Abstract
Background:
Chronic noncommunicable diseases (NCDs) could increase the risk of catastrophic health expenditure (CHE). The present study aims to analyze CHE among households with and without chronic NCDs in Hamedan.
Methods:
In this cross-sectional study, 780 households’ patients, who were being discharged from hospitals in Hamedan, were selected using a proportional stratified random sampling method. Required data were collected through interview and observation using World Health Organization standard questionnaire. A household with chronic NCDs is defined as the one with ≥1 chronic disease patient. Both descriptive and analytical statistics, as well as different approaches and thresholds, were used to study CHE among households.
Results:
The households with chronic disease had higher incidence and intensity of CHE in all approaches and threshold. This result was shown through distributive-sensitive measures. The Regression analysis revealed that lower economic status, lower household size, and high utilization of health care were associated with the CHE incidence and intensity in the households with chronic NCDs in Hamedan.
Conclusions:
There is a high degree of CHE were caused by chronic NCDs. By thoughtful reconsideration in health-care financing, along with addressing relevant socioeconomic factors, the health system of Iran could cope with financial adversities caused by chronic NCDs.
Keywords: Catastrophic health expenditure, chronic diseases, Hamedan, Iran
Introduction
Despite the substantial improvement in health outcome, it seems that financial catastrophe with the use of health-care services emerges as a health system-threatening event.[1,2] Catastrophic health expenditure (CHE), defined as out-of-pocket (OOP) health spending that goes far from a certain proportion of a household financial capability, accounted as the failure of the health system to shelter the public from the financial consequences of health care.[2,3] CHE could pose household in formidable situation and especially in its high degrees push financially vulnerable households into poverty.[3,4] In this regard, various studies have emphasized that households with chronic disease are in the high risk to incur CHE.[5,6,7]
Chronic noncommunicable diseases (NCDs) impose a formidable burden on the health system in the world.[8] In the recent decades, because of epidemiological transition, this burden has been accelerated, especially among developing nations; currently, these nations simultaneously suffered from both chronic diseases and infectious diseases.[9] These diseases not only caused premature death but also had major negative effects on the quality of well-being of suffered individuals and caused influences to damage economic of families and in higher degrees of societies.[10,11] The management of chronic NCDs requires more complex and more expensive health-care services. This could enlarge the risk of catastrophic health payment, especially for households without insurance and for those covered by a weak insurance plan.[8]
Like other developing nations, Iran has undergone rapid epidemiological transition in the recent decades. While infectious diseases were the main causes of mortality in Iran in 1960, temporarily chronic NCDs and other noncommunicable conditions such as cardiovascular disease and traffic injuries play a prominent role.[12] Although many studies examined CHE in Iran, most focused on whole populations rather than vulnerable groups such as households with chronic disease. Accordingly, we not only compare the incidence and intensity of CHE among households with and without chronic NCDs patients in Hamedan but also it was investigated the determinant factors of the incidence and intensity of CHE among households with chronic disease members.
Methods
Study context
The study was carried out in Hamedan, the capital of Hamedan province, Iran. According to the National Census held in 2011, the population of the province was1.75 million. Hamedan province has different regions in terms of economic conditions. There is a remarkable economic inequality between the villages and the cities of Hamedan province.[13] Pervious research emphasized that chronic NCDs and their risk factors were increasing in this province.[14]
Sampling
The sample size was determined using the level of significance (α) of 0.05, relative precision (d) of 0.0228, and the expected proportion of households incurring catastrophic health-care payment (P) of = 12%.[15] A total of 780 households were selected from the list of households that benefited from inpatient services in hospitals of Hamedan using proportional random sampling method. The designing and conducting of this cross-sectional study were spanned from July to August 2014. After excluding the missing data, the analysis was performed for 772 households.
Data collection
The household-related section of the World Health Survey questionnaire, developed by World Health Organization in 2003, was used as data collection instrument. The questionnaire was used to evaluate the performance of health systems in various studies. The validity and reliability of this section were verified in a previous study.[15] Alongside the socioeconomic variables, the presence of chronic NCDs such as cardiovascular disease, diabetes, cancer or malignant tumor, kidney disease, arthritis, and asthma was investigated in this study. A household with chronic NCDs is defined as the one with ≥1 chronic disease patient. Required data were collected through interview and observation.
