Abstract
Rationale:
Spinal epidural abscess is an uncommon complication in clinical practice. If the abscess is large enough, the patient will rapidly develop neurologic signs of spinal injury, and urgent neurosurgical intervention may be required.
Patient concerns:
Rapid and correct diagnosis and treatment is important for spinal epidural abscess complication.
Diagnoses:
This report describes a cervical epidural abscess (CEA) caused by epidural analgesia, wherein the patient was punctured twice. A CEA was suspected based on the patient's significant neck pain and elevated white blood cell and neutrophil counts. A CEA from C6 to T8 was confirmed by magnetic resonance imaging scan.
Interventions:
The patient was treated with a combination of intravenous vancomycin and imipenem/cilastatin for more than 4 weeks.
Outcomes:
After more than 2 weeks of intensive antibiotic treatment, the epidural abscess gradually diminished in size, the white blood cell count, neutrophil count, hyperallergic C-reactive protein (CRP), and general CRP decreased, and the patient's neck and back pain resolved. After more than 4 weeks of anti-inflammation therapy, the epidural abscess was completely absorbed, and there was no relapse during the 3-month follow-up period.
Lessons:
Although an effective combination of intravenous antibiotics can cure an epidural abscess, caution is warranted when performing epidural steroid injections in immunocompromised patients.
Keywords: antibiotics, cervical epidural abscess, epidural analgesia
1. Introduction
A cervical epidural abscess (CEA) is a rare complication after epidural puncture and injection. Immunocompromised hosts, diabetes mellitus, and epidural catheter placement, are risk factors for epidural abscess.[1–6] The classical triad of a spinal epidural abscess (SEA) is pain, fever, and neurologic deficits.[7] Specifically, CEA seems to initially present with neck pain, neck stiffness, and/or fever.[8] The combination of neck pain or stiffness along with fever should raise the suspicion for CEA. Magnetic resonance imaging (MRI) is a useful diagnostic method to identify an epidural abscess and has contributed to the recent increase in SEA diagnoses. After diagnosis, urgent treatment, including early, effective, and adequate antibiotics as well as surgical decompression may be necessary to facilitate neurologic recovery.[8] In this article, we present a unique case of a patient who developed an epidural abscess after a cervical epidural puncture and injection. Once the diagnosis of CEA was made, antibiotics were promptly started, the patient was closely monitored, and the abscess was cured without surgical intervention.
2. Case presentation
A 65-year-old woman with 4 days of neck and shoulder pain that affected her sleep in addition to left arm numbness was seen in our Pain Management Department. Prior to her arrival, the patient had taken some medications (specific details were not clear), but the pain did not improve and became intolerable. The patient had a history of hypertension that had not been treated regularly, and her highest blood pressure was 180/100 mm Hg. All of the patient's examinations and treatments were approved by the ethics committee of 903 Hospital.
Upon arrival, the patient's vital signs showed hypertension with a blood pressure of 170/92 mm Hg; her other vital signs were normal. Physical examination showed a normal spine and extremities. There was slight tenderness over the cervical and the corresponding paravertebral area. The Spurling test, Jackson test, and left Eaton test were all positive. Sensation to pain and muscular tension of the extremities were normal bilaterally, and motor strength was grade 4/5 in the upper and lower extremities bilaterally. The biceps and triceps reflexes were normal bilaterally, and the Hoffmann sign was negative.
When she arrived, the patient underwent an MRI scan that showed multiple disc herniation at cervical 3/4, 4/5, and 5/6, and the epidural sac was compressed by the disc herniation (Fig. 1).
Figure 1.
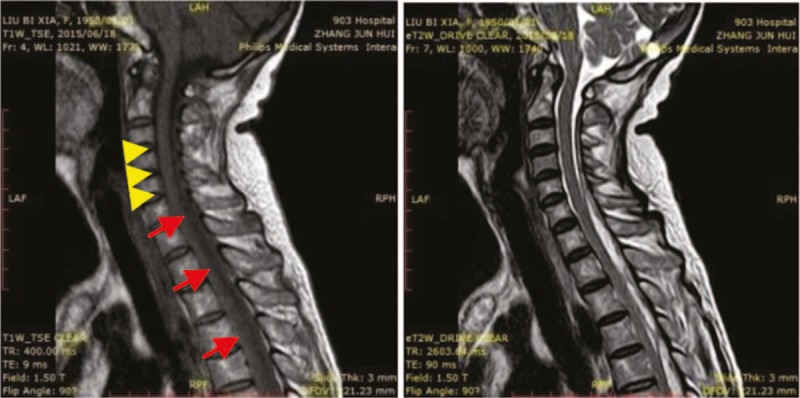
Magnetic resonance imaging shows multiple disc herniation of cervical 3/4, 4/5, and 5/6. The epidural sac is compressed by disc herniation (yellow arrow head). Epidural inflammation is seen with increased signal intensity (red arrow).
