Abstract
Introduction
Varicella, although a frequently benign childhood disease, nevertheless represents a considerable health burden. WHO recommends including varicella vaccines in universal routine vaccination programs, and maintaining coverage >80%. Many countries have successfully introduced varicella vaccination and have benefited from lower disease burden, but many others have not adopted the vaccine. Reasons include cost commitment for a ‘mild childhood disease’ or concerns that vaccination will shift varicella to older age groups or increase herpes zoster incidence.
Areas covered
This literature review summarizes the effectiveness and epidemiological impact of varicella immunization programs.
Expert commentary
Varicella vaccines are immunogenic with acceptable safety profiles. One and two dose schedules are highly effective against varicella and large reductions in disease incidence, particularly moderate-severe disease, have been widely reported. There is currently no evidence to suggest that the introduction of varicella vaccination results in a shift of varicella disease burden to older age groups. Although epidemiological studies have shown an increased incidence of herpes zoster since the vaccines were launched, there are many other contributing factors, and indeed, this secular trend was evident before their introduction. In conclusion, varicella vaccination easily fits into existing immunization programs and significantly reduces the often underestimated burden of varicella.
Keywords: Varicella, herpes zoster, vaccines, effectiveness, immunization
1. Introduction
Varicella-zoster virus (VZV) causes both varicella (also known as chickenpox) and herpes zoster (HZ, also known as shingles). Varicella is a common childhood disease, which usually confers lifetime immunity, whereas HZ arises when dormant VZV in the nerve ganglia reactivates in previously infected individuals [1]. HZ usually occurs later in life, with ≥95% immunocompetent individuals over 50 years of age being seropositive for VZV and at risk of developing HZ [2]. The lifetime risk for HZ is around 32% [1].
Varicella is not a universally notifiable disease, but standardized annual incidence rates from 300–1291 per 100,000 population have been reported in Europe [3]. Although varicella is mainly benign in children, serious complications can develop [4], and in 2014, the World Health Organization (WHO) estimated that approximately 4.2 million severe complications leading to hospitalization and 4200 related deaths occur globally each year [5]. In the pre-vaccination era, approximately 30.9 per 100,000 varicella cases were hospitalized in the United States [6], and 0.41 cases per million population were fatal [7]. However, post-licensure, varicella-related hospitalizations decreased to 14.5 per 100,000 cases [6], and deaths to 0.05 per million population [7]. Varicella is usually more severe in adults, with those aged ≥45 years having 4–50 times greater risk of hospitalization and 174-fold higher risk of dying than individuals aged 5–14 years [8]. Nevertheless, it should be noted that the burden of hospitalization is highest in immunocompetent or previously healthy individuals [9,10].
The main burden of varicella disease is economic due to the high number of cases and the need for parents and caregivers to look after their children. Noncomplicated cases tend to last for up to 2 weeks [11], during which time affected children will not be able to attend day care or school. It has recently been reported that in Sweden, one in four parents needs to take time off from work to care for children with varicella [12]. The indirect costs associated with parents taking time off from work make a significant but potentially underestimated contribution to the economic impact of VZV infection [13–16].
Varicella vaccines are highly effective in reducing the global incidence and burden of the disease [17]. The vaccine, as a frozen formulation, was licensed for use in 1984 and was the first commercially available varicella vaccine. It subsequently became the first refrigerator-stable varicella vaccine, its development commenced in 1991, and it has been licensed for use since 1994 [18]. Although not universally adopted, WHO recommends that in countries where varicella is an important public health burden, varicella vaccination should be introduced into their routine immunization programs [17].
Varicella dosing recommendations can include one or two doses, separated by a long or short dosing interval. The most common schedule comprises a first dose at 12–18 months followed, if adopted, by a second dose at between 4 and 6 years of age. Alternatively, the second dose can be administered in children below 4 years of age, provided that 3 or more months have elapsed since the first dose [19,20]. Although it is assumed that a shorter interval may be optimal in terms of epidemiologic impact, pragmatically some countries retain longer intervals to better fit with their childhood vaccination programs [19].
A single-dose schedule is effective at controlling severe disease, but varicella breakthrough still occurs [21–24]. Alternatively, the addition of a second dose provides protection against all severities [25]. The economics of implementing one- or two-dose schedules have been widely debated [20,26,27], but national choices will ultimately depend on whether their priorities are varicella elimination or prevention of severe disease. Interestingly, a recent modeling study from Italy demonstrated that out of coverage, efficacy, number of doses, or dosing interval, high coverage is the critical success factor [28]. Indeed, WHO has already recommended that vaccine coverage should be maintained above 80% [17].
The varicella vaccine can be administered as a monovalent vaccine (e.g. Varilrix; GSK, Belgium or Varivax; Merck & Co. Inc., USA) [29,30] or combined with the measles, mumps, and rubella vaccine as a quadrivalent vaccine (MMRV; e.g. Priorix-Tetra; GSK, Belgium or ProQuad; Merck & Co. Inc., USA) [31,32]. The immunogenicity and safety of both the varicella monovalent vaccine and MMRV are well established and have been extensively reviewed [18,33]. As there is no accepted correlate of immunity for varicella, efficacy data provide more clinically relevant information than immunologic data and the efficacy of varicella-containing vaccines in preventing VZV infections has been widely studied and reviewed [34]. High levels of long-term protection have been observed after both single and two-dose schedules [35,36].
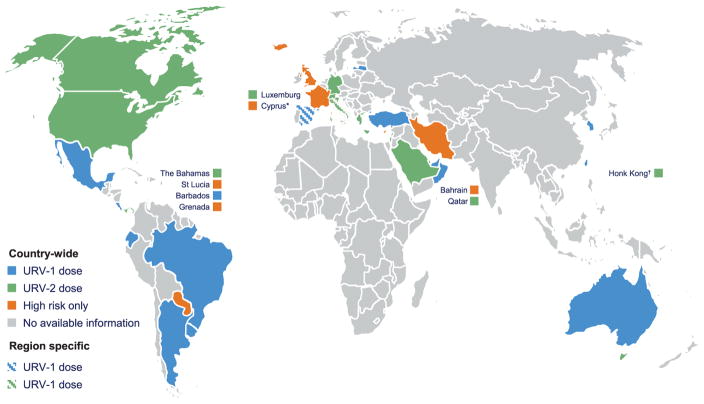
In December 2014, varicella vaccines were recommended in 33 predominantly higher socioeconomic status countries (Figure 1), implying that despite established effectiveness, many countries still do not routinely vaccinate children against VZV. Reasons for low adoption could include cost of implementation for a ‘mild childhood disease,’ or fears that vaccination may shift the disease to older individuals in whom the disease is more severe or may increase the incidence of HZ [3]. We therefore undertook this review to ascertain the effectiveness of the varicella vaccine and its impact upon disease-associated morbidity and mortality, as well as determining whether there is any published evidence to support either an age-shift in varicella incidence or an increased incidence of HZ.
Figure 1.
World map representing different national universal routine vaccination (URV) schedules against varicella (national-level guidelines are represented, unless specific region data was publically available). *In Cyprus, varicella vaccination is administered universally in the private sector. †Varicella URV is recommended in Hong Kong, but not yet implemented [7,37,42,70,72,115,116].
2. Evidence for varicella vaccination
2.1. Effectiveness
Vaccine effectiveness (VE), defined as the measure of protection attributable to a vaccine administered under field conditions to a given population [43], provides an estimate of the effect of vaccines in real-world settings. The effectiveness of the varicella vaccine has been assessed in outbreak, case-control and longitudinal, database, observational, and modeling studies, of which outbreak studies are the most numerous.
Table 1 presents the results from individual studies showing the VE of the varicella vaccine. As can be seen, VE is influenced by a number of factors including the number of administered doses, disease severity, and age at which the vaccine is administered [25,44]. VE for one dose of varicella vaccine against any disease ranged from 55% to 87%, while after two doses, the VE ranged between 84% and 98% [23,44–46]. VE was higher against moderate or severe disease, ranging from 70% to 98% after one dose and 94% to 98% after two doses [23,47]. Two studies from Israel [48] and Korea [49] recorded much lower VE – in case of Israel, this was most probably due to the very low coverage (37%) [48] and in the case of Korea was due to the ineffectiveness of one of the administered vaccines [49]. With these exceptions, the ranges shown are consistent with previous reviews [50,51]. Additionally, in the recent meta-analysis from Marin et al., VE against all varicella was estimated as 81% after one and 92% after two vaccine doses and as 98% after one dose for moderate/severe varicella [25]. Further, the incremental VE of two doses over one has recently been calculated as 84.6% [52].