Measuring catastrophic health-care expenditure
We followed the income approach, proposed by Wagstaff and van Doorslaer[16] to measure catastrophic health-care payments. In this approach, an OOP payment of health care is considered “catastrophic” when the payment exceeds some threshold. This threshold could be defined as a fraction of the total household expenditure or nonfood expenditure.[8,16] As different studies used different thresholds,[8,17] in this study simultaneously we used different thresholds. The indicator E was used to show whether CHE occurred:[8,16]

Where xi is the total expenditures of household i, f(x) is the food expenditure of that household, and Z is the given catastrophic threshold. Based on this definition, the incidence and intensity[8,16] of CHE could be obtained by:
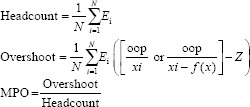
In the abovementioned formulas, N is the sample size. The headcount, standing as the incidence of CHE, is the percentage of households whose OOP expenditures, as a fraction of total household expenditures or nonfood household expenditures, exceeded a predefined threshold.[8,16] The intensity of CHE could be studied by calculating the overshoot and the mean positive overshoot (MPO). In this regard, the degree by which an average OOP expenditure crossed the given catastrophic threshold was measured by the overshoot index. Moreover, MPO shows the degree by which the average OOP expenditure of a household passed the predefined threshold.[16,17] However, the inclusion of distributional considerations in the analysis could reflect the real feature of the sample.[16] To do this, we had to merge the distributional index, here a complement of the respective concentration index (CI), to intensity and overshoot measures. These distributional-oriented measures, as it calls rank-weighted measures, could be obtained by the following formulas.[8,17]
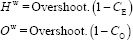
In the above-mentioned formulas, CE and CO respectively show the CI of CHE incidence and intensity. The formula for estimating the CI is:[18]

Where Y stand for the headcount and overshoot of CHE in this study, is its mean, and is the fractional rank of households in the distribution of economic status.[18] In this study, the household total expenditure was considered for the economic status.
Statistical analysis
The Mann–Whitney test was used to compare OOP health payments and other expenditures alongside health-care utilization among households with and without chronic disease members. Furthermore, the Chi-square and t-tests were used to compare the headcount and overshoot measures, respectively, between these households. Univariate analysis such as Chi-square, t-test, one-way ANOVA, and Pearson correlation was used to analyze headcount and overshoot measures across factors of households with chronic NCDs. Supplementary insurance status (yes/no), sex of household head (male/female), household size (1–2 members/3–6 members/≥7 members), having a member over 60 years of age (yes/no), economic status (Quintile 1 [poorest]/Quintile 2/Quintile 3/Quintile 4/Quintile 5 [richest]), and reporting inpatient (number of hospitalizations) and outpatient service (number of outpatient visits) usage were the variables included in the univariate analysis. Because all the studied households with chronic NCDs were under the coverage of basic health insurance, we excluded this variable from the analysis. Finally, multiple logistic regression and linear regression analysis were respectively used to estimate determinant factors of the incidence and intensity of CHE in households with chronic disease patients. The data were analyzed using Stata 12 (Stata Corp, College Station, TX, USA). A significance level of P < 0.05 was used in the present study.
