Abstract
Purpose The aim of this study was to evaluate the efficacy and safety of intra-articular injection treatment with high molecular weight HA (Hyalubrix, 30 mg/2 mL, molecular weight > 1,500 kDa) in patients affected by moderate to severe glenohumeral osteoarthritis (OA).
Methods Seventy-eight patients, affected by shoulder OA grade II–IV were randomized in two groups. Patients included in case group were treated with three intra-articular injections of HA and a specific physiotherapy program, whereas patients included in the control group received the only physical therapy. The follow-up examination was 6 months for both groups. The evaluation of functional status of treated shoulder, range of motion, and pain was performed before treatment and at the final follow-up examination by means of the Constant score. The safety evaluation of the treatment was also performed recording any adverse events.
Results Statistical analysis revealed a significant difference ( p < 0.05) between the two groups in terms of pain reduction and improvement in the activities of daily living. In particular, case group subjects affected by grade III and IV OA had a significant improvement in the Constant score (18.2 ± 5.4 and 19.2 ± 5.9, respectively).
Conclusion This study showed that the combination of intra-articular injection of hyaluronic acid (Hyalubrix, 30 mg/2 mL) with physical therapy program was more effective in comparison with the only physical therapy in reducing pain in patients affected by glenohumeral OA.
Level of Evidence Level II, randomized controlled study.
Keywords: hyaluronic acid, injection, glenohumeral, osteoarthritis, shoulder
Introduction
Glenohumeral osteoarthritis (OA) is characterized by the appearance of typical degenerative changes in the cartilage, synovial membrane, synovial fluid, and subchondral bone. 1 OA is one of the main reasons of persistent shoulder pain and reduced range of motion (ROM) 2 3 and can compromise the activities of work and daily living leading to the development of depressive syndromes. 1 4 The treatment of this pathology can be conservative in patients affected by grade I–III OA or grade IV OA with contraindications to surgical treatment. The conservative approach generally includes intra-articular injections with corticosteroids, hyaluronic acid (HA), physical therapy, or the use of oral analgesics. 5 6 7 8 9 10 11 However, analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) are often associated with essential side effects. 12 13 14 Viscosupplementation with HA intra-articular injections is a nonsurgical treatment that can improve pain relief and lead to a partial recovery of glenohumeral joint ROM. Many studies have demonstrated that HA intra-articular injections may improve the cartilage homeostasis having protective effects on the joint cartilage in this degenerative pathology, 15 16 17 18 19 20 21 22 23 24 25 26 27 28 especially in knee OA. 29 30 31 32 33 However, the efficacy and safety of HA intra-articular injection treatment in glenohumeral OA needs to be further investigated, since only few studies have evaluated the efficacy and safety of HA in OA of the shoulder. 8 17 21 34 35 36
The objective of this randomized prospective open-label clinical trial was to evaluate the efficacy and safety of intra-articular injection treatment with high-molecular-weight HA in patients affected by moderate to severe glenohumeral OA in terms of pain reduction and improvements of limited ROM. The hypothesis of the study was that HA intra-articular injections in patients affected by moderate to severe glenohumeral OA is a safe procedure that can reduce shoulder pain and improve glenohumeral ROM.
Methods
Study Design
This randomized controlled prospective open-label monocentric study was designed to determine whether intra-articular injections of HA (Hyalubrix, 30 mg/2 mL, molecular weight > 1,500 kDa, Fidia Farmaceutici S.p.A.) in patients affected by grade II–IV shoulder OA provide significant reduction in pain during activity at up to 6 months.
Participants
Seventy-eight patients affected by grade II and III OA and grade IV shoulder OA with contraindications to surgical treatment were considered for the purpose of this study and followed for 6 months. Local ethics committee approval (Concordia Hospital for Special Surgery Rome Ethical Committee approval no. 3/2014) and written informed consent were obtained prior to the patient's enrolment, and the study was conducted in accordance with the Helsinki Declaration of 1975 and subsequent revisions.
The criteria for the inclusion in the study were: patients with good general health status older than 50 years, radiographic confirmation of grade II or III shoulder OA or grade IV shoulder OA with contraindications to surgical treatment, chronic shoulder pain for at least 6 months but less than 2 years, and limitations in ROM.
