SYNOPSIS
Objective
Recognizing that not all mothers at risk for depression engage in insensitive parenting, this study examined predictors of individual differences in sensitive parenting of infants by mothers with histories of depression, who are at elevated risk for depression during the perinatal period.
Design
We examined maternal personal characteristics, context, and early infant temperament as predictors of sensitive parenting. Seventy-six women with a history of major depression were followed through pregnancy and postpartum and observed during play and feeding interactions with their 12-month-old infants.
Results
Maternal personal characteristics (recurrence of clinically significant depression symptom levels during pregnancy or postpartum and higher trait anxiety), context (lower social context and lower income), and early infant temperament (higher negative affectivity, surgency/extraversion, and orienting/regulation) are often associated with less sensitive parenting, with stronger and clearer associations for play than feeding and with some differences based on whether sensitivity was defined as affective matching or rated sensitivity.
Conclusions
The findings extend support for multi-determination of sensitive parenting of infants to women with histories of depression, albeit with small to medium effect sizes, and suggest ways to identify those who may be most at risk for insensitive parenting and the potential value of intervening in pregnancy to enhance subsequent sensitivity of parenting.
INTRODUCTION
Sensitive parenting, the ability to respond promptly and appropriately to infants’ cues, plays a central role in attachment theory’s concept of stage-salient socialization in the first year of life (Ainsworth, Bell, & Stayton, 1971). It is well established as significantly related to infants’ quality of attachment (with a medium effect size based on a meta-analytic review by De Wolff & van IJzendoorn, 1997), stress response system (Gunnar & Quevedo, 2007), and social-emotional and cognitive development (Sroufe, Egeland, Carlson, & Collins, 2005) and has enduring predictive significance for social and academic functioning through at least mid-adolescence (Raby, Roisman, Fraley, & Simpson, 2014). Moreover, sensitive parenting has been found to mediate associations between depression in mothers and infants’ subsequent development (Milgrom, Westley, & Gemmill, 2004). Thus, it is essential to understand the factors that contribute to mothers’ ability to sensitively interact with their infants.
Based on a rich history of research on this topic, with seminal contributions from Belsky and Bornstein, sensitive parenting has come to be recognized as multiply determined, with three generally agreed upon factors: parents’ personal psychological resources (psychological well-being), children’s characteristics (with temperament being paramount), and contextual factors such as stress and social support (Belsky, 1984; Bornstein, 2002b, 2016). Although developed to reflect sensitive parenting for the general population, this model may be particularly apt for mothers with depression, whether defined as meeting Diagnostic and Statistical Manual (DSM; American Psychiatric Association, 2013) diagnostic criteria or by elevated symptom levels, given theoretical and empirical links between depression and all three of the factors in the model. We propose and examine such a model, focused on women at elevated risk for perinatal depressive symptoms.
In terms of personal psychological resources, depression in mothers has been noted as perhaps the strongest determinant of parenting qualities (Belsky, 1984), and depression (diagnosed or elevated symptoms) in mothers is reliably associated with more negative and disengaged and less positive parenting with infants, with moderate effect sizes (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). However, studies typically failed to take into account the heterogeneity in chronicity and timing that characterizes depression (Ingram & Siegle, 2009), because most studies were limited to a single measure of depression, typically concurrent with the parenting measure. In two exceptions, low sensitivity was found to be most strongly associated with depression that was chronic over the course of infancy (Campbell, Cohn, & Meyers, 1995; NICHD Early Child Care Research Network, 1999b). Both Campbell et al. and the NICHD study, however, studied general population samples, among which depression symptom levels are typically highly skewed, with the majority of women scoring very low.
To address questions about depressive symptoms and sensitive parenting, sampling women with histories of depression episodes may be preferable to normative population samples given that they are at highly elevated risk of perinatal depression (as meta-analytically reviewed in Robertson, Grace, Wallington, & Stewart, 2004), and thus this sampling strategy would yield a higher percentage of women with clinically significant levels of depression symptoms. Moreover, perinatal depression in such women is, by definition, a recurrence. Recurrent depression, relative to first episode depression, is associated with a set of cognitive, interpersonal, or biological vulnerabilities, such as self-focused attention, which may interfere with sensitive parenting (Phillips, Sharpe, Matthey, & Charles, 2010). Further, most studies of mothers’ depression and the sensitivity of their parenting failed to measure depression during the prenatal period, even though prenatal depression is a predictor of postpartum depression (Heron, O’Connor, Evans, Golding, & Glover, 2004) and of elevated levels of parenting stress in the postpartum (Misri et al., 2010). Relevant to public health, detection of risk for insensitive parenting during pregnancy offers the potential to intervene early to enhance the likelihood of subsequent sensitive parenting. Thus, we sampled women at risk for elevated perinatal depressive symptom levels, conducting a longitudinal study repeatedly sampling depression symptoms beginning in pregnancy and, subsequently, over the first year postpartum.
In further consideration of the personal characteristics component of a model predicting sensitive parenting, it is important to note that most studies of depression and mother-infant interaction failed to consider depression’s common comorbidities. Of particular concern is trait anxiety, given that it is not only highly correlated with depression, but also has been associated with less sensitive parenting (Kaitz & Maytal, 2005). Thus, trait level anxiety may be an important aspect of a model predicting sensitive parenting among women at risk for perinatal depression and is included in the current study.
Another set of factors in both Belsky’s and Bornstein’s models of sensitive parenting reflect the context in which parenting occurs. Context variables such as stress, social support, partner relationship satisfaction, and family socioeconomic status have received strong empirical support for associations with sensitive parenting of infants in normative populations (Bornstein, 2002a). Moreover, women’s higher prenatal levels of satisfaction with their amount of social support were associated with their more sensitive parenting of their infants (Goldstein, Diener, & Mangelsdorf, 1996). Context is particularly relevant to sensitive parenting of infants by women with depression given that depression in women is associated with more stress and hassles (Hammen, 2002), more marital conflict (Whisman, Weinstock, & Tolejko, 2006), more poverty (Yen & Kaplan, 1999), and fewer and less supportive relationships (Brown & Harris, 1978), even during the perinatal period (Goodman & Tully, 2009). Thus, it is essential to examine the roles of social context and income in relation to sensitive parenting among women at high risk for perinatal depression.
Turning to infant characteristics, the infant characteristic that plays a central role in both Belsky’s and Bornstein’s models of sensitive parenting is temperament, defined by Rothbart and colleagues as consisting of three factors: negative affectivity, surgency/extraversion, and orienting/regulation (Gartstein & Rothbart, 2003). In a meta-analytic review, higher levels of negative affectivity have been found to be associated with less sensitive parenting of infants with a small effect size in general population samples and a larger effect size in “at risk” samples (Paulussen-Hoogeboom, Stams, Hermanns, & Peetsma, 2007). Much less is known about the other two temperament factors in relation to sensitive parenting of infants. In the only study we found to report on this, higher infant surgency/extraversion was found to be associated with mothers’ lower sensitivity and orienting/regulation was not related to sensitivity (Planalp, Braungart-Rieker, Lickenbrock, & Zentall, 2013).
Infant temperament is especially relevant to consider in a model of sensitive parenting in mothers with histories of depression given that both prenatal and postpartum depression have been found to be associated with more “difficult” temperament in infants (Britton, 2011; Rouse & Goodman, 2014). Moreover, infant irritability and other aspects of “difficult” temperament predict the onset of depression in the postpartum among women at high risk for postnatal depression (Murray, Stanley, Hooper, King, & Fiori-Cowley, 1996).
In sum, despite the strong theoretical models and empirical support for multiple determinants of mothers’ sensitive parenting of infants in general population samples, little is known about the origins of individual differences in sensitive parenting of infants by mothers with histories of depression prior to pregnancy, the group that is known to have the highest rates of perinatal depression (Heron et al., 2004). Thus, we aimed to extended Belsky’s and Bornstein’s work by testing all three components of their models of determinants of sensitive parenting in a study of women at elevated risk for perinatal depression.