Results
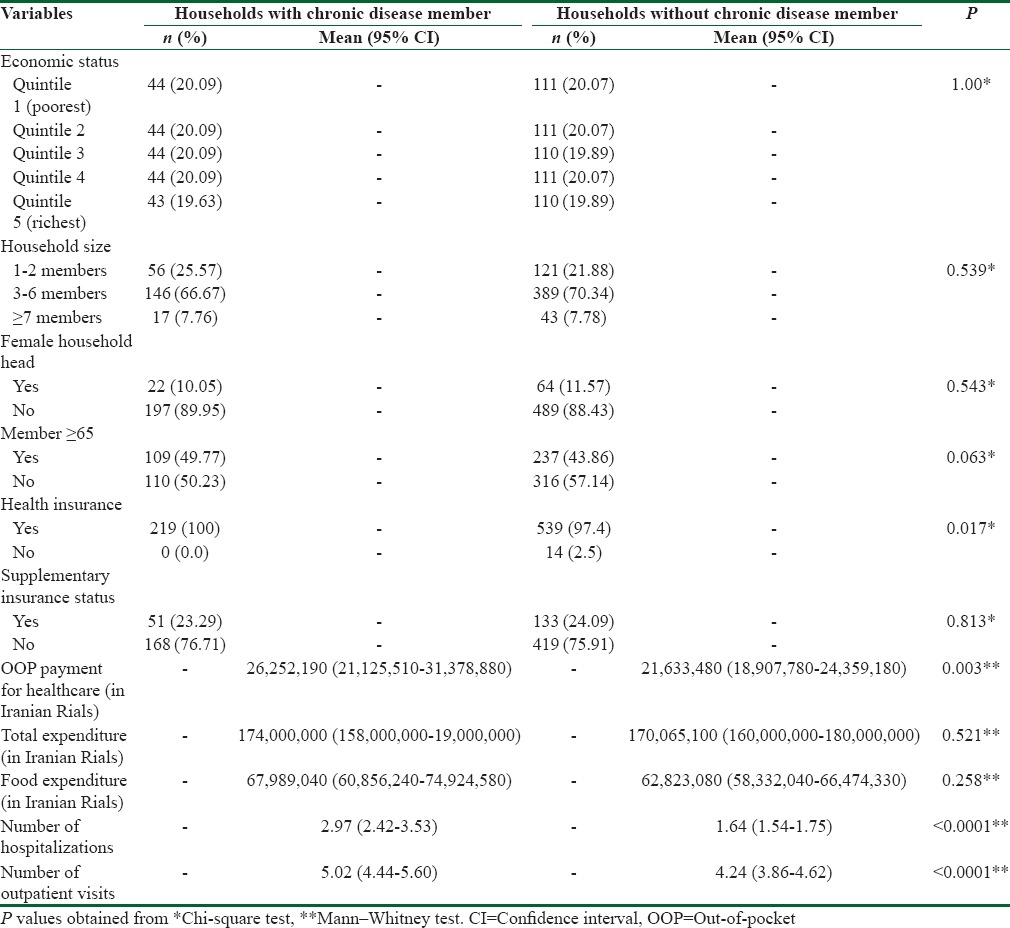
We identified that 219 (28.3%) of the studied households reported at least one member with chronic NCDs. On the other side, 553 (71.7%) households reported no chronic patient. As Table 1 shows, most of the studied households were under the coverage of health insurance. Nevertheless, a majority of them did not have any supplementary insurance. The mean of utilized health-care services alongside the OOP health payment and other expenditures for those households with and without chronic disease members are also reported in Table 1. As this shows, households with chronic NCDs, in comparison with their counterparts, had larger OOP health care (P < 0.01). These households also had higher inpatient and outpatient health service utilization patterns (P < 0.01). On the other hand, there is no significant difference regards to total expenditure and food expenditure of the studied households.
Table 1.
Socioeconomic characteristics, out-of-pocket, total expenditures, food expenditure, and health-care utilization of studied households
The CHE incidence and intensity, defined by headcount and overshoot measures, for entire households and the households with and without chronic disease were depicted in Table 2. As shown in this table, for every defined threshold, both the headcount and the overshoot measures of nonfood expenditure approach are larger than their counterparts related to the total expenditure approach.
Table 2.