Table 1.
Effectiveness of varicella vaccines.
| Outbreak investigations
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Country [Reference] | Setting | Vaccine | N vaccinated cases | Vaccinated population | Vaccine doses | VE (%) (CI)
|
Vaccine coverage (%) | |
| Any disease | Moderate/severe disease | |||||||
| Germany [23] | Prospective, 7 day-care centers | Varilrix | 19 | 77 | 1 | 56 (29–72) | 86 (62–95) | 62 (49–81) |
| Priorix-Tetra | 7 | 38 | 1 | 55 (8–78) | 70 (4–90) | |||
| 2 | 56 | 2 | 91 (65–98) | 94 (54–99) | ||||
| Varivax | 4 | 48 | 1 | 86 (56–96) | 96 (67–99) | |||
| Italy [117] | Day-care center/elementary school | NR | 17 | 210 (Day care) | 1 | 60 (48–70) | – | 86.6 |
| 358 (School) | 1 | 69 (51–88) | – | 51.9 | ||||
| Italy [24] | Preschool | NR | 7 | 55 | 1 | 82.4 | – | 53.9 |
| USA [45] | Prospective elementary and affected schools | NR | 16 | 109 | 1 | 81 (67–89) | – | 32.7 |
| 9 | 220 | 2 | 95 (89–97) | – | 66.1 | |||
| 13 | 85 | 1 | 80 (64–89) | – | 31.4 | |||
| 22 | 181 | 2 | 84 (74–90) | – | 66.8 | |||
| Taiwan [118] | Elementary school | NR | 10 | 321 | NR | 69–100 | 86 | 71.2 |
| Israel [48] | Day-care centers | NR | 37 | 89 | NR | 20 (0–40) | 93 (75–98) | 37 |
| Case-control studies
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Country [Reference] | Setting | Vaccine | N cases | N matched controls | Vaccine doses | VE (%) (CI)
|
Vaccine coverage (%) | |
| Any disease | Moderate/Severe disease | |||||||
| Germany [47] | Pediatric practices | Any | 432 | 432 | 1 | 86 (77–92) | 98 (91–99) | 13.2 (Cases); 45.1 (controls) |
| OKA/GSK | 35 | 63 | 1 | 72 (49–84) | 95 (78–99) | |||
| China [53] | General community | Any | 1000 | 1000 | 1 | 84 (77–89) | – | 19 |
| Varilrix | 1 | 86 (73–93) | – | |||||
| China [54] | Schools and day-care centers | Any | 180 | 679 | 1 | 83 (71–90) | – | 10.0 (Cases); 34.5 (controls) |
| USA: New Haven, Connecticut [119] | Pediatric practices | Any | 202 | 389 | 1 | 85 (78–90) | 97 (93–99) | 23 (Cases); 61 (controls) |
| USA: New Haven, Connecticut [44] | Pediatric practices | Any | 339 | 669 | 1 | 87 (81–91) | – | 36 (Cases); 70 (controls) |
| Note that this study expands upon results from the same source as Ref. [119] above | ||||||||
| USA: New Haven, Connecticut [46] | Pediatric practices | Any | 66 | 117 | 1 | 86 (−45–99) | – | 93.0 (Cases); 83.6 (controls) |
| Note that this study expands upon results from Refs. [119] and [44] above | 0 | 22 | 2 | 98 (84–100) | – | 0 (Cases) 15.7 (controls) | ||
| USA: Antelope Valley CA, Philadelphia [120] | Immunization registries | Any | 32 (1–3 years) | 103 (1–3 years) | 1 | 76 (39–90) | 78 (13–95) | |
| 93 (≥4 years) | 305 (≥4 years) | 2 | 94 (76–98) | 98 (83–100) | – | |||
| Korea [49] | National Notifiable Disease Surveillance | 1 MAV 3 OKA |
537 | 537 | 1 | 13 (−17–36) | – | – |
| Longitudinal, database, observational, and modeling studies
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Country [Reference] | Setting | Vaccine | N cases | Sample size | Vaccine doses | VE (%) (CI)
|
Vaccine coverage (%) | |
| Any disease | Moderate/Severe disease | |||||||
| Turkey [21] | Well-child clinic and private pediatrician | Various | 466 | 1683 | 1 | 62 (57–66) | – | 60.1 |
| No vaccine | 723 | 1119 | 0 | – | ||||
| Germany [121] | Primary care modeling | Various | 679 | NR | 1 | 83 (80–86) | – | 78 |
| Germany [52] | Linear modeling based on Sentinel data | Various | 8153 | 31,288 | 1 | 87 (85–88) | – | 28.8 |
| 2 | 97 (97–98) | 58.8 | ||||||
CI: confidence intervals; N: number; NR: not reported; VE: vaccine effectiveness.
Several studies have been undertaken to assess whether VE wanes over time [22,54,55]. In the longest study to date, VE showed no reduction against any severity varicella disease for up to 14 years [55]. These findings were reinforced by other works [22,54], and although a generally accepted correlate of protection has not yet been identified for varicella, these studies suggest that VE mirrors antibody persistence [53–55].
Despite the effectiveness of the vaccine, low-level breakthrough varicella does however occur. Individual studies have reported incidences ranging from 8% to 32% after single-dose varicella vaccine [21–24], and 4% after two doses [23].
2.2. Impact of varicella vaccination on varicella incidence, morbidity, and mortality
The impact of vaccination is expressed as the proportionate reduction in disease burden, comparing incidences and mortality rates in the same population between the pre-vaccine era and after vaccine implementation [43]. Table 2 shows the difference in varicella incidence rates occurring before vaccination was implemented to that after one and two-dose schedules were introduced. All studies have shown impressive reductions in disease incidence compared with the pre-vaccination era. After one-dose programs, reductions up to 74% have been recorded [56]. Whereas reductions exceeding 90% have been recorded after two-dose schedules [37,57,58].
Table 2.
Decrease in incidence rates following the implementation of varicella vaccination.
| Country [Reference] | Data source | Year introduced | Doses compared | Years compared | Change |
|---|---|---|---|---|---|
| Germany [59] | Sentinel data | 2004 (Dose 1) | 0 vs. 1 | 2009 vs. 2005 | ↓55% |
| Munich, Germany [60] | Annual parent surveys. Monthly pediatric practice surveillance, pediatric hospital databases | 2009 (Dose 2) | 0 vs. 1 | 2008–9 vs. 2006–7 | 4.0 vs. 6.6 cases/1000 |
| 0 vs. 2 | 2010–11 vs. 2006–7 | 2.2 vs. 6.6 cases/1000 | |||
| 1 vs. 2 | 2010–11 vs. 2008–9 | 2.2 vs. 4.0 cases/1000 | |||
| Italy [61] | Regional surveillance | 2005 | 0 vs. 1 | 2008 vs. 2000–7 | ↓51% |
| Italy; Sicily [57] | National Surveillance System | 2003 (Dose 1) 2010 (Dose 2) |
0 vs. 2 | 2012 vs. 2003 | ↓95% |
| Italy; Tuscany [38] | Regionally notified varicella cases | 2008 | 0 vs. 1 | 2009–12 vs. 2004–7 | 0.89 vs. 2.3 cases/1000 |
| Italy; Apulia, Sicily, Veneto [122] | Statutory notification, National Hospital Discharge, mortality data | 2003 (Dose 1) 2010 (Dose 2) |
0 vs. 2 | 2010 vs. 2001–9 | 103 vs. 151 cases/100,000 |
| Spain; Navarre [37] | Regional surveillance data | 2007 | 0 vs. 2 | 2012 vs. 2006 | 1.0 vs. 50 cases/1000 (↓98.1%) |
| USA; Connecticut [62] | Varicella surveillance data | 1995 (Dose 1) 2006 (Dose 2) |
1 vs. 2 | 2014 vs. 2009 | 5.1 vs. 13.8/100,000 (p < .001) |
| USA [58] | Kaiser group | 1995 (Dose 1) 2006 (Dose 2) |
0 vs. 2 | 2009 vs. 1995 | 1.3 vs. 25.8/1000 person-years (↓90–95%) |
| USA [123] | Population-based active surveillance | 1995 (Dose 1) 2006 (Dose 2) |
0 vs. 2 | 2013–14 vs. 2005–6 | 3.9 vs. 25.4/100,000 population (↓85%) |
| USA, Washington State [63] | Group Health Cooperative | 1995 (Dose 1) | 0 vs. 1 | 2002 vs. 1992 | 2.63 (1995); 2.29 (1998); 0.92 (2002) cases/1000 |
| Taiwan [64] | National Health Insurance Claims Database | 2004 (Mass vaccination) | 0 vs. 1 | 2008 vs. 2000 | 2.23 vs. 8.28 cases/1000 |
| Taiwan [65] | National Health Insurance Claims Database | 2004 (Mass vaccination) | 0 vs. 1 | 2004–8 vs. 2000–3 | Non-specified significant reduction |
| Costa Rica [56] | National surveillance data | 2007 | 0 vs. 1 | 2015 vs. 2008 | ↓73.8% (↓79% <5 years) |
Many studies have also shown that vaccination is associated with a significant decrease in varicella-related hospitalization rates (Table 3; ranging from 23% to 93% over a 4–14-year time period) [6,37,60,61,64–69]. The highest reductions were observed in individuals below 15 years old [6,37,60,61,65–67] and specifically in the youngest children [38,62,69]. Some studies found a relatively small decrease in varicella hospitalization rates [6,60,61,66,67,70], possibly due to reduced vaccination coverage and shorter study periods. Recently, Mota et al., who studied VZV-related hospitalizations and mortality in Brazil from 1996 to 2011, showed that average annual mortality rates for varicella in Brazil before vaccine implementation were 0.88/100,000 in infants under 1 year and 0.40/100,000 in children aged 1–4 years [71].
