Abstract
Background
Childhood physical abuse is a major public health issue with negative consequences to health and well-being manifested in childhood and adolescence, and persisting into adulthood. Yet much childhood physical abuse is not identified when it occurs and little is known about how to screen for it.
Methods
To address this gap, the effectiveness of four modes of administration of screens to identify childhood physical abuse were compared in a sample of 506 adolescents and young adults ages 12 – 24 years seeking general health services at a primary care clinic. Comparisons were made between paper and pencil screen, Audio Computer Assisted Self Interview (ACASI) screen, face to face structured screen (all three utilizing the same measure), and face to face unstructured interview.
Results
Overall, 44.5% of the sample disclosed that they had been physically abused. When compared to paper and pencil screen, the odds of reporting physical abuse was 1.5 (95%CI: 0.92, 2.58) and 4.3 (95%CI: 2.49, 7.43) higher among participants using face-to-face structured screen and face-to-face unstructured interview methods, respectively. The face-to-face unstructured interview identified significantly higher reports than the paper and pencil screen.
Conclusions
While the unstructured interview was the most effective mode for screening for childhood physical abuse, additional research is needed to confirm whether this holds true in other health care settings. Further research should examine how a health provider’s training, experience, and comfort level might influence the identification of physical abuse disclosure in primary care settings using face to face unstructured interview.
Keywords: Screens, Childhood Physical Abuse, Adolescent, Young Adult, Modes of Administration
Introduction
Childhood physical abuse is a major public health issue with tremendous emotional and financial burden.1 Though much abuse goes unreported2 the number of reported cases among children and adolescents nationally is high: in 2013 there were 3.5 million reports of child maltreatment involving 6.4 million children of which 18% were for physical abuse.3
Childhood physical abuse has both short and long-term negative consequences which affect all aspects of functioning throughout the victim’s life course.2,4,5 In adolescents, the problems associated with abuse include teen pregnancy,6 high stress, poor self-esteem, cigarette smoking, drug and alcohol abuse,7,8 and depression and suicidality.9 These negative effects can be diminished through treatment interventions if the abuse is identified by a health care provider.1,2,10,11 While most victims do not spontaneously disclose a history of childhood physical abuse, they are likely to disclose if asked in a medical setting as part of a comprehensive health history.12,13,14 Unfortunately most health care providers do not ask about abuse when there are no obvious signs or symptoms, as is most commonly the case.15 Though very few studies have focused on understanding why providers do not assess for childhood abuse,16 there is evidence that they feel ill-prepared and lack the knowledge of effective methods for identification.18, 17
A number of modes of administration of screens have been used to identify a history of childhood abuse including paper and pencil questionnaires, interviewer conducted questionnaires, computer assisted questionnaires, and face to face interviews.18 Each has its merits. The paper and pencil questionnaire is easy to administer but depends on the reader understanding and correctly interpreting questions.19 In contrast the Audio Computer Assisted Self Interview (ACASI) has an audio component which speaks the questions to the participant and does not require the same level of reading skills.22 Structured screens, such as the Childhood Maltreatment Interview Schedule-Short Form (CMIS-SF)20 or the Computer Assisted Maltreatment Inventory (CAMI)21 use a defined set of questions. In contrast, the face to face unstructured interview allows the give and take of a conversation22,23 allowing the interviewer to probe. Thus, an experience of physical punishment that a participant might initially define as non-abusive might upon further probing become re-defined as abuse. ACASI, which has not previously been studied in childhood abuse per se, has been found to be more effective than other modes of inquiry in research on highly sensitive issues in adolescents and young adults,24,,25,26,27,28,29 as it has also been shown to enhance the participants’ sense of privacy and to reduce the influence of social desirability in shaping participants’ responses.30
Our aim was to compare the effectiveness of four modes of administration of screens – paper and pencil screen, ACASI screen, face to face structured screen, and face to face unstructured interview – to identify a history of childhood physical abuse, during a clinical visit.
Research Design and Methods
Study Population
The study sample was recruited from English speaking youth ages 12 to 24 years, seeking general health services, between December 5, 2005 and April 13, 2007, at a New York City primary care clinic specifically designed for young people. A total of 532 young people were screened for history of childhood physical abuse.
Study Recruitment
Institutional Review Board approval was obtained from the Icahn School of Medicine at Mount Sinai along with a waiver of parental consent to allow consent from adolescents under age 18. A certificate of confidentiality was obtained to protect participants’ privacy.
