Abstract
Background/Aim:
Early diagnosis of chronic illnesses and cancers mainly occurs at primary health care centers (PHCs) by primary health care physicians (PHPs). The incidence of colorectal cancer (CRC) in the Kingdom of Saudi Arabia (KSA) is rising and this has been attributed to many factors. The increasing incidence of CRC is compounded by nonadherence to screening recommendations. Therefore, evaluating PHPs knowledge, attitudes, and practices of screening for CRC is clinically important. We aimed to evaluate the knowledge, attitudes, and practices of PHPs regarding CRC screening and to identify the factors associated with nonadherence of PHPs to screening recommendations.
Materials and Methods:
PHPs working at three tertiary care centers and PHCs across the city of Jeddah were randomly recruited. Participants were surveyed using a comprehensive questionnaire that recorded data on demographics, qualifications, and knowledge of various modalities and guidelines related to CRC screening. Perspectives about effectiveness of, or adherence to, factors that influence physicians' perspectives or recommendations for CRC screening were also assessed. Logistic regression analysis was used to identify physician characteristics associated with PHPs perspectives and nonadherence to CRC screening.
Results:
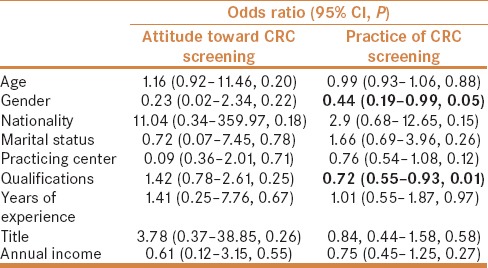
A total of 127 PHPs were recruited. The average age of participants was 34 (±8.4) years, 86.6% were native Saudi's and 56.7% were females. The majority of surveys (66.9%) were completed at 24 PHCs and the remaining at hospital-based family medicine clinics. Most of the PHPs (55%) had a bachelor's degree and 31.5% were board-certified or carried a PhD in family medicine; 95% of participants believed that CRC screening in general was effective, but as much as 55% reported that they did not practice screening. The male physicians [odds ratio (OR) = 0.44, 95% confidence interval (CI) = 0.19–0.99, P = 0.048)] and PHPs with only a bachelor degree or less (OR = 0.72, 95% CI = 0.55–0.93, P = 0.011) were less likely to recommend screening for CRC.
Conclusions:
A considerable proportion of PHPs do not adhere to CRC screening recommendations despite a wide belief that screening is effective. Male PHPs with lower qualifications appear to be less likely to recommend screening.
Keywords: Belief, colorectal cancer, knowledge, primary health care, screening
INTRODUCTION
Colorectal cancer (CRC) is one of the most lethal cancers in the world and it is the third most common cancer in males and the second in females worldwide.[1] Unfortunately, studies have shown that the incidence rate of CRC in the Kingdom of Saudi Arabia (KSA) has increased over the past decade reaching 14.5/100,000 in 2010.[2] This phenomenon is thought to be secondary to increased consumption of red meat and Western diet.[3] The median age of CRC presentation in KSA is estimated to be around 60 and 55 years for men and women, respectively.[2] Moreover, 28.4% of the patients are found to have distant metastasis at the time of presentation.[4]
Screening has been proven to be a beneficial tool for preventing CRC through early identification and removal of premalignant adenomas and thus decreasing related mortality. Studies have shown that screening can lead to a 53% decline in the rate of mortality due to CRC based on data from the United States (US). The US Preventive Services Task Force (USPSTF) guidelines recommend annual screening for CRC high-sensitivity fecal occult blood testing (FOBT), or sigmoidoscopy every 5 years, or full colonoscopy every 10 years for adults between 50 and 75 years old.[5] On the contrary, the Canadian guidelines recommend screening adults aged 60–74 years for CRC with FOBT every 2 years or flexible sigmoidoscopy every 10 years, and recommended against colonoscopy as a routine screening test.[6] The Saudi guidelines recommend offering CRC screening for those above the age of 45 years (strong recommendation; low-quality evidence).[7]
The ideal setting is to initiate screening campaigns at the primary health care level. However, despite the emphasis on the importance of screening, only an estimated 10–50% of the eligible population is being screened.[8,9] Reasons behind the relatively low uptake of screening have been investigated. Some contributing factors related to physicians include lack of physician knowledge and overall attitude toward CRC screening.[10] For example, one survey that included 168 internal medicine residents at four accredited programs in the US identified many misperceptions regarding CRC screening and the utility of the FOBT.[11]
Another study that included 600 primary care physicians stated that the rate of CRC screening was lower than the goal set by the American Cancer Society in 2015. This low uptake was attributed to cost, availability, procedural risks, and lack of proof of effectiveness by surveyed physicians.[12] Moreover, a survey of staff physicians working in three university-affiliated hospitals in Montreal showed that the physicians lacked the knowledge about different modalities and intervals for CRC screening.[1] The two studies demonstrated that most physicians were aware of methods of CRC screening, but have low belief in the effect of screening on CRC occurrence, confusion about how methods of screening are performed, and insufficient information concerning the ages and frequency of screening.[13,14] Similar data specific to the primary health care community in KSA is lacking.
