Abstract
Aim
To evaluate whether performing ventral hernia repairs using the Ethicon Physiomesh™ Open Flexible Composite Mesh Device in conjunction with the Ethicon Securestrap® Open Absorbable Strap Fixation Device reduces surgical time and surgeon stress levels, compared with traditional surgical repair methods.
Methods
To repair a simulated ventral incisional hernia, two surgeries were performed by eight experienced surgeons using a live porcine model. One procedure involved traditional suture methods and a flat mesh, and the other procedure involved a mechanical fixation device and a skirted flexible composite mesh. A Surgery Task Load Index questionnaire was administered before and after the procedure to establish the surgeons’ perceived stress levels, and saliva samples were collected before, during, and after the surgical procedures to assess the biologically expressed stress (cortisol and salivary alpha amylase) levels.
Results
For mechanical fixation using the Ethicon Physiomesh Open Flexible Composite Mesh Device in conjunction with the Ethicon Securestrap Open Absorbable Strap Fixation Device, surgeons reported a 46.2% reduction in perceived workload stress. There was also a lower physiological reactivity to the intraoperative experience and the total surgical procedure time was reduced by 60.3%.
Conclusions
This study provides preliminary findings suggesting that the combined use of a mechanical fixation device and a skirted flexible composite mesh in an open intraperitoneal onlay mesh repair has the potential to reduce surgeon stress. Additional studies are needed to determine whether a reduction in stress is observed in a clinical setting and, if so, confirm that this results in improved clinical outcomes.
Keywords: ventral hernia, SURG-TLX, flexible composite mesh device, hernia repair, salivary cortisol, salivary alpha amylase
Introduction
Ventral incisional hernias are a common, costly complication of midline abdominal incisions.1,2 A recent systematic review and a meta-analysis of published studies describing midline incisions reported a postoperative incisional hernia prevalence of over 12% and a >5% risk of undergoing surgical repair after midline laparotomy.1 As approximately one-third of all individuals in developed countries will undergo abdominal surgery in their lifetime, this represents a significant economic burden.2,3 In the USA, the number of ventral hernia repairs performed has risen from an estimated 360,000 in 2003 to over 500,000 in 2010.4,5
Despite surgical improvements, hernia repair procedures are associated with a high incidence of serious postoperative complications including hernia recurrence.6,7 Systematic reviews and expert consensus on best practice in the management of ventral hernias recommend using mesh reinforcement for ventral hernia repairs to reduce recurrence rates.8 However, other factors have also been shown to influence surgical outcome.8 Patient comorbidities, such as obesity and smoking, wound class, operative factors,6,8 and surgeon factors including procedural inexperience and stress experienced during a complex or unfamiliar procedure, have all been associated with poor patient outcomes.8–12 Consequently, reducing surgeon stress by reducing surgical procedure complexity has the potential to improve patient outcomes and minimize surgical error.
The Ethicon Securestrap® Open Absorbable Strap Fixation Device (Ethicon US, LLC, Cincinnati, OH, USA) is a mechanical fixation device designed to secure prosthetic materials to soft tissue, including open intraperitoneal onlay mesh (IPOM) used for ventral/incisional hernia repair procedures. Ethicon Physiomesh™ Open Flexible Composite Mesh Device (Ethicon US, LLC, Cincinnati, OH, USA) is a skirted mesh designed specifically for use with absorbable tackers for open ventral hernia repairs (Figure 1). Using mechanical fixation in conjunction with skirted mesh reduces the complexity of the procedure, facilitating fast, secure fixation of the mesh to the defect site.11 This decreases procedure time which, in conjunction with the use of absorbable tackers instead of transfacial sutures, has the potential to improve patient outcomes, for example, by limiting postoperative pain.13
Figure 1.
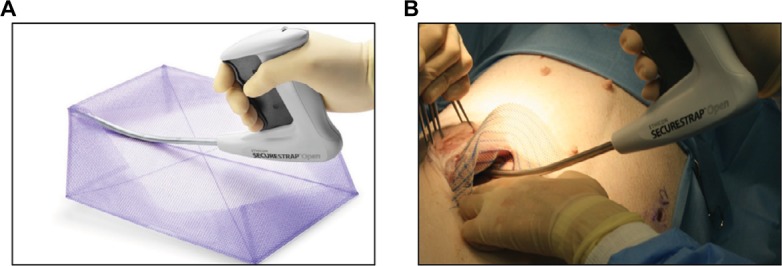
(A) Illustration of the use of Ethicon Securestrap® Open Absorbable Strap Fixation Device to secure Ethicon Physiomesh™ Open Flexible Composite Mesh for an IPOM hernia repair and (B) intraoperative image obtained during fixation of Ethicon Physiomesh Open Flexible Composite Mesh using the Ethicon Securestrap Open Absorbable Strap Fixation Device in a porcine simulated ventral hernia model.