While waiting to see their medical provider, patients were approached by a research assistant who described the project as a confidential study on how to best take a psychosocial history from young people. Patients were told that they could decide against participation at any time without this affecting their care. Those with difficulty understanding the study materials and consent form were not enrolled. No formal sampling or selection protocol was used. Patients who agreed to participate, once consented, were randomized within clinician and non-clinician arms to one of four modes of administration of screens to identify a history of childhood physical abuse. Participants received two movie tickets upon completion of all the study instruments. Safety protocols were put in place to ensure an immediate assessment for any participant who disclosed childhood abuse or suicidality. For those under 18 years who disclosed abuse, child protection reporting protocols were followed.
Study Randomization
The study was limited by the fact that only one clinician was assigned to conduct the two face-to-face screening groups. Therefore, random allocation was stratified based on clinician's availability. When the clinician was not available, participants were randomized to paper and pencil screen versus ACASI screen and when the clinician was available participants were randomized to face to face structured screen versus face to face unstructured interview.
Outcome
The study outcome was self-reported history of childhood physical abuse occurring before 17 years of age disclosed during any of the three structured screening methods (paper and pencil, ACASI or face to face structured screens) or a face to face unstructured interview. The outcome was specified as childhood physical abuse or no childhood physical abuse regardless of the screening method used. For all three structured methods, childhood physical abuse was identified using the Childhood Maltreatment Interview Schedule-Short Form (CMIS-SF) (see Appendix) modified to better fit the speech used by the study population.
Predictors
Once participants completed the history of childhood abuse using one of the four randomly assigned modes of administration of childhood abuse screens, the participants completed a demographic questionnaire and the Beck Depression Inventory for Primary Care-Fast Screen (BDI-FS)31 using ACASI.
The primary predictor of interest is the mode of screening to identify a history of childhood physical abuse. The following covariates: age, gender, race, ethnicity, zip code, nativity status (immigration status), last grade completed, school enrollment status, school performance, and living arrangement most of the time within the last year) were considered as potential confounders and were adjusted for in the statistical model.
Statistical Analysis
The statistical analysis was conducted by Viswanathan Shankar, DrPH. The distribution of socio-demographic variables was presented as frequencies and percentages and bivariate associations were examined using the Pearson chi-square statistics.
Approximately, five percent of the covariates had missing information, thus we modeled the data both as complete case data (n=506) and as a multiply imputed data (532 × 10 dataset). Multiple imputation was done using fully conditional specification methods which is a flexible imputation procedure that models incomplete variables by a set of conditional densities using different regression procedure. Ten imputation datasets were created with 200 burn in iterations under the missing at random (MAR) assumptions.
Multivariable logistic regression models were fitted to examine the effect among the modes of administration and physical abuse status after adjusting for potential confounders for both complete case and multiple imputation data. Potential covariates that were associated with the outcome at 20% level were selected for final models.
All analyses were performed using SAS software 9.4.32
Results
The distribution of participant characteristics by study arms (modes of screen) are presented in table 1. Over half of the participants were age 18 and older (52.2%). Most were female (85.3%), Hispanic/Latino or black (93.3%), and almost a third resided in Harlem (32.7%). The majority were U.S. born (81.6%), currently in school (79.5%) and most had graduated from high school or were still in school at the right grade for their age (88.3%). More than a quarter of participants (27.2%) were found to have depression on the BDI-SF. Sixty-seven (12.9%) of the 520 research participants disclosed suicidal thoughts within the last two weeks via the BDI-FS. None of these 67 participants were determined to be actively suicidal.
Table 1.