The aim of this study was to assess the attitude, practices, and knowledge of primary health care physicians (PHPs) working at primary health care centers (PHCs) in KSA regarding screening for CRC, and determine the factors that influence adherence to CRC screening from a physician's perspective.
MATERIALS AND METHODS
Study design and participants
We conducted a cross-sectional survey of PHPs through direct interview questionnaires. Target physicians included all physicians practicing at PHCs in Jeddah, KSA regardless of age, gender, nationality, title (intern, resident, specialist, consultant), location of PHC (Clinics affiliated with the Saudi joint program of family medicine, Ministerial PHC Centers, King Abdulaziz University (KAAU) Hospital general clinic, King Fahad General Hospital, King Fahad Military Hospital, National Guard Hospital), or level of training (Bachelor degree of Medicine, Bachelor degree of Surgery (MBBS), Diploma or Masters of Family Medicine or other specialties, Board or PhD of Family Medicine or other specialties). Physicians from all PHCs in the city of Jeddah were approached for participation between October and December 2016. A written informed consent for participation was provided prior to recruitment. This study was approved by KAAU Ethics Committee prior to initiation.
Study questionnaire
An Arabic self-administered questionnaire previously modified and used by Demyati et al.[15] [Supplementary Figure 1 (156.6KB, pdf) ] that included data on participant demographics, level of training, perception, knowledge and attitude toward screening for CRC guidelines, and practice was administered and completed by all participants. Questions were in line with the Centers for Disease Control and Prevention (CDC) and USPSTF guidelines recommendations. To ensure clarity, 10 physicians tested the questionnaire prior to study commencement. At the time of recruitment, members of the research team gave physicians brief instructions on how to complete the questionnaire. Once completed, questionnaires were labeled and collected by the research team. Subsequently, a standard data extraction sheet was used to collect data; then data were entered into an electronic spreadsheet for analysis.
Statistical analysis
We summarized the results using means for continuous variables and frequencies for categorical variables. “Yes” and “No” answers to knowledge and attitude questions were translated into numerical scores, such that “Yes” answer was recorded as “1” and “No” as “0,” then summed separately into total scores of 11 and 8, respectively. Higher scores indicated higher levels of knowledge and attitude. Standard Student's t-test was used to compare means, while Mann–Whitney U-test was used to compare medians. Analysis of variance testing was used to compare means when multiple groups existed. For categorical variables, frequencies were reported and Chi-square test or Fisher's exact test was used where appropriate. Predictors of poor knowledge, attitude, and noncompliance with screening recommendations were evaluated using logistic regression analysis. Simple and multiple linear regression analysis was used to identify predictors of knowledge and attitude scores. Missing data were conservatively managed as low score answers. A P value of 0.05 was considered statistically significant. STATA 11.2 (StataCorp, Texas, USA) statistical software was used.
RESULTS
Physician characteristics
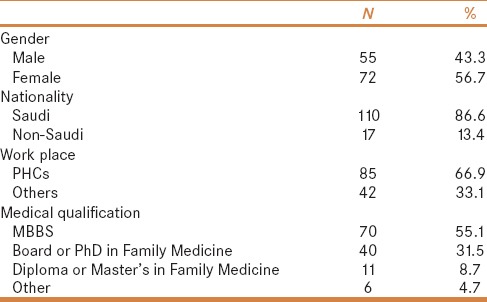
The total number of participants was 127 PHP with mean age of 34 ± 8.49 years, and 127 of 150 (85%) physicians that were approached agreed to participation; 56.7% of PHPs were females and 86.6% were Saudis. Questionnaires were collected at different work places in Jeddah, including 66.9% from ministerial PHCs. Regarding PHPs level of education, 55.12% had a MBBS, 31.5% carried a Board or PhD of Family Medicine, and the remaining were divided between having a Board or PhD of other specialties, Diploma or Master of Family Medicine or of other specialties. The majority of PHPs were residents (66.14%) and 52% reported a work experience ranging between 2 and 10 years [Table 1].
