Abstract
Background
Depression and anxiety are common comorbidities in chronic pain including osteoarthritis patients undergoing total joint arthroplasty (TJA). What is not clear is whether psychiatric comorbidity precedes the manifestation of painful states or represents a reaction to living with chronic pain and associated functional impairment. The objective of this research was to explore whether decreases in depressive and anxiety symptoms after lower extremity total joint arthroplasty (TJA) would be due to postsurgical reductions in pain.
Methods
We conducted a secondary analysis of data from 1,448 TJA patients enrolled in the Analgesics Outcome Study. Patients completed measures of pain intensity, functional status, and depressive and anxiety symptoms preoperatively and at 3 and 6 months postoperatively. Data were analyzed using a structural equation modeling approach.
Results
We found that improvement in pain and physical function from baseline to 6 months postoperatively was associated with improvement in depression and anxiety symptoms. We also found that a change in overall body pain at 3 months after surgery significantly mediated changes in both the depression and anxiety scores at 6 months after surgery even when controlling for age, sex, baseline body pain, education, opioid use and type of surgery.
Conclusions
Presurgical affective symptoms not only have an effect on change in postsurgical pain, whereby lower preoperative scores on depression and anxiety were associated with lower postsurgical pain, but also postsurgical decreases in pain were associated with lower levels of depression and anxiety after surgery. Taking these points into consideration may prove useful in working towards better outcomes for TJA.
Keywords: Pain, Arthroplasty, Depression, Anxiety, Osteoarthritis
INTRODUCTION
Psychiatric comorbidities are commonly observed in most chronic pain states1–4 including patients with osteoarthritis requiring total joint arthroplasty (TJA). Significant symptoms of depression and anxiety have been reported in as many as 20% to 30% of patients in advance of undergoing TJA.5, 6 What is not clear is whether these psychiatric symptoms are antecedent (part of the patient’s long-term history and preceding the painful state) or a reaction to living with chronic pain and the associated loss of functioning, as well as other related psychosocial complications.7 Either way, depression and anxiety are important factors to consider and address in that their presence before surgery is predictive of poor postsurgical outcomes including postoperative pain severity, persistent postsurgical pain and increased opioid consumption.8–10
There are complicated, but important relationships between pain and affect in this and other surgical populations. Historically, baseline measures of depression and anxiety have been used as predictors of poor postoperative outcomes, but more recent work suggests that many surgical patients have improvements in mood once pain has improved and functioning has been restored as a result of surgery.11 For example, after successful outcomes in bariatric surgery, pelvic organ prolapse correction, lumbar spinal surgery, and coronary artery bypass graft (CABG), significant reductions in depression scores and improved quality of life have been noted.11–14 Similarly, one recent small study of 40 patients undergoing TJA found that anxiety and depression improved after total knee arthroplasty (TKA).15 These studies are suggestive, but by no means provide conclusive evidence for answering the question, “Is psychological distress cause or effect in osteoarthritis pain populations?”
The objective of this study was to explore whether depression and anxiety improve as pain and functioning improve post-TJA. Most studies to date exploring this question have been limited by their cross-sectional designs and/or small sample sizes. Thus, data from a large ongoing prospective, observational cohort study in the perioperative setting known as the Analgesic Outcomes Study (AOS) are reported. Herein, we hypothesized that individuals reporting significant postsurgical reductions in pain and improvement in physical functioning after TKA and THA would be more likely to also experience decreases in depressive and anxiety symptoms. Further, we hypothesized that higher baseline depression and anxiety scores would be associated with decreased improvements in pain following surgery. Lastly, we hypothesized that changes in pain severity following surgery would mediate the relationship between depression and anxiety at baseline and changes observed at 6 months post-TJA.