Based on this model, we conducted a longitudinal, prospective study, measuring women’s depression symptom levels at multiple time points in pregnancy and the first year postpartum and their sensitivity of parenting, based on a multi-method approach to measurement, when infants were 12 months of age. We predicted that lower levels of parenting sensitivity would be associated with: (1) women’s more chronic elevated depression symptom levels, during pregnancy and during the first year postpartum, and their depressive symptom levels at the time of the parenting assessment, and higher trait levels of anxiety; (2) mothers’ perception of having higher stress, fewer and less satisfying supports, higher levels of marital/dyadic distress both over the course of pregnancy and the first year postpartum, and lower income; and (3) infants’ higher negative affectivity early in infancy. The latter hypothesis is consistent with the notion that predictors of sensitive parenting might be set relatively early in mother-infant relationships and that mothers early on begin to settle on strategies for parenting their infant (Bigelow et al., 2010). With regard to the other temperament factors, given inadequate bases for hypotheses, we examined in an exploratory manner the potential association between maternal sensitivity and surgency/extraversion and orienting/regulation early in infancy.
Although there is no consensus on how best to measure sensitive parenting, we addressed validity concerns (Seifer, Schiller, Sameroff, Resnick, & Riordan, 1996) in two ways. First we observed parenting in two conditions, to better capture representative patterns of parenting, whereas most published studies relied on a single condition (typically play). Second, we developed a multi-dimensional operational definition of sensitive parenting, following recommendations of mother-infant dyad researchers (Beebe et al., 2010) to incorporate multiple indices.
Two complementary approaches to measuring sensitivity from observed mother-infant interactions are global rating scales and micro-analytic coding; we took advantage of the benefits of each (Adamson, Bakeman, Deckner, & Nelson, 2012; Bakeman & Quera, 1995). Using rating items, we derived a global measure of sensitivity as others have done (Belsky, Jaffee, Sligo, Woodward, & Silva, 2005). And using micro-analytic coding, we derived a measure of affective matching. Others have expressed a concern that depression may manifest in a mother’s limited capacity to match her infant’s positive expressions and that matching, or affective synchrony, may contribute to the development of infant self-regulation of emotions (Tronick & Beeghly, 2011). Further, evidence that depressed mothers match their infants’ positive affective states for significantly lower percentages of time than non-depressed mothers (Field, Healy, Goldstein, & Guthertz, 1990) informed our decision to focus on positive affective states during the coded interactions. To minimize variability that might be associated with age, we studied one particular infant age, specifically 12-month-old infants, given that by this age infants are able to engage actively with both their interacting partner and with objects, such as toys and food (Rochat, 2001).
METHOD
Participants
Potential participants were recruited from obstetrical offices (65%) or through media announcements (35%) in a major southeastern city. We determined eligibility using a two-stage process. First, a brief phone screen determined whether a woman met our inclusion criteria: likely to have ever experienced a major depression episode as defined by DSM-IV (American Psychiatric Association, 1994), pregnant with their first child, married or cohabiting, having a medically uncomplicated pregnancy, age 19 or older, no more than 6 months pregnant, and either European American or African American (the major ethnic groups in the region from which we recruited). Participation was limited to primiparous women who were married or cohabitating with a partner to further reduce the variability in quality of parenting associated with multiparity (Fish & Stifter, 1993) and single parenthood (Cheadle & Amato, 2011). Second, eligible women were invited to the laboratory where, after giving informed consent, they were administered a diagnostic interview to determine whether they met DSM-IV criteria for at least one lifetime major depression episode and whether any exclusion criteria applied: current active suicidality; current or past substance use disorders, schizophrenia, psychotic, or bipolar disorders; and a positive urine toxicology screen for drug or alcohol use.
A total of 122 women met criteria for inclusion in the study. Of those, 46 were excluded from the study sample: 38 dropped out during pregnancy, 4 dropped out postpartum, 2 missed their 12-month visit, and for 2 we encountered equipment problems at this visit. Thus, the study sample consisted of 76 mothers and their infants; 35 of the infants were male and 41 female. One mother participated in two separate laboratory visits with each of her twin infants, but data for only one twin, randomly selected, were included in the analysis.
Women in the study sample did not differ significantly from those excluded in either demographics or depression or trait anxiety. Demographic characteristics of the mothers for whom we had data are given in Table 1. The age, education, income, marital status, and ethnicity of mothers in the study sample did not differ from the excluded mothers (ps per t-test and chi-squares were .28, .71, .52, .68, and .68, respectively), nor did the two groups differ with respect to mean prenatal BDI scores (M = 9.4 vs. 8.7, t[103] < 1, n = 74 vs. 31, p = .55) or STAI scores (M = 37.3 vs. 36.8, t[94] < 1, n = 75 vs. 21, p = .84), or whether their BDI score exceed 13 for 1 or more months during pregnancy, χ2(1, N = 107) = 1.05, n = 76 vs. 31, p = .22.
TABLE 1.
Maternal Demographics
| Variable | Sample | Excluded |
|---|---|---|
| Age (years) | 30.3a | 29.2b |
| Education (%) | ||
| Completed high school | 29 | 34 |
| Completed college | 42 | 34 |
| Some post-college | 29 | 32 |
| Income (%) | ||
| $10,000–$50,000 | 26 | 29 |
| $51,000–$75,000 | 29 | 24 |
| $51,000–$75,000 | 18 | 29 |
| More than $100,000 | 26 | 18 |
| Marital status (%) | ||
| Married | 74 | 78 |
| Ethnicity (%) | ||
| European American | 32 | 28 |
| African American | 68 | 72 |
Note. N = 76 for the study sample; of the 46 excluded, age, education, and income data were available for 38, marital status for 37, and ethnicity for 36.
SD = 5.4, range = 19–42
SD = 4.2, range = 22–4
Procedure
Participants completed a psychiatric diagnostic interview and the trait anxiety measure at the first visit during pregnancy and then completed questionnaire measures of depression symptom levels, stress, social support, and marital/dyadic satisfaction on a monthly basis from their entry into the study (mean number of months pregnant at entry = 3.7, SD = 1.2) through 6 months postpartum and completed the depression measure again at 12 months postpartum. Participants completed an average of 5 data collections during pregnancy (SD = 1.5) and 7 during the postpartum period (SD = 1.0).
Mothers completed a measure of infant temperament when the infants were 3, 6, and 12 months of age. At 12 months of age, mothers and their infants were videorecorded in two 5-min face-to-face interactions in the laboratory: feeding and play. During both feeding and free play segments, infants were seated in a high chair with mothers seated directly in front of them. During the free play segment, mothers were provided a box of age-appropriate toys and instructed to play with their baby as they would at home. During the feeding segment, mothers spoon-fed infants and/or assisted infants with finger foods and/or liquids. Interactions were coded with the assistance of the INTERACT System (Mangold, 2010).
Measures
Maternal Personal Characteristics: Depression
The Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P; First, Spitzer, Gibbon, & Williams, 2002), administered at the initial visit, was used to determine if the women experienced at least one major depression episode prior to pregnancy. All interviews were conducted by a master’s level psychologist, psychiatric nurse, or social worker and audio recorded for purposes of maintaining interrater reliability. A licensed clinical psychologist, blind to other information on the participants, listened to all interviews, reviewed the notes, and derived diagnoses.