Abbreviation: IPOM, intraperitoneal onlay mesh.
This study was an interventional, randomized, paired-within-subject, crossover study. It was designed to investigate whether, compared with traditional hernia repair methods, the surgical benefits associated with mechanical fixation using the Ethicon Securestrap Open Absorbable Strap Fixation Device in conjunction with the Ethicon Physiomesh Open Flexible Composite Mesh Device reduce surgeon stress during a hernia repair procedure. In this study, surgeons performed two hernia repairs using a porcine simulated hernia repair model. Surgical task load was measured using the surgical task load index (SURG-TLX), a validated self-reported questionnaire that measures intraoperative mental stress and workload by evaluating six different dimensions: mental demands, physical demands, temporal demands, task complexity, situation stress, and distractions.14,15
This study expanded on an earlier work performed using a similar simulated hernia repair model by measuring the levels of cortisol and alpha amylase in the saliva of surgeons to evaluate surgeon stress.15 Previous studies have demonstrated that cortisol correlates with hypothalamic–pituitary–adrenal (HPA) activity, which is associated with lack of perceived control, withdrawal, and distress; whereas, salivary alpha amylase (sAA) correlates with autonomic nervous system (ANS) arousal, an indicator of perceived control, cognitive effort, and an identified need to mobilize existing skills and strategies to solve problems.16,17 Using a mechanical strap fixation device in conjunction with a preformed skirted mesh product was predicted to reduce surgical time and surgeon stress levels compared with traditional suture fixation performed using a standard flat mesh, resulting in reduced HPA activity and ANS arousal.
Methods
Study design
This randomized study applied a paired-within-subject cross-over design to measure surgeon stress levels experienced during two simulated ventral hernia mesh repair procedures, both performed on the same day using an IPOM technique. A live porcine model was used for this investigation. The surgeons participating in the study were experienced in performing hernia repairs using both traditional suture methods and mechanical fixation repair techniques, but were naïve to the use of both the Ethicon Physiomesh Open Flexible Composite Mesh Device and the Ethicon Securestrap Open Absorbable Strap Fixation Device. The order in which surgeons performed the two mesh repair procedures was randomized. The study was reviewed and approved by the Western Institutional Review Board, Puyallup, WA, USA, and the Institutional Animal Care and Use Committee (protocol number 14-0031) at Ethicon Inc. Eight surgeons were recruited and written informed consent was obtained. Table 1 presents the specific eligibility and exclusion criteria that were utilized. Each eligible surgeon was assigned a unique identification number that was retained throughout the study to protect his/her confidentiality, and physicians were compensated for participation in the study.
Table 1.
Study inclusion and exclusion criteria
| Inclusion criteria: | |
| • At least 18 years old | |
| • Experienced in hernia repairs using mechanical fixation devices and suturing | |
| • Provided the written informed consent form on the day of surgery | |
|
| |
| Exclusion criteria: | |
|
| |
| • History of Cushing’s, Addison’s, or Thyroid disease | |
| • Smoked cigarettes or used other forms of tobacco or nicotine within 8 hours of the procedures | |
| • Had any dental work that may have caused injury to tissue in the mouth within the prior 24 hours | |
| • Any open (i.e., bleeding) sores or abrasions in the mouth | |
| • Salivary gland diseases or disorders | |
| • Currently taking steroid-based antiinflammatory or adrenergic agonists/antagonists | |
Surgical procedures
To prevent experimentally independent elevations in cortisol and sAA, surgeons were instructed not to consume a large meal within 1 hour of sample collection, or to consume dairy, acidic, or high sugar-content foods within 20 minutes of the first saliva sample collection time. In the event that a surgeon ingested any salivary stimulants, he/she was instructed to rinse their mouth with water at least 10 minutes prior to initial sample collection.
Participating surgeons were blinded to the order of the IPOM procedures until the start of the first simulated IPOM hernia repair. For study documentation purposes, the two procedures were designated as Procedure A (traditional hernia repair method with Proceed Surgical Mesh and suture fixation) and Procedure B (mechanical fixation using Ethicon Physiomesh Open Flexible Composite Mesh Device with Ethicon Securestrap Open Fixation Device). The randomization was performed to ensure that both procedural orderings (A then B, and B then A) were performed an equal number of times.