METHODS
Institutional Review Board (University of Michigan, Ann Arbor, Michigan) approval was obtained. This is a secondary analysis of data from the AOS.16–19 The following study aims to conform to guidelines set forth in the Strengthening the Reporting of Observation Studies in Epidemiology Statement.20 Study participants consist of men and women at least 18 years of age who were scheduled for a primary, unilateral TKA or THA at the University of Michigan Health System from March 2010 to November 2015. For the AOS parent study, patients were approached either in the preoperative waiting area or at a pre-operative lower-extremity TJA workshop. Written, informed consent was obtained from all patients indicating a willingness to participate in the AOS. Excluded from this study were: prisoners, those unable to give consent, non-English speakers, and patients who were undergoing bilateral or revision TJA. On the day of surgery in the preoperative area, participants completed validated self-report measures for the assessment of pain severity, functional status, and depressive and anxiety symptoms. Follow-up assessments were conducted at 3 and 6 months after surgery using the same questionnaires by phone interview.
Measures
Pain Intensity: Pain intensity was measured by the four questions about pain intensity (worst, least, average, and right now) from the Brief Pain Inventory (BPI). Recorded values from the BPI (numeric rating scale, where 0=no pain, 10=pain as bad as you can imagine) were used to create a composite score (0–10) for pain intensity.21
Functional Status: Functional status was assessed using the Western Ontario and McMaster Universities Arthritis Index (WOMAC) scale. The WOMAC is a 24-item measure with subscales that assess pain, stiffness and physical function. Seventeen items comprise the functioning subscale and address ability to rise from a sitting position, stand, bend, walk, get in and out of a car, shop, put on and take off socks, rise from bed, lie in bed, get in and out of the bath, sit, get on and off the toilet, and engage in heavy and light household duties. Scores range from 0–68 with higher scores indicating worse function.22
Depressive and Anxiety Symptoms: The Hospital Anxiety and Depression Scale (HADS) was used to assess depressive and anxiety symptoms. The HADS consists of 14 questions in total, with 7-question subscales for both anxiety and depression. Each item is scored from 0–3 and subscale scores range from 0–21, where higher scores indicate more depressive and anxiety symptoms. Likely cases of depression and anxiety are indicated by scores ≥ 11.23
Opioid Use: The use of opioid pain medication was assessed with a self-report item at each time point.
Pain severity scores were collected at baseline, at 3 months postoperatively, and at 6 months postoperatively. WOMAC function scores and HADS depression and anxiety scores were collected at baseline and 6 months postoperatively. For examining correlations between change in affect and change in pain and function from baseline to 6 months, change scores were calculated such that a negative variable indicates improvement in pain or affect from baseline to 6 months. For the mediation models examining change in pain severity as a mediator of the relationship between affect at baseline and 6 months, pain severity change scores were calculated such that a negative variable indicates improvement in the pain from baseline to 3 months postoperatively. Per the guidelines for using the HADS assessments, if a participant did not answer one of the questions in either the depression or anxiety subset in HADS, then the numerical average of the answered questions was manually taken and imputed for the missing data point.
Statistical Analysis
All patient information and data were entered into the AOS APOLO database24 and analyzed using STATA version 13.1 (Stata Corp., 2013). Baseline univariate statistics were computed to describe the overall sample. Between-subjects t-tests and chi-square tests were conducted to assess differences in pain, depression, and anxiety between TKA and THA patients. Two within-subjects t-tests were conducted to assess change in depression and anxiety scores from baseline to 6 months. To assess the relationship between change in affect and change in pain and function from baseline to 6 months, partial correlations were conducted, controlling for age, sex, type of surgery, and baseline affect, as well as pain or function scores. To further assess the potential relationship between changes in affect and changes in postsurgical pain severity, two separate mediation models were conducted with a path analysis model utilizing the structural equation modeling package in Stata 13.1. In the first model, change in pain severity from baseline to 3 months was included as a mediator of the relationship between baseline depression scores and 6-month postoperative depression scores. In the second model, change in pain severity from baseline to 3 months was included as a mediator of the relationship between baseline anxiety scores and 6-month postoperative anxiety scores. In each model, age, sex, type of surgery (TKA vs THA), baseline pain severity scores, education, and opioid use at day of surgery and 6 months were included as predictors of change in pain and 6-month depression and anxiety scores, respectively. Full information maximum likelihood estimation was used to handle missing data in these models. This approach utilizes all available data points and has been shown to be a less biased approach than using complete case only.25 Bootstrapped standard errors with 50 replications were used to calculate the indirect (mediated) effects in the path analysis models.