The Beck Depression Inventory-II (BDI-II), a 21-item scale assessing the intensity of depressive symptoms in the previous 2 weeks, has strong evidence of reliability and validity in clinical and nonclinical samples including during pregnancy (Holcomb, Stone, Lustman, Gavard, & Mostello, 1996). Higher scores indicate more severe depression; scores greater than 13 indicate at least mild clinically significant symptom levels of depression (Beck, Steer, & Brown, 1997). Cronbach’s alphas at each time point the BDI-II was administered ranged from .75 to .97. To index chronicity, following the approach taken in the NICHD study (bNICHD Early Child Care Research Network, 1999b), mothers were initially assigned to one of three groups during pregnancy and, separately, during the first 6 months postpartum: (1) those whose depression scores never exceeded the cut-off (ns = 40 and 47, for pregnancy and postpartum, respectively), (2) those whose depression scores only exceeded the cut-off at one of the monthly assessments (ns = 16 and 15 for pregnancy and postpartum, respectively), and (3) those women whose depression scores exceeded the cut-off at two or more of the monthly assessments (ns = 20 and 14, for pregnancy and postpartum, respectively).
Maternal Personal Characteristics: Trait Anxiety
The trait anxiety score of the State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970) has strong psychometric properties and is widely used to assess stable personality traits associated with a propensity for anxiety. Chronbach’s alpha for this sample = .94. The scale consists of 20 Likert-scaled items which are summed; higher scores indicate higher trait anxiety. Scores of 43 or above are considered a risk indicator for anxiety disorders. In our study sample, 35% scored in this range (26 of the 75 women for whom we had STAI scores).
Maternal Context: Social Support
To assess their perceived social support, mothers completed the 6-item Social Support Questionnaire (SSQ: Sarason, Sarason, Shearin, & Pierce, 1987), which has strong reliability and validity (Sarason et al., 1987). This measure yields two scores: network size (SSQ-N, the mean number of people available for help or support in different aspects, with a possible range 0–9) and mean satisfaction with available supports (SSQ-S; scores can range from 1 to 6 with higher scores indicating more satisfaction). For this sample, Cronbach’s alpha ranged from .90 to .95 for the SSQ-N and from .90 to .96 for SSQ-S across the multiple times they were administered.
Maternal Context: Quality of Relationship with Husband/Partner
To assess level of distress with their husband or partner, mothers completed the 8-item Dyadic Adjustment Scale (DAS; Sharpley & Rogers, 1984), which has good validity and high internal consistency. Scores can range from 0 to 36 with higher scores indicating less distressed relationships. Cronbach’s alphas for the DAS at each time it was administered ranged from .81 to .91.
Maternal Context: Perceived Stress
To assess the degree to which women considered any experiences in the last month to be stressful, mothers completed the 10-item Perceived Stress Scale (PSS; S. Cohen, Kamarck, & Mermelstein, 1983), which has adequate validity and reliability. Scores can range from 0 to 40, with higher scores indicating more appraised stress. Chronbach’s alpha for the PSS at each time it was administered ranged from .88 to .94.
Maternal Context Summary Scores
Mean scores for the four context scores just described were computed separately for the pregnancy and postpartum periods. Our initial intent was to consider the periods separately, but pregnancy and postpartum scores correlated .75–.94 and the summary scores for each period correlated .87. Consequently, we formed a single score for each scale—the average of its pregnancy and postpartum scores—and a single summary maternal context score—the mean of z scores (to weight each variable equally), computed if no more than two of the eight scale scores were missing. The Cronbach’s alpha for this summary score was .79. To avoid negative and small values, we multiplied the summary scores by 10 and added 80, resulting in scores with means near 80 and ranges of about 60–100. Descriptive statistics for the component variables are given in Table 2.
TABLE 2.
Descriptive Statistics for Context Component Variables
| Variable | M | SD | min | max | n |
|---|---|---|---|---|---|
| Pregnancy | |||||
| Social support – network size (0–9) | 3.54 | 1.65 | 1.22 | 8.67 | 74 |
| Social support – satisfaction (1–6) | 5.24 | 0.75 | 2.67 | 6.00 | 75 |
| Dyadic Adjustment Scale (0–42) | 29.5 | 6.24 | 7.33 | 40.4 | 76 |
| Perceived Stress Scale (0–40) | 13.7 | 6.26 | 1.20 | 26.4 | 76 |
| Postpartum | |||||
| Social support – network size (0–9) | 3.31 | 1.76 | 0.67 | 9.00 | 76 |
| Social support – satisfaction (1–6) | 4.95 | 0.85 | 2.36 | 6.00 | 76 |
| Dyadic Adjustment Scale (0–42) | 29.0 | 7.02 | 2.00 | 39.8 | 73 |
| Perceived Stress Scale (0–40) | 13.2 | 6.40 | 1.20 | 25.0 | 76 |
Note. Possible ranges are indicated in parentheses.
Infant Characteristics: Temperament
The Infant Behavior Questionnaire - Revised (IBQ-R; Gartstein & Rothbart, 2003) is a factor-analytically derived measure of infant temperament, based on the Rothbart and Derryberry (1981) definition of temperament. The questionnaire contains 191 items scored from 1 (Never) to 7 (Always) reflecting 14 scales. Scores are the means for the items on three empirically derived factors, extraversion/surgency, negative affectivity, and orienting/regulating; higher scores indicate more of the factor. The IBQ-R by design minimizes subjectivity and is robust to any tendency for depressed mothers to rate their children negatively (Gartstein & Marmion, 2008). Most relevant to concerns about negative bias in relation to depression, Gartstein and Marmion found that mothers’ depression symptom levels did not significantly predict differences between observed and mother-rated (IBQ-R) infant fear or positive emotionality. Although completed by mothers when infants were 3, 6, and 12 months of age, only the 3-month scores for each of the three factors are analyzed here as an index of early infant temperament.
Maternal Sensitivity: Affect Coding and Matching
Two independent teams coded mothers’ and infants’ moment-to-moment affective behavior, based on observed facial expression and tone of voice from the videorecorded segments and without other knowledge of the mother or infant, during the play and feeding sessions. Mother and infant affective codes, modified from Dawson et al. (1999), included three levels of positive affect (positive interest, smile/excitement, and laughter/squeal), neutral, and three levels of negative affect (tension/negative interest, brief distress/frown/protest/fuss, and marked distress/cry; coding manual available from the first author). In both conditions, 98% of the total interaction times were considered codeable (play: M = 292 s, SD = 31; feeding: M = 294 s, SD = 28).
A second observer coded a randomly selected 19% of the corpus. Time-unit kappas reflecting the extent of agreement for positive, neutral, and negative maternal affect within a 2-s tolerance were .90 during play and .81 during feeding; comparable kappas for infant affect were .60 and .67. Interpretation of Kappa depends on the number of categories; for 3 codes whose frequencies are highly variable, as here, Kappa scores above .83, .68, and .55, result when observers are 95%, 90%, and 85% accurate (see Bakeman & Quera, 2011, pp. 66–68, 165–166). To assess the extent of affective matching, we then computed the proportion of time (expressed as a percentage) that mothers matched the valence of their infants’ positive affective states (given that their infants were in positive affective states).
Maternal Sensitivity: Ratings of Global Sensitivity
To rate women’s global sensitivity, nine rating scales were taken from the standardized rating scales of Ainsworth (1969), Clark (1985), and Campbell and colleagues (aNICHD Early Child Care Research Network, 1999a). This set of scales was selected to assess the quality of the mother’s interactive behavior with her infant and were chosen to reflect parenting characteristics known to be associated with depression in mothers (Lovejoy et al., 2000): insensitive parenting (reflected by sensitivity/responsiveness to nondistress), intrusiveness (reflected by intrusiveness and cooperation vs. interference), (low) positive affect (reflected by positive regard for the child, warmth, and stimulation of development), maternal withdrawal (reflected by detached/disengaged, flat affect), and negative affect (reflected by quality and amount of physical contact: negative). Scores for each of the scales are based on a 4- or 5-point Likert scale and take into consideration both the quality and quantity or intensity of the behavior measured in the scale. Raters assign a score based on whether the behavior is characteristic or not characteristic of the mother or some gradient in between. Raters assigned scores separately for the play and feeding conditions without knowledge of other information on mothers or babies. Interrater reliability was assessed for a randomly selected subset of play (17%) and feeding (20%) videos. Raters nearly always were in agreement within 1 point on each rating scale (feeding range 92–100% agreement within 1 point; play range 93–100% agreement within 1 point), indicating excellent reliability.