Table 3.
Decrease in hospitalization rates following the implementation of varicella vaccination.
| Country [Reference] | Data source | Year introduced | Doses compared | Years compared | Change |
|---|---|---|---|---|---|
| Germany [69] | National hospital discharge data | 2004 (1 dose) 2006 (2 doses) |
0 vs. 2 | 2005–12 vs. 1995–2003 | 1.9 vs. 3.3/100,000 |
| Germany; Munich [60] | Annual parent surveys. Monthly pediatric practice surveillance, pediatric hospital databases | 2004 | 0 vs. 1 | 2009 vs. 2005 | 4.3 vs. 7.6/100,000 (↓43%) |
| Germany; Bavaria [124] | Pediatric hospital discharge data | 2004 | 0 vs. 1 | 2011 vs. 2005 | ↓60% |
| Italy [61] | Regional surveillance | 2005 | 0 vs. 1 | 2007–8 vs. 2000 | ↓53% |
| Italy; Tuscany [38] | Regionally notified varicella cases | 2008 | 0 vs. 1 | 2009–12 vs. 2004–7 | 2.2 vs. 4.1/100,000 |
| Italy; Sicily [57] | National Surveillance System | 2003 | 0 vs. 2 | 2012 vs. 2003 | 0.8 vs. 4.8/100,000 |
| Italy [72] | Aggregate regional data | 2003–13 | 0 vs. 2 | 2012 vs. 2004 | ↓75% |
| Spain; Navarre [37] | Regional surveillance data | 2007 | 0 vs. 2 | 2012 vs. 2006 | ↓89% |
| Spain [70] | Hospital discharge data | 2006 (2 doses) | 0 vs. 2 | 2010 vs. 2005 | 37 vs. 47/100,000 (Children < 5 years) |
| Israel; Tel-Aviv [125] | Retrospective hospital chart review | 2008 | 0 vs. 2 | 2009–12 vs. 2004–8 | ↓63% (↓75% in 1–6 years) |
| Canada [73] | Hospital discharge database | 2000–6 (1 dose) 2010 (2 doses) |
0 vs. 1 | 2010 vs. 1990 | >70%↓ (All ages less than 40) |
| Australia; Victoria [66] | Medical consulting data | 2005 | 0 vs. 1 | 2007 vs. 2000 | ↓23% (Annual 7% reduction) |
| Australia [74] | National hospital morbidity database | 2005 | 0 vs. 1 | 2006–10 vs. 1998–9 | ↓52.7% |
| USA [58] | Kaiser group | 1995 (Dose 1) 2006 (Dose 2) |
0 vs. 2 | 2009 vs. 1994 | 0.25 vs. 2.13/100,000 (↓90%) |
| USA [68] | Truven claims data | 1995 (Dose 1) 2006 (Dose 2) |
0 vs. 2 | 2012 vs. pre-vaccination | ↓93% (↓38% vs. one dose period) |
| USA; Connecticut [126] | Hospital discharge data | 1995 (Dose 1) 2006 (Dose 2) |
0 vs. 1 | 2001–5 vs. 1994–5 | ↓83% (p < 0.001) |
| Taiwan [65] | National Health Insurance Claims Database | 2004 | 0 vs. 1 | 2004–8 vs. 2000–3 | Non-specified significant reduction |
| Costa Rica [56] | ational surveillance data | 2007 | 0 vs. 1 | 2015 vs. 2008 | ↓85.9% (↓87% (<5 years)) |
In the United States, few years after the implementation of the varicella vaccination program, significant reductions in varicella-related deaths, compared with the 5 years preceding the vaccination program, were demonstrated (92% in children 1–4 years, and 74–89% in infants <1 year and persons 5–49 years) [75].
2.3. Shift in varicella to older age groups
Data from the United States suggested an upward shift in the age distribution of varicella, as a result of childhood vaccination programs [76]. For example, surveillance data from Antelope Valley indicated a shift in varicella incidence peaks, from 3 to 6-year olds (in 1995) to 9–11-year olds (in 2004) [77]. Mathematical models predicted that the age shift occurred if coverage rates fell below 80–85% [78]. Such observations have prompted WHO to recommend that coverage rates above 80% should be achieved and maintained [79]. However, the number of varicella cases and varicella-related hospitalizations in the whole population fall after vaccine introduction; there does not appear to be an age shift. Furthermore, recent surveillance data from different countries have shown a reduction in the VZV incidence in all age groups [80] or under the age of 40 [74], suggestive of a herd effect.
When introducing a vaccine for routine childhood vaccination, there may be immunity gaps in older individuals, necessitating a catchup program. Some countries, such as Australia, have therefore implemented varicella vaccination of older individuals to prevent any potential shift to older age groups, despite available evidence suggesting that varicella rates still decrease in unvaccinated groups [6,59,67,73,74,77]. A two-dose schedule is recommended for adolescents and adults, as clinical trials have indicated a low response rate after single-dose varicella vaccination in these age groups [81,82].
2.4. Varicella vaccination and the incidence of HZ
In 2000, a model by Brisson et al. theoretically linked the implementation of universal varicella vaccination in children to an increased incidence of HZ, in the short and medium term following vaccination, in older populations [83]. In the long term, however, a decreasing incidence of HZ is expected to occur, assuming that vaccinated individuals are less likely to develop zoster when compared to naturally infected individuals [73]. The theory behind this model is that exogenous boosting by VZV exposure is needed to maintain cell-mediated immunity above a threshold and reduce the risk of developing HZ [84–86]. Further models have calculated that a temporary increase in HZ incidence, as a result of varicella vaccination, could be anticipated over the next 50–70 years [87,88]. As a potential increase in HZ can have implications on acceptability to a population and also on cost calculations [89,90], such observations can cause a delay or rejection of the varicella vaccination into national programs.
Epidemiological studies on the long-term trend of HZ show that the incidence of HZ has increased more than 4 times over the last six decades among all age groups and both sexes [91–93]. Although some studies show an increase in the HZ incidence after the introduction of varicella immunization program [64,69,94–97], others have shown no increase [63] and there is no concrete evidence to attribute this trend directly to varicella vaccination (Table 4) [70,98–101]. Otherwise, there is some evidence that children vaccinated for varicella have lower risk of developing HZ than those with history of varicella [102,103]. A review by Ogunjimi et al. concluded that although exogenous boosting plays a role in HZ incidence, its magnitude has yet to be accurately determined [104]. For example, increased oral corticosteroid use [105], chronic comorbid conditions [106–110], stress [107,110], and an increasing elderly population [111,112] all have an impact on the incidence of HZ. In addition, endogenous boosting, i.e. the subclinical reactivation of the latent VZV due to internal factors, can also play a role in boosting the anti-varicella immune response and hence changes in the incidence of HZ [113]. More research into the pathophysiology of HZ is warranted, particularly with reference to the endogenous and exogenous boosting hypotheses.
