Abstract
Introduction
Considering the joint association of neighborhood socioeconomic environment and individual-level health behaviors with health outcomes may help officials design effective disease prevention strategies. Herein, the joint influences of neighborhood socioeconomic environment and individual health behaviors on mortality are evaluated in a cohort primarily comprising persons with low individual-level SES.
Methods
The prospective Southern Community Cohort Study includes 77,896 white and African Americans recruited in the years 2002–2009; 55% of participants had a household income <$15,000 at baseline interview. Mortality from cancer (n=2,471), cardiovascular diseases (n=3,005), and all-causes (n=10,099) was identified from the National Death Index through December 31, 2013 (median follow-up, 8 years). Data were analyzed in the years 2016 and 2017. Associations were assessed between mortality, a neighborhood deprivation index composed of 11 census tract-level variables, five health behaviors, and a composite healthy lifestyle score.
Results
Living in a neighborhood with the greatest socioeconomic disadvantage was associated with higher all-cause mortality in both men (hazard ratio=1.41, 95% CI=1.27, 1.57) and women (hazard ratio=1.77, 95% CI=1.57, 2.00). Associations were attenuated after adjustment for individual-level SES and major risk factors (hazard ratio for men=1.09, 95% CI=0.98, 1.22, and hazard ratio for women=1.26, 95% CI=1.12, 1.42). The dose–response association between neighborhood disadvantage and mortality was less apparent among smokers. Nevertheless, individuals who lived in disadvantaged neighborhoods and had the unhealthiest lifestyle scores also experienced the highest mortality.
Conclusions
Disadvantaged neighborhood socioeconomic environments are associated with increased mortality in a cohort of individuals of low SES. Positive individual-level health behaviors may help negate the adverse effect of neighborhood disadvantage on mortality.
INTRODUCTION
Epidemiologic studies report associations between disadvantaged neighborhood socioeconomic environments and mortality.1–7 The relations between neighborhood socioeconomic environment and individual-level health outcomes may reflect correlations with individual-level SES, residents’ self-selection into neighborhoods, influences on resident health behaviors, access to health care, or the social environment, including neighborhood violence.8 Studies show residents of disadvantaged neighborhood socioeconomic environments report that they have less social support9 and their neighborhoods have lower social capital,10 both of which are associated with higher mortality.11–13 Proposed mechanisms by which neighborhoods may affect health behaviors include the influence of social and cultural norms around health behaviors; the ease of access to alcohol, energy-dense foods, and tobacco; and the level of difficulty in engaging in outdoor physical activity.14–18
Few published studies have evaluated potential interactions between neighborhood socioeconomic environment and individual-level health behaviors in association with mortality. Previous studies conducted using data from the NIH-AARP Diet and Health Study found the association between neighborhood socioeconomic environment and mortality is not modified by smoking status or consumption of red or processed meat.19,20 No previous study has evaluated the combined influence of health behaviors and neighborhood socioeconomic environment on mortality, in African American or socioeconomically disadvantaged populations. Considering the joint influence of neighborhood socioeconomic environment and individual-level health behavior on health may help health officials design effective disease prevention strategies to reduce mortality.
The Southern Community Cohort Study (SCCS) provides a unique opportunity to evaluate associations between neighborhood socioeconomic environment, individual-level health behavior, and mortality in a racially diverse low-SES population. A previous SCCS publication reported higher mortality associated with low individual SES and disadvantaged neighborhood socioeconomic environment.21 Herein, the mortality follow-up time is expanded, increasing the numbers of deaths by more than 65%, and the joint associations of neighborhood disadvantage with five behavioral (and one composite) health indicators on mortality is assessed.
METHODS
Study Population
Data available for analysis arise from 84,514 adults enrolled in the previously described prospective SCCS.22,23 Participants were eligible for enrollment if they were aged 40–79 years, English-speaking, and were not under treatment for cancer within the past year. Participants were recruited during 2002–2009, primarily from community health centers24 (86%) where trained interviewers collected information on lifestyle factors and demographics. The remaining cohort was enrolled using an identical mailed questionnaire sent to stratified random samples of residents in the same states. The SCCS was approved by IRBs at Vanderbilt University and Meharry Medical College. All participants provided written informed consent.
Measures
Vital status was obtained via linkage to the Social Security Administration’s Death Master File. Cause of death was ascertained from the National Death Index through December 31, 2013. Causes of death were grouped according to ICD-10 codes and were classified as cardiovascular diseases (CVD) (I00–I69), cancer (C00–C97), and all other-causes excluding CVD, cancer, and external causes, including accidents and injuries (deaths with codes beginning with the letter V, W, X or Y).
The previously developed neighborhood deprivation index variable21,25 was used as a measure of neighborhood socioeconomic environment. Briefly, the index was constructed through principal components analysis and incorporates 11 census tract-level variables that capture five domains including education, employment, housing, occupation, and poverty, described in more detail in Appendix Table 1 and a previous publication.21 The variables were obtained from 2000 U.S. Census data26 and linked to the geographic coordinates of participant’s residential address.27
Joint associations were evaluated between neighborhood socioeconomic environment and self-reported health behaviors at cohort entry for smoking status, alcohol intake, physical activity, sedentary behavior, diet quality, and a healthy lifestyle variable. For each participant, the healthy lifestyle score was created by counting and summing (0–4) the number of current public health guidelines followed by the participant for: alcohol intake, physical activity, sedentary behavior, and diet quality (Appendix Table 2).28–30 These behaviors were chosen due to their strong established associations with risk of premature death. Detailed information on health behavior ascertainment and variable categorization in statistical models can be found in Appendix Methods.