Distribution of study participant characteristics of study participants’ by modes of administration of screens to identify childhood abuse:
| Methods | |||||
|---|---|---|---|---|---|
|
| |||||
| Characteristics | Paper & Pencil N(%) |
ACASI N (%) |
Face to Face Structured N(%) |
Face to Face Unstructured N(%) |
P Value |
| 174 (32.7) | 138 (25.9) | 108 (20.3) | 112 (21.1) | ||
| Demographics | |||||
| Age** | |||||
| 14 and younger | 12(6.9) | 5(3.6) | 12(11.1) | 16(14.3) | 0.0010 |
| 15–17 | 74 (42.5) | 44 (31.9) | 39 (36.1) | 53 (47.3) | |
| 18 and older | 88 (50.6) | 89 (64.5) | 57 (52.8) | 43 (38.4) | |
| Gender | |||||
| Females | 151 (86.8) | 11((86.2) | 97 (89.8) | 87 (77.7) | 0.2584 |
| Males | 23 (13.2) | 19 (13.8) | 11 (10.2) | 25 (22.3) | |
| Race | |||||
| Hispanic/Latin | 88 (50.6) | 68 (49.3) | 62 (57.4) | 62 (55.4) | |
| Black | 70 (40.2) | 61 (44.2) | 42 (38.9) | 44 (39.3) | 0.5375 |
| Asian or white | 16 (9.2) | 9 (6.5) | 4 (3.7) | 6 (5.4) | |
| Borough | |||||
| Bronx | |||||
| South Bronx | 23 (13.32) | 19 (13.8) | 15 (13.9) | 14 (12.5) | 0.2734 |
| Other Bronx | 33 (19) | 17 (12.3) | 13 (12.)) | 17 (15.2) | |
| Brooklyn | 13 (7.5) | 20 (14.5) | 9 (8.3) | 5 (4.5) | |
| Manhattan | |||||
| Central and East Harlem | 54 (31.0) | 51 (36.9) | 37 (34.3) | 32 (28.6) | |
| Other Manhattan | 35 (20.1) | 21 (15.2) | 23 (21.3) | 27 (24.1) | |
| Queens | 12 (6.9) | 7 (5.1) | 9 (8.3) | 15 (13.4) | |
| Other | 4 (2.3) | 3 (2.2) | 2 (1.9) | 2 (1.8) | |
|
| |||||
| Nativity Status | |||||
| US | 141 (81.3) | 112 (81.2) | 82 (75.9) | 99(88.4) | 0.1214 |
|
| |||||
| Last grade Completed* | |||||
| Eight or lower | 17 (9.8) | 9 (6.5) | 16 (14.8) | 16 (14.3) | 0.0327 |
| Ninth | 23 (13.2) | 18 (13.0) | 10 (9.3) | 21 (18.8) | |
| Tenth | 17 (9.8) | 17 (12.3) | 13 (12.0) | 23 (20.5) | |
| Eleventh | 40 (22.9) | 22 (15.9) | 20 (18.5) | 19 (17.0) | |
| Twelfth | 34 (19.5) | 29 (21.0) | 17 (15.7) | 13 (11.6) | |
| Some/completed college | 43 (24.7) | 43 (31.6) | 32 (29.6) | 20 (17.8) | |
|
| |||||
| Education Status | |||||
| Dropped out | 10 (5.8) | 9 (6.5) | 8 (7.4) | 3 (2.7) | |
| Currently in k – 12th grade but left behind | 10 (5.8) | 9 (6.5) | 5 (4.6) | 8 (7.4) | |
| Graduated HS or currently in K-12th grade and on track | 154 (88.5) | 120 (86.9) | 95 (87.9)) | 101 (90.2) | |
|
| |||||
| Living Arrangement for the Last year | 0.2877 | ||||
| Both parents | 42 (24.1) | 27 (19.6) | 21 (19.4) | 27 (24.1) | |
| One parent & step | 24 (13.8) | 14 (10.1) | 17 (15.7) | 14 (12.5) | |
| Single parent no other adults | 50 (28.7) | 46 (33.3) | 47 (43.5) | 41 (36.6) | |
| Single parent and other adults | 25 (14.4) | 20 (14.5) | 11 (10.2) | 15 (13.4) | |
| Other family member, foster care, group home | 33 (18.9) | 31 (22.5) | 12 (11.1) | 15 (13.4) | |
|
| |||||
| Depression* | |||||
| None | 116 (66.7) | 89 (64.5)) | 80 (74.1) | 88 (78.6) | 0.0877* |
| Any depression | 47 (27.0) | 44 (31.9) | 28 (25.9) | 20 (17.9) | |
| Missing | 11 (6.3) | 5 (3.6) | 0 | 4 (3.6) | |
|
| |||||
| Suicidal Ideation | |||||
| Yes | 21 (12.5) | 16 (11.8) | 18 (16.7) | 12 (11.1) | 0.6035 |
| No | 147 (84.5) | 120 (86.9) | 90 (83.3) | 96 (85.7) | |
| Missing | 6 (3.5) | 2 (1.5) | 0 | 4 (3.6) | |
based on complete case analysis
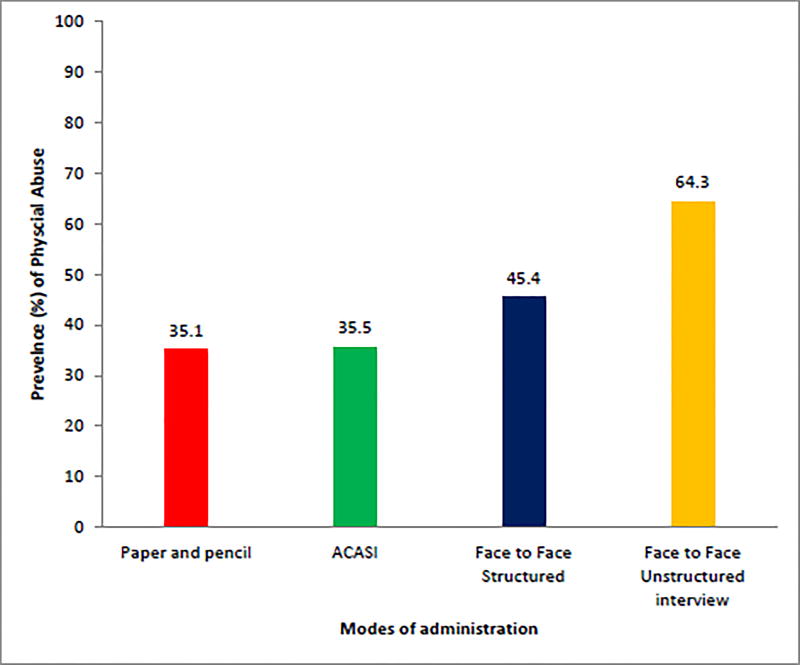