Global sensitivity summary scores were computed separately for both feeding and play conditions and were based on the 9 ratings just described. First, the 1–4 rating items were rescaled 1–5 (2 became 2.33, 3 became 3.67, and 4 became 5), then the summary score was the mean of the items, computed so long as no more than 2 were missing; the Cronbach’s alpha for the play summary score was .90 and for the feeding summary score was .89. Descriptive statistics for the separate items are given in Table 3.
TABLE 3.
Descriptive Statistics for Maternal Sensitivity Rating Scale Items
| Variable | M | SD | min | max | n |
|---|---|---|---|---|---|
| Play | |||||
| Sensitivity/responsiveness to nondistress | 3.54 | 1.01 | 1 | 5 | 71 |
| Intrusiveness | 2.43 | 1.01 | 1 | 5 | 72 |
| Cooperation vs. interference | 3.58 | 0.87 | 1 | 5 | 72 |
| Positive regard for the child | 3.56 | 1.09 | 1 | 5 | 72 |
| Warmth | 3.40 | 0.91 | 1 | 5 | 72 |
| Stimulation of development | 2.90 | 0.89 | 1 | 5 | 71 |
| Detached/disengaged | 2.24 | 0.96 | 1 | 5 | 72 |
| Flat affect | 2.22 | 0.97 | 1 | 5 | 72 |
| Quality and amount of physical contact: negative | 4.38 | 0.62 | 2 | 5 | 72 |
| Feeding | |||||
| Sensitivity/responsiveness to nondistress | 3.86 | 1.17 | 1 | 5 | 75 |
| Intrusiveness | 1.34 | 0.70 | 1 | 3.67 | 75 |
| Cooperation vs. interference | 3.93 | 0.83 | 2 | 5 | 74 |
| Positive regard for the child | 3.76 | 1.17 | 1 | 5 | 75 |
| Warmth | 3.16 | 1.04 | 1 | 5 | 75 |
| Stimulation of development | 3.33 | 1.37 | 1 | 5 | 64 |
| Detached/disengaged | 1.87 | 1.06 | 1 | 5 | 75 |
| Flat affect | 2.07 | 1.14 | 1 | 5 | 75 |
| Quality and amount of physical contact: negative | 4.92 | 0.36 | 3 | 5 | 75 |
Note. All items rescaled 1–5.
Data Analysis and Modification
Before conducting correlation and multiple regression analyses, we first examined the distributional properties of the variables. For chronicity of depression symptom levels, we found that the number of months BDI-II score exceeded 13 was positively skewed (standardized skews > 2.58) as was the three-level variable we had proposed: chronicity recoded as 0 = 0 months, 1 = 1 month, 2 = 2 or more. Consequently, for multiple regression analyses we renamed these variables BDI-II > 13 during pregnancy and BDI-II > 13 postpartum, binary recoded with 0 = no months > 13 and 1 = 1 or more months > 13; but used the three-level variable to address our questions about chronicity with t-tests subsequent to the regression analyses. BDI-II scores at 12 months were likewise positively skewed, but a square-root transformation—used for subsequent analyses—resulted in an acceptable standardized skew (0.42). Standardized skews for the remaining variables were acceptable (they ranged from –2.55 to 2.32).
RESULTS
Preliminary Analyses and Descriptive Statistics
Table 4 gives descriptive statistics for predictor and outcome variables, and Table 5, which includes background variables (infant gender, maternal age and education), gives their correlations. With regard to the background variables, maternal age correlated strongly with maternal education and weakly with income, whereas education and income correlated moderately (following Cohen, 1988, we refer to correlations of .10 as weak, .30 as moderate, and .50 as strong). Maternal age also correlated with our four outcome variables: weakly with affective matching during play and feeding, weakly with sensitivity rated during play, and moderately with sensitivity rated during feeding. Infant gender had little association with outcome, with one exception—mothers’ affective matching during play was higher with female then male infants (.54 vs..39, SD = .21 and .23, r = –.32, p = .005)—whereas maternal education was weakly to moderately associated with the other three outcomes.
TABLE 4.
Descriptive Statistics for Predictor and Outcome Variables
| Variable | M | SD | min | max | n |
|---|---|---|---|---|---|
| Maternal personal characteristics | |||||
| # months BDI-II > 13 during pregnancy1 | 1.0 | 1.4 | 0 | 6 | 76 |
| # months BDI-II > 13 postpartnum1 | 0.7 | 1.2 | 0 | 6 | 76 |
| Trait anxiety | 37.3 | 10.3 | 20 | 63 | 75 |
| BDI-II, 12 months postpartum | 5.8 | 6.2 | 0 | 25 | 73 |
| Context | |||||
| Social context | 80.0 | 7.2 | 66.7 | 96.3 | 76 |
| Infant temperament | |||||
| Negative Affectivity, 3 months | 3.04 | 0.78 | 1.59 | 5.54 | 71 |
| Surgency/Extraversion, 3 months | 4.29 | 0.92 | 2.12 | 6.70 | 71 |
| Orienting/Regulation, 3 months | 4.98 | 0.61 | 3.46 | 6.05 | 71 |
| Outcome | |||||
| Affective matching during play | 47 | 23 | 0 | 95 | 73 |
| Affective matching during feeding | 21 | 14 | 0 | 60 | 74 |
| Sensitivity rated during play | 3.61 | 0.70 | 1.96 | 5.00 | 72 |
| Sensitivity rated during feeding | 3.97 | 0.76 | 2.00 | 5.00 | 75 |
Note. BDI-II: Beck Depression Inventory, Second Edition.
Number of months in which BDI-II scores exceeded 13, indicating at least mild depression.
TABLE 5.
Correlations Between Background, Predictor, and Outcome Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Infant gender1 | – | ||||||||||||||
| 2. Maternal age | −.01 | – | |||||||||||||
| 3. Maternal education2 | −.03 | .52** | – | ||||||||||||
| 4. BDI-II > 13 during pregnancy2 | .08 | −.32** | −.35** | – | |||||||||||
| 5. BDI-II > 13 postpartum2 | .04 | .06 | .00 | .23* | – | ||||||||||
| 6. Trait anxiety | .01 | −.11 | −.18 | .57** | .20 | – | |||||||||
| 7. BDI–II, 12 months postpartum | .17 | .17 | .09 | .16 | .52** | .30** | – | ||||||||
| 8. Social context | −.15 | .04 | .25* | −.59** | −.31** | −.67** | −.38** | – | |||||||
| 9. Income4 | .03 | .29* | .47** | −.16 | .05 | −.10 | .10 | .23* | – | ||||||
| 10. Negative Affectivity, 3 months | −.09 | −.22 | −.19 | .23 | .03 | .43** | .17 | −.41** | −.12 | – | |||||
| 11. Surgency/Extraversion, 3 months | −.02 | −.39** | −.40** | .04 | −.05 | −.04 | −.22 | .12 | −.22 | .19 | – | ||||
| 12. Orienting/Regulation, 3 months | .05 | −.28* | −.31** | .16 | .14 | −.04 | −.17 | .14 | −.36** | −.20 | .68** | – | |||
| 13. Affective matching during play | −.32** | .15 | .28* | −.39** | −.10 | −.40** | −.13 | .42** | .31** | −.22 | −.09 | −.05 | – | ||
| 14. Affective matching during feeding | .08 | .24* | .18 | −.16 | .01 | −.24* | −.03 | .17 | .15 | −.08 | −.07 | −.05 | .19 | – | |
| 15. Sensitivity rated during play | −.06 | .25* | .26* | −.33** | −.26* | −.25* | −.08 | .28* | .21 | −.19 | −.29* | −.27* | .38** | .34** | – |
| 16. Sensitivity rated during feeding | −.02 | .46** | .31** | −.26* | .07 | −.30** | .11 | .25* | .22 | −.13 | −.01 | .09 | .33** | .57** | .35** |
Note. N = 67–76 due to some missing data. BDI-II = Beck Depression Inventory, Second Edition.