Table 1.
Baseline demographics of 127 primary health care physicians
Knowledge, attitude, and practice of CRC screening
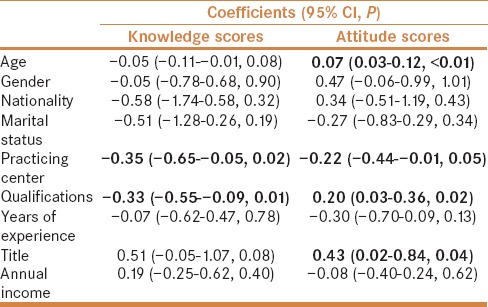
The mean value for the knowledge score was 3.8 ± 2.2. Physicians carrying a board or PhD had higher mean knowledge scores compared to physicians with MBBS only (4.9 ± 2.3 vs. 3.1 ± 1.8, P < 0.01), as did family medicine trained physicians (4.3 ± 2.5 vs. 3.1 ± 1.8, P < 0.01). Physicians who reported preforming CRC screening scored higher on knowledge scores compared to those who reported not practicing CRC screening (4.4 ± 2.3 vs. 3.3 ± 1.9, P < 0.01). Participants who indicated that their decision to follow screening or not was influenced by the USPSTF recommendations scored better on knowledge questions compared to those who were not familiar or not influenced by these recommendations (4.2 ± 2.1 vs. 3.1 ± 1.9 vs. 2.9 ± 2.3, P < 0.01). Similarly, physicians who reported being influenced by American Cancer Society had better knowledge scores than those who were not influenced or those who were not familiar with these guidelines (4.0 ± 2.2 vs. 2.7 ± 1.6 vs. 3.3 ± 2.4, P < 0.01). Physicians influenced by their patients' preference for CRC screening scored higher knowledge score when compared to those who were not influenced and responded as “not applicable” (4.3 ± 2.6 vs. 3.7 ± 1.9 vs. 2.8 ± 1.9, P < 0.01). Having a reminder system like a calendar or electronic system linking patients to date of screening according to their age showed no significant differences with regards to practice (4 ± 1.6 vs. 3.8 ± 2.2, P = 0.75) [Tables 2 and 3]. On multiple linear regression analysis, site of practice (coefficient = −0.35, 95% CI = −0.65, −0.05, P = 0.02), and physician qualifications (coefficient = −0.33, 95% CI = −0.55, −0.09, P = 0.01) significantly predicted knowledge scores [Table 4].
Table 2.
Knowledge, attitude, and practice questionnaire responses of participants stratified according to gender
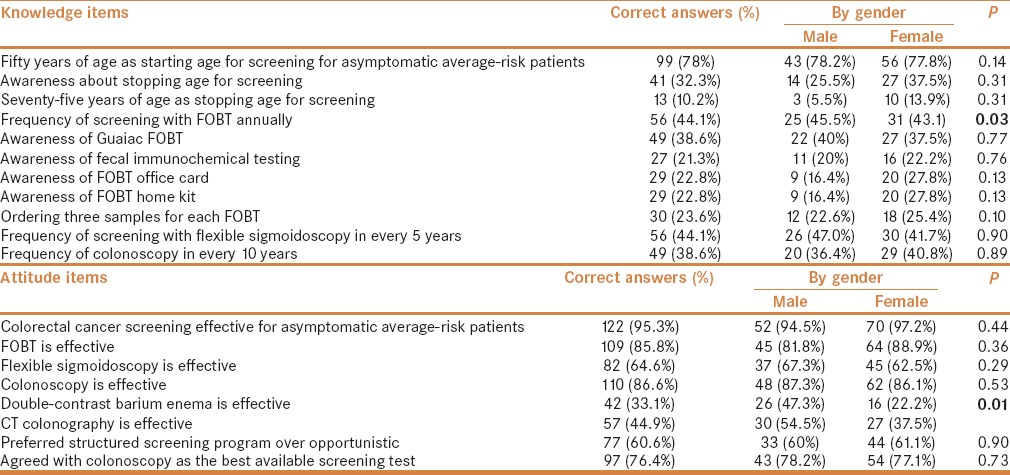
Table 3.