The distribution of characteristics of the total sample was similar across the methods of administration with the exception of age, last grade of education completed and depression. The prevalence of child physical abuse reported under each screening mode is presented in figure 1. Overall, 43.4% of participants disclosed childhood physical abuse. The face to face unstructured interview identified higher percentages of abuse (66.3%), followed by face to face structured screen (45.4%), ACASI (35.5%) and paper and pencil (35.1%) and was significantly different (p value <0.0001).
Figure 1.
prevalence of child physical abuse reported under each screening mode
Childhood physical abuse was not associated with the selected covariates in the study population with the exception of depression (Table 2). Participants who reported childhood physical abuse showed positive association with depression, with 31% depression in those who had physical abuse compared to 23% in those who did not (p=0.0380)
Table 2.
Distribution of participant characteristics by physical abuse
| Characteristics | No physical abuse 301 (56.6) |
Physical abuse 231 (43.4) |
P Value * |
|---|---|---|---|
|
| |||
| N(%) | N(%) | ||
| Mode | |||
| Paper and pencil | 113 (37.5) | 61(26.4) | |
| ACASI | 89 (29.6) | 49 (21.2) | <0.0001 |
| Face to Face Structured | 59 (19.6) | 49 (21.2) | |
| Face to Face Unstructured interview | 40 (13.2) | 72 (31.2) | |
|
| |||
| Age | |||
| 14 and younger | 29 (9.6) | 16 (6.9) | 0.4259 |
| 15–17 | 121 (40.2) | 89 (38.5) | |
| 18 and older | 151 (50.2) | 126 (54.6) | |
|
| |||
| Gender | |||
| Females | 259 (86.1) | 199 (86.2) | 0.9735 |
| Males | 42 (13.9) | 32 (13.9) | |
|
| |||
| Race | |||
| Hispanic/Latin | 160 (53.6) | 120 (51.9) | 0.6133 |
| Black | 124 (41.2) | 93 (40.3) | |
| Asian or white | 17 (5.7) | 18 (7.8)) | |
|
| |||
| Borough | |||
| Bronx | |||
| South Bronx | 41 (13.6) | 30 (12.9) | 0.0788 |
| Other Bronx | 44 (14.6) | 36 (15.5) | |
| Brooklyn | 24 (7.9) | 23 (9.9) | |
| Manhattan | |||
| Central and East Harlem | 111 (36.8) | 63 (27.3) | |
| Other Manhattan | 58 (19.3) | 48 (20.8) | |
| Queens | 16 (5.3) | 27 (11.7 | |
| Other | 7 (2.3) | 4 (1.7) | |
|
| |||
| Nativity Status | |||
| US | 253 | 181 (78.4) | 0.09029 |
|
| |||
| Last grade Completed | |||
| Eight or lower | 39 (12.9) | 19 (8.2) | 0.2204 |
| Ninth | 42 (13.9) | 30 (12.9) | |
| Tenth | 42 (13.9) | 28 (12.1) | |
| Eleventh | 54 (17.9) | 47 (20.4) | |
| Twelfth | 56 (18.6) | 37 (16.0) | |
| Some/completed college | 68 (22.6) | 70 (30.3) | |
|
| |||
| Education Status | |||
| Dropped out | 18 (5.9) | 12 (5.1) | 0.7141 |
| Currently in k – 12th grade but left behind | 20 (6.6) | 12 (5.2) | |
| Graduated HS or currently in K-12th grade and on track | 263 (87.4) | 207 (89.6) | |
|
| |||
| Living Arrangement for the Last year | |||
| Both parents | 69 (22.9) | 48 (20.8) | 0.4885 |
| One parent & step | 35 (11.6) | 34 (14.7) | |
| Single parent no other adults | 98 (32.6) | 86 (37.2) | |
| Single parent and other adults | 43 (14.3) | 28 (12.1) | |
| Other family member, Foster care, group home | 56 (18.6) | 35 (15.1) | |
|
| |||
| Depression | |||
| None | 218 (72.4) | 155 (67.1) | 0.0380 |
| Any depression | 67 (22.3) | 72 (31.3) | |
| Missing | 16 (5.3) | 4 (1.7) | |
|
| |||
| Suicidal Ideation | |||
| Yes | 31 (10.3) | 36 (15.6) | 0.0806 |
| No | 261 (86.7) | 192 (83.1) | |
| Missing | 9 (2.9) | 3 (1.3) | |
based on complete case analysis