Statistical Analysis
Frequency distributions of participant characteristics were tabulated for the total sample and stratified by sex and race. Hazard ratios and 95% CIs were estimated using Cox proportional hazard models for the association between neighborhood deprivation index and mortality with age as the time scale. Cox models included robust variances based on the sandwich estimator to account for the potential of non-independence between participants because of clustering within census tracts. Entry time was defined as age at baseline interview and exit time as age at death or December 31, 2013, whichever came first.31 Comparison groups for the neighborhood deprivation index were created by dividing participants into quartiles based on the distribution of neighborhood deprivation index values of all census tracts in the 12 states that encompass the SCCS recruitment area. As expected by study design, a large number of SCCS participants fell in the quartile group for the most deprived neighborhood deprivation index. The joint associations of neighborhood deprivation index with five health behaviors and a healthy lifestyle score on all-cause mortality were evaluated. The behavioral variables were categorized as follows: smoking status (never, former, current smoker of <20 years or <20 cigarettes/day, current smoker of ≥20 years and ≥20 cigarettes/day), alcohol intake (non-drinker, moderate drinker, heavy drinker), physical activity (sex-specific tertiles), sedentary behavior (tertiles), and Healthy Eating Index diet quality (quartiles). Participants with missing Healthy Eating Index data (n=4,061) were set to the race, sex, and smoking status-specific medians. Statistical models were stratified by birth year (categorized into 10-year age groups) and adjusted for the following variables selected a priori: enrollment source, race, education, income, marital status, and insurance status. Missing covariate data were set to the race and sex-specific medians (mode for marital status and insurance status). Sample sizes for participants missing covariate data are as follows: education n=243, household income n=239, marital status n=347, and insurance coverage n=47. Analyses were conducted separately by sex because the association between lower neighborhood deprivation index and poorer mortality outcome was stronger in women (p for interaction=0.02). P‐values for trend tests were calculated using an ordinal variable representing neighborhood deprivation index quartiles in the model. The proportional hazards assumption was evaluated graphically and considered met. Interactions between neighborhood deprivation index X factors of interest were assessed by likelihood ratio tests to compare main effects models with and without the addition of cross-product terms. Statistical analyses were performed using SAS statistical software, version 9.4. Data analysis was conducted in the years 2016 and 2017.
RESULTS
Participants with <1 year of follow-up time (n=364) and those missing data on neighborhood deprivation index (n=1,223), smoking status (n=2,085), alcohol intake (n=2,933), physical activity (n=3,086), and sedentary behavior (n=2,535) were excluded from analysis. Data from 77,896 SCCS participants were available for analysis after these, not mutually exclusive, exclusions.
The majority of the cohort was African American, had household income <$15,000 at baseline, and did not have educational attainment beyond high school (Table 1). In comparisons with women, men were more likely to be current smokers, heavy drinkers, and have met the public health recommendation for physical activity.
Table 1.
Characteristics of Southern Community Cohort Study Subjects at Baseline, 2002–2009, by Sex and Race
| Baseline characteristic, % | Cohort | Women | Men | ||
|---|---|---|---|---|---|
| African American |
White | African American |
White | ||
| Participants, N | 77,896 | 30,076 | 14,380 | 21,417 | 8,859 |
| Age, median (IQR), years | 51 (13) | 50 (12) | 53 (13) | 49 (11) | 53 (13) |
| Enrollment source | |||||
| Community Health Center | 88.2 | 93.0 | 83.4 | 93.2 | 70.9 |
| General population | 11.8 | 7.0 | 16.6 | 6.8 | 29.1 |
| Education | |||||
| <High school | 28.8 | 29.9 | 24.4 | 33.6 | 22.8 |
| High school | 33.0 | 32.9 | 32.8 | 35.9 | 29.7 |
| >High school | 37.9 | 37.2 | 42.8 | 30.4 | 47.4 |
| Income, $ | |||||
| <15,000 | 54.9 | 58.8 | 49.0 | 59.8 | 42.2 |
| 15,000–24,999 | 20.9 | 22.8 | 19.3 | 21.2 | 17.0 |
| ≥25,000 | 22.9 | 17.3 | 30.2 | 18.1 | 39.6 |
| Marital status | |||||
| Married | 34.9 | 26.9 | 45.1 | 31.4 | 52.4 |
| Divorced | 33.6 | 34.6 | 33.6 | 33.8 | 28.7 |
| Widowed | 9.6 | 13.9 | 13.1 | 3.7 | 3.6 |
| Single | 21.5 | 24.3 | 7.7 | 31.0 | 14.0 |
| Insurance coverage, yes | 60.1 | 62.3 | 63.5 | 52.7 | 64.3 |
| Employeda | 41.7 | 42.6 | 41.2 | 39.6 | 44.1 |
| BMI, median (IQR), kg/m2 | 29.1 (9.4) |
31.5 (10.4) | 29.3 (10.3) | 26.6 (7.3) | 27.6 (7.3) |
| Current smoker | 41.2 | 32.6 | 35.9 | 57.3 | 41.2 |
| Non and moderate alcohol consumers | 82.2 | 87.3 | 91.6 | 69.1 | 80.1 |
| Meets physical activity guideline b | 21.0 | 16.2 | 17.9 | 27.3 | 26.2 |
| Sedentary time,c median (IQR), hours | 8.5 (6.3) | 9.0 (6.5) | 8.0 (5.7) | 8.3 (6.5) | 8.0 (5.8) |
Notes: Subjects with missing data not included in this analysis.