Infant gender coded 0 = female, 1 = male.
Maternal education coded 1= completed high school, 2= completed college, 3 = some post-college.
BDI-II > 13 coded 0 = no months and 1 = one or more months in which BDI-II scores exceeded 13.
Income coded 1= $10,000–$50,000, 2= $51,000–$75,000, 3 = $51,000–$75,000, 4 = > $100,000.
p < .05.
p < .01.
Figure 1 portrays the results of regressing the outcome variables on the three categories of predictor variables we defined: maternal personal characteristics, context, and early infant temperament. Given the moderate correlation between infant gender and affective matching during play, and the weak-to-moderate correlations between maternal age and the other three outcomes, we considered entering these two variables first in hierarchic regression models (as what are often called covariates), but realized this would obscure what we wanted to discover: the relative strength of the predictor categories in accounting for variation in outcome. When one variable correlates more strongly with an outcome than other variables (as maternal age with sensitive rated during feeding, r = .46), and when it correlates with those other variables, entering it first will obscure contributions of the other variables. Consequently, for each regression, first we entered variables in one of the predictor categories (Step 1) and then added either infant gender or maternal age second (Step 2) so that we could gauge its additional effect, above and beyond that of the variables in the particular category. In the following sections, we rely primarily on Table 5 when discussing effects of individual predictor variables (the rs) and Figure 1 when discussing effects of the sets of variables in the three categories working in concert (the R2s) and the additional effects of infant gender or maternal age (the ΔR2s).
Figure 1.
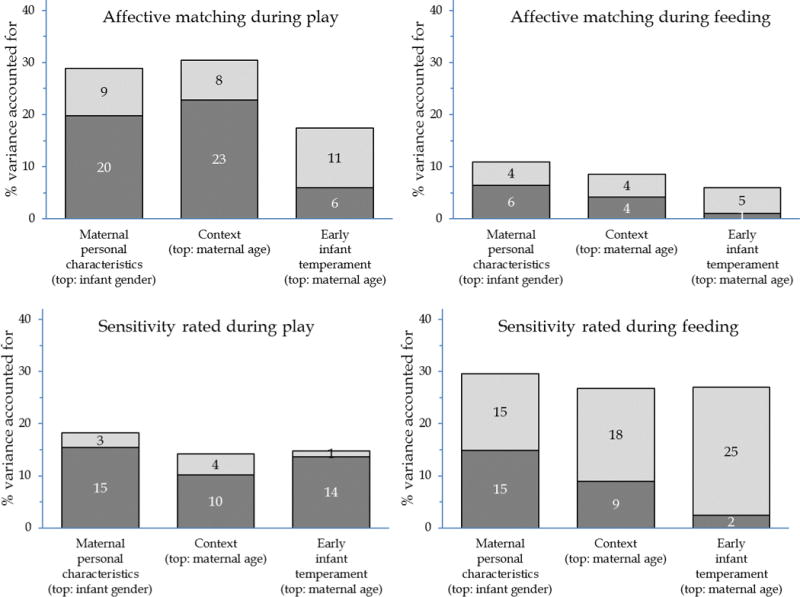
N = 71, 71, 70, and 72 for affective matching during play and feeding and for sensitivity rated during play and feeding, respectively, due to missing data. The figure shows R2 and ΔR2 for 12 hierarchic multiple regressions, one for each of the four outcomes for each of three categories, when variables for the specified category are added first and either infant gender or maternal age second.
Hypothesis 1: Effects of Depression and Anxiety
Out first hypothesis predicted that at least 1 month of clinically significant levels of depression (BDI > 13) during pregnancy and the first 6 months postpartum, elevated depression symptom levels at 12 months postpartum, and elevated trait anxiety symptom levels (maternal personal characteristics) would be associated with worse outcome. Trait anxiety and clinically significant levels of depression during pregnancy stood out (see Table 5). Higher trait anxiety was consistently associated with less sensitive parenting: correlations with all four outcomes were weak or moderate and statistically significant (ps = .001, .038, .037, .009). A clinically significant level of depression symptoms during pregnancy was also consistently associated with less sensitive parenting: correlations with all but affective matching during play were moderate and statistically significant (ps = .001, .16, .005, .026). Moreover, the four correlations of the pregnancy measure with outcome were all greater than the corresponding correlations for both the postpartum measure and the BDI scores 12 months postpartum (the difference between the pregnancy and postpartum correlations with affective matching during play, and the differences between pregnancy and postpartum and between pregnancy and 12 months postpartum correlations with sensitivity rated during feeding, were significant, p < .05).
In the regression models (see Figure 1), the set of personal characteristic variables, working in concert, accounted for significant variation in affective matching during play and sensitivity rated during both play and feeding (20%, 15%, and 15%; ps = .005, .026, .027), but not for affective matching during feeding (6%, p = .35).
To determine whether chronicity per se was associated with affective matching or maternal sensitivity during play or feeding, we used t-tests. First, we compared the mothers whose BDI scores exceeded 13 for 1 month with the mothers whose BDI scores exceeded 13 for 2 or more months during pregnancy. Second, we made the same comparison, but for the postpartum period. None of the eight t-tests was significant: t-ratios varied from 0.21–1.19, dfs from 25–33, η2s from .001–.054, and ps from .24–.84.
Hypothesis 2: Effects of Social Support, Marital Satisfaction, and Stress
Our second hypothesis predicted that fewer and less satisfying social supports, lower levels of dyadic (or marital) satisfaction, and perception of higher stress (both over the course of pregnancy and the first year postpartum), as well as lower income, would be associated with worse outcome. As noted earlier, the scores we analyzed were averaged over pregnancy and postpartum due to strong correlations. The size of the social support network stood out (see Table 6). A smaller size was consistently associated with less sensitive parenting: correlations with all four outcomes were weak or moderate and statistically significant (ps = .002, .028, .041, .049). Affective matching during play was the outcome most affected by context. In addition to network size, lower dyadic adjustment, more perceived stress (Table 6), and less income (Table 5) were associated with less affective matching during play—all moderate, statistically significant correlations (ps = .002, .001, .008). Additionally, lower dyadic adjustment was associated with lower sensitivity rated during feeding and greater perceived stress was associated with lower sensitivity rated during play (see Table 6)—both weak or moderate, statistically significant correlations (ps = .006, .019).
TABLE 6.
Correlations Between Individual Context and Outcome Variables
| Outcome variable | Social support – network size | Social support – satisfaction | Dyadic Adjustment Scale | Perceived Stress Scale |
|---|---|---|---|---|
| Affective matching during play | .36** | .16 | .35** | −.38** |
| Affective matching during feeding | .26* | .03 | .15 | −.05 |
| Sensitive parenting during play | .24* | .09 | .20 | −.28* |
| Sensitive parenting during feeding | .23* | .10 | .31** | −.11 |
Note. N = 72–75 due to missing data. The context variables were computed as the mean of their values during pregnancy and postpartum.
p < .05.
p < .01.
In the regression models (see Figure 1), a summary index formed from the context variables and income, working in concert, accounted for significant variation in affective matching during play and sensitivity rated during both play and feeding (23%, 10%, 9%; ps < .001, .024, .034), but not for affective matching during feeding (4.1%, p = .22).