RESULTS
Baseline demographics, as well as baseline and postoperative pain and affect scores for the 1,448 participants are presented in Table 1. The majority of patients were female (53.04%), Caucasian (90.12%), married (66.02%), college graduates (51.80%), and underwent THA (59.53%). Using the standard cut point for HADS, we found that the instances of baseline depression were not significantly different for TKA (6.59%) and THA (8.33%) patients (p = 0.255). There were also no significant differences in instances of baseline anxiety for TKA (11.42%) and THA (10.39%) patients (P = 0.566). THA patients reported significantly higher overall body pain scores than TKA patients at baseline (5.0 vs 4.5), t[1402] = 4.44, P < 0.001). However, TKA patients reported significantly higher overall body pain scores than THA patients at 6 months postoperative (2.1 vs 1.7, t[898] = 3.59, P < 0.001). Only one patient reported a surgical complication that occurred between day of surgery and one-month follow-up (ie, an emergency room visit for a potential blood clot).
Table 1.
Demographic and outcomes data for entire sample of 1,448 patients
| N (%) | |
|---|---|
| Agea | 62.18 (12.01%) |
| Female | 768 (53.04%) |
| Knee surgery | 586 (40.47%) |
| Caucasian | 1,305 (90.12%) |
| College graduate | 750 (51.80%) |
| Married | 956 (66.02%) |
| HADS Depression baseline | 4.81 (3.44) |
| HADS Depression 6 months | 3.06 (3.25) |
| HADS Anxiety baseline | 5.4 (3.83) |
| HADS Anxiety 6 months | 3.87 (3.33) |
| BPI Overall Body Pain Severity baseline | 4.80 (2.06) |
| BPI Overall Body Pain Severity 3 months | 2.09 (1.91) |
. Means and standard deviations reported for continuous variables
Patients who completed the 6 month survey were older (63 years vs 60 years, P < 0.001), had lower HADS depression scores at day of surgery (4.6 vs 5.3, P = 0.001), had lower HADS anxiety scores at day of surgery (5.2 vs 5.9, P = 0.002), and had lower overall body pain at day of surgery (4.6 vs 5.2, P < 0.001) than patients who did not complete the 6 month survey. No significant differences between depression or anxiety scores, or instances of depression or anxiety were found at 6 months postoperative between TKA and THA patients. Across the entire sample, there were significant reductions in both depression scores (t[777] = 15.10, P < 0.001) and anxiety scores (t[776] = 12.23, P < 0.001) from baseline to 6 months.
Correlations between changes in affect and changes in pain and function
Improvement in depression from baseline to 6 months was significantly correlated with improvement in pain severity from baseline to 6 months controlling for age, sex, type of surgery, and baseline pain severity (partial r = 0.24, P < 0.001). Similarly, improvement in anxiety from baseline to 6 months was significantly correlated with improvement in pain severity from baseline to 6 months controlling for age, sex, type of surgery, and baseline pain severity (partial r = 0.18, P < 0.001). Improvement in depression from baseline to 6 months was also significantly correlated with improvement in physical function from baseline to 6 months controlling for age, sex, type of surgery, and baseline WOMAC function scores (partial r = 0.25, P < 0.001). Further, improvement in anxiety from baseline to 6 months was also associated with improvement in physical function from baseline to 6 months controlling for age, sex, type of surgery, and baseline WOMAC function scores (partial r = 0.10, P = 0.009).