Among those under age 65 years.
Participants reporting ≥150 minutes/week of moderate activity, ≥75 minutes/week of vigorous activity or ≥150 minutes/week of moderate and vigorous activity combined.
Sedentary time is defined as the average sitting time per day over the course of the week.
IQR, interquartile range.
The range of neighborhood deprivation index values was wider, and on average more disadvantaged for African American participants than white participants (interquartile range, African Americans, 1.65, whites, 0.99). The median neighborhood deprivation index value for African American men (1.11) was higher than the median neighborhood deprivation index value for African American women (0.92), suggesting more socioeconomically disadvantaged neighborhood conditions for African American male participants. Men and women participants of white descent tended to live in neighborhoods with similar neighborhood deprivation index scores (median, white men, −0.11, white women, −0.12).
Individuals with neighborhood deprivation index values that indicated greater neighborhood disadvantage were at higher risk of death (Table 2), with stronger associations among women than men. Sex-specific associations were more evident in African Americans than in white participants. The higher risk associated with higher neighborhood deprivation index was attenuated after adjustment for individual-level SES variables, particularly among men and white women. Hazard ratios for the associations between neighborhood deprivation index and mortality were largely unchanged with additional adjustment for individual health behaviors. However, all covariates included in statistical models (potential confounders, individual-level SES, and health behavior variables) were associated with mortality at statistical significance p<0.05. There was no statistical differences in the associations between neighborhood deprivation index and all-cause mortality in African Americans and whites (p-interaction=0.58 in men and p-interaction=0.38 in women). Among men, point estimates were similar for the associations of neighborhood deprivation index with CVD, cancer, and all other non-external causes of mortality, however, CIs were wider due to smaller sample sizes (Appendix Table 3). In women, stronger significant trends with were observed for associations between neighborhood deprivation index with CVD and other-cause mortality than for cancer.
Table 2.
Associations Between Neighborhood Deprivation Index and All-Cause Mortality Among Men, the Southern Community Cohort Study
| Neighborhood deprivation index | Cohort | Deaths | Median age at death, years | HR (95% CI)a | HR (95% CI)b | HR (95% CI)c | HR (95% CI)d |
|---|---|---|---|---|---|---|---|
| All participants | |||||||
| Q1 (least deprived) | 3,456 | 438 | 60 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 4,554 | 697 | 60 | 1.14 (1.01, 1.29) | 1.02 (0.90, 1.15) | 1.10 (0.97, 1.24) | 1.01 (0.90, 1.14) |
| Q3 | 5,976 | 1,003 | 60 | 1.23 (1.10, 1.38) | 1.04 (0.93, 1.17) | 1.17 (1.04, 1.31) | 1.04 (0.93, 1.17) |
| Q4 (most deprived) | 17,468 | 3,212 | 58 | 1.41 (1.27, 1.57) | 1.12 (1.00, 1.24) | 1.29 (1.16, 1.43) | 1.09 (0.98, 1.22) |
| p-trend | <0.0001 | 0.008 | <0.0001 | 0.03 | |||
| African American participants | |||||||
| Q1 (least deprived) | 1,234 | 153 | 60 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 1,962 | 280 | 59 | 1.12 (0.92, 1.36) | 0.99 (0.81, 1.20) | 1.08 (0.89, 1.31) | 0.99 (0.81, 1.20) |
| Q3 | 3,340 | 548 | 59 | 1.26 (1.06, 1.51) | 1.08 (0.90, 1.29) | 1.21 (1.01, 1.45) | 1.08 (0.90, 1.29) |
| Q4 (most deprived) | 14,881 | 2,674 | 58 | 1.41 (1.20, 1.66) | 1.13 (0.96, 1.33) | 1.29 (1.10, 1.52) | 1.11 (0.94, 1.30) |
| p-trend | <0.0001 | 0.02 | <0.0001 | 0.05 | |||
| White participants | |||||||
| Q1 (least deprived) | 2,006 | 257 | 60 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 2,348 | 375 | 60 | 1.12 (0.96, 1.31) | 1.03 (0.88, 1.21) | 1.07 (0.92, 1.26) | 1.02 (0.87, 1.20) |
| Q3 | 2,362 | 416 | 61 | 1.17 (1.00, 1.37) | 1.02 (0.87, 1.20) | 1.11 (0.95, 1.30) | 1.02 (0.87, 1.20) |
| Q4 (most deprived) | 2,143 | 467 | 59 | 1.45 (1.24, 1.70) | 1.16 (0.99, 1.36) | 1.28 (1.09, 1.50) | 1.11 (0.95, 1.31) |
| p-trend | <0.0001 | 0.06 | 0.002 | 0.16 |
Notes: Comparison groups for neighborhood deprivation index were created by dividing participants into quartiles based on the distribution of neighborhood deprivation index value of all the census tracts in the 12 states that encompass the Southern Community Cohort Study recruitment area. Q1 represents participants who reside in neighborhoods with the least deprived values for neighborhood deprivation index.