Table 4.
HZ incidence and varicella vaccination.
| Country [Reference] | Study design | Sample | Age at vaccination | Year introduced | Years compared | Change in incidence |
|---|---|---|---|---|---|---|
| Spain [70] | Hospital discharge data | 27,236 HZ discharges | Dose 1 at 15–18 months/susceptible adolescents | 2006 | 2010 vs. 2005 | 10.9 vs. 9.7/100,000 (>84 years: 98 vs. 70) Hospitalization rates |
| Canada; Ontario [101] | Retrospective analysis | 13.2 million | Dose 1 at 12–15 months Dose 2 at 4–6 years |
2005a | 2005–9 vs. 1992–8 | 303 vs. 309/100,000 |
| Australia; New-South Wales [99] | Hospitalizations, antiviral prescriptions; presentations | Dose 1 at 18 months Catch-up: 12–13 years |
2005 | 2006–7 vs. 1998–9 | Annual age-specific hospitalization rates: 3.7%↓ (20–39 years); ↑1.6% (40–59 years) | |
| Australia [94] | Retrospective analysis of management encounters | 1,078,671 Encounters | Dose 1 at 18 months Catchup: 10–13 years |
2005a | 2000–9 vs. 1998–9 | 2.01 vs. 0.58/1000 (↑55%) |
| Australia [74] | National hospital morbidity database | 300,000 | Dose 1 at 18 months Catchup: 12–13 years |
2005 | 1998–2010 | 10.4 vs. 9.9/100,000 Hospitalization rates |
| Canada; British Columbia [127] | Population-DataBC database | 238,295 cases | Dose 1 at 12–15 months Dose 2 at 4–6 years |
2000–6 (1 dose) 2010 (2 doses) |
2012 vs. 1997 | 4.5 vs. 3.2/1000 |
| USA [102] | Population-based active surveillance | 350,000 | Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2006 vs. 2000 | <10 years: 33 vs. 75/100,000 (55%↓) 10–19 years: 97 vs. 60 (63%↑) |
| USA [100] | Medical claims data | 3.5 million (1993) 10.9 million (2006) |
Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2006 vs. 1993 | 4.4 vs. 1.7/1000 |
| USA [95] | HZ hospitalization data | Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2004 vs. pre-2002 | 2.5/10,000 vs. not specified (significant↑) Hospitalization rates |
|
| USA [98] | Population-based active surveillance | Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2007–10 vs. 2000–6 | 12.8 vs. 42/100,000 (<10 years) 78 vs. 68 (10–19 years) |
|
| USA, Washington State [63] | Group Health Cooperative | 1995 (Dose 1) | 2000 vs. 1992 | 3.47 vs. 4.05/1000 person years | ||
| USA; Minnesota [91] | Population-based cohort study | 8017 Cases | Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2000–7 vs. 1945–9 | 3.15 vs. 0.76/1000 person-years |
| USA; Massachusetts [97] | Retrospective study | Dose 1 at 12–15 months Dose 2 at 4–6 years |
1995 (Dose 1) 2006 (Dose 2) |
2003 vs. 1999 | 5.25 vs. 2.77/1000 (90%↑) | |
| Taiwan [64] | National Health Insurance Claims Database | Dose 1 > 12 months | 2004 (Mass vaccination) | 2008 vs. 2000 | 6.89 vs. 4.45/1000 | |
| Taiwan [96] | Insurance claims data study | 1 million | Dose 1 > 12 months | 2004 (Mass vaccination) | 2009 vs. 2000 | 6.24 vs. 4.04/1000 person-years |
| Germany [69] | National hospital discharge data | Doses 1 and 2 at <24 months | 2004 (1 Dose) 2009 (2 Doses) |
2005–12 vs. 1995–2003 | 16.8 vs. 8.8/100,000 |
Publically funded. HZ: herpes zoster.
A recent model considered three main outcomes after varicella vaccination in relation to HZ development: progressive accumulation of immunity following repeated VZV exposure, partial VZV protection that wanes over time, and full but temporary HZ immunity. The authors concluded that better understanding of the processes is therefore needed [114]. If routine infant varicella vaccination causes an albeit small increase in the incidence of HZ, there is a potential ethical dilemma whereby varicella vaccination although protecting one population (children) might have a deleterious effect on older individuals [39]. Other workers have proposed a more pragmatic approach in which zoster vaccination is used to supplement the varicella program and prevent HZ in older adults [40,41]. Nevertheless, long-term data within general populations are needed to determine the potential direct impact of universal varicella vaccination on HZ incidence.
3. Conclusions
Varicella poses a significant public health concern in children and can be prevented with effective varicella vaccination programs. The balance of evidence shows that one dose of varicella vaccine provides high protection against moderate-to-severe varicella but two doses are required for optimal protection against all varicella disease, to limit transmission and to reduce the risk of breakthrough cases and outbreaks. In countries where routine universal vaccination has been implemented, real-world effectiveness and impact studies show significant reduction in the incidence and disease burden of varicella without predicted rises in adult varicella and HZ.
4. Expert commentary
VZV is a highly contagious virus, infecting nearly the whole population. Over 90% of infected individuals subsequently develop varicella, and though the disease is generally mild, serious complication may occur. Indeed, WHO estimates that approximately 4.2 million severe complications leading to hospitalization and 4200 related deaths occur globally each year. However, even mild disease has a significant societal impact, with parents and caregivers having to take time off work to look after infected individuals.
There is robust evidence in the literature showing that varicella vaccines are safe and effective in preventing morbidity and mortality associated with the disease. However, despite the impressive VE, not all countries recommend routine varicella vaccination. In fact, recommendations currently only exist in 33 countries. Nevertheless, where implemented, real-world data have shown impressive reductions in disease incidence compared with the pre-vaccination era. After one-dose programs, reductions up to 74% have been recorded and after two-dose schedules, reductions exceeding 90% have been observed. Not surprisingly, vaccination programs have also been associated with a decrease in varicella-related hospitalization rates and death.
It has been suggested that childhood vaccination programs might result in an upward shift in the age distribution of varicella. However, to avoid this scenario, WHO recommends coverage rates above 80%. These measures as well as wider implementation of vaccination programs should see the effective reduction of this ‘mild,’ but potentially ‘serious,’ and frequently burdensome disease.
5. Five-year view
Over the next 5 years, more real-world data, particularly on long-term protection after one- and two-dose vaccination programs, will be available. These data will be supported by economic studies showing how vaccination can reduce the societal and economic burden of the disease. Better knowledge regarding varicella epidemiology under different coverage levels will emerge, and the impact of varicella vaccination upon the incidence of HZ will be more fully understood. Overall, more countries will have introduced universal varicella vaccination programs, as a result of clinical, real-world, and economic evidence.
Key issues.
VZV is a highly contagious virus infecting nearly all individuals
Varicella is generally a mild disease but with potential serious complications and a high societal burden
Varicella vaccines proved to be safe and effective in preventing the morbidity and mortality associated with the disease
Vaccine recommendations currently exist in 33 countries
Where implemented, real world data have shown impressive reductions in disease incidence compared with the pre-vaccination era, as well as fewer hospitalizations and deaths
Acknowledgments
The authors acknowledge Preethi Govindarajan (GSK, Bangalore, India) and Julia Donnelly (Freelancer for XPE Pharma and Science, Wavre, Belgium c/o GSK) for writing support; and Ashmita Ravishankar (GSK, Bangalore, India) and Adrian Kremer (XPE Pharma and Science, Wavre, Belgium c/o GSK) for editorial support and publication management. The authors would also like to thank Dr. Iris Depaz, Dr. Nicolas Praet, Dr. Christophe Tournay and Dr. Jennifer Cnops for their critical input in the paper.
Funding
GlaxoSmithKline S.A. sponsored and funded this study and was involved in all stages of the study conduct and analysis and also took charge of all costs associated with the manuscript.
Footnotes
Trademark
Varilrix and Priorix-Tetra are trademarks of the GSK group of companies. Varivax and ProQuad are trademarks of Merck & Co. Inc., USA.