Mean knowledge and attitude item scores
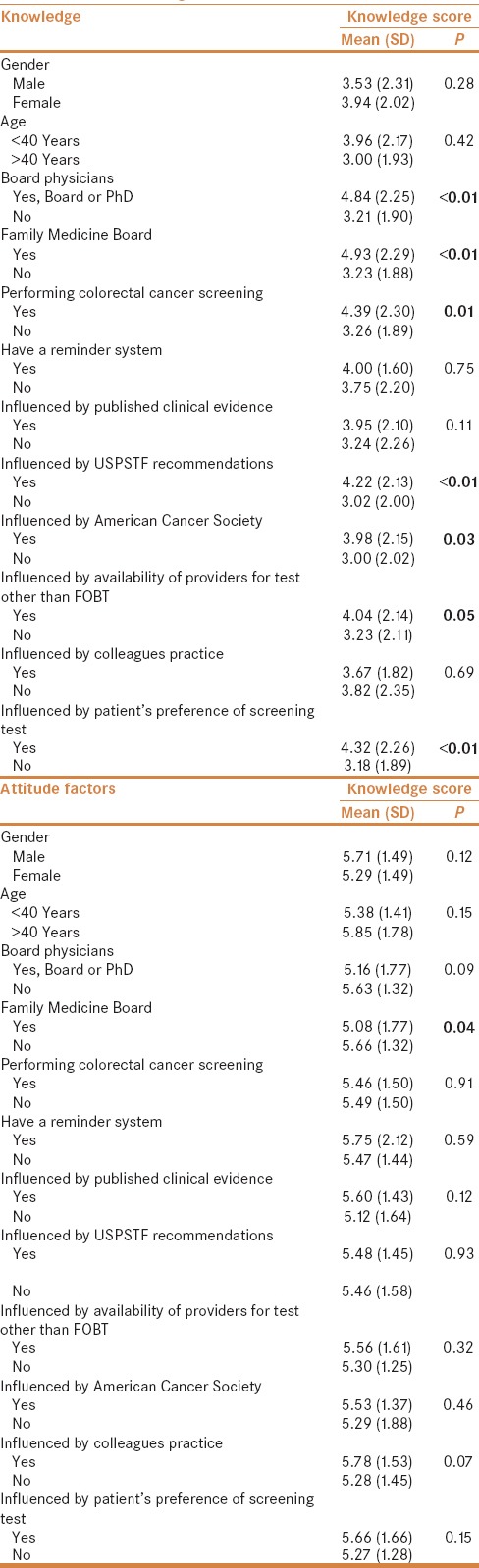
Table 4.
Predictors of knowledge and attitude scores of CRC screening among primary health care physicians based on multiple linear regression analysis
The mean attitude score was 5.5 ± 1.5. Of the 127 participating physicians, 95.3% considered CRC screening for asymptomatic average-risk patients to be effective and 60.6% preferred having a structured screening programs over opportunistic screening. Among screening modalities, colonoscopy was considered effective by 86.6% of PHPs. FOBT was considered effective by 85.8%, and 64.6% reported flexible sigmoidoscopy also to be an effective modality. Computed tomography (CT) colonography was considered an effective strategy by only 44.9%, and 76.4% agreed that colonoscopy was the best available screening test. Family physician who carried a Board or PhD scored lower than those carrying a Diploma or Bachelor's degree (5.1 ± 1.8 vs. 5.5 ± 1.2 vs. 6.3 ± 1.5, P = 0.30). Physicians influenced by published clinical evidence scored better than those not influenced or others who responded as “not applicable” (5.6 ± 1.4 vs. 4.2 ± 1.8 vs. 5.5 ± 1.5, P = 0.03). Although not statistically significant, physicians who reported having a reminder system for CRC screening scored better on attitude questions than those who did not (5.8 ± 2.1 vs. 5.5 ± 1.5, P = 0.59). Attitude scores of female physicians were lower compared to male physicians (5.3 ± 1.5 vs. 5.7 ± 1.5, P = 0.12) [Tables 2 and 3].
On simple linear regression analysis, no correlation was seen between mean knowledge and attitude scores (coefficient = 0.02, 95% CI = −0.10 to 0.14, P = 0.74). However, age (coefficient = 0.07, 95% CI = 0.03–0.12, P < 0.01, i.e., older age meant higher scores), site of practice (coefficient = −0.22, 95% CI = −0.44 to −0.001, P = 0.049, i.e., scores at PHCs and sites affiliated with family medicine joint program were lower compared to tertiary hospitals), qualification level (coefficient = 0.20, 95% CI = 0.03–0.36, P = 0.02, i.e., scores were higher with highly qualified (Board or PHD) compared to MBBS or Diploma holding physicians), and title (coefficient = 0.43, 95% CI = 0.02–0.84, P = 0.04, i.e., consultants scored higher compared to interns and residents) appeared to be significantly associated with attitude toward CRC screening [Table 4].