Reasons for exclusion from the study were: concomitant rotator cuff tears, adhesive capsulitis, previous shoulder surgery, previous humeral head fractures, chondrocalcinosis, cervical spine disorders, metabolic diseases, and poor general health status. Furthermore, patients with grade I OA and those with grade IV OA with surgical indications (shoulder arthroplasty) were not included in the study. All analgesics, bisphosphonates, and oral pharmaceutical products containing glucosamine and chondroitin sulfate had to be discontinued 15 days prior to the beginning of treatment and baseline assessment.
Interventions
Patients were randomly allocated to two different homogeneous groups. Thirty-nine patients for the first group (case group) and 39 patients for the second group (control group) were recruited. The sample was systematically randomized; for every two patients, the assignment criteria were inverted to allocate the patients uniformly to two different groups.
The treatment for patients belonging to the case group consisted of three intra-articular injections with HA (molecular weight > 1,500 kDa) and one injection every 15 days combined with a specific physiotherapy program. The intra-articular injections were performed by using a posterior shoulder approach. Patients belonging to the control group were treated only with physical therapy.
The physical therapy program was the same for both groups. It was performed with a professional therapist, had a 3-month duration with a frequency of 3 days every week, and started for both groups the day after the first medical examination. It consisted of passive capsular stretching for recovery of ROM, isometric exercises for deltoid, rotator cuff, and scapulothoracic muscles, isotonic exercises for scapulothoracic muscles (closed kinetic chain), and hydrokinesis therapy.
Outcome Measures
The follow-up examination was performed at 6 months from the beginning of the therapy for both groups. The evaluation of functional status of treated shoulder, ROM, and pain was performed before treatment and at the final follow-up examination by means of the Constant score. The safety evaluation of intra-articular injection with Hyalubrix (30 mg/2 mL) was further performed recording any adverse events (AEs) experienced by the patients during the study.
Statistical Analysis
Sample size calculation was based on the expected difference between groups in the primary outcome (Constant score). According to data obtained in our previous study, 35 setting α value equal to 0.05 and minimum accepted power of 80%, we retained the sample of 78 patients (39 for each group) appropriate for this study.
Statistical analysis was performed by STATISTICA 7.0 software (StatSoft Inc, Tulsa, Oklahoma, United States). Outcome variables (forward elevation, external rotation, and Constant score) were considered as continuous, and distribution of subjects along the three variables verged on normality ( p > 0.05; Shapiro–Wilk = 0.958, 0.975, and 0.946, respectively); therefore, a one-way ANOVA for repeated measures was performed. Post hoc tests (Tukey's test, p < 0.05) were scheduled between the two groups and within the same group. Afterward, a subgroup analysis was performed within the case group according to the severity of OA (16 patients with grade II, 14 with grade III, and 9 with grade IV). In this way, a one-way ANOVA for independent groups was performed. The treatment safety was assessed through descriptive statistics of vital signs and summary of AEs.
Results
Of the 39 patients belonging to the case group, 17 were males and 22 were females. The mean age of the patients was 71.3 ± 6.7 years. There were 31 right shoulders and 8 left shoulders. The dominant side was treated in 28 patients (71.8%). All patients referred shoulder pain since many months (average 11.4 ± 4.8 months); 25 of the patients (64.1%) had moderate pain and 14 (35.9%) had severe pain; none of them had mild pain; 10 (25.6%) of our patients had been involved in trauma; and 29 (74.4%) of the patients had a spontaneous pain. All the patients showed signs of OA at the X-ray examination: grade II in 16 (41%), grade III in 14 (35.9%), and grade IV in 9 (23.1%) OA.
Of the 39 patients belonging to the control group, 15 were males and 24 were females. The mean age of the patients was 69.8 ± 6.4 years. There were 29 right shoulders and 10 left shoulders. The dominant side had been treated in 31 patients (79.5%). All patients referred shoulder pain for several months (average 10.2 ± 3.8 months); 4 of the patients (10.3%) had mild pain, 27 (69.2%) had moderate pain, and 8 (20.5%) had severe pain; 9 (23.1%) of our patients had been involved in trauma, and 30 (76.9%) of the patients had a spontaneous pain. All the patients showed signs of OA at the X-ray examination: 18 (46.1%) had grade II, 14 (35.9%) had grade III, and 7 (17.9%) had grade IV OA. No significant differences were observed between the two groups for baseline characteristics.