Declaration of interest
P Wutzler reports personal fees from the GSK group of companies and Sanofi Pasteur MSD for participating in advisory boards and payment for lecture fees. P Bonanni reports grants and personal fees from Pfizer, GSK groups of companies, Novartis and Sanofi Pasteur MSD. A Gershon reports service contracts (molecular VZV diagnosis for vaccine safety) for ad hoc consulting on VZV by Merck & Co, for serving as a chair on the data and safety monitoring board for the VZV vaccine by the GSK group of companies and receiving NIH research funding. M Safadi reports grants and personal fees from the GSK group of companies, Novartis Vaccines, Sanofi Pasteur MSD and Pfizer for research and speakers’ honoraria. G Casabona is an employee of the GSK group of companies and holds shares in the GSK group of companies. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Centers for Disease Control and Prevention. 13. Varicella: The Pink Book; [Accessed on Dec 5th, 2016]. Available from: www.cdc.gov/vaccines/pubs/pinkbook/downloads/varicella.pdf. [Google Scholar]
- 2.Herman L, Levin MJ, Rehm S. Shedding Light on Shingles: the Power of Prevention. Am J Med. 2016;129:1137. doi: 10.1016/j.amjmed.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed on Dec 6th, 2016];Varicella Vaccination in the European Union. Available from: http://ecdc.europa.eu/en/publications/Publications/Varicella-Guidance-2015.pdf.
- 4.Bozzola E, Bozzola M. Varicella complications and universal immunization. J Pediatr (Rio J) 2016;92:328–330. doi: 10.1016/j.jped.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Varicella and herpes Zoster vaccines. WHO position paper, June 2014. Wkly Epidemiol Rec. 2014;89:265–287. [PubMed] [Google Scholar]
- 6.Shah SS, Wood SM, Luan X, et al. Decline in varicella-related ambulatory visits and hospitalizations in the United States since routine immunization against varicella. Pediatr Infect Dis J. 2010;29:199–204. doi: 10.1097/INF.0b013e3181bbf2a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marin M, Zhang JX, Seward JF. Near elimination of varicella deaths in the US after implementation of the vaccination program. Pediatrics. 2011;128:214–220. doi: 10.1542/peds.2010-3385. [DOI] [PubMed] [Google Scholar]
- 8.Boelle PY, Hanslik T. Varicella in non-immune persons: incidence, hospitalization and mortality rates. Epidemiol Infect. 2002;129:599–606. doi: 10.1017/s0950268802007720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Helmuth IG, Poulsen A, Suppli CH, et al. Varicella in Europe-A review of the epidemiology and experience with vaccination. Vaccine. 2015;33:2406–2413. doi: 10.1016/j.vaccine.2015.03.055. [DOI] [PubMed] [Google Scholar]
- 10.Hobbelen PH, Stowe J, Amirthalingam G, et al. The burden of hospitalisation for varicella and herpes zoster in England from 2004 to 2013. J Infect. 2016;73:241–253. doi: 10.1016/j.jinf.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Heininger U, Seward JF. Varicella. Lancet. 2006;368:1365–1376. doi: 10.1016/S0140-6736(06)69561-5. [DOI] [PubMed] [Google Scholar]
- 12.Widgren K, Giesecke J, Lindquist L, et al. The burden of chickenpox disease in Sweden. BMC Infect Dis. 2016;16:666. doi: 10.1186/s12879-016-1957-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Banz K, Wagenpfeil S, Neiss A, et al. The burden of varicella in Germany. Potential risks and economic impact. Eur J Health Econ. 2004;5:46–53. doi: 10.1007/s10198-003-0200-7. [DOI] [PubMed] [Google Scholar]
- 14.Carapetis JR, Russell DM, Curtis N. The burden and cost of hospitalised varicella and zoster in Australian children. Vaccine. 2004;23:755–761. doi: 10.1016/j.vaccine.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 15.Somekh E, Dalal I, Shohat T, et al. The burden of uncomplicated cases of chickenpox in Israel. J Infect. 2002;45:233–236. doi: 10.1053/jinf.2002.1039. [DOI] [PubMed] [Google Scholar]
- 16.Unim B, Saulle R, Boccalini S, et al. Economic evaluation of Varicella vaccination: results of a systematic review. Hum Vaccin Immunother. 2013;9:1932–1942. doi: 10.4161/hv.25228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17••.Varicella and herpes zoster vaccines: WHO position paper, June. Recommendations. Vaccine. 2014;2016(34):198–199. doi: 10.1016/j.vaccine.2014.07.068. WHO positions paper on vaccination against varicella and herpes. [DOI] [PubMed] [Google Scholar]
- 18.Kreth HW, Lee BW, Kosuwon P, et al. Sixteen years of global experience with the first refrigerator-stable varicella vaccine (Varilrix) Biodrugs. 2008;22:387–402. doi: 10.2165/0063030-200822060-00005. [DOI] [PubMed] [Google Scholar]
- 19.Bonanni P, Gershon A, Gershon M, et al. Primary versus secondary failure after varicella vaccination: implications for interval between 2 doses. Pediatr Infect Dis J. 2013;32:e305–13. doi: 10.1097/INF.0b013e31828b7def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marin M, Guris D, Chaves SS, et al. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56:1–40. [PubMed] [Google Scholar]
- 21.Kurugol Z, Halicioglu O, Koc F, et al. Varicella rates among unvaccinated and one-dose vaccinated healthy children in Izmir, Turkey. Int J Infect Dis. 2011;15:e475–80. doi: 10.1016/j.ijid.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 22.Pieri L, Porchia BR, Pieralli F, et al. Assessment of the effectiveness of the universal varicella vaccination program in Toscana (Italy), in the period 2010–2013. Epidemiol Prev. 2015;39:119–123. [PubMed] [Google Scholar]
- 23.Spackova M, Wiese-Posselt M, Dehnert M, et al. Comparative varicella vaccine effectiveness during outbreaks in day-care centres. Vaccine. 2010;28:686–691. doi: 10.1016/j.vaccine.2009.10.086. [DOI] [PubMed] [Google Scholar]
- 24.Tafuri S, Martinelli D, De Palma M, et al. Report of varicella outbreak in a low vaccination coverage group of otherwise healthy children in Italy: the role of breakthrough and the need of a second dose of vaccine. Vaccine. 2010;28:1594–1597. doi: 10.1016/j.vaccine.2009.11.047. [DOI] [PubMed] [Google Scholar]
- 25••.Marin M, Marti M, Kambhampati A, et al. Global varicella vaccine effectiveness: a meta-analysis. Pediatrics. 2016;137:1–10. doi: 10.1542/peds.2015-3741. This review reports the results of a recent meta-analysis on the effectiveness of varicella vaccination. [DOI] [PubMed] [Google Scholar]
- 26.Banz K, Iseli A, Aebi C, et al. Economic evaluation of varicella vaccination in Swiss children and adolescents. Hum Vaccin. 2009;5:847–857. doi: 10.4161/hv.9898. [DOI] [PubMed] [Google Scholar]
- 27.Maman K, Zollner Y, Greco D, et al. The value of childhood combination vaccines: from beliefs to evidence. Hum Vaccin Immunother. 2015;11:2132–2141. doi: 10.1080/21645515.2015.1044180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holl K, Sauboin C, Amodio E, et al. Coverage, efficacy or dosing interval: which factor predominantly influences the impact of routine childhood vaccination for the prevention of varicella? A model-based study for Italy. BMC Public Health. 2016;16:1103. doi: 10.1186/s12889-016-3738-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.RGlaxoSmithKline. [Accessed on Dec 6th, 2016];Varilrix™ Summary of Product Characteristics 2015. Available from: https://www.medicines.org.uk/emc/medicine/9787.
- 30.Sanofi Pasteur MSD Limited. [Accessed on Dec 6th, 2016];Varivax™ Summary of Product Characteristics. 2013 Available from: https://www.medicines.org.uk/emc/medicine/15264.
- 31.GlaxoSmithKline. [Accessed on Dec 6th, 2016];Priorix-Tetra™ Summary of Product Characteristics. 2014 Available from: http://www.hpra.ie/img/uploaded/swedocuments/LicenseSPC_PA1077-117-003_20052014100041.pdf.