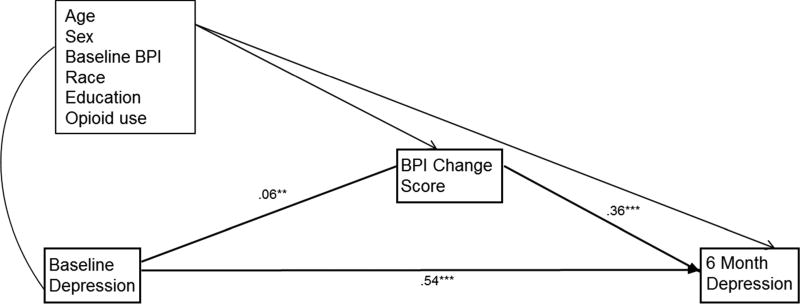
Mediation model 1: Depression scores were significantly mediated by changes in overall body pain
Unstandardized coefficients are presented in Figure 1. The relationship between depression at baseline and depression at 6 months was mediated by change in overall body pain from baseline to 3 months, after controlling for age, sex, baseline body pain, type of surgery, race, education, and opioid use at day of surgery and 6 months (indirect effect = 0.02, P = 0.003). As seen in Figure 1, the path from HADS depression scores at baseline to change in pain from baseline to 3 months was positive, such that lower scores on HADS depression were associated with greater decreases in overall body pain from baseline to 3 months (P = 0.002). The path from change in overall body pain to HADS depression scores at 6 months was also positive, such that greater decreases in overall body pain were associated with lower HADS depression scores at 6 months (P < 0.001).
Figure 1.
The relationship between day of surgery depression score and 6-month postoperative depression score is mediated by change in overall body pain from day of surgery to 3 months postoperative.
Note: *** P < 0.001, ** P < 0.01, * P < 0.05. Unstandardized path coefficients are presented. Age, sex, overall body pain score at baseline, race, education, and opioid use were included as covariates of both BPI change score and depression score at 6 months. Correlations were allowed among all exogenous variables. The indirect effect of baseline depression on depression at 6 months through BPI change score was statistically significant (indirect effect = 0.02, P = 0.003).
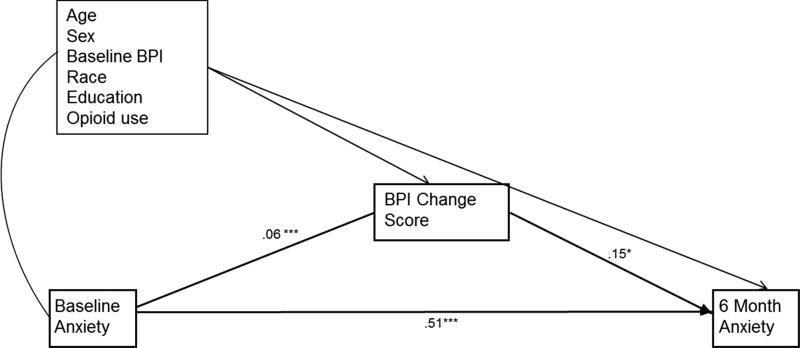
Mediation model 2: Anxiety scores were also significantly mediated by changes in overall body pain
Unstandardized coefficients are presented in Figure 2. The findings in regard to anxiety mediation analysis were similar to those for depression. We found that the relationship between anxiety at baseline and anxiety at 6 months was also mediated by change in overall body pain from baseline to 3 months even while controlling for age, sex, baseline body pain, type of surgery, race, education, and opioid use at day of surgery and 6 months (indirect effect = 0.01, P = 0.038). As seen in Figure 2, the path from HADS anxiety scores at baseline to change in pain from baseline to 3 months was positive, showing that lower scores on HADS anxiety were associated with greater decreases in overall body pain from baseline to 3 months (P < 0.001). The path from change in overall body pain to HADS anxiety scores at 6 months was also positive, such that greater decreases in overall body pain were associated with lower HADS anxiety scores at 6 months (P = 0.011).
Figure 2.
The relationship between day of surgery anxiety score and 6-month postoperative anxiety score is mediated by change in overall body pain from day of surgery to 3 months postoperative.
Note: *** P < 0.001, ** P < 0.01, * P < .05. Unstandardized path coefficients are presented. Age, sex, overall body pain score at baseline, race, education and opioid use were included as covariates of both BPI change score and anxiety score at 6 months. Correlations were allowed among all exogenous variables. The indirect effect of baseline anxiety on anxiety at 6 months through BPI change score was statistically significant (indirect effect = 0.01, P = 0.038).