Means and standard deviations of the outcome measures for each group, before and after treatment, are reported in Table 1 . There were no significant differences between the two groups before the treatment. Constant score, forward elevation, and external rotation variables were similar in the two groups at the baseline evaluation ( p > 0.05). The ANOVA analysis for repeated measures for Constant score revealed a significant effect of the treatment between the groups (F 1.76 = 7.885, p < 0.05) and within groups (F 1.76 = 15.735, p < 0.05). Regarding the forward elevation, the ANOVA analysis for repeated measure depicted a significant effect only within groups (F 1.76 = 6.611, p < 0.05), suggesting that there was a significant effect of the treatment along the time but not between the type of treatment (F 1.76 = 0.655, p > 0.05). Differently, about the external rotation, the statistical analysis did not show a significant difference between the groups (F 1.76 = 1.061, p > 0.05) nor within the groups (F 1.76 = 0.835, p > 0.05).
Table 1. Means and standard deviations for case and control groups before (t 0 ) and after (t 1 ) treatment .
| Control group | HA group | |
|---|---|---|
| Constant score t0 | 67.1 ± 15.1 | 71.9 ± 12.1 |
| Constant score t1 | 77.3 ± 13.8 | 88.1 ± 9.3 a |
| Elevation t0 | 137.9 ± 21.5 | 138.6 ± 16.7 |
| Elevation t1 | 146.8 ± 19.8 | 152.8 ± 15.9 |
| External rotation t0 | 24.2 ± 6.2 | 22.3 ± 6.9 |
| External rotation t1 | 26.4 ± 7.9 | 25.1 ± 7.1 |
Note: t0 Baseline evaluation; t1 Follow-up evaluation.
p < 0.05; post hoc Tukey's test.
The one-way ANOVA performed only for the case group subjects revealed a significant effect of the treatment (F 2.36 = 7.829, p < 0.05). In particular, patients affected by grade III and IV OA had a significant improvement in the Constant score (18.2 ± 5.4 and 19.2 ± 5.9, respectively). On the other hand, patients affected by grade II OA had no significant improvement in the Constant score ( p < 0.05 at the post hoc Tukey's test, Fig. 1 ).
Fig. 1.
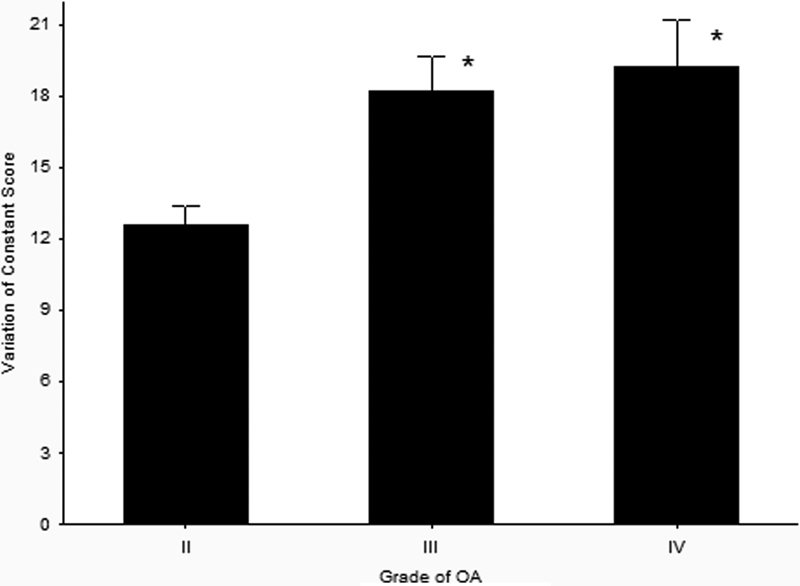
Variation of Constant score (y-axis) after treatment in the case group, according to severity of OA (bars indicate the standard error). Grade III and IV OA showed a significantly higher variation compared with grade II (* p < 0.05 post hoc Tukey's test).
Discussion
Glenohumeral OA is a progressive disease that can compromise the activities of work and daily living because of its symptoms such as pain and reduction of ROM. Therefore, nonsurgical treatments are directed toward reducing symptoms and improving joint function.