All institutional and national guidelines for the care and use of laboratory animals were followed and the study protocol was approved by the local Institutional Animal Care and Use Committee. Animals were anesthetized, intubated, and maintained under a surgical plane of anesthesia for the duration of the study. Animals were draped for abdominal surgery and a preclinical veterinary surgeon performed a full thickness ventral midline abdominal incision of ~12 cm in length to create a simulated ventral hernia. Participating surgeons were then brought into the operating room where they were required to follow standard sterile operating room procedures in an effort to replicate a human operating room environment. Once scrubbed, gowned, and gloved, the surgeons were shown the ventral midline defect and asked to repair the simulated hernia using Procedure A or B as assigned.
For Procedure A, the surgeons trimmed and prepared the Proceed Surgical Mesh using their preferred method. The surgeons then followed standard surgical procedures to secure the mesh to the ventral abdominal wall using an IPOM technique and a suture pattern of their preference. For Procedure B, the skirted mesh was designed so that no modifications were required before use. Surgeons secured the skirted mesh (15×20 cm Ethicon Physiomesh Open Flexible Composite Mesh Device) to the peritoneal layer and underlying musculature using the Ethicon Securestrap Open Absorbable Strap Fixation Device using an IPOM technique. Prior to surgery, the surgeons were given access to the instructions for use (IFU) for the Ethicon products and were instructed to place the straps through the skirted portion of the mesh as directed in the IFU (Figure 1).
The surgeons were instructed in advance to notify the surgical team once half of the mesh fixation for each procedure was completed to permit staff members to collect the mid-fixation saliva samples. For each procedure, the surgeons were permitted to place trans-abdominal stay sutures around the border of the mesh prior to insertion into the abdomen. The surgical start time was defined as the time the surgeon first handled the mesh and the surgical finish time was defined as the time that mesh fixation was complete (i.e., when the last suture knot was tied or fixation strap fired). Following completion of each procedure, the surgeon was instructed to leave the operating room for the postprocedural saliva sample collection. The preclinical veterinary surgeon then removed the first implant device and the second procedure was performed using the same animal.
Saliva collection and analysis
HPA axis activity and ANS arousal were assessed noninvasively using saliva.18 The validity of using salivary cortisol as a measure of the HPA axis and sAA as a surrogate marker of ANS activity has been extensively documented elsewhere.17–21
Saliva samples were collected by an independent study nurse by placing a 1×4 cm absorbent swab (SalivaBio, Carlsbad, CA, USA) under each participant’s tongue for 90 seconds. The samples were defined as the preprocedure sample (collected ~30 minutes before initiating each fixation procedure), the mid-procedure sample (collected at the mid-point of the fixation procedure as dictated by the surgeon), and two postprocedure samples (collected at ~5 and 20 minutes following completion of the fixation).
Following sample collection, samples were placed on dry ice and transferred to −80°C storage. All samples were shipped on dry-ice overnight delivery to the Institute for Interdisciplinary Salivary Bioscience Research (IISBR) for analysis.
Salivary analytes
Samples were thawed and centrifuged to remove mucin. Saliva samples were assayed using a commercially available assay kit for the kinetic measurement of sAA activity (Salimetrics, State College, PA, USA). Cortisol was assayed in duplicate using a commercially available enzyme immunoassay (Salimetrics, Carlsbad, CA, USA). All analyses were performed according to manufacturer’s instructions.
SURG-TLX and task load assessments
The surgeon-reported SURG-TLX questionnaire methodology has been reported elsewhere.14
The first stage of the questionnaire calculates the weighting of the six dimensions using a set of 15 paired comparisons. The dimension with the highest weight is the most important contributing factor for the perceived work-load (scores range from 0 to 5). Then, within 5 minutes of completing the procedure, surgeons were asked to describe their experience of the procedure by rating each of the six domains on a 20-point scale. The scores for each measurement were multiplied by the number of instances recorded for the “pair-wise” comparison for each of the dimensions. The scores for each of the adjusted dimensions were used to generate the overall SURG-TLX score for each procedure and each surgeon.
Analytical strategy
For each of the study end points, the difference between Procedures A and B was calculated for each surgeon and was used to determine the median difference between procedures. Descriptive statistics were calculated for the maximum change from baseline in both the sAA levels and the salivary cortisol levels. The maximum change from baseline in surgeon sAA and cortisol levels was estimated along with a two-sided 97.5% CI for the median difference between the maximum change from baseline recorded for the two mesh fixation methods (Ethicon Securestrap Open Fixation Device with Ethicon Physiomesh Open minus Proceed Surgical Mesh with suture).