We examined the effect of different screening modes to identify child physical abuse, our multivariable model adjusting for potential confounders showed that in both types of face-face interviews, the participants were more likely to report abuse. Specifically in complete case models, the estimated odds of identifying (being reported) child physical abuse is 4.3 times more in the unstructured face- to- face interviews with more probes compared to the paper and pencil screens, as shown in table 3. Similarly, the estimated odds of child physical abuse reported under structured interview was 1.5 times more compared to paper and pencil screen though the effect was not statistically different. Multiple imputation results show similar results to the complete case but the confidence intervals were a bit tighter interval and the structured face to face interview shows a marginal significance.
Table 3.
Adjusted odds ratios, 95% confident intervals and P value of the relationship of mode of administration of screens to identify childhood physical abuse and proportion of childhood abuse: Complete case and Multiple imputation model
| Exposure | Complete case model (N=512) |
P value | Multiple imputation model (N=532 × 10) |
P Value |
|---|---|---|---|---|
| Mode of Administration | ||||
| Paper & Pencil | 1.0 | 1.0 | ||
| ACASI | 1.02 (0.63, 1.67) | 0.9297 | 0.99 (0.61– 1.61) | 0.9781 |
| Structured face to face | 1.53 (0.92, 2.58) | 0.1029 | 1.58 (0.95–2.65) | 0.0779 |
| Unstructured face to face | 4.30 (2.49, 7.43) | <0.0001 | 4.16 (2.45–7.08) | <0.0001 |
Final model was adjusted by age, gender, race/ethnicity, depression, living arrangement and last grade completed in both complete case and imputation model.
Discussion
The prevalence of childhood physical abuse identified by the face to face unstructured interview was four and one half times that of paper and pencil screen, significantly more than all three structured modes of administration. The interviewer who conducted the face to face interviews was a very experienced physician with an expertise in childhood abuse assessment which may account for some of this difference. Another possible contributor is the fact that the face to face unstructured interview allows further probing.
Only one prior study, by DiLillo and colleagues, has compared different modes of administration of screens to identify a history of both childhood physical abuse, comparing three modes (paper and pencil questionnaire, computer assisted survey and face to face structured interview), in a sample of female college students.33 The DeLillo study reported an overall prevalence of childhood physical abuse of 15.5% but concluded that the mode of administration was unrelated to disclosure of a history of childhood physical abuse (X2=1.1; p value = 0.58). The present study found prevalence that was more than twice that; 38.6% vs. 15.5%, despite the latter asking about a history of childhood abuse that occurred before age 18 years and the present study using age 17 years as the cutoff. The large difference in prevalence between the two studies when comparing the structured modes of screening is most likely to be explained by differences between the study populations: the former sampled female students, in a college setting; an overwhelmingly white and middle class group. In contrast, the present study sampled males and females ages 12–24 years, who were 53% Hispanic and 41% non-Hispanic black, recruited from an urban poor population.