- 32.Sanofi Pasteur MSD ProQuad™. [Accessed on Dec 6th, 2016];Summary of Product Characteristics. 2014 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000622/WC500044070.pdf.
- 33.Ma SJ, Li X, Xiong YQ, et al. Combination measles-mumps-rubella-varicella vaccine in healthy children: a systematic review and meta-analysis of immunogenicity and safety. Medicine (Baltimore) 2015;94:e1721. doi: 10.1097/MD.0000000000001721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang L, Zhu L, Zhu H. Efficacy of varicella (VZV) vaccination: an update for the clinician. Ther Adv Vaccines. 2016;4:20–31. doi: 10.1177/2051013616655980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuter B, Matthews H, Shinefield H, et al. Ten year follow-up of healthy children who received one or two injections of varicella vaccine. Pediatr Infect Dis J. 2004;23:132–137. doi: 10.1097/01.inf.0000109287.97518.67. [DOI] [PubMed] [Google Scholar]
- 36.Prymula R, Bergsaker MR, Esposito S, et al. Protection against varicella with two doses of combined measles-mumps-rubella-varicella vaccine versus one dose of monovalent varicella vaccine: a multicentre, observer-blind, randomised, controlled trial. Lancet. 2014;383:1313–1324. doi: 10.1016/S0140-6736(12)61461-5. [DOI] [PubMed] [Google Scholar]
- 37.Garcia Cenoz M, Castilla J, Chamorro J, et al. Impact of universal two-dose vaccination on varicella epidemiology in Navarre, Spain, 2006 to 2012. Euro Surveill. 2013;18:20552. doi: 10.2807/1560-7917.es2013.18.32.20552. [DOI] [PubMed] [Google Scholar]
- 38.Boccalini S, Bonanni P, Bechini A. Preparing to introduce the varicella vaccine into the Italian immunisation programme: varicella-related hospitalisations in Tuscany, 2004–2012. Euro Surveill. 2016;21 doi: 10.2807/1560-7917.ES.2016.21.24.30257. pii=30257. [DOI] [PubMed] [Google Scholar]
- 39.Luyten J, Ogunjimi B, Beutels P. Varicella-zoster virus vaccination under the exogenous boosting hypothesis: two ethical perspectives. Vaccine. 2014;32:7175–7178. doi: 10.1016/j.vaccine.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 40•.Betta M, Laurino M, Pugliese A, et al. Perspectives on optimal control of varicella and herpes zoster by mass routine varicella vaccination. Proc Biol Sci. 2016;283:20160054. doi: 10.1098/rspb.2016.0054. This recent review describes the perspectives on optimal control of varicella and herpes zoster by mass routine varicella vaccination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gershon AA, Breuer J, Cohen JI, et al. Varicella zoster virus infection. Nat Rev Dis Primers. 2015;1:15016. doi: 10.1038/nrdp.2015.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Australian Government Department of Health and Ageing. [Accessed on Dec 6th, 2016];Immunise Australia Program. 2016 Available from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook10-home~handbook10part4~handbook10-4-22.
- 43•.Hanquet G, Valenciano M, Simondon F, et al. Vaccine effects and impact of vaccination programmes in post-licensure studies. Vaccine. 2013;31:5634–5642. doi: 10.1016/j.vaccine.2013.07.006. This manuscript describes the vaccine impact in real-life setting. [DOI] [PubMed] [Google Scholar]
- 44.Vazquez M, LaRussa PS, Gershon AA, et al. Effectiveness over time of varicella vaccine. Jama. 2004;291:851–855. doi: 10.1001/jama.291.7.851. [DOI] [PubMed] [Google Scholar]
- 45.Mahamud A, Wiseman R, Grytdal S, et al. Challenges in confirming a varicella outbreak in the two-dose vaccine era. Vaccine. 2012;30:6935–6939. doi: 10.1016/j.vaccine.2012.07.076. [DOI] [PubMed] [Google Scholar]
- 46.Shapiro ED, Vazquez M, Esposito D, et al. Effectiveness of 2 doses of varicella vaccine in children. J Infect Dis. 2011;203:312–315. doi: 10.1093/infdis/jiq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liese JG, Cohen C, Rack A, et al. The effectiveness of varicella vaccination in children in Germany: a case-control study. Pediatr Infect Dis J. 2013;32:998–1004. doi: 10.1097/INF.0b013e31829ae263. [DOI] [PubMed] [Google Scholar]
- 48.Miron D, Lavi I, Kitov R, et al. Vaccine effectiveness and severity of varicella among previously vaccinated children during outbreaks in day-care centers with low vaccination coverage. Pediatr Infect Dis J. 2005;24:233–236. doi: 10.1097/01.inf.0000154323.20387.82. [DOI] [PubMed] [Google Scholar]
- 49.Lee YH, Choe YJ, Cho SI, et al. Effectiveness of varicella vaccination program in preventing laboratory-confirmed cases in children in Seoul, Korea. J Korean Med Sci. 2016;31:1897–1901. doi: 10.3346/jkms.2016.31.12.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bayer O, Heininger U, Heiligensetzer C, et al. Metaanalysis of vaccine effectiveness in varicella outbreaks. Vaccine. 2007;25:6655–6660. doi: 10.1016/j.vaccine.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 51.Seward JF, Marin M, Vazquez M. Varicella vaccine effectiveness in the US vaccination program: a review. J Infect Dis. 2008;197(Suppl 2):S82–9. doi: 10.1086/522145. [DOI] [PubMed] [Google Scholar]
- 52.Siedler A, Rieck T, Tolksdorf K. Strong additional effect of a second varicella vaccine dose in children in Germany, 2009–2014. J Pediatr. 2016;173:202–206. doi: 10.1016/j.jpeds.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 53.Fu C, Wang M, Liang J, et al. The effectiveness of varicella vaccine in China. Pediatr Infect Dis J. 2010;29:690–693. doi: 10.1097/INF.0b013e3181d7380e. [DOI] [PubMed] [Google Scholar]
- 54.Wang Z, Yang H, Li K, et al. Single-dose varicella vaccine effectiveness in school settings in China. Vaccine. 2013;31:3834–3838. doi: 10.1016/j.vaccine.2013.06.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baxter R, Ray P, Tran TN, et al. Long-term effectiveness of varicella vaccine: a 14-Year, prospective cohort study. Pediatrics. 2013;131:e1389–96. doi: 10.1542/peds.2012-3303. [DOI] [PubMed] [Google Scholar]
- 56.Avila-Aguero ML, Ulloa-Gutierrez R, Camacho-Badilla K, et al. Varicella prevention in Costa Rica: impact of a one-dose schedule universal vaccination. Expert Rev Vaccines. 2016;16:229–234. doi: 10.1080/14760584.2017.1247700. [DOI] [PubMed] [Google Scholar]
- 57.Amodio E, Tramuto F, Cracchiolo M, et al. The impact of ten years of infant universal Varicella vaccination in Sicily, Italy (2003–2012) Hum Vaccin Immunother. 2015;11:236–239. doi: 10.4161/hv.36157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baxter R, Tran TN, Ray P, et al. Impact of vaccination on the epidemiology of varicella: 1995–2009. Pediatrics. 2014;134:24–30. doi: 10.1542/peds.2013-4251. [DOI] [PubMed] [Google Scholar]
- 59.Siedler A, Arndt U. Impact of the routine varicella vaccination programme on varicella epidemiology in Germany. Euro Surveill. 2010;15 pii=19530. [PubMed] [Google Scholar]
- 60.Streng A, Grote V, Carr D, et al. Varicella routine vaccination and the effects on varicella epidemiology - results from the Bavarian Varicella Surveillance Project (BaVariPro), 2006–2011. BMC Infect Dis. 2013;13:303. doi: 10.1186/1471-2334-13-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pozza F, Piovesan C, Russo F, et al. Impact of universal vaccination on the epidemiology of varicella in Veneto, Italy. Vaccine. 2011;29:9480–9487. doi: 10.1016/j.vaccine.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 62.Mullins J, Kudish K, Sosa L, et al. Continuing decline in varicella incidence after the 2-dose vaccination recommendation-connecti-cut, 2009–2014. Open Forum Infect Dis. 2015;2:ofv150. doi: 10.1093/ofid/ofv150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jumaan AO, Yu O, Jackson LA, et al. Incidence of herpes zoster, before and after varicella-vaccination-associated decreases in the incidence of varicella, 1992–2002. J Infect Dis. 2005;191:2002–2007. doi: 10.1086/430325. [DOI] [PubMed] [Google Scholar]