The initial diagnosis was cervical spondylosis and primary hypertension. It was decided to treat the patient conservatively with loxoprofen 60 mg twice a day, nifedipine sustained release tablets 10 mg daily, and an intravenous drip of 250 mL of 20% mannitol daily.
Two days later, the patient manifested clusters of tiny blisters along the C4 and C5 dermatome; the vesicular fluid was clear and there was no tenderness, suggesting the patient might have a concurrent acute herpes zoster infection. The antiviral drug famciclovir 0.25 g was started 3 times a day. The next day, the patient under went a nerve block procedure with an epidural puncture at the C7 to T1 space, and a catheter was inserted. The patient received an injection of 3 mL of the following mixture through the epidural catheter: 5 mL of 2% lidocaine, dexamethasone 10 mg, vitamin B1 100 mg, vitamin B6 100 mg, mecobalamine 1 mg, and 2 mL 0.9% saline, total volume 12 mL). The patient was observed for 10 minutes after the injection, and there were no signs of spinal anesthesia; the remaining volume of the mixture was subsequently injected and the catheter was removed.
The following day, the patient's pain had decreased and the clusters of blisters were somewhat reduced in size. A second epidural puncture and injection were performed, and the patient received the same nerve block mixture as before. The patient then showered and began to complain of body soreness, slight weakness, and a headache. Bilateral lung wheezing was heard on physical examination, and the patient was given 1 capsule of amoxicillin. However, the patient experienced severe pain of the shoulder, neck, and head accompanied by a low-grade fever (37.8°C), fatigue, and nighttime muscle aches. The patient also fell 1 time on the ward. Blood was tested due to these aggravated symptoms, and the white blood cell count was 24.27 × 109/L, neutrophil percentage was 92.41%, erythrocyte sedimentation rate (ESR) was 66 mm/h, hyperallergic C-reactive protein (CRP) was over 10 mg/L, and general CRP was 193.8 mg/L, suggesting an acute inflammation. The patient underwent a chest x-ray and cervical/thoracic MRI scan and was started on intravenous cefperazone/sulbactam 2 g twice a day and fosfomycin sodium. One day later the patient still complained of severe shoulder pain and headache; physical examination revealed C4 to T8 tenderness and neck stiffness; however, limb strength was normal. The MRI scan indicated epidural inflammation from C6 to T8 and an abscess formation (Fig. 2).
Figure 2.
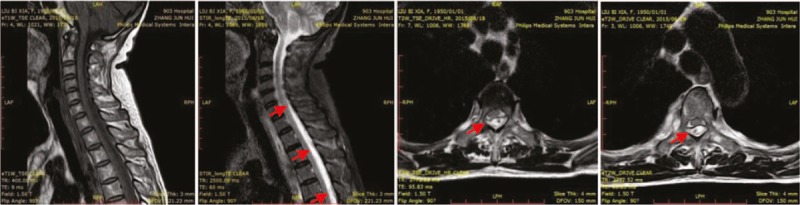
Magnetic resonance imaging shows cervical and thoracic epidural inflammation accompanying the abscess in the axial T2-weighted image. The epidural space in the C6 to T8 segment shows high signal gathering, and the right spinal cord has been compressed (red arrow).
