure to corticosteroids and chloroquine with implications for systemic lupus erythematosus. Scand J Immunol. 2010;72(5):434–443. doi: 10.1111/j.1365-3083.2010.02450.x. [DOI] [PubMed] [Google Scholar]
- 27.Massart A, Pallier A, Pascual J, et al. The DESCARTES-Nantes survey of kidney transplant recipients displaying clinical operational tolerance identifies 35 new tolerant patients and 34 almost tolerant patients. Nephrol Dial Transplant. 2016;31(6):1002–1013. doi: 10.1093/ndt/gfv437. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.