HRs are estimated using Cox models with age as the time scale and stratified by birth year. Statistical models are adjusted for enrollment source, and race.
Adjusted for enrollment source, race, education, income, marital status, and insurance status.
Adjusted for enrollment source, race, smoking status, alcohol intake, diet quality, physical activity, and sedentary time.
Adjusted for enrollment source, race, education, income, marital status, insurance status, smoking status, alcohol intake, diet quality, physical activity, and sedentary time.
HR, hazard ratio; Q1–Q4, quartile 1–4.
Participants with values in the quartile for least deprived neighborhood index tended to have higher (better) diet quality scores, were more likely to meet the physical activity recommendation and less likely to be current smokers (Appendix Table 4). Notably, the majority (60%) of men falling in the quartile for highest neighborhood deprivation index were current smokers compared with 35% of the men falling in the quartile for lowest neighborhood deprivation index. In general, the patterns observed between the deprivation index and all-cause mortality tended to hold within strata of the behavioral variables, although some significant interactions were observed. Specifically, weaker trends in current smokers, especially heavy smokers (Figure 1 and Appendix Table 5), and stronger trends in both female heavy alcohol drinkers (p-interaction=0.03), and less physically active men (p-interaction=0.001). The association between neighborhood deprivation index and all-cause mortality was consistent in each strata of the healthy lifestyle variable, where participants who exhibited fewer healthy behaviors and resided in neighborhoods with more deprived neighborhood deprivation index values were at the highest risk of death (Appendix Tables 6–9).
Figure 1.
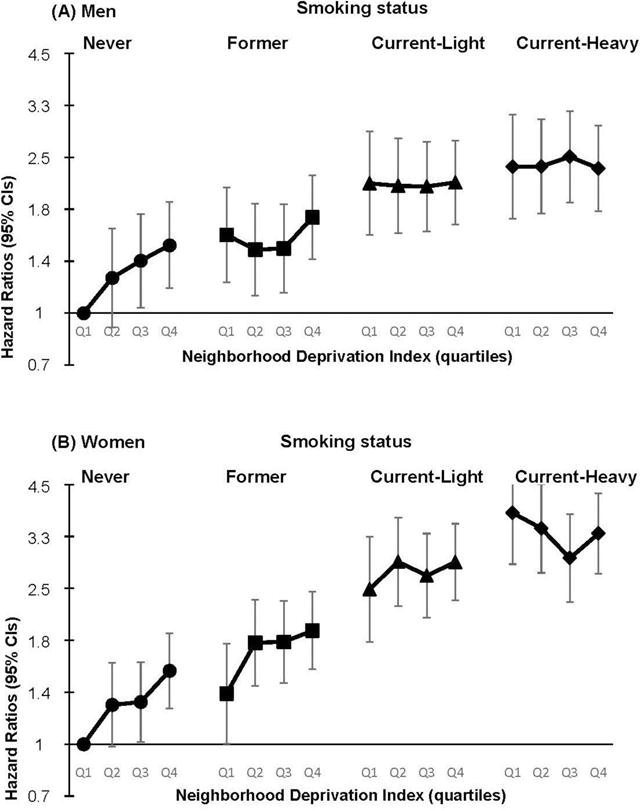
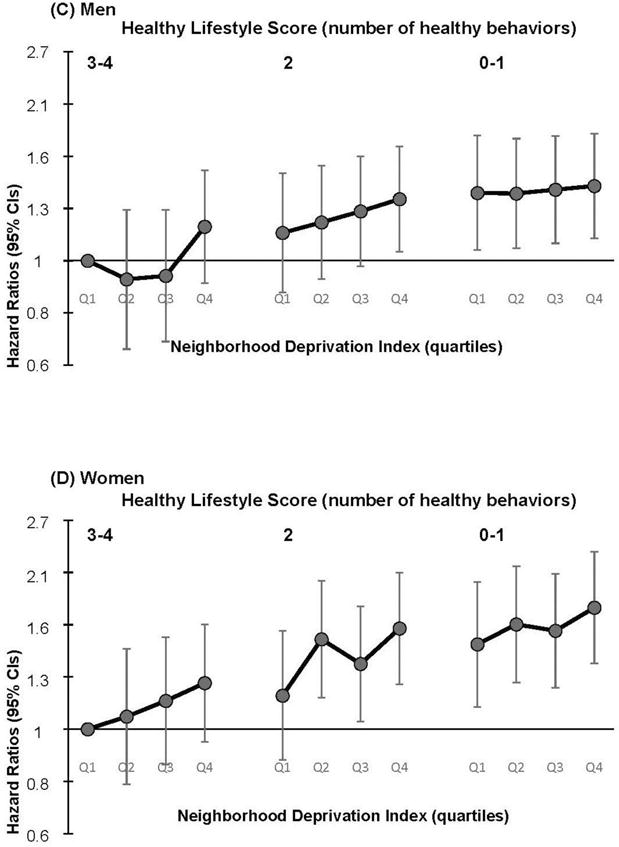
The joint associations of the Neighborhood Deprivation Index and health behaviors with all-cause mortality by sex, the Southern Community Cohort Study.