The patient was moved to the intensive care unit to receive more intensive antibiotic treatment with vancomycin 1 g every 12 hours combined with imipenem/cilastatin sodium 1 g every 8 hours for anti-inflammation. Famciclovir was also changed to gentinovir 0.15 g twice a day for antiviral treatment. The patient's neck and back pain significantly improved after 4 days of anti-inflammation therapy, and the MRI scan showed significant absorption of the abscess (Fig. 3). This therapeutic regimen was continued for 17 days, during which the white blood cell count decreased to 5.11 × 109/L, the neutrophil percentage decreased to 57.3%, the ESR decreased to 76 mm/h, the hyperallergic CRP decreased to 4.71 mg/L, and the general CRP was less than 10 mg/L. The patient's neck and back pain disappeared, and the clusters of blisters scabbed over. On physical examination, there was slight tenderness to percussion but no pressing pain or neck stiffness. After 3 weeks of anti-inflammation therapy, the antibiotics were gradually weaned. After over a month of anti-inflammation therapy, the epidural abscess was completely absorbed and the patient was discharged from the hospital (Fig. 4).
Figure 3.
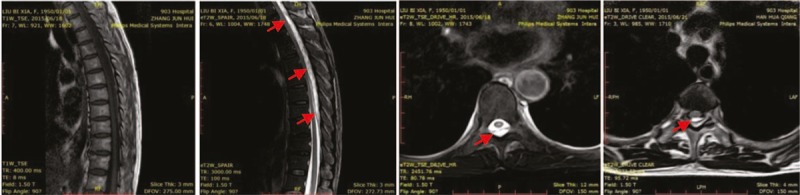
Magnetic resonance imaging shows partial resolution of the abscess. On axial T2-weighted imaging, the gathering signal intensity is reduced, and the area of inflammation has decreased compared to Fig. 2.
Figure 4.
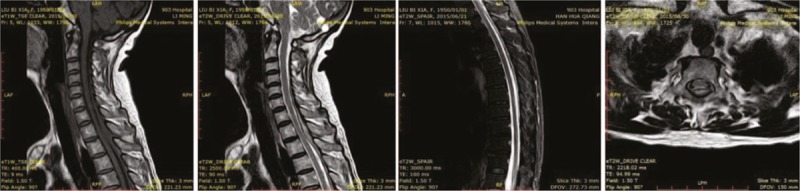
Magnetic resonance imaging shows that the epidural abscess is almost completely absorbed, and the epidural space now shows normal signal intensity (red arrow).
3. Discussion
An epidural abscess is a life-threatening infection with a high risk of disability and mortality. If the patient in this case had not been diagnosed and treated promptly, the patient may have developed permanent complications such as paraplegia or even death.[9] Therefore, rapid identification and treatment of an epidural abscess will yield the best outcomes.[10]
The most common symptoms and signs reported with an SEA are neck and back pain, fever, and neurologic deficits.[7,8,11] In this case, the patient showed some of the signs and symptoms, such as neck pain, neck stiffness, and a low-grade fever, which raised the suspicion for an epidural abscess. The inflammatory markers, such as the ESR, CRP, and white blood cell count, supported the diagnosis of an epidural abscess.[8] An MRI scan can provide a definitive diagnosis once an SEA is suspected, and MRI enhancement has a sensitivity over 90%.[7,12] In this case, the MRI scan provided direct evidence of an epidural abscess between C6 and T8, which guided the treatment strategy.
An MRI is able to differentiate between SEAs and other spinal lesions such as subdural abscesses and tumors. The classical description of an SEA on MRI is an iso- or hyperintense collection in the epidural space on a T1-weighted image that enhances with gadolinium contrast and a non-homogeneous and hyperintense signal on a T2-weighted image.[8,11,13] These classical imaging signs of an epidural abscess were present in this case (Fig. 2).
Anti-inflammation by antibiotics is an important non-surgical treatment for an epidural abscess, especially in the early stages before any neurologic deficit occurs. Chan and Oh[11] reported that there is no guarantee that medical treatment will succeed. If antibiotic therapy alone is considered for aneurologically intact patient, frequent neurologic examinations, blood testing (such as ESR, CRP, and white blood cell count), and MRI examinations are required to monitor the development of the disease. Once the patient shows any neurologic deficit, surgical decompression should be considered.[8] Although the period of antibiotic therapy for epidural abscess is still being debated, it is preferable to continue treatment for at least 4 weeks, because studies have shown a 25% rate of relapse in patients who were treated for less than 4 weeks.[11,14,15] In the present case, the patient received antibiotic therapy for more than 1 month and showed no evidence of relapse during the 3-month follow-up period.