Predictors of nonadherence to CRC screening recommendations
On logistic regression analysis, none of the studied PHP characteristics appeared to be associated with lack of PHP belief about CRC screening effectiveness. Conversely, male physicians (OR = 0.44, 95% CI = 0.19–0.99, P = 0.05) and PHPs with lower qualifications (OR = 0.72, 95% CI = 0.55–0.93, P = 0.01) were less likely to recommend screening for CRC [Table 5].
Table 5.
Predictors of attitude and practice of CRC screening among PHPs based on multiple logistic regression analysis
DISCUSSION
The role that screening plays in reducing the incidence of CRC is unequivocal, which is why it is imperative to identify barriers to screening for CRC. Such barriers can be related to patients and whether or not they recognize the threat CRC poses on the general population and their level of education about modes of prevention. A recent study by Almadi et al., involving 500 participants, concluded that only 7% of the target population eligible for screening was actually screened, but surprisingly 71% were willing to undergo screening. Willingness to undergo screening was not predicted by any patient characteristics according to regression analysis.[16] As such, local barriers related to physicians involved in screening require examination. A survey by Demyati et al. that surveyed 130 physicians working at a single center in Riyadh reported that 56% of physicians did not practice CRC screening, despite that 95% considered it an effective strategy to detect early CRC.[15] To investigate whether or not those results were specific to one center, we performed a city-wide cross-sectional survey of PHPs in an attempt to identify the degree of physician uptake for CRC screening recommendations and factors that might be influencing physician attitude. Similarly, we found that more than half of the surveyed physicians (55%) did not adhere to CRC screening, despite that 95% thought CRC screening is effective. Factors behind this low rate of uptake warrant further investigation on a national level.
Similar to patients, physician's knowledge of CRC screening guidelines is highly relevant and influential. To better understand why screening for CRC is not being recommended or performed, assessing the knowledge level of PHPs is necessary. According to our results, a large variation in the degree of knowledge of CRC screening exists between physicians practicing in PHCs. Physicians recommending CRC screening clearly demonstrate higher levels of knowledge as judged by mean knowledge scores. Furthermore, physicians with higher qualifications (i.e., more specialized physicians compared to interns or recent graduates) demonstrated higher knowledge scores. Linear regression analysis identified that PHPs practicing at PHC had lower qualifications and had significantly lower scores. These observations not only suggest that physicians practicing at PHCs require more education/orientation about the magnitude of the problem we face with CRC, but to the impact screening might have on reducing this threat. Another concern that can be raised is the standard level placed by institutions at the time of hiring; however, this might be directly related to resource constraints. In the meantime, a national campaign or standardized training program or workshop directed toward educating PHPs about screening methods for CRC is necessary to counteract this obvious deficiency.
The attitude of physicians toward screening and how they perceive recommendations and guidelines is also an area that needs clarification. Based on our analysis, there is no correlation between attitude and knowledge scores (coefficient = 0.02, 95% CI = −0.10 to 0.14, P = 0.74), indicating that attitude toward screening for CRC is likely to be independent of knowledge. On the contrary, statistical analysis identified age (coefficient = 0.07, 95% CI = 0.03–0.12, P < 0.01), site of practice (coefficient = −0.22, 95% CI = −0.44 to −0.001, P = 0.05), qualification level (coefficient = 0.20, 95% CI = 0.03–0.36, P = 0.02), and title (coefficient = 0.43, 95% CI = 0.02–0.84, P = 0.04) as significant predictors of attitude toward CRC screening such that older, more qualified PHPs are more likely to have a positive attitude toward screening. This reinforces the notion that educating younger physicians or even medical students about the importance of preventive medicine is a high priority that results in better attitude toward preventive medicine in the long run. Whether or not this deficiency can be attributed to changes in medical curriculums or teaching strategies cannot be assessed by this study.
We acknowledge that our study is limited by its cross-sectional design and exclusivity of its participant to one city. Performing a more comprehensive study that involves PHPs practicing throughout the kingdom is needed.