The use of HA in patients affected by shoulder OA is described in literature in a few studies. Kwon et al, 17 in a multicenter, randomized, double-blind, placebo-controlled trial, showed that only patients without concomitant shoulder pathologies, treated with intra-articular injections of HA, had a significant improvement in terms of pain. Similarly, Porcellini et al 34 and Di Giacomo et al, 35 in their prospective studies, showed that HA treatment for shoulder OA significantly decreased pain and improved shoulder function for up to 6 months from the first injection. Also, Merolla et al, 21 in a retrospective controlled trial, found that patients affected by mild to moderate glenohumeral OA had significant pain reduction and satisfaction, for up to 6 months, after treatment with intra-articular injections of HA. Silverstein et al 36 found a significant improvement of shoulder pain in patient treated with 3 weekly HA intra-articular injections and no adverse events were observed. On the other hand, Blaine et al 8 and Colen et al 37 indicated that sodium hyaluronate is effective and well tolerated for the treatment of OA and persistent shoulder pain, but significant improvement in terms of shoulder pain was not achieved.
The purpose of the study was to evaluate the efficacy and safety of intra-articular injections with high-molecular-weight HA (Hyalubrix) in patients affected by moderate to severe glenohumeral OA. To achieve this, two different kinds of treatments were compared: three intra-articular injections with HA (Hyalubrix, 30 mg/2 mL, molecular weight > 1,500 kDa) associated with physical therapy rehabilitation versus the only physical therapy treatment. This open-label study on 78 patients showed a significant difference in pain relief ( p < 0.05) between the two groups of patients in favor of HA. This demonstrated that patients affected by grade II–IV OA, who received HA intra-articular injections treatment in association with physical therapy, had a greater positive effect in terms of pain reduction compared with patients who received the only physical therapy treatment. Differently, this study did not show a significant difference in terms of ROM, between the two different types of treatment. Moreover, the reduction of pain led to an improvement in glenohumeral function and activity of daily living. This was due to the specific characteristics of HA able to restore synovial fluid properties in this degenerative disease. 15 16 17 18 19 20 21 22 23 24 25 26 27 28
Results of the study also showed a significant difference within the case group. In particular, patients affected by grade III and IV OA had a significant pain reduction, whereas patients affected by grade II OA had an improvement in pain, but it was not significant. This could be due to the molecular weight of Hyalubrix (>1,500 kDa) that also has an important mechanical effect.
Thanks to the efficacy of HA treatment and to the absence of side effects or adverse events, we can confirm that three intra-articular injections of Hyalubrix can be considered a safe and effective treatment option for the management of shoulder pain due to moderate to severe glenohumeral OA. However, further prospective randomized controlled trials are necessary to provide exhaustive evidence of the long-term efficacy of HA-derived products in the treatment of glenohumeral OA in a larger population.
In conclusion, this study demonstrates the greater and long-lasting efficacy and safety of an intra-articular injection treatment with HA (Hyalubrix, 30 mg/2 mL) combined with a physical therapy program in patients affected by moderate to severe glenohumeral OA in terms of pain relief and function improvement, compared with alternative treatments such as only physical therapy.