Incidence and intensity of catastrophic health expenditure in Hamadan
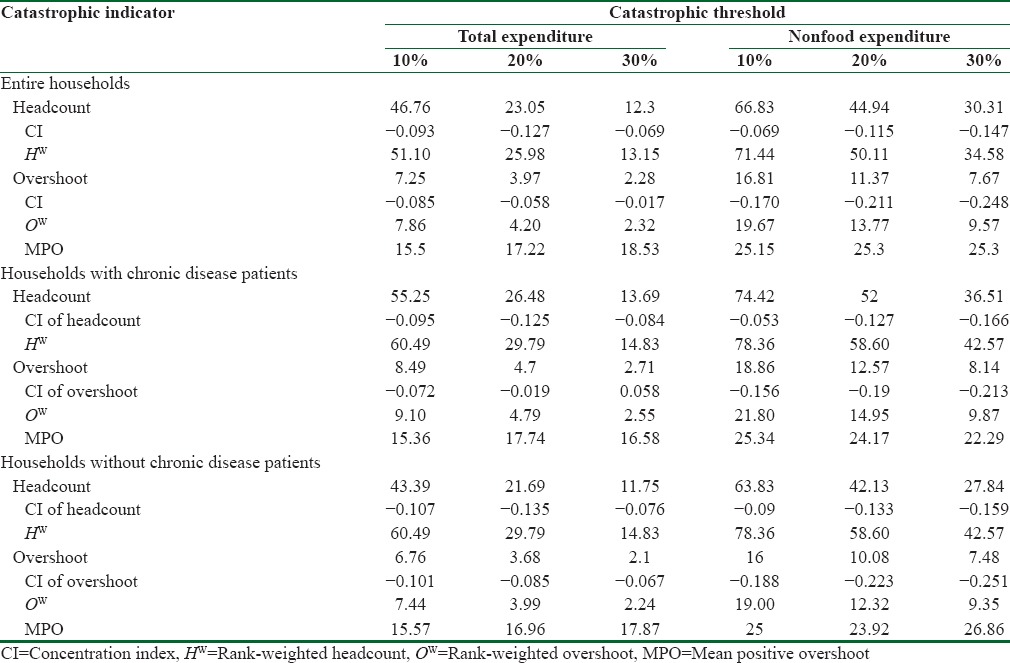
As the threshold was raised from 10% to 30% of the total expenditure, the headcount of CHE decreased from 46.76% to 12.3%, and the mean of overshoot decreased from 7.25% to 2.28% of the total expenditures. This decreasing pattern could also be seen for the OOP share of the nonfood expenditures. MPO was the proportion of overshoot on headcount, and it did not need to decline as the threshold was raised. As mentioned above, MPO shows the degree by which the average OOP expenditure of a household passed the predefined threshold. For example, the household that faced with CHE at 10% of the total expenditure averagely devoted 25.5% (15.5% +10%) of their earning to afford health services.
At every given threshold, households with chronic NCDs had the greater headcount and overshoot. In this regard, at 30% of nonfood expenditure, the headcount and overshoot measures for the household with chronic disease patient were 36.51 and 21.14, respectively, whereas households without chronic patient experienced lower incidence and intensity of CHE. The Chi-square test revealed that the observed headcounts of the households with chronic NCDs were significantly greater than those of their counterparts (all of the Chi-square statistics were significant at P = 0.05). On the other hand, for the overshoot masseurs, there is no statistically significant (all of the t-test statistics were insignificant at P = 0.05).
Table 2 also represents the distributive-oriented incidence and intensity of CHE for the given thresholds in Hamedan. As this table shows, except the overshoot at 30% of the total expenditure, the households with chronic disease patients as well as their counterparts had negative CI of headcount and overshoot. This means that poor households were mostly affected by CHE. After the modifications of distributive measures, households with chronic disease patients had still greater incidence and intensity of CHE because of having higher rank-weighted headcount and overshoot.
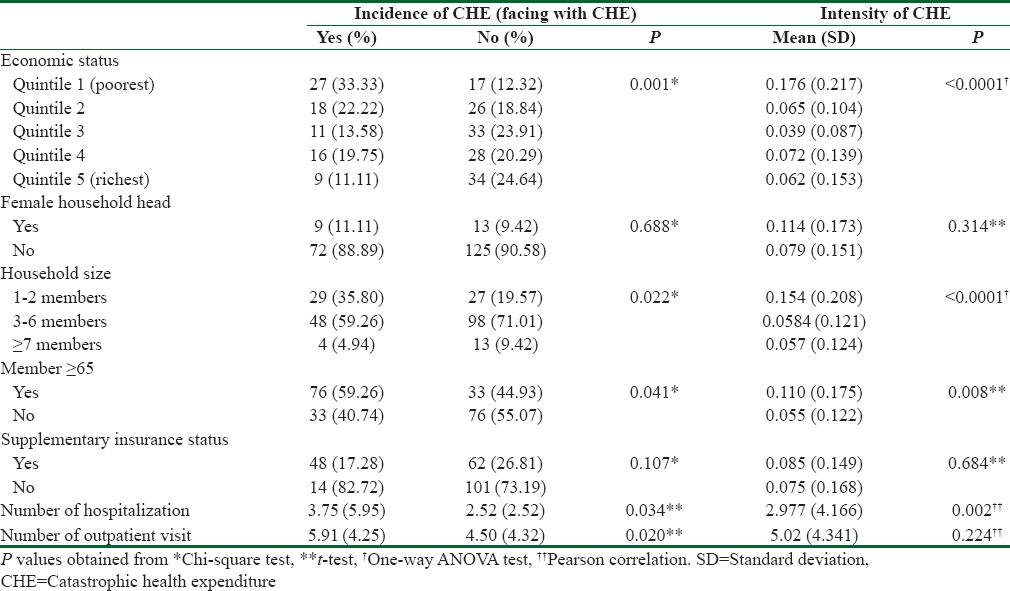
Table 3 represents the results of univariate analysis for the incidence and intensity of CHE at a nonfood expenditure threshold of 30% for households with chronic NCDs member. As this table shows, except the female household head and supplementary insurance (P > 0.05), all of the analyzed factors were significantly related to the incidence of CHE. Like incidence of CHE, apart from the female household head, supplementary insurance, and a number of outpatient visit (P > 0.05), other analyzed factors have a statistically significant relationship with intensity of CHE.