DISCUSSION
In this secondary analysis of a large, prospective cohort study of TJA patients, we found significant improvement in postoperative depressive and anxiety symptoms after surgery; moreover, such improvement was more often seen in individuals who experienced a reduction in pain severity and improvement in physical function after surgery. To explore the temporal role of change in pain in negative affective symptom improvement, two mediation models were conducted - one for depression and one for anxiety. We found that a change in overall body pain at 3 months after surgery significantly mediated changes in both depression (Fig. 1) and anxiety (Fig. 2) scores 6 months after surgery even when controlling for age, sex, education, baseline body pain, opioid use and type of surgery, highlighting the unique relationship between pain and affect. Not only does affect appear to have an effect on change in pain postsurgically, whereby lower preoperative scores on depression and anxiety were associated with lower overall body pain at 3 months postsurgery, but also that postsurgical decreases in pain were also associated with lower depression and anxiety scores at 6 months.
To the best of our knowledge, this study is the first to analyze the elements of a potential bi-directional relationship between changes in pain and affect over time in TJA patients using a prospective study design. Previous studies have looked at each piece separately, or have shown that both change together over time, but our study breaks down each piece of the causal chain. For example, Duivenvoorden and colleagues found a significant decrease in the prevalence of anxiety and depressive symptoms for both TKA and THA patients after surgery.5 In their prospective study of 149 hip and 133 knee patients, they found that a decrease in the prevalence of psychological symptoms accompanied a reduction in postsurgical pain and disability, and they suggested that anxiety and depressive symptoms had an influence on patient reported outcomes after TJA. Their study found a difference in depressive symptoms between hip and knee patients. A major strength of the present study is that it controls for several confounding factors including age, sex, race, level of education, type of surgery, opioid use, and baseline affect (anxiety and depression) and pain or physical function scores.
In another study, Blackburn et al raised the question of whether psychological distress in TKA patients is antecedent or the result of living with persistent knee pain.15 They found that overall depression and anxiety scores, as well as Oxford Knee Scores26 (another index of knee pain and function following TKA) significantly improved postoperatively. They also found that more severe preoperative anxiety and depression were associated with higher knee disability, and that postoperatively, a reduction in anxiety and depression was associated with a reduction in knee disability at both 3 and 6 months postsurgery. The same study suggested that preoperative knee pain was a significant, but not the only contributor to reductions in both anxiety and depression.
Whereas studies have shown associations between preoperative negative affect and poorer postoperative outcomes, clinicians may struggle as to the clinical applicability of the findings. Few would argue with the decision to avoid or postpone surgery in patients with severe, untreated anxiety and depression, but many patients have more moderate symptoms or already receive treatment for psychological distress. Despite the general understanding that patients with even moderate levels of preoperative negative affect may do more poorly, surgeons may not routinely use this information to inform their clinical decision-making.
While negative affect can be predictive of postsurgical outcomes, there is likely more to the story. Wylde et al showed that depression was independently associated with poorer pain outcomes after TKA and THA; however, the effect size for depression (adjusted odds ratio 1.27–1.29) was far smaller when compared to the presence of pain in other locations (adjusted odds ratio for pain in 5 or more areas = 11.78–14.80).27 In an earlier study from our surgery cohort, we demonstrated that the 2011 Fibromyalgia Survey Criteria were independently predictive of poorer long-term outcomes for knee/hip change in pain, change in overall body pain and patient global impression of change.16 Depression, anxiety and catastrophizing were all included in the multivariate models, and none were independently predictive. As such, it may be more appropriate to consider changes in affective distress as an important secondary benefit from the improvement in pain often accompanying TJA, rather than as a strong predictor of poorer outcomes.