For the overall surgeon-reported SURG-TLX score (i.e., the compilation of all task-load components), the median difference was estimated along with a two-sided 95% CI. The median difference in fixation time between the two mesh fixation methods (Ethicon Securestrap Open Fixation Device with Ethicon Physiomesh Open minus Proceed Surgical Mesh with suture) was determined along with a two-sided 95% CI.
Results
Surgical task load
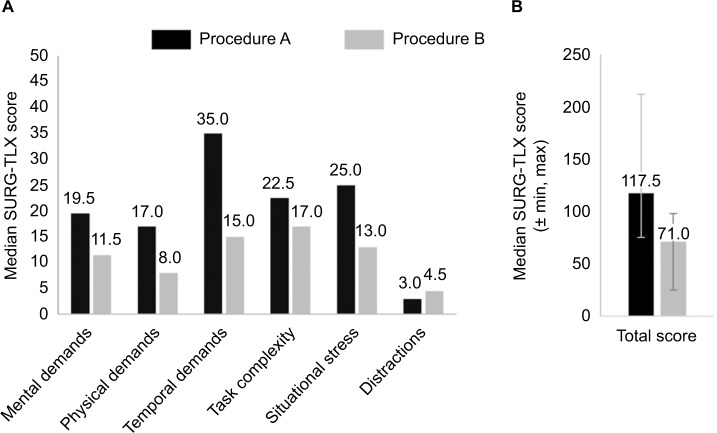
The weighted SURG-TLX results for each fixation procedure are summarized in Table 2. The overall score and the scores for each dimension were lower for Procedure B (skirted mesh and mechanical fixation) compared with Procedure A (flat mesh and traditional suture fixation), with the exception of Distractions. The median difference (95% CI) for the Total (Overall) Weighted Score between procedures was −49.50 (−114.00, −16.00). On average, self-reported surgical stress and demand load were 46.17% lower for surgeons performing a hernia repair using a Securestrap Open Fixation Device with Physiomesh Open (Procedure B) compared with suture fixation with Proceed (Procedure A; Figure 2).
Table 2.
SURG-TLX by procedure
| Dimension | Suture with Proceed
|
Securestrap Open Fixation Device: Physiomesh Open
|
||||
|---|---|---|---|---|---|---|
| Mean (SD) | Median | Min, Max | Mean (SD) | Median | Min, Max | |
| Mental demands | 21.25 (15.21) | 19.5 | 0, 45 | 12.13 (9.76) | 11.5 | 0, 27 |
| Physical demands | 17.38(10.01) | 17.0 | 0, 30 | 8.63(5.18) | 8.0 | 0, 16 |
| Temporal demands | 34.50(13.80) | 35.0 | 16, 60 | 15.63 (7.98) | 15.0 | 5, 28 |
| Task complexity | 27.25 (19.76) | 22.5 | 9, 70 | 14.88 (7.34) | 17.0 | 5, 25 |
| Situational stress | 26.63 (21.25) | 25.0 | 0, 65 | 14.50 (12.68) | 13.0 | 0, 40 |
| Distractions | 3.75 (3.88) | 3.0 | 0, 10 | 4.63(5.07) | 4.5 | 0, 15 |
| Total score | 130.75 (44.97) | 117.5 | 75, 212 | 70.38 (23.94) | 71.0 | 25, 98 |
| Median (95% CI) difference between procedures (Securestrap – Proceed) | −49.50 (−118.00, −16.00) | |||||
Note: Bold values in “Total Score” indicates total workload score determined by aggregating the scores from the six individual dimensions.
Abbreviations: SURG-TLX, surgical task load index; min, minimum; max, maximum.
Figure 2.
(A) Weighted individual SURG-TLX domain scores and (B) total median SURG-TLX scores for all surgeons. Lower median scores were seen with Securestrap compared with Proceed across five out of six SURG-TLX domains.
Notes: Procedure A= traditional hernia repair method with Procced Surgical Mesh and suture fixation; Procedure B= mechanical fixation using Ethicon Physiomesh Open Flexible Composite Mesh Device with Ethicon Securestrap Open Fixation Device.
Abbreviation: SURG-TLX, surgical task load index.