Table 3.
Association between the incidence and intensity of catastrophic health expenditure and sociodemographical characteristics of the households with cryonic disease member
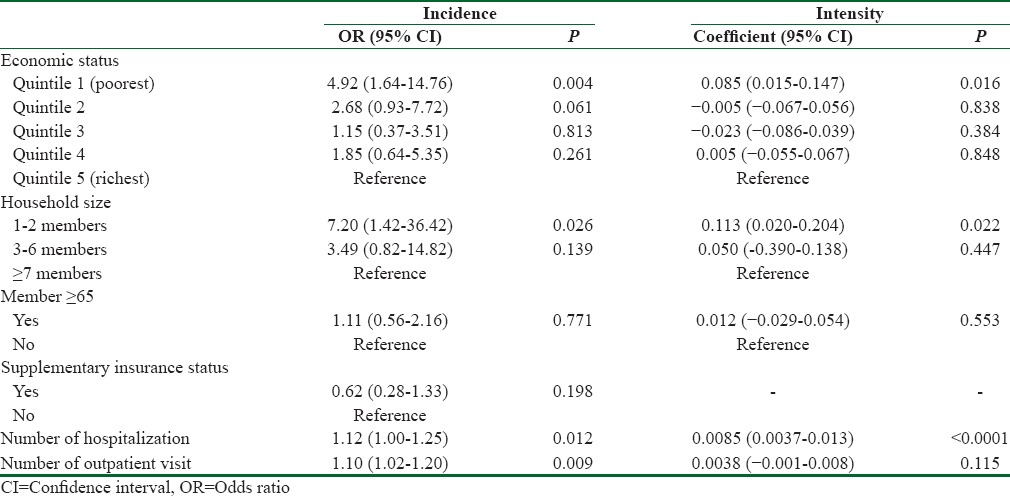
The determinant factors of the incidence and intensity of CHE at a nonfood expenditure threshold of 30% for households with chronic NCDs member are represented in Table 4. As this table shows, some factors (factors with P > 0.25) in the univariate analysis have been excluded from the logistic and linear regression analysis. The multiple logistic regression revealed that poorest economic status significantly increases the incidence of CHE (P < 0.01). Other analyzed factors that increased the odds of incidence of CHE were lower household size (P < 0.01), number of hospitalization (P < 0.05), and number of outpatient visit (P < 0.01). Linear regression analysis was used to quantify determinant factor of CHE intensity. Like incidence of CHE, poorest economic status (P < 0.05) significantly increases the intensity of CHE in Hamadan. Lower household size (P < 0.05) and a number of hospitalization (P < 0.01) were other significant determinant factors of CHE intensity in Hamadan.
Table 4.