References
- 1.Nakagawa Y, Hyakuna K, Otani S, Hashitani M, Nakamura T. Epidemiologic study of glenohumeral osteoarthritis with plain radiography. J Shoulder Elbow Surg. 1999;8(06):580–584. doi: 10.1016/s1058-2746(99)90093-9. [DOI] [PubMed] [Google Scholar]
- 2.Chakravarty K, Webley M. Shoulder joint movement and its relationship to disability in the elderly. J Rheumatol. 1993;20(08):1359–1361. [PubMed] [Google Scholar]
- 3.Steinfeld R, Valente R M, Stuart M J. A commonsense approach to shoulder problems. Mayo Clin Proc. 1999;74(08):785–794. doi: 10.4065/74.8.785. [DOI] [PubMed] [Google Scholar]
- 4.Memel D S, Kirwan J R, Sharp D J, Hehir M. General practitioners miss disability and anxiety as well as depression in their patients with osteoarthritis. Br J Gen Pract. 2000;50(457):645–648. [PMC free article] [PubMed] [Google Scholar]
- 5.Andrews J R. Diagnosis and treatment of chronic painful shoulder: review of nonsurgical interventions. Arthroscopy. 2005;21(03):333–347. doi: 10.1016/j.arthro.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, Calis H T. Is intraarticular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis? Rheumatol Int. 2006;26(06):536–540. doi: 10.1007/s00296-005-0022-2. [DOI] [PubMed] [Google Scholar]
- 7.Carfagno D G, Ellenbecker T S. Osteoarthritis of the glenohumeral joint: nonsurgical treatment options. Phys Sportsmed. 2002;30(04):19–30. doi: 10.3810/psm.2002.04.253. [DOI] [PubMed] [Google Scholar]
- 8.Blaine T, Moskowitz R, Udell J et al. Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. A multicenter study. J Bone Joint Surg Am. 2008;90(05):970–979. doi: 10.2106/JBJS.F.01116. [DOI] [PubMed] [Google Scholar]
- 9.Brander V A, Gomberawalla A, Chambers M, Bowen M, Nuber G. Efficacy and safety of hylan G-F 20 for symptomatic glenohumeral osteoarthritis: a prospective, pilot study. PM R. 2010;2(04):259–267. doi: 10.1016/j.pmrj.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Itokazu M, Matsunaga T. Clinical evaluation of high-molecular-weight sodium hyaluronate for the treatment of patients with periarthritis of the shoulder. Clin Ther. 1995;17(05):946–955. doi: 10.1016/0149-2918(95)80072-7. [DOI] [PubMed] [Google Scholar]
- 11.Ramonda R, Franceschini M, Leardini G.Treatment of shoulder periarthritis with hyaluronic acid Riv Ital Biol Med 199851(2 Suppl):1 [Google Scholar]
- 12.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines.Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update Arthritis Rheum 200043091905–1915. [DOI] [PubMed] [Google Scholar]
- 13.Singh G.Recent considerations in nonsteroidal anti-inflammatory drug gastropathy Am J Med 1998105(1B):31S–38S. [DOI] [PubMed] [Google Scholar]
- 14.Jordan K M, Arden N K, Doherty M et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) Ann Rheum Dis. 2003;62(12):1145–1155. doi: 10.1136/ard.2003.011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinusas K. Osteoarthritis: diagnosis and treatment. Am Fam Physician. 2012;85(01):49–56. [PubMed] [Google Scholar]
- 16.Balazs E A, Denlinger J L. Viscosupplementation: a new concept in the treatment of osteoarthritis. J Rhematol Suppl. 1993;39:3–9. [PubMed] [Google Scholar]
- 17.Kwon Y W, Eisenberg G, Zuckerman J D. Sodium hyaluronate for the treatment of chronic shoulder pain associated with glenohumeral osteoarthritis: a multicenter, randomized, double-blind, placebo-controlled trial. J Shoulder Elbow Surg. 2013;22(05):584–594. doi: 10.1016/j.jse.2012.10.040. [DOI] [PubMed] [Google Scholar]
- 18.Colen S, Haverkamp D, Mulier M, van den Bekerom M P. Hyaluronic acid for the treatment of osteoarthritis in all joints except the knee: what is the current evidence? BioDrugs. 2012;26(02):101–112. doi: 10.2165/11630830-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Gu Q, Zhou N, Shanghai J. Research progress of viscosupplementation [Article in Chinese] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011;25(06):755–760. [PubMed] [Google Scholar]
- 20.Abate M, Pulcini D, Di Iorio A, Schiavone C. Viscosupplementation with intra-articular hyaluronic acid for treatment of osteoarthritis in the elderly. Curr Pharm Des. 2010;16(06):631–640. doi: 10.2174/138161210790883859. [DOI] [PubMed] [Google Scholar]