The major strengths of our study relative to those in the past include the robust sample size and prospective design that limit our potential for bias and confounding factors. In the present study, data were collected via self-reported questionnaires at three standardized time points. Pain severity scores were collected at 3 months postsurgery, and depression and anxiety, as well as physical function scores were collected at 6 months postsurgery. These relationships could be limited by the frequency and timing of data points taken. It is unclear whether the same relationship would exist at more frequent time points, or time points extending further out than 6 months postsurgery. We did not collect depression or anxiety scores at 3 months, and it is unclear whether the inclusion of these affect measures at 3 months would have substantially changed the mediation model. Additionally, the study is limited by the use of self-report questionnaires as such data can be subject to recall and social desirability biases. Most of the patients in our study were Caucasian (90.12%) and a majority (51.8%) was college graduates. It is possible that these demographic majorities could limit the generalization of our findings to all patients undergoing TJA. Further research is warranted to address the limitations of our study. Areas to be explored would include adding more objective measures of functioning and implementing structured interviews to assess the presence of depression and anxiety. Data could also be collected at more frequent time points and follow-up assessments could be extended. In addition, patients lost to follow up had significantly higher depression and anxiety scores, which could have biased our findings. Lastly, a more diverse patient population should be sought to explore whether or not the relationships found in this study generalize more broadly.
In conclusion, we found that improvement in depression and anxiety symptoms after surgery were associated with improvement in pain severity and physical function. We also showed that change in pain severity mediated psychiatric comorbidity, suggesting that change in pain is both caused by and effected by negative affective symptoms. Taking these points into consideration may prove useful in working towards the improvement of outcomes for patients undergoing total joint arthroplasty.
Acknowledgments
Sources of Funding
Funding: The study was funded by R01AR060392 (Co-PI Brummett and Clauw) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (National Institutes of Health, Bethesda, MD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Arthritis and Musculoskeletal and Skin Diseases or the National Institutes of Health. Additional funding was provided by the Department of Anesthesiology, University of Michigan. The study sponsors had no role in the design, conduct, collection, analysis, or interpretation of this study, nor the preparation, review, or approval of the manuscript.
Dr. Hassett has received research funding from Bristol-Myers Squibb (Princeton, New Jersey, USA) and is a consultant for Happify, Inc. (New York, New York, USA). Dr. Hassett also receives salary support from the American College of Rheumatology as the President of the Association of Rheumatology Health Professionals. Dr. Clauw is a consultant for Pfizer, Inc. (New York, New York, USA); Johnson and Johnson (New Brunswick, New Jersey, USA); Forest Pharmaceuticals (New York, New York, USA); Merck (Whitehouse Station, New Jersey, USA); Nuvo Research, Inc. (Mississauga, Ontario, Canada); Eli Lilly, Inc. (Indianapolis, Indiana, USA); Grunenthal Pharma Ltd. (Dublin, Ireland); and Jazz Pharmaceuticals, Inc. (Palo Alto, California, USA). Dr. Clauw also receives research funding from Merck Pharmaceuticals, Cerephex, and Forest Pharmaceuticals. Dr. Brummett receives research funding from Neuros Medical Inc. (Willoughby Hills, Ohio).
Footnotes
Conflicts of Interest
Potential Conflicts of Interest: There are otherwise no relevant disclosures.