Determinants of incidence and intensity of catastrophic health expenditure among households with chronic disease member
Discussion
To the best of our knowledge, although former research[19] studied the incidence of CHE among households with cancer patients in Shiraz, this research is the first to analyze and compare the incidence and intensity of CHE among families with and without chronic disease members in Islamic Republic of Iran. The higher proportion of households with self-reported chronic NCDs in this study (28.3%) demonstrates that these diseases have already impacted a large population in this city. Another study in Hamedan also emphasized the higher prevalence of chronic diseases’ risk factors.[14] Several other studies pointed out that chronic NCDs had prompted substantial burden of disease in Iran.[12]
Findings showed that the studied households had greater OOP health expenditure than the national level, reflected in household's budget survey. Households with patients of chronic disease, in comparison with their counterparts, averagely spent a higher proportion of their earnings on health services. This is in line with other studies[5,6] conducted in this field. To examine the incidence and intensity of financial hardship due to utilization of health services, two approaches and different thresholds were used among the studied households. As discussed in a former research, this could bring a wider view about CHE incurrence and intensity in every context.[17]
Findings revealed that households with chronic disease members, at any thresholds, had greater incidence and intensity of CHE in comparison with the total sample and their counterparts. Of course, the observed differences in terms of the overshoot measures between the studied households were statistically insignificant. Anyway, the greater risk of CHE incidence related to the households with chronic disease patients must attract much attention of policymakers. Different studies in other countries[5,6,8,11] also reported that chronic NCDs could increase the catastrophic health payment.
As the CIs revealed, the disadvantaged households, in both groups, suffered from CHE incidence and intensity. Other studies also showed that the incidence and intensity of CHE were unequally distributed among poor households with chronic disease member.[6,8] Due to higher opportunity costs of health-care spending by the poor, the increasing CHE among poor households is a very concerning issue.[6] After the distributional modification, we showed that the households with chronic disease members had higher incidence and intensity of CHE. This finding confirms another study conducted in India.[6]
We proved that poor households with chronic disease patients were at higher risk to incur CHE and also suffered from its intensity. Previous researches in other nations[6,8,11] also reported the same results. This finding seems logical; the poor households affected by chronic conditions paid higher proportions of their earnings to afford the required health-care services. This issue must prompt policymakers to devise health-care financing framework to shelter not only poor households with chronic disease members but also other poor households, from facing with CHE.
The lower household size was another factor that could increase the incidence and intensity of CHE among households who were affected by chronic NCDs. In general, a decrease in the household size was accompanied with a decrease in the household's total income and savings.[20] This could intenerate small households, especially those with chronic disease members, against CHE incidence and intensity. The positive effect of lower household sizes on facing with CHE had been well documented in previous researches[8,20] both for the groups with chronic disease patients and the general population.
Nevertheless, we observed that supplementary insurance was negatively associated with the incidence and intensity of CHE among households affected by NCDs, but this result is insignificant. Apparently, people with chronic diseases have complicated health-care needs[6] that may not be included in the benefit package of basic health insurance. In this situation, supplementary insurance programs could relive financial hardships of vulnerable groups. Unfortunately, the public sector in Iran rarely contributes to provide supplementary insurance and these insurance plans are largely provided by the private sector.[21]
The findings also showed that utilization of health services was another factor that could increase the incidence and intensity of catastrophic payment among households with chronic disease members. Chronic NCDs forced the affected individuals to use somewhat complicated and expensive health-care services more and more.[6,8] Consequently, the households had to dedicate much more of theirs resources on health care for those ill members. Other studies also emphasized this fact.[8,9,11] Hence, it is strongly suggested that, alongside the improvisation to decrease CHE among chronic NCDs patients, the third-party payers and health-care providers must provide cost-effective health-care services not only to reduce their organizational expenditures but also to decrease indirectly the potential CHE incidence and intensity, especially among the groups with more health-care needs.
Some limitations of present research must be clarified. First, the cross-sectional design of this study did not allow the examination of long-term impacts of household direct OOP expenditures. Second, the OOP health payments and CHE incidence and intensity were only examined on the households with and without chronic disease members. Hence, we would not certainly assert that these OOP expenditures truly related with chronic diseases. Nevertheless, the potential side effects of chronic NCDs on health outcomes and welfare of the world must not be neglected. The tsunami of these diseases in every health system could surge formidable waves of financial burdens, both to households and health systems and probably widen the inequality of CHE among different groups socioeconomically.