Hypothesis 3: Effects of Infant Temperament
Our third hypothesis predicted that higher negative affectivity at 3 months would be associated with worse outcome. As an exploratory matter, we examined associations of the other two aspects of infant temperament, but made no specific predictions. Sensitivity rated during play seemed more affected by infant temperament at 3 months than the other outcomes (see Table 5). Higher negative affectivity, surgency/extraversion, and orienting/regulation were all associated with lower sensitivity rated during play; weakly and not significantly for negative affectivity (p = .12), but moderately and significantly for surgency/extraversion and orienting/regulation (ps = .027, .019). Higher negative affectivity also correlated weakly and not significantly with affective matching during play and sensitivity rated during feeding (ps = .068, .30).
In the regression models (see Figure 1), the three aspects of temperament at 3 months, working in concert, accounted for significant variation only in sensitivity rated during play (14%, p = .025).
Infant Gender and Maternal Age
In the regression model for affective matching during play (see Figure 1), infant gender accounted for additional significant variation above that accounted for by variables in each of the three predictor categories (9%, 8%, 11%; ps = .005, .008, .004; for maternal personal characteristics, context, and early infant temperament, respectively). These significant associations with infant gender reflect the finding, described earlier, that mothers’ affective matching during play was higher with female than male infants. Similarly, in the regression model for affective matching during feeding marginally (4%, 4%, 5%, ps = .075, .069, .072) and for sensitivity rated during feeding significantly (15%, 18%, 25%, p < .001 for all), maternal age accounted for additional significant variation. During feeding, comparing mothers under 30 to those 30 or older, affective matching was 18% versus 23% and their mean sensitivity rating was 3.65 versus 4.24.
DISCUSSION
We extended models of determinants of sensitive parenting by mothers in normative populations to the study of determinants of sensitive parenting of 12 month olds in women at risk for perinatal depression due to their history of major depression episodes prior to pregnancy. Such women, relative to the general population, have higher rates of perinatal depression and anxiety, their infants have higher levels of negative affectivity, and their lives are more stressful. Essentially, these mothers share a trifecta of issues that have been found to interfere with sensitive parenting in studies of normative populations, yet have received minimal attention in studies of sensitive parenting.
Our findings on women’s personal characteristics suggest that, among women with histories of depression prior to pregnancy, even one month of clinically significant symptom levels, suggestive of depression recurrence, during pregnancy, should be given consideration in understanding who may engage in less sensitive parenting of their 12 month olds. This finding is all the more remarkable given the absence of a role of postpartum depression symptom levels, even concurrent with the sensitivity measures. The findings are consistent with Belsky and colleagues’ model (Belsky et al., 2005), giving precedence to earlier, relative to more proximal, experiences in the prediction of sensitive parenting. In contrast to Campbell et al. (1995) and the NICHD (1999b) study’s findings on chronicity, our findings suggested that even a single pregnancy month during which depressive symptoms were at a clinically significant level for at least 2 weeks was sufficient to predict women’s insensitive parenting with their 12-month-old infant.
As predicted, another personal characteristic, trait anxiety, yielded strong and consistent findings. Women who are highly anxious may be less able to help their infants regulate their affective states, one of the central roles of parenting infants, with important implications for infants’ development of stress regulatory abilities and the later development of an anxiety disorder (Newman, Harris, & Allen, 2011). Our findings on anxiety as a predictor of sensitivity are consistent with descriptions of under-responsiveness that others have noted in mothers with mixed anxiety and depression (for a review, see Kaitz & Maytal, 2005). More broadly, our finding contributes to the literature on maternal personality and parenting (McCabe, 2014).
Next, we turned to our second hypothesis, that lower levels of sensitivity would be associated with mothers’ perception of having higher stress, fewer and less satisfying supports, lower levels of marital/dyadic satisfaction both over the course of pregnancy and the first year postpartum, and lower income. We found that the clearest and strongest associations were with smaller social network size, although lower dyadic adjustment, more perceived stress, and less income all played roles and especially in relation to sensitivity indexed by affective matching during play. The social context variables were highly intercorrelated, and each was also highly correlated from pregnancy to the postpartum, and we relied on a summary score, which was a significant predictor of sensitivity in three of the four models, all but for affective matching during feeding. Overall, consistent with findings on predictors of sensitive parenting in normative populations and knowledge of the importance of social context in the understanding of depression, we found support for our prediction that poorer social context would be associated with less sensitivity.
The high degree of association between context measured at the two time points suggests that families for whom social context raises concerns about the potential for less sensitive parenting can be identified during pregnancy, when preventive interventions might be delivered most effectively, potentially precluding the likelihood of infants being exposed to insensitive parenting. Taken together, these findings suggest that perceptions of stress, social support, and dyadic distress, which emerge during pregnancy, and lower income, may have pernicious and enduring effects on sensitive parenting.
In addition to mothers’ personal characteristics and context, comprehensive models of parenting include considerations of infant contributions to the dyad, particularly infant temperament. Thus, with our third hypothesis, we tested theoretically and empirically based hypotheses on the role of early infant negative affectivity and also, in an exploratory manner, examined the other two temperament factors in early infancy. Contrary to our hypothesis, negative affectivity at 3 months of age was only weakly and not significantly associated with sensitivity, and that was solely for sensitivity rated during play. Zero-order correlations revealed that higher surgency/extraversion and orienting/regulation at 3 months were associated with lower rated sensitivity during play (but not feeding). Overall, temperament accounted for a significant portion of the variance in sensitivity during play. Taken together, these findings suggest an important, albeit limited role of the broader construct of early infant emotionality or affectivity, rather than positive (surgency/extraversion) or negative affectivity per se, on later qualities of sensitive parenting, consistent with how some researchers conceptualize the core structure of temperament (Goldsmith & Campos, 1990).
It should be noted that our ability to predict maternal sensitivity differed across conditions. Our predictive models were more often supported for sensitive parenting during play than during feeding. Others have also found differences in the ways mothers and their infants interact depending on the condition. Four-month-old infants have been found to be less responsive and less spontaneous during feeding when compared to other caregiving conditions, which may reflect feeding potentially being a more structured interaction (Seifer, Sameroff, Anagnostopolou, & Elias, 1992). Similarly, mothers in the Seifer et al. study were observed to be significantly less responsive, less spontaneous, and more negative with their infants in feeding as compared to other caregiving conditions, suggestive of the transactional nature of the interaction. Infant physiology may help explain some of these observed differences. For example, the normative reduction in respiratory sinus arrhythmia (RSA) associated with feeding (Porges & Furman, 2011) may necessitate a lowered capacity for social engagement. Such a tradeoff may help account for infants’, and by proxy mothers’, differential interactive behaviors during feeding as compared to play (Beauchaine, 2015). With this understanding of how sensitive parenting may differ across conditions, it is up to future studies to replicate our findings and continue to develop and test models of the predictors of maternal sensitivity during feeding as well as play.