- 64.Chao DY, Chien YZ, Yeh YP, et al. The incidence of varicella and herpes zoster in Taiwan during a period of increasing varicella vaccine coverage, 2000–2008. Epidemiol Infect. 2012;140:1131–1140. doi: 10.1017/S0950268811001786. [DOI] [PubMed] [Google Scholar]
- 65.Chang LY, Huang LM, Chang IS, et al. Epidemiological characteristics of varicella from 2000 to 2008 and the impact of nationwide immunization in Taiwan. BMC Infect Dis. 2011;11:352. doi: 10.1186/1471-2334-11-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carville KS, Riddell MA, Kelly HA. A decline in varicella but an uncertain impact on zoster following varicella vaccination in Victoria, Australia. Vaccine. 2010;28:2532–2538. doi: 10.1016/j.vaccine.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 67.Lopez AS, Zhang J, Brown C, et al. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics. 2011;127:238–245. doi: 10.1542/peds.2010-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leung J, Harpaz R. Impact of the maturing varicella vaccination program on varicella and related outcomes in the United States: 1994–2012. J Pediatric Infect Dis Soc. 2016;5:395–402. doi: 10.1093/jpids/piv044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Siedler A, Dettmann M. Hospitalization with varicella and shingles before and after introduction of childhood varicella vaccination in Germany. Hum Vaccin Immunother. 2014;10:3594–3600. doi: 10.4161/hv.34426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gil-Prieto R, Walter S, Gonzalez-Escalada A, et al. Different vaccination strategies in Spain and its impact on severe varicella and zoster. Vaccine. 2014;32:277–283. doi: 10.1016/j.vaccine.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 71.De Martino Mota A, Carvalho-Costa FA. Varicella zoster virus related deaths and hospitalizations before the introduction of universal vaccination with the tetraviral vaccine. J Pediatr (Rio J) 2016;92:361–366. doi: 10.1016/j.jped.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 72.Bechini A, Boccalini S, Baldo V, et al. Impact of universal vaccination against varicella in Italy. Hum Vaccin Immunother. 2015;11:63–71. doi: 10.4161/hv.34311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Waye A, Jacobs P, Tan B. The impact of the universal infant varicella immunization strategy on Canadian varicella-related hospitalization rates. Vaccine. 2013;31:4744–4748. doi: 10.1016/j.vaccine.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 74.Heywood AE, Wang H, Macartney KK, et al. Varicella and herpes zoster hospitalizations before and after implementation of one-dose varicella vaccination in Australia: an ecological study. Bull World Health Organ. 2014;92:593–604. doi: 10.2471/BLT.13.132142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nguyen HQ, Jumaan AO, Seward JF. Decline in mortality due to varicella after implementation of varicella vaccination in the United States. N Engl J Med. 2005;352:450–458. doi: 10.1056/NEJMoa042271. [DOI] [PubMed] [Google Scholar]
- 76.Guris D, Jumaan AO, Mascola L, et al. Changing varicella epidemiology in active surveillance sites–United States, 1995–2005. J Infect Dis. 2008;197(Suppl 2):S71–5. doi: 10.1086/522156. [DOI] [PubMed] [Google Scholar]
- 77.Papaloukas O, Giannouli G, Papaevangelou V. Successes and challenges in varicella vaccine. Ther Adv Vaccines. 2014;2:39–55. doi: 10.1177/2051013613515621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Van Hoek AJ, Melegaro A, Zagheni E, et al. Modelling the impact of a combined varicella and zoster vaccination programme on the epidemiology of varicella zoster virus in England. Vaccine. 2011;29:2411–2420. doi: 10.1016/j.vaccine.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 79.World Health Organization. [Accessed on Dec 6th, 2016];Immunization, vaccines and biologicals: varicella. 2015 Available from: http://www.who.int/immunization/diseases/varicella/en/
- 80.Bialek SR, Perella D, Zhang J, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics. 2013;132:e1134–40. doi: 10.1542/peds.2013-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuter BJ, Ngai A, Patterson CM, et al. Safety, tolerability, and immunogenicity of two regimens of Oka/Merck varicella vaccine (Varivax) in healthy adolescents and adults. Oka/Merck Varicella Vaccine Study Group. Vaccine. 1995;13:967–972. doi: 10.1016/0264-410x(95)00046-4. [DOI] [PubMed] [Google Scholar]
- 82.Sperber SJ, Smith BV, Hayden FG. Serologic response and reactogenicity to booster immunization of healthy seropositive adults with live or inactivated varicella vaccine. Antiviral Res. 1992;17:213–222. doi: 10.1016/0166-3542(92)90042-4. [DOI] [PubMed] [Google Scholar]
- 83.Brisson M, Edmunds WJ, Gay NJ, et al. Modelling the impact of immunization on the epidemiology of varicella zoster virus. Epidemiol Infect. 2000;125:651–669. doi: 10.1017/s0950268800004714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Oxman MN. Herpes zoster pathogenesis and cell-mediated immunity and immunosenescence. J Am Osteopath Assoc. 2009;109:S13–7. [PubMed] [Google Scholar]
- 85.Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med. 1965;58:9–20. [PMC free article] [PubMed] [Google Scholar]
- 86.Horn J, Karch A, Damm O, et al. Current and future effects of varicella and herpes zoster vaccination in Germany - Insights from a mathematical model in a country with universal varicella vaccination. Hum Vaccin Immunother. 2016;12:1766–1776. doi: 10.1080/21645515.2015.1135279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gidding HF, Brisson M, Macintyre CR, et al. Modelling the impact of vaccination on the epidemiology of varicella zoster virus in Australia. Aust N Z J Public Health. 2005;29:544–551. doi: 10.1111/j.1467-842x.2005.tb00248.x. [DOI] [PubMed] [Google Scholar]
- 88.Karhunen M, Leino T, Salo H, et al. Modelling the impact of varicella vaccination on varicella and zoster. Epidemiol Infect. 2010;138:469–481. doi: 10.1017/S0950268809990768. [DOI] [PubMed] [Google Scholar]
- 89.Damm O, Ultsch B, Horn J, et al. Systematic review of models assessing the economic value of routine varicella and herpes zoster vaccination in high-income countries. BMC Public Health. 2015;15:533. doi: 10.1186/s12889-015-1861-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Van Lier A, Lugner A, Opstelten W, et al. Distribution of health effects and cost-effectiveness of varicella vaccination are shaped by the impact on herpes zoster. EBioMedicine. 2015;2:1494–1499. doi: 10.1016/j.ebiom.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kawai K, Yawn BP, Wollan P, et al. Increasing Incidence of herpes zoster over a 60-year period from a population-based study. Clin Infect Dis. 2016;63:221–226. doi: 10.1093/cid/ciw296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ragozzino MW, Melton LJ, 3rd, Kurland LT, et al. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore) 1982;61:310–316. doi: 10.1097/00005792-198209000-00003. [DOI] [PubMed] [Google Scholar]
- 93.Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82:1341–1349. doi: 10.4065/82.11.1341. [DOI] [PubMed] [Google Scholar]
- 94.Nelson MR, Britt HC, Harrison CM. Evidence of increasing frequency of herpes zoster management in Australian general practice since the introduction of a varicella vaccine. Med J Aust. 2010;193:110–113. [PubMed] [Google Scholar]
- 95.Patel MS, Gebremariam A, Davis MM. Herpes zoster-related hospitalizations and expenditures before and after introduction of the varicella vaccine in the United States. Infect Control Hosp Epidemiol. 2008;29:1157–1163. doi: 10.1086/591975. [DOI] [PubMed] [Google Scholar]