Notes: The top portion of the figure displays the associations between smoking status and neighborhood deprivation index with all-cause mortality. Participants who have never smoked and live in the least deprived neighborhoods are used as the reference group. Panel (A) includes men and panel (B) includes women. The lower portion of the Figure displays the joint associations of a healthy lifestyle score and neighborhood deprivation index with all-cause mortality. The healthy lifestyle score is a composite variable for number of public health guidelines met for alcohol intake, physical activity, diet quality, and sedentary time. Participants who met three or more public health guidelines and lived in the least deprived neighborhoods were used as the reference group. Panel (C) includes men and panel (D) includes women. Hazard ratio and 95% CIs are located in Appendix Tables 5 and 6.
DISCUSSION
This cohort study demonstrates an independent association between residing in a disadvantaged neighborhood socioeconomic environment and higher mortality in low-SES Americans. The association remains after adjustment for individual-level SES and individual-level health behaviors. Previous studies also report that neighborhood-level socioeconomic factors are associated with increased mortality.1–7,32 In the current study, the association between disadvantaged neighborhood socioeconomic environment and mortality was stronger in women than men, particularly for non-cancer mortality. The reasons for a stronger association in women than men are unclear. However, it is likely that the sex differences in the association may be partially explained by differences in neighborhood characteristics, reliance on their neighborhood for healthful resources (outdoor activity), or coping strategies in relation to neighborhood-related stressors. Most studies have not specifically evaluated whether the association between neighborhood socioeconomic environment and mortality varies by sex, but find inverse associations between neighborhood and mortality in both sexes when analyses are stratified by sex.2,19
The strongest associations observed between neighborhood socioeconomic environment and cause-specific mortality were observed for CVD and other-cause mortality (including diabetes). Associations between neighborhood socioeconomic environment and cancer mortality were not strong in men or women. Lifestyle factors generally have stronger associations with incidence of CVD and diabetes than with incidence of cancer. Additionally, previous studies report residing in a disadvantaged neighborhood socioeconomic environment has been linked to higher incidence of obesity, CVD, and diabetes.8,33
Many investigators stratify analyses by race because of differences in individual-level SES by race, U.S. residential racial segregation, and potentially non-overlapping distributions of neighborhood characteristics of African American and white participants. In stratified analyses, these studies find neighborhood socioeconomic environment–mortality associations in both whites and African Americans.1,4 In the current study, the association between disadvantaged neighborhood socioeconomic environment and mortality was not modified by race. The study design of the SCCS allows for more sufficient control of confounding by individual-level SES, in that the majority of both African American and white participants are low-income and have minimal education. Additionally, the range of neighborhood deprivation index values for African American participants largely overlapped the range for white participants, although on average African Americans lived in more disadvantaged neighborhoods.
A hypothesized mechanism explaining the association between neighborhood socioeconomic environment and health outcomes is that disadvantaged neighborhoods position individuals at higher risk of choosing unhealthy behaviors. For instance, neighborhoods with more access to alcohol, energy-dense foods, and tobacco may facilitate residents’ consumption of these products.14–17 A recent meta-analysis finds associations between residing in more disadvantaged neighborhoods with higher smoking and physical inactivity.34 The current study provides evidence in line with these findings. Residents falling in the quartile for most-deprived neighborhood deprivation index were more often current smokers, heavy drinkers, physically inactive, and had poorer diet quality scores. The social standards of a neighborhood and the prevalence of healthy behaviors may affect an individual’s health behaviors by influencing what residents consider as acceptable behavioral norms.8,35
Few published studies have evaluated interactions between neighborhood socioeconomic environment and individual-level health behaviors. In the NIH-AARP Diet and Health Study, which includes participants of relatively high SES, investigators find no evidence of effect modification of the association between neighborhood socioeconomic environment and mortality by smoking status or by consumption of red or processed meat.19,20 The current study’s analyses show the relation between neighborhood socioeconomic environment and mortality varies by individual-level smoking behavior, being most apparent in never smokers and weakest in heavy smokers. Non-smokers are at lower risk of death than smokers are and thus the effects of additional mortality risk factors, such that disadvantaged neighborhood socioeconomic environment, result in a more apparent association with risk of mortality than in smokers. Smokers, regardless of the community they lived in, experience a higher risk of death than never smokers, with heavy smoking apparently dominating any effect of disadvantaged neighborhood socioeconomic environment. Interactions were observed between neighborhood socioeconomic environment and alcohol consumption and physical activity, but they are not consistent between men and women. No interactions were observed with sedentary activity, the dietary index, or the healthy lifestyle score. However, in analyses that combine neighborhood socioeconomic environment and individual health behaviors, individuals who live in disadvantaged neighborhood socioeconomic environments and meet few public health recommendations for health behaviors are at substantially higher risk of death, suggesting that lifestyle modification of health behaviors could reduce mortality risk, irrespective of neighborhood SES. Maintaining a healthy lifestyle was associated with lower risk of death in all strata of neighborhood socioeconomic environment.