The patient in this case had a prodrome of herpes zoster infection of the shoulder and posterior neck pain with numbness followed by clusters of tiny blisters along the C4 to C5 dermatome; this suggests that the patient may have been immunocompromised, which could explain the development of an epidural abscess. There were other iatrogenic mechanisms that could significantly increase the risk of an epidural abscess that we cannot exclude, including repeated punctures, epidural catheter placement, and injection of drugs,[16] which can disturb the local microenvironment and result in the spread of pathogens into the epidural space. Based on the events in this case, it is suggested that repeated epidural punctures should be avoided in immunocompromised patients to decrease the risk of an epidural abscess.
4. Conclusions
In conclusion, an epidural abscess is a rare complication that requires rapid diagnosis and treatment. An MRI scan has a high sensitivity and specificity when an epidural abscess is suspected, and prompt diagnosis and treatment are key to curing this disease.
Footnotes
Abbreviations: CEA = cervical epidural abscess, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, MRI = magnetic resonance imaging, SEA = spinal epidural abscess.
The authors report no conflicts of interest.
References
- [1].Tang HJ, Lin HJ, Liu YC, et al. Spinal epidural abscess—experience with 46 patients and evaluation of prognostic factors. J Infect 2002;45:76–81. [DOI] [PubMed] [Google Scholar]
- [2].Huang RC, Shapiro GS, Lim M, et al. Cervical epidural abscess after epidural steroid injection. Spine 2004;29:E7–9. [DOI] [PubMed] [Google Scholar]
- [3].Alcock E, Regaard A, Browne J. Facet joint injection: a rare form cause of epidural abscess formation. Pain 2003;103:209–10. [DOI] [PubMed] [Google Scholar]
- [4].Philipneri M, Al-Aly Z, Amin K, et al. Routine replacement of tunneled, cuffed, hemodialysis catheters eliminates paraspinal/vertebral infections in patients with catheter-associated bacteremia. Am J Nephrol 2003;23:202–7. [DOI] [PubMed] [Google Scholar]
- [5].Bang MS, Lim SH. Paraplegia caused by spinal infection after acupuncture. Spinal Cord 2006;44:258–9. [DOI] [PubMed] [Google Scholar]
- [6].Sillevis Smitt P, Tsafka A, van den Bent M, et al. Spinal epidural abscess complicating chronic epidural analgesia in 11 cancer patients: clinical findings and magnetic resonance imaging. J Neurol 1999;246:815–20. [DOI] [PubMed] [Google Scholar]
- [7].Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM 2008;101:1–2. [DOI] [PubMed] [Google Scholar]
- [8].Al-Hourani K, Al-Aref R, Mesfin A. Upper cervical epidural abscess in clinical practice: diagnosis and management. Global Spine J 2016;6:383–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Murata M, Yoshikawa K, Hiratsuka M, et al. A case of extensive sacral decubitus ulcer complicated by an epidural abscess. Plast Reconstr Surg Glob Open 2016;4:e790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ramos AD, Rolston JD, Gauger GE, et al. Spinal subdural abscess following laminectomy for symptomatic stenosis: a report of 2 cases and review of the literature. Am J Case Rep 2016;17:476–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Chan JJ, Oh JJ. A rare case of multiple spinal epidural abscesses and cauda equina syndrome presenting to the emergency department following acupuncture. Int J Emerg Med 2016;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].An HS, Seldomridge JA. Spinal infections: diagnostic tests and imaging studies. Clin Orthop Relat Res 2006;444:27–33. [DOI] [PubMed] [Google Scholar]
- [13].Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 2002;137:586–97. [DOI] [PubMed] [Google Scholar]
- [14].Shweikeh F, Saeed K, Bukavina L, et al. An institutional series and contemporary review of bacterial spinal epidural abscess: current status and future directions. Neurosurg Focus 2014;37:1–1. [DOI] [PubMed] [Google Scholar]
- [15].Suppiah S, Meng Y, Fehlings MG, et al. How best to manage the spinal epidural abscess? A current systematic review. World Neurosurg 2016;93:20–8. [DOI] [PubMed] [Google Scholar]
- [16].Philipneri M, Al-Aly Z, Amin K, et al. Routine replacement of tunneled, cuffed, hemodialysis catheters eliminates paraspinal/vertebral infections in patients with catheter-associated bacteremia. Am J Nephrol 2003;23:202–7. [DOI] [PubMed] [Google Scholar]