Fixation time
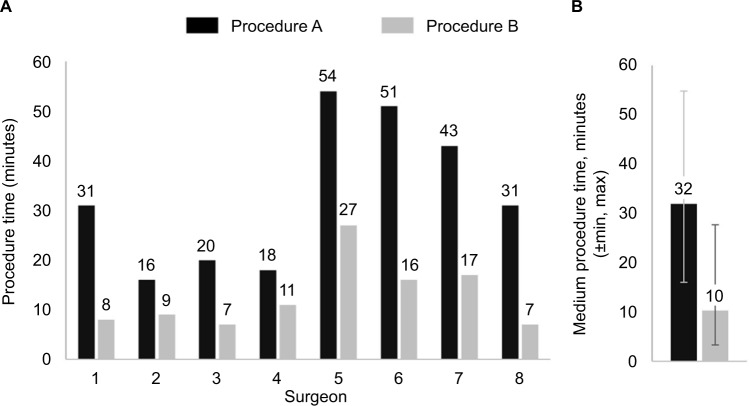
Procedure fixation time reported by each surgeon is summarized in Table 3. The mean (SD) for fixation time for Procedure B was 13.29 (6.89) minutes compared with 33.46 (15.08) minutes for Procedure A, representing a significant reduction in time of 20.17 minutes. The median difference (95% CI) in fixation times between the procedures was −23.64 (−27.15, −6.58) minutes (Figure 3). On average, fixation time was 60.28% lower when using mechanical fixation with Procedure B compared with suture fixation with Procedure A.
Table 3.
Fixation time summary
| Surgeon ID number | Suture with Proceed
|
Securestrap Open Fixation Device with Physiomesh Open
|
||
|---|---|---|---|---|
| Fixation start time | Fixation end time | Fixation start time | Fixation end time | |
| 001 | 11:54 | 12:25 | 13:44 | 13:52 |
| 002 | 13:53 | 14:09 | 11:55 | 12:04 |
| 003 | 11:34 | 11:55 | 13:06 | 13:15 |
| 004 | 14:11 | 14:29 | 12:37 | 12:49 |
| 005 | 14:01 | 14:56 | 12:13 | 12:40 |
| 006 | 12:15 | 13:07 | 14:16 | 14:33 |
| 007 | 12:00 | 12:44 | 14:06 | 14:23 |
| 008 | 14:24 | 14:56 | 13:21 | 13:29 |
| Mean duration of the procedure (SD) | 33.46 (15.08) | 13.29 (6.89) | ||
| Median (95% CI) difference between the duration of procedures (Securestrap – Proceed) | −23.64 (−27.15, −6.58) | |||
Figure 3.
(A) Individual procedural time for each surgeon and (B) median procedural time for all surgeons. Fixation duration was faster for Securestrap Open with Physiomesh Open vs Proceed.
Notes: Procedure A= traditional hernia repair method with Proceed Surgical Mesh and suture fixation; Procedure B= mechanical fixation using Ethicon Physiomesh Open Flexible Composite Mesh Device with Ethicon Securestrap Open Fixation Device.
Abbreviations: min, minimum; max, maximum.
Salivary analytes
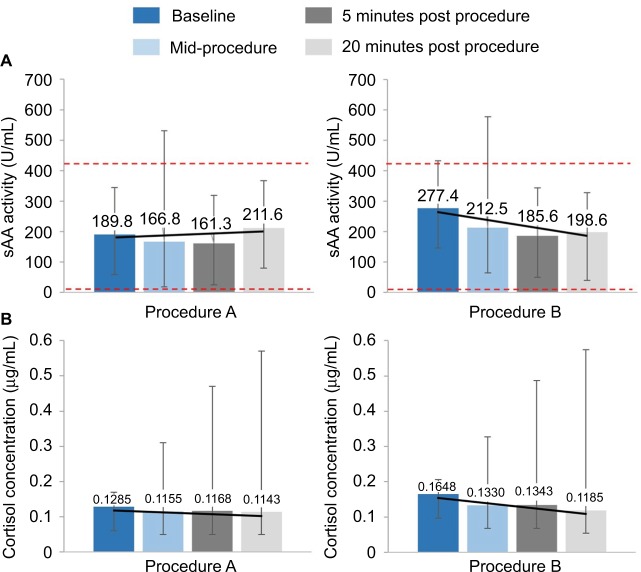
Cortisol concentrations and sAA activity at each time point are shown in Table 4 and Figure 4.
Table 4.