Limitations
This study has notable strengths and limitations. Strengths include complete detailed information provided by cohort members at baseline on individual-level health behaviors, including diet, physical activity, alcohol, and smoking, which allows for comprehensive analyses of these variables. Additionally, the cohort’s linkage with the National Death Index for vital status allows for complete ascertainment of individual-level outcomes that are obtained objectively. The SCCS sample consists primarily of low-SES Americans and the majority of the participants are African Americans. These groups have been underrepresented in previous neighborhood epidemiologic investigations. This study also has certain limitations. The neighborhood deprivation index used in this study is derived from census tract-level variables and represents an approximation for the participants’ neighborhood-level exposures. This study uses a census tract measure, instead of participant-defined neighborhoods or direct measurement of specific neighborhood characteristics, because of the systematic and standardized data collection methods employed by the U.S. Census Bureau. Additionally, this type of index has been frequently used in previous studies and consistently associated with health outcomes.2,21,25,36 However, a limitation of using census tract-level data is the inability to determine how closely the neighborhood deprivation index variable aligns with the participants’ experiences in their self-defined neighborhoods. In using a composite variable that encompasses the domains of neighborhood-level education, employment, housing, occupation, and poverty, this study is unable to identify any singular causal mechanism of the association between neighborhood socioeconomic environment and mortality. Currently, it is not known exactly how these neighborhood-level socioeconomic factors are related to health. Associations may be reflective of truly causal conditions or may represent residents’ self-selection into neighborhoods because of individual-level socioeconomic position, or personal preferences, possibly related to access to amenities, racial composition, or social/cultural norms.8 Associations may also be attributed to residual confounding by individual-level SES, such as household income. Another limitation is the large number of statistical tests conducted in order to evaluate potential effect modification of health behaviors on the association between neighborhood depreciation index and mortality. However, using a Bonferroni adjusted p-value of 0.0002 (0.05/256 [the number of statistical tests conducted]) would lead to similar conclusions about the nature of the associations between neighborhood socioeconomic environment, healthy lifestyle, and mortality. Lastly, single baseline measurements of participants’ health behaviors and neighborhood-level exposures were used. Future studies taking into account exposures over the life course may improve upon the study design.
CONCLUSIONS
Residing in a neighborhood with greater socioeconomic disadvantage is associated with higher mortality for low income and African American residents, especially women. Individuals living in disadvantaged neighborhood socioeconomic environments and who exhibit unhealthy behaviors experienced the greatest increase in all-cause mortality. Positive individual-level health behaviors could substantially negate the effect of disadvantaged neighborhood socioeconomic environment on mortality. Maintaining a healthy lifestyle is associated with lower mortality in all socioeconomic environments. Identifying individual-level health behaviors that modify associations between disadvantaged neighborhood socioeconomic environment and health outcomes is of public health significance and could help prioritize future policy. Health policies and interventions should be implemented with the goal of improving socioeconomic position in disadvantaged communities, such as programs to improve high school graduation rates, decrease community-level unemployment rates, and move residents out of poverty.33 This study provides evidence for comprehensive approaches for lifestyle modification and community improvement to reduce the risk of death in African Americans and low-income populations.
Supplementary Material
Table 3.
Associations Between Neighborhood Deprivation Index and All-Cause Mortality Among Women, the Southern Community Cohort Study
| Neighborhood deprivation index | Cohort | Deaths | Median age at death, years | HR (95% CI)a | HR (95% CI)b | HR (95% CI)c | HR (95% CI)d |
|---|---|---|---|---|---|---|---|
| All participants | |||||||
| Q1 (least deprived) | 4,916 | 335 | 61 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 7,962 | 753 | 61 | 1.39 (1.22, 1.58) | 1.19 (1.04, 1.35) | 1.30 (1.14, 1.48) | 1.17 (1.03, 1.34) |
| Q3 | 10,317 | 1,000 | 62 | 1.39 (1.23, 1.57) | 1.13 (0.99, 1.27) | 1.28 (1.13, 1.45) | 1.12 (0.99, 1.27) |
| Q4 (most deprived) | 23,247 | 2,661 | 60 | 1.77 (1.57, 2.00) | 1.33 (1.18, 1.50) | 1.52 (1.35, 1.71) | 1.26 (1.12, 1.42) |
| p-trend | <0.0001 | <0.0001 | <0.0001 | 0.0002 | |||
| African American participants | |||||||
| Q1 (least deprived) | 1,718 | 94 | 62 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 3,219 | 261 | 60 | 1.46 (1.16, 1.84) | 1.29 (1.02, 1.63) | 1.44 (1.14, 1.81) | 1.32 (1.05, 1.67) |
| Q3 | 5,486 | 490 | 62 | 1.48 (1.19, 1.84) | 1.26 (1.01, 1.57) | 1.45 (1.17, 1.80) | 1.29 (1.04, 1.61) |
| Q4 (most deprived) | 19,653 | 2,186 | 59 | 1.88 (1.54, 2.31) | 1.48 (1.20, 1.81) | 1.70 (1.38, 2.08) | 1.43 (1.17, 1.76) |
| p-trend | <0.0001 | <0.0001 | <0.0001 | 0.0003 | |||
| White participants | |||||||
| Q1 (least deprived) | 2,852 | 222 | 60 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Q2 | 4,271 | 439 | 61 | 1.28 (1.09, 1.51) | 1.08 (0.92, 1.28) | 1.17 (0.99, 1.37) | 1.07 (0.91, 1.26) |
| Q3 | 4,343 | 469 | 62 | 1.30 (1.11, 1.52) | 1.04 (0.88, 1.22) | 1.16 (0.99, 1.36) | 1.03 (0.87, 1.20) |
| Q4 (most deprived) | 2,914 | 390 | 60 | 1.64 (1.39, 1.93) | 1.20 (1.01, 1.42) | 1.38 (1.17, 1.63) | 1.16 (0.98, 1.38) |
| p-trend | <0.0001 | 0.07 | 0.0004 | 0.13 |
Notes: Comparison groups for neighborhood deprivation index were created by dividing participants into quartiles based on the distribution of neighborhood deprivation index value of all the census tracts in the 12 states that encompass the Southern Community Cohort Study recruitment area. Q1 represents participants who reside in neighborhoods with the least deprived values for neighborhood deprivation index.