The two studies used two different measures to identify physical abuse: The former used the CAMI and the present study used the CMIS-SF, but it is unlikely that the difference in the instruments used in each study accounts for the large difference in prevalence, as both measures utilize detailed and behaviorally specific questions which is considered to be the most effective type of screen.42,34 The inclusion of the face to face unstructured interview as a fourth mode of administration in the present study is likely to account for the fact that when looking at overall prevalence of childhood physical abuse in this study, we see a prevalence triple that of DiLillo (44.5% vs. 15.5%).
The present study has some limitations. The retrospective, self-report has been found in some history of childhood physical abuse research to be somewhat unreliable due to error in recall resulting in false positives and false negatives.35 Some researchers suggest that official child protective service reports and self-report used together should be the gold standard36 but, this is not practical for studies in most settings where official childhood abuse records are not available. More important, a significant proportion – perhaps even a majority – of childhood abuse cases go unreported, so studies using only verified reported cases are likely to undercount.1,2,24, Indeed, a number of studies have shown that retrospective self-report has shown high stability over time.37
Having one sole clinician for the administration of the unstructured interview rather than a number of clinicians with different levels of experience and comfort, an approach taken to reduce the influence of clinician variability on disclosure, limits the generalizability of the findings.
Conclusion
Although research on how best to identify childhood physical abuse history is in its infancy, this study suggests that face to face methods may offer the most effective ways to screen young people in primary care settings. However, because health care providers are not routinely inquiring about it, we need to better understand the trajectory from suspicion of abuse to the reporting of it in the primary care setting18.19. While the present study tells us nothing about how health provider training, experience, competency and comfort level influence the willingness to inquire about abuse, it does underline the need for further lines of research inquiry.
The effectiveness of a given mode of administration of screens to identify childhood abuse should not be confused with its practical application in the clinical setting. Health care providers in primary care practice settings face significant time pressures38 and therefore, we need to examine whether face to face modes are the most labor intensive and time consuming compared to computer and paper or pencil questionnaires. Furthermore although computer technology is increasingly shaping health care, it is unclear how we will see the adoption of computer based screening for a range of health issues.39 Computer based methods for communication between patient and health care provider still present significant challenges for primary care settings where they are not yet seen as practical.40 Finding the screening method to identify childhood abuse that will prove to be most practical in the primary health care environment, where the use of technology is ever evolving, is a complex issue. Which mode of screening is most practical in the health care setting remains an open question.
Appendix
Modified Childhood Maltreatment Interview Schedule-Short Form (mCMIS-SF)
| Structured interviews: |
| Before you were 17 years of age (Each question had answer choices of “Yes” or “No): |
| 1. a parent or guardian ever do something to you on purpose (for example, hit or punch or cut you, or push you down) that made you bleed or gave you bruises or scratches |
| 2. Did, or that broke bones or teeth?” |
| 3. Did either of your parents or guardians get so mad at you that they hurt you physically? |
| 4. Did either of your parents or guardians use physical punishment for discipline? |
| Face to face unstructured interview method: |
| 1. How do your parents or guardians discipline you? |
| 2. Do they ever physically hit you? |
| 3. How do they punish you? |
| 4. Further probing was done depending on the responses to the questions: : having been hit, punched, kicked, or otherwise struck or pushed down; cut, bruised, made to bleed, scratched, having broken bones, broken teeth, or having been hurt physically |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors confirm that the manuscript is original research that has not been published and is not under consideration elsewhere. The authors confirm that all of the authors participated in the preparation of the manuscript. The authors confirm that we have permission to reprint any figures or tables that were initially printed elsewhere.
Contributor Information
Angela Diaz, Department of Pediatrics and Department of Environmental Medicine and Public Health, Icahn School of Medicine at Mount Sinai, Address: 320 East 94th Street, New York, New York, 10128, USA. Phone: 212 423 2900.
Ken Peake, Icahn School of Medicine at Mount Sinai, New York, NY.
Anne Nucci-Sacks, Icahn School of Medicine at Mount Sinai, New York, NY.
Viswanathan Shankar, Albert Einstein College of Medicine, Bronx, NY.