Saliva sAA activity and cortisol concentration by procedure and sampling time point
| Sampling time point | Suture with Proceed
|
Securestrap Open Fixation Device with Physiomesh Open
|
|
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| sAA activity (U/mL) | Baseline | 186.84 (108.67) | 296.86 (218.27) |
| Mid-procedure | 189.75 (167.82) | 266.46 (224.14) | |
| Five minutes post procedure | 166.23 (111.79) | 217.10 (145.54) | |
| Twenty minutes post fixation procedure | 197.72 (98.06) | 226.22 (174.24) | |
| Cortisol concentration (μg/mL) | Baseline | 0.1253 (0.0347) | 0.1836 (0.0960) |
| Mid-procedure | 0.1365 (0.0850) | 0.1709 (0.1364) | |
| Five minutes post procedure | 0.2005 (0.1617) | 0.1912 (0.1281) | |
| Twenty minutes post procedure | 0.2072 (0.1828) | 0.1651 (0.1040) |
Abbreviation: sAA, salivary alpha amylase.
Figure 4.
(A) Median sAA activity (U/mL) and (B) median cortisol concentration (μg/dL) by procedure and sample collection time point.
Notes: Dotted red line represents the normal range for sAA activity (3.1–433.1 U/mL). Trend line is shown in black. All data shown are median ± min, max. Procedure A= traditional hernia repair method with Proceed Surgical Mesh and suture fixation; Procedure B= mechanical fixation using Ethicon Physiomesh Open Flexible Composite Mesh Device with Ethicon Securestrap Open Fixation Device.
Abbreviations: sAA, salivary alpha amylase; min, minimum; max, maximum.
The median differences (95% CI) between the maximum change from baseline of the two procedures for sAA and cortisol were −81.02 (−291.92, 131.36) U/mL and −0.0275 (−0.3290, 0.1105) μg/dL, respectively (Tables 4 and 5). Post-hoc analysis demonstrated that this was caused by variations in cortisol response; four of the eight surgeons had no increase in cortisol across time when performing either Procedure A or B. Among the four surgeons who showed a meaningful increase in cortisol across time, three showed markedly greater cortisol increases when using the suture method in Procedure A compared with the mechanical method used in Procedure B. Only one surgeon had a higher cortisol response when using the mechanical method in Procedure B, and the magnitude of that change was very small relative to the measurement error of the assay.
Table 5.
Median difference in maximum change from baseline in sAA and salivary cortisol
| Median difference | Lower 97.5% CI | Upper 97.5% CI | |
|---|---|---|---|
| sAA (U/mL) | −81.02 | −291.92 | 131.36 |
| Cortisol (μg/mL) | −0.0275 | −0.3290 | 0.1105 |
Abbreviation: sAA, salivary alpha amylase.
Discussion
Surgeon stress can impact overall performance and lead to surgical errors that, in turn, can adversely influence patient outcomes. Workload, procedural complexity, and time constraints are primary causes of such stress.9,22 Addressing the causes of surgeon stress has the potential to help improve surgical performance, leading to better patient outcomes, a decrease in the length of hospital stays, and ultimately, a reduction in procedural costs.9,22 Surgical procedure length is of particular importance as longer procedures are correlated with complications such as an increase in infections, resulting in longer hospital stay and greater readmission rates.23–26
Mechanical fixation devices are designed to facilitate fixation and are expected to reduce procedure time compared with other mesh repair methods that rely on suture fixation. Skirted meshes provide a matrix to further facilitate fixation by providing a preformed platform for tacker placement and do not require any modification prior to use. Combining both devices in IPOM hernia repairs should further reduce procedure time and decrease surgeon-perceived stress. The results from this study confirmed this hypothesis, demonstrating that procedure time, surgical stress, and demand loads were reduced when using mechanical fixation with a skirted mesh. These results support the results observed in a previous study, which demonstrated reductions in surgeon stress measured by SURG-TLX and faster fixation times.15
In this study, the concentrations of both sAA and cortisol were measured before, during, and after completing IPOM repairs to evaluate the biobehavioral response to stress associated with both procedures. The median differences and 97.5% CI in the maximum change from baseline concentrations of sAA and cortisol were generally consistent with the behavioral data above. However, there was evidence of individual differences in the surgeons’ physiological reactivity to the procedures, with a greater proportion of surgeons exhibiting larger HPA axis reactivity when using the suture fixation method compared with the mechanical method. This suggests that there was a reduction in HPA activity and ANS arousal when using Procedure B (Securestrap Open Fixation Device in conjunction with Physiomesh Open procedure) compared with using Procedure A (suture with Proceed procedure).