Conclusions
We found that households affected by NCDs had higher OOP health payments in comparison with their peers without chronic disease members. Furthermore, the households, with and without distributional qualification, had greater incidence and intensity of CHE. Some socioeconomic factors significantly affected CHE occurrence and tolerance among households with chronic disease members. This means that relevant policies must consider the socioeconomic factors to decrease CHE more effectively. Moreover, thoughtful reconsideration must orient health insurance programs according to the expensive health-care needs emerged by NCDs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. Genvea: World Health Organization; 2000. [Google Scholar]
- 2.Anbari Z, Mohammadbeigi A, Mohammadsalehi N, Ebrazeh A. Health expenditure and catastrophic costs for inpatient-and out-patient care in Iran. Int J Prev Med. 2014;5:1023–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ, et al. Household catastrophic health expenditure: A multicountry analysis. Lancet. 2003;362:111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 4.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T, et al. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–83. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 5.Bhojani U, Thriveni B, Devadasan R, Munegowda C, Devadasan N, Kolsteren P, et al. Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore, India. BMC Public Health. 2012;12:990. doi: 10.1186/1471-2458-12-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One. 2013;8:e56873. doi: 10.1371/journal.pone.0056873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JW, Choi JW, Kim JH, Yoo KB, Park EC. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Serv Res. 2015;15:26. doi: 10.1186/s12913-014-0675-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z, Li X, Chen M. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. 2015;14:8. doi: 10.1186/s12939-015-0134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Counts CJ, Skordis-Worrall J. Recognizing the importance of Chronic disease in driving healthcare expenditure in Tanzania: Analysis of panel data from 1991 to 2010. Health Policy Plan. 2016;31:434–43. doi: 10.1093/heapol/czv081. [DOI] [PubMed] [Google Scholar]
- 10.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: How many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 11.Van Minh H, Xuan Tran B. Assessing the household financial burden associated with the chronic non-communicable diseases in a rural district of Vietnam. Glob Health Action. 2012;5:18892. doi: 10.3402/gha.v5i0.18892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forouzanfar MH, Sepanlou SG, Shahraz S, Dicker D, Naghavi P, Pourmalek F, et al. Evaluating causes of death and morbidity in Iran, global burden of diseases, injuries, and risk factors study 2010. Arch Iran Med. 2014;17:304–20. [PubMed] [Google Scholar]
- 13.Peirovedin MR, Mahdavi M, Ziyari YA. An analysis of effective factors on spatial distribution of poverty in rural regions of Hamedan Province. Int J Geogr Geol. 2016;5:86. [Google Scholar]
- 14.Poorolajal J, Zamani R, Mir-Moeini R, Amiri B, Majzoobi M, Erfani H, et al. Five-year evaluation of chronic diseases in Hamadan, Iran: 2005-2009. Iran J Public Health. 2012;41:71–81. [PMC free article] [PubMed] [Google Scholar]
- 15.Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27:613–23. doi: 10.1093/heapol/czs001. [DOI] [PubMed] [Google Scholar]
- 16.Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: With applications to Vietnam 1993-1998. Health Econ. 2003;12:921–34. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 17.Ghiasvand H, Abolghasem Gorji H, Maleki M, Hadian M. Catastrophic health expenditure among Iranian rural and urban households, 2013-2014. Iran Red Crescent Med J. 2015;17:e30974. doi: 10.5812/ircmj.30974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramezani Doroh V, Vahedi S, Arefnezhad M, Kavosi Z, Mohammadbeigi A. Decomposition of health inequality determinants in Shiraz, South-West Iran. J Res Health Sci. 2015;15:152–8. [PubMed] [Google Scholar]
- 19.Kavosi Z, Delavari H, Keshtkaran A, Setoudehzadeh F. Catastrophic health expenditures and coping strategies in households with cancer patients in Shiraz Namazi hospital. Middle East J Cancer. 2014;5:13–22. [Google Scholar]
- 20.Hajizadeh M, Nghiem HS. Out-of-pocket expenditures for hospital care in Iran: Who is at risk of incurring catastrophic payments? Int J Health Care Finance Econ. 2011;11:267–85. doi: 10.1007/s10754-011-9099-1. [DOI] [PubMed] [Google Scholar]
- 21.Nouraei Motlagh S, Abolghasem Gorji H, Mahdavi G, Ghaderi H. Main determinants of supplementary health insurance demand: (Case of Iran) Glob J Health Sci. 2015;7:285–94. doi: 10.5539/gjhs.v7n6p285. [DOI] [PMC free article] [PubMed] [Google Scholar]