- 21.Merolla G, Sperling J W, Paladini P, Porcellini G. Efficacy of Hylan G-F 20 versus 6-methylprednisolone acetate in painful shoulder osteoarthritis: a retrospective controlled trial. Musculoskelet Surg. 2011;95(03):215–224. doi: 10.1007/s12306-011-0138-3. [DOI] [PubMed] [Google Scholar]
- 22.Abatangelo G, O'Regan M. Hyaluronan: biological role and function in articular joints. Eur J Rheumatol Inflamm. 1995;15:9–16. [Google Scholar]
- 23.Altman R D, Moskowitz R; Hyalgan Study Group.Intraarticular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial J Rheumatol 199825112203–2212. [PubMed] [Google Scholar]
- 24.Carrabba M, Paresce E, Angelini M, Re K A, Torchiana E EM, Perbellini A. The safety and efficacy of different dose schedules of hyaluronic acid in the treatment of painful osteoarthritis of the knee with joint effusion. Eur J Rheumatol Inflamm. 1995;15:25–31. [Google Scholar]
- 25.Maheu E. Hyaluronan in knee osteoarthritis: a review of clinical trials with Hyalgan. Eur J Rheumatol Inflamm. 1995;15:17–24. [Google Scholar]
- 26.Kotz R, Kolarz G.Intra-articular hyaluronic acid: duration of effect and results of repeated treatment cycles Am J Orthop 199928(11, Suppl)5–7. [PubMed] [Google Scholar]
- 27.Frizziero L, Govoni E, Bacchini P. Intra-articular hyaluronic acid in the treatment of osteoarthritis of the knee: clinical and morphological study. Clin Exp Rheumatol. 1998;16(04):441–449. [PubMed] [Google Scholar]
- 28.Listrat V, Ayral X, Patarnello F et al. Arthroscopic evaluation of potential structure modifying activity of hyaluronan (Hyalgan) in osteoarthritis of the knee. Osteoarthritis Cartilage. 1997;5(03):153–160. doi: 10.1016/s1063-4584(97)80010-6. [DOI] [PubMed] [Google Scholar]
- 29.Migliore A, Tormenta S, Martin Martin L S et al. The symptomatic effects of intra-articular administration of hylan G-F 20 on osteoarthritis of the hip: clinical data of 6 months follow-up. Clin Rheumatol. 2006;25(03):389–393. doi: 10.1007/s10067-005-0052-x. [DOI] [PubMed] [Google Scholar]
- 30.Stitik T P, Blacksin M F, Stiskal D M et al. Efficacy and safety of hyaluronan treatment in combination therapy with home exercise for knee osteoarthritis pain. Arch Phys Med Rehabil. 2007;88(02):135–141. doi: 10.1016/j.apmr.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Phiphobmongkol V, Sudhasaneya V. The effectiveness and safety of intra-articular injection of sodium hyaluronate (500-730 kDa) in the treatment of patients with painful knee osteoarthritis. J Med Assoc Thai. 2009;92(10):1287–1294. [PubMed] [Google Scholar]
- 32.Foti C, Cisari C, Carda S et al. A prospective observational study of the clinical efficacy and safety of intra-articular sodium hyaluronate in synovial joints with osteoarthritis. Eur J Phys Rehabil Med. 2011;47(03):407–415. [PubMed] [Google Scholar]
- 33.Vetro A, Iovane A, Di Gesu M, Giordan N, Mantia F, Mantia R. Pain relief and functional recovery over a six-month period after intra-articular injection with sodium hyaluronate (Mw 1500 - 2000 Kda) in osteoarthritis of the knee. Eur J Musculoskel Dis. 2014;3:25–33. [Google Scholar]
- 34.Porcellini G, Merolla G, Giordan N et al. Intra-articular glenohumeral injections of HYADD®4-G for the treatment of painful shoulder osteoarthritis: a prospective multicenter, open-label trial. Joints. 2016;3(03):116–121. doi: 10.11138/jts/2015.3.3.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Giacomo G, De Gasperis N. The role of hyaluronic acid in patients affected by glenohumeral osteoarthritis. J Biol Regul Homeost Agents. 2015;29(04):945–951. [PubMed] [Google Scholar]
- 36.Silverstein E, Leger R, Shea K P. The use of intra-articular hylan G-F 20 in the treatment of symptomatic osteoarthritis of the shoulder: a preliminary study. Am J Sports Med. 2007;35(06):979–985. doi: 10.1177/0363546507300256. [DOI] [PubMed] [Google Scholar]
- 37.Colen S, Geervliet P, Haverkamp D, Van Den Bekerom M P. Intra-articular infiltration therapy for patients with glenohumeral osteoarthritis: a systematic review of the literature. Int J Shoulder Surg. 2014;8(04):114–121. doi: 10.4103/0973-6042.145252. [DOI] [PMC free article] [PubMed] [Google Scholar]