This study is associated with several limitations. The procedural time measurement started after handing the surgeon the mesh and so the time required to alter the mesh before use was included as part of this measurement. Consequently, the experimental design would provide a small benefit to the skirted mesh as the design required no trimming before use. To minimize bias and mitigate anticipatory stress, surgeons were randomized to the order in which each procedure would be performed. However, as described above, it was not possible to blind the study after the surgeon had performed the first surgery. Although designed to be robust and to closely mimic the clinical operating room situation, the study was performed in a porcine model which does not fully reproduce the human surgical experience. In addition, accurate surgical exposure of the hernia ring is a critical part of hernia repair in surgical practice; however, for this study model the hernia was simultaneously created and exposed by the study veterinarian; participating surgeons only performed the fixation portion of the surgery. Finally, the sample size for this pilot study was relatively small, although it was determined to be large enough to permit assessment of all study end points.
The baseline concentrations of sAA and cortisol were 277.4 and 189.8 U/mL, and 0.1648 μg/dL and 0.1285 μg/dL, respectively, for surgeons starting Procedure B and Procedure A. A possible explanation for the elevated baseline sAA and cortisol levels observed for the Securestrap Open Fixation Device may have been the blinding method used, as it was only possible to blind the first procedure. Consequently, the elevation may be an indicator of perceived excitement for a novel task, as all surgeons were naïve to this method. For example, sAA has been reported to be an indicator of the early fight/flight response preparing an individual to react to perceived stimuli.27
The results of this study may inform future studies designed to assess the correlation of stress with other confounding factors associated with mechanical fixation procedures. Understanding how surgical performance is affected by factors such as distractions, fatigue, and overall familiarity with the surgical procedure and devices, may help explain the variability observed between surgeons. Additional studies could also confirm the optimal saliva sampling time points (before, during, and after surgery) in order to better align the measurement of salivary biomarkers with other physiological markers of stress including blood pressure and pulse rate.
Conclusions
This pilot study provides preliminary findings suggesting that mechanical fixation with the Ethicon Securestrap Open Absorbable Strap Fixation Device in open IPOM repair using the Ethicon Physiomesh Open Flexible Composite Mesh Device has the potential to reduce surgeon stress, as evidenced by a reduction in perceived workload stress, fixation time, and physiological reactivity to the intraoperative experience. Future studies could focus on determining whether the reduction in stress is also observed in a real-life setting, and whether this results in reduced surgical errors and improved patient outcomes.
Acknowledgments
Sponsorship for this study and article processing charges were funded by Ethicon, Inc., a subsidiary of Johnson & Johnson. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. The authors acknowledge the significant contributions of Vivienne Mendoza, Preclinical Research Assistant, who functioned as the research coordinator for the study, and Diana Frisica who managed saliva sample collection and shipment for the study. In addition, we acknowledge the contributions of Kelly Henning, IISBR program manager, and former Ethicon employees who helped with the preparation of the study protocol and conduct. These include Benjamin Kamhi (Data Management), Jessica Panish (Health Economics and Market Access-protocol development), Martin Chomiak (Marketing-study sponsor), and Ross Saunders (Marketing-study sponsor). Medical writing and editorial support were provided by Simon Foulcer, PhD, Costello Medical Consulting Ltd, which was funded by Ethicon Inc.
Footnotes
Author contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosure
DAG is the founder and chief scientific and strategy advisor at Salimetrics LLC and SalivaBio LLC and the nature of these relationships have been managed by the policies of the committees on conflict of interest at the Johns Hopkins University School of Medicine and the University of California at Irvine. NS, MHM, JL, BI, and PH are employees of Ethicon. The authors report no other conflicts of interest in this work.