- 96.Wu PY, Wu HD, Chou TC, et al. Varicella vaccination alters the chronological trends of herpes zoster and varicella. Plos One. 2013;8:e77709. doi: 10.1371/journal.pone.0077709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yih WK, Brooks DR, Lett SM, et al. The incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccine coverage, 1998–2003. BMC Public Health. 2005;5:68. doi: 10.1186/1471-2458-5-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Civen R, Marin M, Zhang J, et al. Update on incidence of herpes zoster among children and adolescents after implementation of varicella vaccination, antelope valley, CA, 2000 to 2010. Pediatr Infect Dis J. 2016;35:1132–1136. doi: 10.1097/INF.0000000000001249. [DOI] [PubMed] [Google Scholar]
- 99.Jardine A, Conaty SJ, Vally H. Herpes zoster in Australia: evidence of increase in incidence in adults attributable to varicella immunization? Epidemiol Infect. 2011;139:658–665. doi: 10.1017/S0950268810001949. [DOI] [PubMed] [Google Scholar]
- 100.Leung J, Harpaz R, Molinari NA, et al. Herpes zoster incidence among insured persons in the United States, 1993–2006: evaluation of impact of varicella vaccination. Clin Infect Dis. 2011;52:332–340. doi: 10.1093/cid/ciq077. [DOI] [PubMed] [Google Scholar]
- 101.Tanuseputro P, Zagorski B, Chan KJ, et al. Population-based incidence of herpes zoster after introduction of a publicly funded varicella vaccination program. Vaccine. 2011;29:8580–8584. doi: 10.1016/j.vaccine.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 102.Civen R, Chaves SS, Jumaan A, et al. The incidence and clinical characteristics of herpes zoster among children and adolescents after implementation of varicella vaccination. Pediatr Infect Dis J. 2009;28:954–959. doi: 10.1097/INF.0b013e3181a90b16. [DOI] [PubMed] [Google Scholar]
- 103.Weinmann S, Chun C, Schmid DS, et al. Incidence and clinical characteristics of herpes zoster among children in the varicella vaccine era, 2005–2009. J Infect Dis. 2013;208:1859–1868. doi: 10.1093/infdis/jit405. [DOI] [PubMed] [Google Scholar]
- 104.Ogunjimi B, Van Damme P, Beutels P. Herpes zoster risk reduction through exposure to chickenpox patients: a systematic multidisciplinary review. Plos One. 2013;8:e66485. doi: 10.1371/journal.pone.0066485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mullooly JP, Riedlinger K, Chun C, et al. Incidence of herpes zoster, 1997–2002. Epidemiol Infect. 2005;133:245–253. doi: 10.1017/s095026880400281x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hambleton S, Steinberg SP, Larussa PS, et al. Risk of herpes zoster in adults immunized with varicella vaccine. J Infect Dis. 2008;197(Suppl 2):S196–9. doi: 10.1086/522131. [DOI] [PubMed] [Google Scholar]
- 107.Hata A, Asanuma H, Rinki M, et al. Use of an inactivated varicella vaccine in recipients of hematopoietic-cell transplants. N Engl J Med. 2002;347:26–34. doi: 10.1056/NEJMoa013441. [DOI] [PubMed] [Google Scholar]
- 108.Ogunjimi B, Willem L, Beutels P, et al. Integrating between-host transmission and within-host immunity to analyze the impact of varicella vaccination on zoster. Elife. 2015;4:e07116. doi: 10.7554/eLife.07116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Poletti P, Melegaro A, Ajelli M, et al. Perspectives on the impact of varicella immunization on herpes zoster. A model-based evaluation from three European countries. Plos One. 2013;8:e60732. doi: 10.1371/journal.pone.0060732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wood SM, Shah SS, Steenhoff AP, et al. Primary varicella and herpes zoster among HIV-infected children from 1989 to 2006. Pediatrics. 2008;121:e150–6. doi: 10.1542/peds.2007-0564. [DOI] [PubMed] [Google Scholar]
- 111.Hales CM, Harpaz R, Joesoef MR, et al. Examination of links between herpes zoster incidence and childhood varicella vaccination. Ann Intern Med. 2013;159:739–745. doi: 10.7326/0003-4819-159-11-201312030-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shirane R, Tang H, Hayashi K, et al. Relationship between cell-mediated immunity to Varicella-Zoster virus and aging in subjects from the community-based Shozu Herpes Zoster study. J Med Virol. 2017;89:313–317. doi: 10.1002/jmv.24629. [DOI] [PubMed] [Google Scholar]
- 113.Ogunjimi B, Theeten H, Hens N, et al. Serology indicates cytomegalovirus infection is associated with varicella-zoster virus reactivation. J Med Virol. 2014;86:812–819. doi: 10.1002/jmv.23749. [DOI] [PubMed] [Google Scholar]
- 114•.Guzzetta G, Poletti P, Merler S, et al. The epidemiology of herpes zoster after varicella immunization under different biological hypotheses: perspectives from mathematical modeling. Am J Epidemiol. 2016;183:765–773. doi: 10.1093/aje/kwv240. This manuscript describes a recent modeling study to predict the epidemiological outcomes after varicella vaccination. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Centro de Vigilancia Epidemiologica “Prof. Alexandre Vranjac”. [Accessed on Dec 6th, 2016];Calendário de Vacinação. 2016 Available from: http://portal.saude.sp.gov.br/resources/cve-centro-de-vigilancia-epidemiologica/areas-de-vigilancia/imunizacao/doc/calendario16_vacinacao.pdf.
- 116.Ministerio de Salud Presidencia de la Nación. [Accessed on Feb 22th, 2017];Calendario Nacional de Vacunación de la República Argentina. 2017 Available from: http://www.msal.gob.ar/index.php/component/content/article/46-ministerio/184-calendario-nacional-de-vacunacion-2016.
- 117.Tafuri S, Martinelli D, Prato R, et al. Vaccine effectiveness evaluation during a varicella outbreak among children of primary schools and day-care centers in a region which adopted UMV. Hum Vaccin Immunother. 2013;9:184–188. doi: 10.4161/hv.22373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lai CC, Chen SC, Jiang DD. An outbreak of varicella among schoolchildren in Taipei. BMC Public Health. 2011;11:226. doi: 10.1186/1471-2458-11-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vazquez M, LaRussa PS, Gershon AA, et al. The effectiveness of the varicella vaccine in clinical practice. N Engl J Med. 2001;344:955–960. doi: 10.1056/NEJM200103293441302. [DOI] [PubMed] [Google Scholar]
- 120.Perella D, Wang C, Civen R, et al. Varicella vaccine effectiveness in preventing community transmission in the 2-dose era. Pediatrics. 2016;137:e20152802. doi: 10.1542/peds.2015-2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hohle M, Siedler A, Bader HM, et al. Assessment of varicella vaccine effectiveness in Germany: a time-series approach. Epidemiol Infect. 2011;139:1710–1719. doi: 10.1017/S0950268810002815. [DOI] [PubMed] [Google Scholar]
- 122.Trucchi C, Gabutti G, Rota MC, et al. Burden of varicella in Italy, 2001–2010: analysis of data from multiple sources and assessment of universal vaccination impact in three pilot regions. J Med Microbiol. 2015;64:1387–1394. doi: 10.1099/jmm.0.000061. [DOI] [PubMed] [Google Scholar]
- 123.Lopez AS, Zhang J, Marin M. Epidemiology of varicella during the 2-dose varicella vaccination program - United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2016;65:902–905. doi: 10.15585/mmwr.mm6534a4. [DOI] [PubMed] [Google Scholar]
- 124.Streng A, Grote V, Rack-Hoch A, et al. Decline of neurologic varicella complications in children during the first 7 years after introduction of universal varicella vaccination in Germany, 2005–2011. Pediatr Infect Dis J. 2017;36:79–86. doi: 10.1097/INF.0000000000001356. [DOI] [PubMed] [Google Scholar]
- 125.Elbaz M, Paret G, Yohai AB, et al. Immunisation led to a major reduction in paediatric patients hospitalised because of the varicella infection in Israel. Acta Paediatr. 2016;105:e161–6. doi: 10.1111/apa.13320. [DOI] [PubMed] [Google Scholar]
- 126.Humes EA, Weinberger DM, Kudish KS, et al. Trends in hospitalizations with primary varicella and herpes zoster during the prevaricella and initial postvaricella and herpes zoster vaccine eras, connecticut, 1994–2012. Open Forum Infect Dis. 2015;2:ofv001. doi: 10.1093/ofid/ofv001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Marra F, Chong M, Najafzadeh M. Increasing incidence associated with herpes zoster infection in British Columbia, Canada. BMC Infect Dis. 2016;16:589. doi: 10.1186/s12879-016-1898-z. [DOI] [PMC free article] [PubMed] [Google Scholar]