References
- 1.Institute of Medicine. Institute of Medicine; National Research Council. New Directions in Child Abuse and Neglect Research. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 2.Diaz A, Petersen AC. Institute of Medicine Report: New Directions in Child Abuse and Neglect Research. JAMA Pediatrics. 2014;168(2):101–2. doi: 10.1001/jamapediatrics.2013.4560. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services, Children’s Bureau, Child Maltreatment. [Accessed November 11, 2016];2013 at http://www.acf.hhs.gov/sites/default/files/cb/cm2013.pdf.
- 4.Anda RF, Felitti VJ, Walker JW, et al. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry & Clinical Neurosciences. 2006;56(3):174–86. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkowitz CD. The long-term medical consequences of sexual abuse. In: Reece RM, editor. Treatment of child abuse: Common Ground for Mental Health, Medical, and Legal Practitioners. Baltimore, MD: Johns Hopkins University Press; 2000. pp. 54–64. [Google Scholar]
- 6.Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial outcomes, and fetal death. Pediatrics. 2004;113(2):320–7. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- 7.Diaz A, Simantov EY, Rickert V. Effect of abuse on health: Results of a national survey. Archives Pediatric & Adolescent Medicine. 2002;156(8):811–17. doi: 10.1001/archpedi.156.8.811. [DOI] [PubMed] [Google Scholar]
- 8.Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health. 2006;38(4):444e1–e10. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Brown J, Cohen P, Johnson J, Smailes E. Child abuse and neglect: Specificity of effects on adolescent and young adult depression and suicidality. Child Abuse & Neglect. 1999;38(12):1490–96. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JA, Mannarino AP, Berliner L, Deblinger E. Trauma-focused cognitive behavioral therapy for children and adolescents: An empirical update. Journal of Interpersonal Violence. 2000;15(11):1202–23. [Google Scholar]
- 11.Bisson JI, Ehlers A, Matthews R, Piling S, Richards D, Turner S. Psychological treatment for chronic post-traumatic stress disorder: Systematic review and meta-analysis. The British Journal of Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- 12.Battaglia TA, Finley E, Liebschutz JM. Victims of intimate partner violence speak out: Trust in the patient-provider relationship. Journal of General Internal Medicine. 2003;18(8):617–23. doi: 10.1046/j.1525-1497.2003.21013.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diaz A, Manigat N. The health care provider role in the disclosure of sexual abuse: The medical interview as a gateway to disclosure. Children's Health Care. 1999;28:141–9. [PubMed] [Google Scholar]
- 14.Diaz A, Edwards S, Neal W, Ludmer P, Sondike SB, Kessler C. Obtaining a history of sexual victimization among adolescent females seeking routine health care. Mount Sinai Journal of Medicine. 2004;71(3):170–3. [PubMed] [Google Scholar]
- 15.Leder MR, Emans SJ, Hafler JP, Rappaport LA. Addressing sexual abuse in the primary care setting. Pediatrics. 1999;104(2):270–5. doi: 10.1542/peds.104.2.270. [DOI] [PubMed] [Google Scholar]
- 16.Weinreb L, Fletcher K, Candib L, Bacigalupe G. Physicians' perceptions of adult patients' history of child abuse in family medicine settings. Journal of the American Board of Family Medicine. 2007;20(4):417–9. doi: 10.3122/jabfm.2007.04.060208. [DOI] [PubMed] [Google Scholar]
- 17.Lane WG, Dubowitz H. Primary care pediatricians' experience, comfort and competence in the evaluation and management of child maltreatment: Do we need child abuse experts? Child Abuse & Neglect. 2009;33(2):76–83. doi: 10.1016/j.chiabu.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Abbey A, Zawacki T, Buck PO, Clinton AM, McAuslan P. Sexual assault and alcohol consumption: What do we know about their relationship and what types of research are still needed? Aggression & Violent Behavior. 2000;9(3):271–303. doi: 10.1016/S1359-1789(03)00011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self-interview and face to face interview modes in assessing response bias among STD clinic patients. Sexually Transmitted Infections. 2005;81(5):421–5. doi: 10.1136/sti.2004.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Briere J. Childhood Maltreatment Interview Schedule Short Form. [Accessed November 11, 2016];Adapted from the full CMIS, published as an appendix in J Briere, Child abuse trauma: Theory and treatment of the lasting effects. 1992 at http://www.johnbriere.com/cmis.htm.