References
- 1.Bosanquet DC, Ansell J, Abdelrahman T, et al. Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 patients. PLoS One. 2015;10(9):e0138745. doi: 10.1371/journal.pone.0138745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillion JF, Sanders D, Miserez M, Muysoms F. The economic burden of incisional ventral hernia repair: a multicentric cost analysis. Hernia. 2016;20(6):819–830. doi: 10.1007/s10029-016-1480-z. [DOI] [PubMed] [Google Scholar]
- 3.Nunoo-Mensah JW, Rosen M, Chan LS, Wasserberg N, Beart RW. Prevalence of intra-abdominal surgery: what is an individual’s lifetime risk? South Med J. 2009;102(1):25–29. doi: 10.1097/SMJ.0b013e318182575b. [DOI] [PubMed] [Google Scholar]
- 4.Beadles CA, Meagher AD, Charles AG. Trends in emergent hernia repair in the United States. JAMA Surg. 2015;150(3):194–200. doi: 10.1001/jamasurg.2014.1242. [DOI] [PubMed] [Google Scholar]
- 5.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045–1051. v–vi. doi: 10.1016/S0039-6109(03)00132-4. [DOI] [PubMed] [Google Scholar]
- 6.Plymale MA, Ragulojan R, Davenport DL, Roth JS. Ventral and incisional hernia: the cost of comorbidities and complications. Surg Endosc. 2017;31(1):341–351. doi: 10.1007/s00464-016-4977-8. [DOI] [PubMed] [Google Scholar]
- 7.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang MK, Holihan JL, Itani K, et al. Ventral hernia management: expert consensus guided by systematic review. Ann Surg. 2016 doi: 10.1097/SLA.0000000000001701. [DOI] [PubMed] [Google Scholar]
- 9.Wetzel CM, Kneebone RL, Woloshynowych M, et al. The effects of stress on surgical performance. Am J Surg. 2006;191(1):5–10. doi: 10.1016/j.amjsurg.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 10.Moorthy K, Munz Y, Dosis A, Bann S, Darzi A. The effect of stress-inducing conditions on the performance of a laparoscopic task. Surg Endosc. 2003;17(9):1481–1484. doi: 10.1007/s00464-002-9224-9. [DOI] [PubMed] [Google Scholar]
- 11.Roy S, Shnoda P, Savidge S, Hammond J, Panish J, Wilson M. Reduction in fixation time and related surgical stress with the use of Ethicon Securestrap™ open absorbable strap fixation device in the deployment of intra-peritoneal onlay mesh (IPOM) for open ventral hernia repair. Value Health. 2013;16(7):A486. [Google Scholar]
- 12.Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228(3):320–330. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sajid MS, Parampalli U, McFall MR. A meta-analysis comparing tacker mesh fixation with suture mesh fixation in laparoscopic incisional and ventral hernia repair. Hernia. 2013;17(2):159–166. doi: 10.1007/s10029-012-1017-z. [DOI] [PubMed] [Google Scholar]
- 14.Wilson MR, Poolton JM, Malhotra N, Ngo K, Bright E, Masters RS. Development and validation of a surgical workload measure: the surgery task load index (SURG-TLX) World J Surg. 2011;35(9):1961–1969. doi: 10.1007/s00268-011-1141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy S, Hammond J, Panish J, Shnoda P, Savidge S, Wilson M. Time savings and surgery task load reduction in open intraperitoneal onlay mesh fixation procedure. Sci World J. 2015;2015:340246. doi: 10.1155/2015/340246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsigos C, Chrousos GP. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. J Psychosom Res. 2002;53(4):865–871. doi: 10.1016/s0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- 17.Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34(4):486–496. doi: 10.1016/j.psyneuen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Granger DA, Fortunato CK, Beltzer EK, Virag M, Bright MA, Out D. Focus on methodology: salivary bioscience and research on adolescence: an integrated perspective. J Adolesc. 2012;35(4):1081–1095. doi: 10.1016/j.adolescence.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier Social Stress Test’-a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28(1–2):76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- 20.Kirschbaum C, Hellhammer DH. Salivary cortisol in psychoneuroendocrine research: recent developments and applications. Psychoneuroendocrinology. 1994;19(4):313–333. doi: 10.1016/0306-4530(94)90013-2. [DOI] [PubMed] [Google Scholar]
- 21.Nater UM, Rohleder N, Gaab J, et al. Human salivary alpha-amylase reactivity in a psychosocial stress paradigm. Int J Psychophysiol. 2005;55(3):333–342. doi: 10.1016/j.ijpsycho.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147(3):318–330.e316. doi: 10.1016/j.surg.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Procter LD, Davenport DL, Bernard AC, Zwischenberger JB. General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg. 2010;210(1):60–65.e62. doi: 10.1016/j.jamcollsurg.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 24.Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(3):420–427. doi: 10.1016/j.jamcollsurg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen MT, Li LT, Hicks SC, et al. Readmission following open ventral hernia repair: incidence, indications, and predictors. Am J Surg. 2013;206(6):942–948. doi: 10.1016/j.amjsurg.2013.08.022. discussion 948–949. [DOI] [PubMed] [Google Scholar]
- 26.Williams S, Bottle A, Aylin P. Length of hospital stay and subsequent emergency readmission. BMJ. 2005;331(7513):371. doi: 10.1136/bmj.331.7513.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chatterton RT, Jr, Vogelsong KM, Lu YC, Hudgens GA. Hormonal responses to psychological stress in men preparing for skydiving. J Clin Endocrinol Metab. 1997;82(8):2503–2509. doi: 10.1210/jcem.82.8.4133. [DOI] [PubMed] [Google Scholar]