Our study findings should be interpreted in terms of several limitations. First, the findings can only be generalized to women with histories of major depressive episodes prior to pregnancy. Given their elevated risk for a perinatal depression episode or clinically significant symptom levels, this is an important group to understand. Even their relatively low levels of depression symptoms were found to make significant and meaningful contributions to the prediction of sensitive parenting. Moreover, it is increasingly understood that large percentages of women with perinatal depression have a history of past depression (Kettunen, Koistinen, & Hintikka, 2014). Nonetheless, they are likely to differ in important ways from women whose perinatal depression is their first episode. Second, we sampled pregnant women who were seeking routine prenatal care or who responded to media announcements about a mother-baby study rather than a clinical sample. Pregnant women seeking care for treatment or prevention of depression may differ in key ways from this community sample. Third, the findings can only be generalized to adult women having their first baby as models of sensitive parenting are likely to differ in teen mothers and in multiparous mothers (Fleming, 1990). Fourth, because of a set protocol, we were unable to test order effects between feeding and play. Fifth, our sample size was not sufficient to allow us to test moderated relations among the predictors. Studies with large samples might examine, for example, potential protective effects of supportive social context or of temperament and social context, although it may be that such effects work only at the extremes of risk for poor parenting (Belsky et al., 2005; Paulussen-Hoogeboom et al., 2007). More broadly, Bornstein (2016) points to the next steps in this line of research involving building models with multiple determinants of parenting, testing a full range of possible ways that determinants may combine. Sixth, our observations were brief snapshots of mother-infant interaction, although the length of observations was consistent with well-established procedures (Clark, 1985) and associations between depression in mothers and observed parenting have been found to yield larger effect sizes for observations that were shorter (1–10 min) rather than longer (11–59 min or 60 min or more) and to not moderate the association (Lovejoy et al., 2000). Seventh, although we created our sensitivity scores to address concerns that had been raised in the literature and to reflect well studied definitions of sensitivity, this score is but one of several alternative approaches. Eighth, although our sample was representative of the proportion of African American families in the region from which we recruited, our sample size precluded our consideration of culture, which is known to play a role in parenting of infants (Bornstein & Tamis-LeMonda, 2014). Ninth, attrition was high, most likely reflecting the burden we imposed on pregnant women with our monthly assessments through pregnancy and the first 6 months postpartum and again at 12 months postpartum. Nonetheless, the retained women did not differ from those who were lost to follow up on any demographic or depression variable that would suggest meaningful differences.
Despite these limitations, the study had several strengths. First was the prospective, longitudinal design, enabling the study to show, for example, how prenatal experiences were associated with mothers’ sensitivity with their 12-month-old infants without having to rely on retrospective reports. Second, many studies of predictors of parenting studied single or a related set of predictors in isolation, such as depression per se, whereas this study, more consistent with family systems theory (Bornstein & Sawyer, 2005), examined a comprehensive set of theory- and empirically based predictors. Third, we defined maternal sensitivity with a measurement approach that took into account the potential contribution of global qualitative ratings as well as affective matching from coded data. Although others have measured sensitivity in ways similar to one or both of these measures, our study benefited from being able to examine predictors of a multi-method conceptualization and measurement of sensitivity. Fourth, we observed parenting during two ecologically valid conditions; our findings support the importance of taking condition into account in studying sensitive parenting.
IMPLICATIONS FOR PRACTICE, POLICY, AND RESEARCH.
The findings have implications for practice, policy, and future studies. First, consistent with increasing understanding of the role of prenatal depression on offspring development (Stein et al., 2014), our findings suggest that prevention of depression recurrence during pregnancy may potentially have the additional benefit of women subsequently engaging in more sensitive parenting. Mindfulness-based cognitive therapy for the prevention of perinatal depression recurrence (MBCT-PD) has been found to be effective among pregnant women at elevated risk for depression recurrence; future studies might examine MBCT-PD’s potential to enhance sensitive parenting (Dimidjian et al., 2016). Second, our findings suggest the importance of intervening during pregnancy in women’s social support network, not waiting until the baby is born. In other work, we found that with persistent perinatal depression, fathers become less involved with their infants over time (Goodman, Lusby, Thompson, Newport, & Stowe, 2014), further suggesting the need to intervene early, to either strengthen couples’ relationship or enlist the partner to help the women prevent depression recurrence. Third, our findings build on those showing association between depression and parenting qualities by suggesting that, among women at risk for perinatal depression, there is a set of personal qualities, contextual, and infant temperament characteristics that are associated with insensitive parenting. These can be used as intervention targets among those most likely to engage in insensitive parenting. Fourth, our small-to-moderate effect sizes suggest that sensitivity of parenting is rather robust, even among women with histories of depression; further study is needed of protective factors that support such resilience.
Acknowledgments
We thank Florence Wilson, Margaret Dennison, Charmayne Dunlop-Thomas, Jennifer Hamel, Jill Mast, and Amanda Whittaker who contributed to the overall conduct of the study, the women who tirelessly participated, and many undergraduate students who assisted with coding and rating.
FUNDING
This research was supported by a grant from the National Institute of Mental Health, 1P50MH58922-01A1.
Contributor Information
Sherryl H. Goodman, Department of Psychology, PAIS Building, Room 467, Emory University, Atlanta, GA 30322. Phone: 404 727 4134. Fax: 404 727 0372
Roger Bakeman, Georgia State University.
Meaghan McCallum, Emory University.
Matthew H. Rouse, Emory University
Stephanie F. Thompson, Emory University
References
- Adamson LB, Bakeman R, Deckner DF, Nelson PB. Rating parent–child interactions: Joint engagement, communication dynamics, and shared topics in autism, down syndrome, and typical development. Journal of Autism and Developmental Disorders. 2012;42:2622–2635. doi: 10.1007/s10803-012-1520-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth MDS. Maternal sensitivity scales: The Baltimore Longitudinal Project (1969) 1969 Retrieved November 21, 2015, from http:/www.psychology.sunysb.edu/ewaters/measures/senscoop.htm.
- Ainsworth MDS, Bell SMV, Stayton DJ. Individual differences in strange situation behavior of one-year-olds. In: Schaffer HR, editor. The origins of human social relations. New York: Academic Press; 1971. pp. 17–57. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Bakeman R, Quera V. Analyzing interactions: Sequential analysis with SDIS and GSEQ. NY: Cambridge University Press; 1995. [Google Scholar]
- Bakeman R, Quera V. Sequential Analysis and Observational Methods for the Behavioral Sciences. Cambridge, UK: Cambridge University Press; 2011. [Google Scholar]
- Beauchaine TP. Respiratory Sinus Arrhythmia: A Transdiagnostic Biomarker of Emotion Dysregulation and Psychopathology. Curr Opin Psychol. 2015;3:43–47. doi: 10.1016/j.copsyc.2015.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. Second. San Antonio: Texas: The Psychological Corporation; 1997. [Google Scholar]
- Beebe B, Jaffe J, Markese S, Buck K, Chen H, Cohen P, Feldstein S. The origins of 12-month attachment: A microanalysis of 4-month mother–infant interaction. Attachment & Human Development. 2010;12:3–141. doi: 10.1080/14616730903338985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Belsky J, Jaffee SR, Sligo J, Woodward L, Silva PA. Intergenerational Transmission of Warm-Sensitive-Stimulating Parenting: A Prospective Study of Mothers and Fathers of 3-Year-Olds. Child Development. 2005;76:384–396. doi: 10.1111/j.1467-8624.2005.00852.x. [DOI] [PubMed] [Google Scholar]