HRs are estimated using Cox models with age as the time scale and stratified by birth year. Statistical models are adjusted for enrollment source, and race.
Adjusted for enrollment source, race, education, income, marital status, and insurance status.
Adjusted for enrollment source, race, smoking status, alcohol intake, diet quality, physical activity, and sedentary time.
Adjusted for enrollment source, race, education, income, marital status, insurance status, smoking status, alcohol intake, diet quality, physical activity, and sedentary time.
HR, hazard ratio; Q1–Q4, quartile 1–4.
Acknowledgments
The Southern Community Cohort Study is funded by grant R01 CA92447 from the National Cancer Institute at NIH. Partial support for Dr. Hargreaves is provided by NIH grants 5P60 DK20593‐24 and 5U01 CA114641‐05. Dr. Warren Andersen is supported by K99 CA207848 and the Vanderbilt Molecular and Genetic Epidemiology of Cancer training program (U.S. NIH grant R25 CA160056, PI: Dr. Xiao-Ou Shu).
WZ and WJB obtained funding, and conceived of, organized, and supervised the parent studies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors’ contributions: SWA searched the literature, analyzed the data, and drafted the report, tables, and figures with contributions from X-OS, WJB, and WZ. MS managed the data. All authors reviewed the manuscript for important intellectual content, and approve of the final version to be published. Each author participated sufficiently in the work to believe in its overall validity and to take public responsibility for its content.
No financial disclosures were reported by the authors of this paper.
References
- 1.Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socioeconomic status. Epidemiology. 1997;8(1):42–47. doi: 10.1097/00001648-199701000-00007. https://doi.org/10.1097/00001648-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Winkleby MA, Cubbin C. Influence of individual and neighbourhood socioeconomic status on mortality among black, Mexican-American, and white women and men in the United States. J Epidemiol Community Health. 2003;57(6):444–452. doi: 10.1136/jech.57.6.444. https://doi.org/10.1136/jech.57.6.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL, Atherosclerosis Risk in Communities Study Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33(2):398–407. doi: 10.1093/ije/dyh063. https://doi.org/10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- 4.Diez Roux AV, Borrell LN, Haan M, Jackson SA, Schultz R. Neighbourhood environments and mortality in an elderly cohort: results from the cardiovascular health study. J Epidemiol Community Health. 2004;58(11):917–923. doi: 10.1136/jech.2003.019596. https://doi.org/10.1136/jech.2003.019596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hastert TA, Beresford SAA, Sheppard L, White E. Disparities in cancer incidence and mortality by area-level socioeconomic status: a multilevel analysis. J Epidemiol Community Health. 2015;69(2):168–176. doi: 10.1136/jech-2014-204417. https://doi.org/10.1136/jech-2014-204417. [DOI] [PubMed] [Google Scholar]
- 6.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. https://doi.org/10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bethea TN, Palmer JR, Rosenberg L, Cozier YC. Neighborhood Socioeconomic Status in Relation to All-Cause, Cancer, and Cardiovascular Mortality in the Black Women’s Health Study. Ethn Dis. 2016;26(2):157–164. doi: 10.18865/ed.26.2.157. https://doi.org/10.18865/ed.26.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. https://doi.org/10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 9.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. https://doi.org/10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 10.Lochner KA, Kawachi I, Brennan RT, Buka SL. Social capital and neighborhood mortality rates in Chicago. Soc Sci Med. 2003;56(8):1797–1805. doi: 10.1016/s0277-9536(02)00177-6. https://doi.org/10.1016/S0277-9536(02)00177-6. [DOI] [PubMed] [Google Scholar]
- 11.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. https://doi.org/10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkman LF, Melchior M, Chastang J-F, Niedhammer I, Leclerc A, Goldberg M. Social integration and mortality: a prospective study of French employees of Electricity of France-Gas of France: the GAZEL Cohort. Am J Epidemiol. 2004;159(2):167–174. doi: 10.1093/aje/kwh020. https://doi.org/10.1093/aje/kwh020. [DOI] [PubMed] [Google Scholar]