- 21.DiLillo D, Hayes-Skelton SA, Fortier MA, Perry AR, Evans SE, Messman Moore TL, Walsh K, Nash C, Fauchier A. Development and initial psychometric properties of the Computer Assisted Maltreatment Inventory (CAMI): A comprehensive self-report measure of child maltreatment history. Child Abuse & Neglect. 2010;34(5):305–17. doi: 10.1016/j.chiabu.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 22.Bryman A. Integrating quantitative and qualitative research: How is it done? Qualitative Research. 2006;6(1):97–113. [Google Scholar]
- 23.Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage Publications Inc.; 2002. [Google Scholar]
- 24.Dolezal C, Marhefka SL, Santamaria EK, Leu CS, Brackis-Cott E, Mellins CA. A comparison of audio computer-assisted self-interviews to face-to-face interviews of sexual behavior among perinatally HIV-exposed youth. Archives of Sexual Behavior. 2012;41(2):401–10. doi: 10.1007/s10508-011-9769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurth AE, Martin DP, Golden MR, et al. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sexually Transmitted Diseases. 2004;31(12):719–26. doi: 10.1097/01.olq.0000145855.36181.13. [DOI] [PubMed] [Google Scholar]
- 26.Reddy MK, Fleming MT, Howells NL, Rabenhorst MM, Casselman R, Rosenbaum A. Effects of method on participants and disclosure rates in research on sensitive topics. Violence and Victims. 2006;21(4):499–506. [PubMed] [Google Scholar]
- 27.Tourangeau R, Smith TW. Asking sensitive questions: The impact of data collection mode, question format, and question context. Public Opinion Quarterly. 1996;60:275–304. [Google Scholar]
- 28.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck IH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 29.Williams ML, Freeman RC, Bowen AM, et al. A comparison of the reliability of self-reported drug use and sexual behaviors using computer-assisted versus face-to-face interviewing. AIDS Education & Prevention. 2000;12(3):199–213. [PubMed] [Google Scholar]
- 30.Jones R. Survey data collection using Audio Computer Assisted Self-Interview. Western Journal of Nursing Research. 2003;25(3):349–58. doi: 10.1177/0193945902250423. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Guth D, Steer RA, Ball R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behaviour Research & Therapy. 1997;35(8):785–91. doi: 10.1016/s0005-7967(97)00025-9. [DOI] [PubMed] [Google Scholar]
- 32.SAS. Statistical Analysis Software Institute Inc. SAS/STAT 9.3 User's Guide. Cary, NC: SAS Institute Inc.; 2011. 2011. [Google Scholar]
- 33.DiLillo D, DeGue S, Kras A, Di Loreto-Colgan A, Nash CL. Participant responses to retrospective surveys of child maltreatment: Does method of assessment matter? Violence & Victims. 2006;21:419–424. [PubMed] [Google Scholar]
- 34.Hulme PA. Psychometric evaluation and comparison of three retrospective, multi-item measures of childhood sexual abuse. Child Abuse Neglect. 2007;31(8):853–869. doi: 10.1016/j.chiabu.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Widom C, Shepard R. Accuracy of adult recollections of childhood victimization: Part 1. Childhood physical abuse. Psychological Assessment. 1996;8(4):412–21. [Google Scholar]; Widom C, Morris S. Accuracy of adult recollections of childhood victimization: Part 2. Childhood sexual abuse. Psychological Assessment. 1997;9(1):34–46. [Google Scholar]
- 36.Brown J, Cohen P, Johnson JG, Salzinger S. A longitudinal analysis of risk factors for child maltreatment: Findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse & Neglect. 1998;22(11):1065–78. doi: 10.1016/s0145-2134(98)00087-8. [DOI] [PubMed] [Google Scholar]
- 37.Friedrich WN, Talley NJ, Panser L, Fett S, Zinsmeister AR. Concordance of reports of childhood abuse by adults. Child Maltreatment. 1997;2(2):164–71. [Google Scholar]
- 38.Halfon N, Gregory D, Stevens K, Larson L, Olson M. Duration of a well-child visit: Association with content, family-centeredness, and satisfaction. Pediatrics. 2011;128(4):657–64. doi: 10.1542/peds.2011-0586. [DOI] [PubMed] [Google Scholar]
- 39.Blumenthal D. Stimulating the adoption of health information technology. New England Journal of Medicine. 2009;360:1477–79. doi: 10.1056/NEJMp0901592. [DOI] [PubMed] [Google Scholar]
- 40.George S, Garth B, Baker R. Factors shaping effective utilization of health information technology in urban safety-net clinics. Health Informatics Journal. 2012;19(3):183–97. doi: 10.1177/1460458212464584. [DOI] [PMC free article] [PubMed] [Google Scholar]