CONCLUSIONS
Although a significant proportion of PHPs practicing at PHCs in Jeddah, KSA, consider screening for CRC effective, nonadherence to screening recommendations remains a problem that could be related to physician characteristics. Strategies targeting less qualified male PHPs are required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sewitch MJ, Burtin P, Dawes M, Yaffe M, Snell L, Roper M, et al. Colorectal cancer screening: Physicians' knowledge of risk assessment and guidelines, practice, and description of barriers and facilitators. Can J Gastroenterol. 2006;20:713–8. doi: 10.1155/2006/609746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mosli MH, Al-Ahwal MS. Colorectal cancer in the Kingdom of Saudi Arabia: Need for screening. Asian Pac J Cancer Prev. 2012;13:3809–13. doi: 10.7314/apjcp.2012.13.8.3809. [DOI] [PubMed] [Google Scholar]
- 3.Di Maso M, Talamini R, Bosetti C, Montella M, Zucchetto A, Libra M, et al. Red meat and cancer risk in a network of case-control studies focusing on cooking practices. Ann Oncol. 2013;24:3107–12. doi: 10.1093/annonc/mdt392. [DOI] [PubMed] [Google Scholar]
- 4.Alsanea N, Abduljabbar AS, Alhomoud S, Ashari LH, Hibbert D, Bazarbashi S. Colorectal cancer in Saudi Arabia: Incidence, survival, demographics and implications for national policies. Ann Saudi Med. 2015;35:196–202. doi: 10.5144/0256-4947.2015.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Guide to Clinical Preventive Services 2014: Recommendations of the US Preventive Services Task Force. Rockville (MD): 2014. [Last accessed 2016 Nov 12]. Available from: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/clinicians-providers/guidelines-recommendations/guide/cpsguide.pdf . [Google Scholar]
- 6.Canadian Task Force on Preventive Health C. Bacchus CM, Dunfield L, Gorber Sc, Holmes NM, Birtwhistle R, et al. Recommendations on screening for colorectal cancer in primary care. CMAJ. 2016;188:340–8. doi: 10.1503/cmaj.151125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alsanea N, Almadi MA, Abduljabbar AS, Alhomoud S, Alshaban TA, Nooh R, et al. National Guidelines for Colorectal Cancer Screening in Saudi Arabia with strength of recommendations and quality of evidence. Ann Saudi Med. 2015;35:189–95. doi: 10.5144/0256-4947.2015.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levenson D. CDC says colorectal cancer screening rates remain low. Rep Med Guidel Outcomes Res. 2003;14:10,12. [PubMed] [Google Scholar]
- 9.Chao A, Connell CJ, Cokkinides V, Jacobs EJ, Calle EE, Thun MJ. Underuse of screening sigmoidoscopy and colonoscopy in a large cohort of US adults. Am J Public Health. 2004;94:1775–81. doi: 10.2105/ajph.94.10.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gennarelli M, Jandorf L, Cromwell C, Valdimarsdottir H, Redd W, Itzkowitz S. Barriers to colorectal cancer screening: Inadequate knowledge by physicians. Mt Sinai J Med. 2005;72:36–44. [PubMed] [Google Scholar]
- 11.Sharma VK, Corder FA, Raufman JP, Sharma P, Fennerty MB, Howden CW. Survey of internal medicine residents' use of the fecal occult blood test and their understanding of colorectal cancer screening and surveillance. Am J Gastroenterol. 2000;95:2068–73. doi: 10.1111/j.1572-0241.2000.02229.x. [DOI] [PubMed] [Google Scholar]
- 12.Taylor ML, Anderson R. Colorectal cancer screening: Physician attitudes and practices. WMJ. 2002;101:39–43. [PubMed] [Google Scholar]
- 13.Sahin MK, Aker S. Family physicians' knowledge, attitudes, and practices toward colorectal cancer screening. J Cancer Educ. 2016 doi: 10.1007/s13187-016-1047-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Akerman S, Aronson SL, Cerulli MA, Akerman M, Sultan K. Resident knowledge of colorectal cancer screening assessed by web-based survey. J Clin Med Res. 2014;6:120–6. doi: 10.14740/jocmr1610w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Demyati E. Knowledge, attitude, practice, and perceived barriers of colorectal cancer screening among family physicians in national guard health affairs, Riyadh. Int J Family Med. 2014;2014:457354. doi: 10.1155/2014/457354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almadi MA, Mosli MH, Bohlega MS, Al Essa MA, Al Dohan MS, AlSagri TY, et al. Effect of public knowledge, attitudes, and behavior on willingness to undergo colorectal cancer screening using the health belief model. Saudi J Gastroenterol. 2015;21:71–7. doi: 10.4103/1319-3767.153814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