- 13.Inoue S, Yorifuji T, Takao S, Doi H, Kawachi I. Social cohesion and mortality: a survival analysis of older adults in Japan. Am J Public Health. 2013;103(12):e60–66. doi: 10.2105/AJPH.2013.301311. https://doi.org/10.2105/AJPH.2013.301311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LaVeist TA, Wallace JM. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51(4):613–617. doi: 10.1016/s0277-9536(00)00004-6. https://doi.org/10.1016/S0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- 15.Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. https://doi.org/10.1016/S0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 16.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–217. doi: 10.1016/j.amepre.2004.06.007. https://doi.org/10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Siahpush M, Jones PR, Singh GK, Timsina LR, Martin J. Association of availability of tobacco products with socio-economic and racial/ethnic characteristics of neighbourhoods. Public Health. 2010;124(9):525–529. doi: 10.1016/j.puhe.2010.04.010. https://doi.org/10.1016/j.puhe.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 18.Christine PJ, Auchincloss AH, Bertoni AG, et al. Longitudinal Associations Between Neighborhood Physical and Social Environments and Incident Type 2 Diabetes Mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA) JAMA Intern Med. 2015;175(8):1311–1320. doi: 10.1001/jamainternmed.2015.2691. https://doi.org/10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Major JM, Doubeni CA, Freedman ND, et al. Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PloS One. 2010;5(11):e15538. doi: 10.1371/journal.pone.0015538. https://doi.org/10.1371/journal.pone.0015538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Major JM, Cross AJ, Doubeni CA, et al. Socioeconomic deprivation impact on meat intake and mortality: NIH-AARP Diet and Health Study. Cancer Causes Control. 2011;22(12):1699–1707. doi: 10.1007/s10552-011-9846-0. https://doi.org/10.1007/s10552-011-9846-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014;104(12):e98–e107. doi: 10.2105/AJPH.2014.302156. https://doi.org/10.2105/AJPH.2014.302156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Signorello LB, Hargreaves MK, Steinwandel MD, et al. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97(7):972–979. [PMC free article] [PubMed] [Google Scholar]
- 23.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21(1 Suppl):26–37. doi: 10.1353/hpu.0.0245. https://doi.org/10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hargreaves MK, Arnold CW, Blot WJ. Multicultural Medicine and Health Disparities. 1st. New York, NY: McGraw-Hill Professional; 2005. Community health centers: their role in the treatment of minorities and in health disparities research; p. 500. [Google Scholar]
- 25.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health Bull N Y Acad Med. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. https://doi.org/10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Census Bureau US. Census of Population and Housing, summary file 3: technical documentation. 2000 www.census.gov/prod/cen2000/doc/sf3.pdf. Published August 18, 2015.
- 27.Sonderman JS, Mumma MT, Cohen SS, Cope EL, Blot WJ, Signorello LB. A multi-stage approach to maximizing geocoding success in a large population-based cohort study through automated and interactive processes. Geospat Health. 2012;6(2):273–284. doi: 10.4081/gh.2012.145. https://doi.org/10.4081/gh.2012.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Office of Disease Prevention and Health Promotion. Physical Activity Guidelines for Americans. Vol. 2008. U.S.: DHHS; 2008. p. 76. [Google Scholar]
- 29.U.S. Department of Agriculture, U.S. DHHS. Dietary Guidelines for Americans. 7th. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- 30.American Cancer Society. Cancer Facts & Figures 2016. Atlanta, GA: American Cancer Society; 2016. [Google Scholar]
- 31.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145(1):72–80. doi: 10.1093/oxfordjournals.aje.a009034. https://doi.org/10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- 32.Meijer M, Röhl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. https://doi.org/10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 33.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. https://doi.org/10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Algren MH, Bak CK, Berg-Beckhoff G, Andersen PT. Health-Risk Behaviour in Deprived Neighbourhoods Compared with Non-Deprived Neighbourhoods: A Systematic Literature Review of Quantitative Observational Studies. PloS One. 2015;10(10):e0139297. doi: 10.1371/journal.pone.0139297. https://doi.org/10.1371/journal.pone.0139297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ivory VC, Blakely T, Richardson K, Thomson G, Carter K. Do changes in neighborhood and household levels of smoking and deprivation result in changes in individual smoking behavior? A large-scale longitudinal study of New Zealand adults. Am J Epidemiol. 2015;182(5):431–440. doi: 10.1093/aje/kwv097. https://doi.org/10.1093/aje/kwv097. [DOI] [PubMed] [Google Scholar]
- 36.Doubeni CA, Schootman M, Major JM, et al. Health status, neighborhood socioeconomic context, and premature mortality in the United States: The National Institutes of Health-AARP Diet and Health Study. Am J Public Health. 2012;102(4):680–688. doi: 10.2105/AJPH.2011.300158. https://doi.org/10.2105/AJPH.2011.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