References
- 1.Hassett AL, Radvanski DC, Buyske S, Savage SV, Sigal LH. Psychiatric comorbidity and other psychological factors in patients with "chronic lyme disease". Am J Med. 2009;122:843–850. doi: 10.1016/j.amjmed.2009.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70:890–897. doi: 10.1097/PSY.0b013e318185c510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnold LM, Hudson JI, Keck PE, Auchenbach MB, Javaras KN, Hess EV. Comorbidity of fibromyalgia and psychiatric disorders. J Clin Psychiatry. 2006;67:1219–1225. doi: 10.4088/jcp.v67n0807. [DOI] [PubMed] [Google Scholar]
- 4.Hooten WM. Chronic pain and mental health disorders: Shared neural mechanisms, epidemiology, and treatment. Mayo Clin Proc. 2016;91:955–970. doi: 10.1016/j.mayocp.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 5.Duivenvoorden T, Vissers MM, Verhaar JA, et al. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: A prospective multicentre study. Osteoarthritis Cartilage. 2013;21:1834–1840. doi: 10.1016/j.joca.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Riddle DL, Wade JB, Jiranek WA. Major depression, generalized anxiety disorder, and panic disorder in patients scheduled for knee arthroplasty. J Arthroplasty. 2010;25:581–588. doi: 10.1016/j.arth.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: Antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kinjo S, Sands LP, Lim E, Paul S, Leung JM. Prediction of postoperative pain using path analysis in older patients. J Anesth. 2012;26:1–8. doi: 10.1007/s00540-011-1249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption a qualitative systematic review. Anesthesiology. 2009;111:657–677. doi: 10.1097/ALN.0b013e3181aae87a. [DOI] [PubMed] [Google Scholar]
- 10.Lungu E, Vendittoli PA, Desmeules F. Preoperative determinants of patient-reported pain and physical function levels following total knee arthroplasty: A systematic review. Open Orthop J. 2016;10:213–231. doi: 10.2174/1874325001610010213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ravven S, Bader C, Azar A, Rudolph JL. Depressive symptoms after cabg surgery: A meta-analysis. Harv Rev Psychiatry. 2013;21:59–69. doi: 10.1097/HRP.0b013e31828a3612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayden MJ, Dixon JB, Dixon ME, Shea TL, O'Brien PE. Characterization of the improvement in depressive symptoms following bariatric surgery. Obes Surg. 2011;21:328–335. doi: 10.1007/s11695-010-0215-y. [DOI] [PubMed] [Google Scholar]
- 13.Dhital R, Otsuka K, Poudel KC, Yasuoka J, Dangal G, Jimba M. Improved quality of life after surgery for pelvic organ prolapse in nepalese women. BMC Womens Health. 2013;13:22. doi: 10.1186/1472-6874-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farzanegan G, Alghasi M, Safari S, Ahmadi SA. Effects of lumbar discectomy on disability and depression in patients with chronic low back pain. Anesth Pain Med. 2011;1:20–24. doi: 10.5812/kowsar.22287523.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blackburn J, Qureshi A, Amirfeyz R, Bannister G. Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee. 2012;19:522–524. doi: 10.1016/j.knee.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Brummett CM, Urquhart AG, Hassett AL, et al. Characteristics of fibromyalgia independently predict poorer long-term analgesic outcomes following total knee and hip arthroplasty. Arthritis Rheumatol. 2015;67:1386–1394. doi: 10.1002/art.39051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janda AM, As-Sanie S, Rajala B, et al. Fibromyalgia survey criteria is associated with increased postoperative opioid consumption in women undergoing hysterectomy. Anesthesiology. 2015;122:1103–1111. doi: 10.1097/ALN.0000000000000637. [DOI] [PubMed] [Google Scholar]
- 18.Brummett CM, Janda AM, Schueller CM, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: A prospective, observational cohort study. Anesthesiology. 2013;119:1434–1443. doi: 10.1097/ALN.0b013e3182a8eb1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157:1259–1265. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (strobe) statement: Guidelines for reporting of observational studies. Internist. 2008;49:688–693. doi: 10.1007/s00108-008-2138-4. [DOI] [PubMed] [Google Scholar]
- 21.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the brief pain inventory for chronic nonmalignant pain. J Pain. 2004;5:133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Bellamy N. Womac osteoarthritis index user guide. Version V. Brisbane, Australia: 2002. [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 24.Hassett AL, Wasserman R, Goesling J, Rakovitis K, Shi B, Brummett CM. Longitudinal assessment of pain outcomes in the clinical setting: Development of the "apolo" electronic data capture system. Reg Anesth Pain Med. 2012;37:398–402. doi: 10.1097/AAP.0b013e3182524672. [DOI] [PubMed] [Google Scholar]
- 25.Enders CK, Bandalos D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [PubMed] [Google Scholar]
- 26.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–69. doi: 10.1302/0301-620x.80b1.7859. [DOI] [PubMed] [Google Scholar]
- 27.Wylde V, Hewlett S, Learmonth ID, Dieppe P. Persistent pain after joint replacement: Prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572. doi: 10.1016/j.pain.2010.11.023. [DOI] [PubMed] [Google Scholar]