- Bigelow AE, MacLean K, Proctor J, Myatt T, Gillis R, Power M. Maternal sensitivity throughout infancy: Continuity and relation to attachment security. Infant Behavior and Development. 2010;33:50–60. doi: 10.1016/j.infbeh.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Bornstein MH. Handbook of parenting. 2nd. Vol. 4. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2002a. (Social conditions and applied parenting). [Google Scholar]
- Bornstein MH. Parenting infants. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2002b. [Google Scholar]
- Bornstein MH. Determinants of parenting. In: Cicchetti D, editor. Developmental Psychopathology: Risk, Resilience, and Intervention. 3rd. Vol. 4. Hoboken, NJ: Wiley; 2016. pp. 180–270. [Google Scholar]
- Bornstein MH, Sawyer J. Family systems. In: McCartney K, Phillips D, editors. Blackwell Handbook of Early Childhood Development. Malden, MA: Blackwell; 2005. pp. 381–398. [Google Scholar]
- Bornstein MH, Tamis-LeMonda CS. Parent-infant Interaction. In: Bremner JG, Wachs TD, editors. The Wiley Blackwell Handbook of Infant Development. Second. Chichester, West Sussex, UK: Wiley & Sons; 2014. pp. 460–484. [Google Scholar]
- Britton JR. Infant temperament and maternal anxiety and depressed mood in the early postpartum period. Women & Health. 2011;51:55–71. doi: 10.1080/03630242.2011.540741. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: A study of psychiatric disorder in women. New York: Free Press; 1978. [Google Scholar]
- Campbell SB, Cohn JF, Meyers T. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1995;31:349–357. [Google Scholar]
- Cheadle JE, Amato PR. A quantitative assessment of lareau’s qualitative conclusions about class, race, and parenting. Journal of Family Issues. 2011;32:679–706. doi: 10.1177/0192513x10386305. [DOI] [Google Scholar]
- Clark R. The Parent-Child Early Relational Assessment: Instrument and manual. Madison: University of Wisconsin Medical School, Department of Psychiatry; 1985. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Dawson G, Frey K, Panagiotides H, Yamada E, Hessl D, Osterling J. Infants of depressed mothers exhibit atypical frontal electrical brain activity during interactions with mother and with a familiar, nondepressed adult. Child Development. 1999;70:1058–1066. doi: 10.1111/1467-8624.00078. [DOI] [PubMed] [Google Scholar]
- De Wolff MS, van IJzendoorn MH. Sensitivity and Attachment: A Meta-Analysis on Parental Antecedents of Infant Attachment. Child Development. 1997;68:571–591. doi: 10.1111/j.1467-8624.1997.tb04218.x. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Goodman S, Felder J, Gallop R, Brown A, Beck A. Staying Well During Pregnancy and the Postpartum: A Pilot Randomized Trial of Mindfulness-Based Cognitive Therapy for the Prevention of Depressive Relapse/Recurrence. Journal of Consulting and Clinical Psychology. 2016;84:134–145. doi: 10.1037/ccp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Healy B, Goldstein S, Guthertz M. Behavior-state matching and synchrony in mother-infant interactions of nondepressed versus depressed dyads. Developmental Psychology. 1990;26:7–14. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. New York. [Google Scholar]
- Fish M, Stifter CA. Mother parity as a main and moderating influence on early mother-infant interaction. Journal of Applied Developmental Psychology. 1993;14:557–572. [Google Scholar]
- Fleming AS. Hormonal and experiential correlates of maternal responsivenss in human mothers. In: Grasnegor NA, Bridges RS, editors. Mammalian parenting: Biochemical, neurobiological, and behavioral determinants. NY: Oxford University Press; 1990. pp. 184–208. [Google Scholar]
- Gartstein MA, Marmion J. Fear and positive affectivity in infancy: Convergence/discrepancy between parent-report and laboratory-based indicators. Infant Behavior and Development. 2008;31:227–238. doi: 10.1016/j.infbeh.2007.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behavior & Development. 2003;26:64–86. [Google Scholar]
- Goldsmith HH, Campos JJ. The structure of temperamental fear and pleasure in infants: A psychometric perspective. Child Development. 1990;61:1944–1964. [PubMed] [Google Scholar]
- Goldstein LH, Diener ML, Mangelsdorf SC. Maternal characteristics and social support across the transition to motherhood: Associations with maternal behavior. Journal of Family Psychology. 1996;10:60–71. [Google Scholar]
- Goodman SH, Lusby CM, Thompson K, Newport, D. J. Stowe ZN. Maternal depression in association with fathers’ involvement with their infants: spillover or compensation/buffering? Infant Ment Health J. 2014;35:495–508. doi: 10.1002/imhj.21469. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Tully EC. Recurrence of depression during pregnancy: Psychosocial and personal functioning correlates. Depression and Anxiety. 2009;26:557–567. doi: 10.1002/da.20421. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Quevedo KM. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Hammen C. Context of stress in families of children with depressed parents. In: Goodman SH, Gotlib IH, editors. Children of Depressed Parents: Mechanisms of Risk and Implications for Treatment. Washington, D.C.: American Psychological Association; 2002. pp. 175–202. [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Holcomb W, Stone L, Lustman P, Gavard JA, Mostello D. Screening for depression in pregnancy: Characteristics of the Beck Depression Inventory. Obstetrics and Gynecology. 1996;88:1021–1025. doi: 10.1016/s0029-7844(96)00329-8. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Siegle GJ. Methodological issues in the study of depression. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2nd. New York: Guilford; 2009. pp. 69–92. [Google Scholar]
- Kaitz M, Maytal H. Interactions between anxious mothers and their infants: An integration of theory and research findings. Infant Mental Health Journal. 2005;26:570–597. doi: 10.1002/imhj.20069. [DOI] [PubMed] [Google Scholar]
- Kettunen P, Koistinen E, Hintikka J. Is postpartum depression a homogenous disorder? Time of onset, severity, symptoms and hopelessness in relation to the course of depression. BMC pregnancy and childbirth. 2014;14:402. doi: 10.1186/s12884-014-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mangold INTERACT Quick Start Manual V2.4. Mangold International BfbH (Ed.) 2010 http://www.mangold-international.com/
- McCabe JE. Maternal personality and psychopathology as determinants of parenting behavior: a quantitative integration of two parenting literatures. Psychological Bulletin. 2014;140:722. doi: 10.1037/a0034835. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Westley DT, Gemmill AW. The mediating role of maternal responsiveness in some longer term effects of postnatal depression on infant development. Infant Behavior and Development. 2004;27:443–454. [Google Scholar]
- Misri S, Kendrick K, Oberlander TF, Norris S, Tomfohr L, Zhang HB, Grunau RE. Antenatal Depression and Anxiety Affect Postpartum Parenting Stress: A Longitudinal, Prospective Study. Canadian Journal of Psychiatry-Revue Canadienne De Psychiatrie. 2010;55:222–228. doi: 10.1177/070674371005500405. [DOI] [PubMed] [Google Scholar]
- Murray L, Stanley C, Hooper R, King F, Fiori-Cowley A. The role of infant factors in postnatal depression and mother-infant interactions. Developmental Medicine & Child Neurology. 1996;38:109–119. doi: 10.1111/j.1469-8749.1996.tb12082.x. [DOI] [PubMed] [Google Scholar]
- Newman LK, Harris M, Allen J. Neurobiological basis of parenting disturbance. Australian and New Zealand Journal of Psychiatry. 2011;45:109–122. doi: 10.3109/00048674.2010.527821. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Child Care and Mother-Child Interaction in the First 3 Years of Life. Developmental Psychology. 1999a;35:1399–1413. [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Chronicity of Maternal Depressive Symptoms, Maternal Sensitivity, and Child Functioning at 36 Months. Developmental Psychology. 1999b;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Paulussen-Hoogeboom MC, Stams GJJ, Hermanns J, Peetsma TT. Child negative emotionality and parenting from infancy to preschool: A meta-analytic review. Developmental Psychology. 2007;43:438. doi: 10.1037/0012-1649.43.2.438. [DOI] [PubMed] [Google Scholar]
- Phillips J, Sharpe L, Matthey S, Charles M. Subtypes of postnatal depression? A comparison of women with recurrent and de novo postnatal depression. Joournal of Affective Disorders. 2010;120:67–75. doi: 10.1016/j.jad.2009.04.011. [DOI] [PubMed] [Google Scholar]
- Planalp EM, Braungart-Rieker JM, Lickenbrock DM, Zentall SR. Trajectories of Parenting During Infancy: The Role of Infant Temperament and Marital Adjustment for Mothers and Fathers. Infancy. 2013;18:E16–E45. [Google Scholar]
- Porges SW, Furman SA. The early development of the Autonomic Nervous System Provides a Neural Platform for Social Behavior: A Polyvagal Perspective. Infant and Child Development. 2011;20:106–118. doi: 10.1002/icd.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raby KL, Roisman GI, Fraley RC, Simpson JA. The Enduring Predictive Significance of Early Maternal Sensitivity: Social and Academic Competence Through Age 32 Years. Child Development. 2014;86:695–708. doi: 10.1111/cdev.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. General Hospital Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Rochat P. The infant’s world. Cambridge: Harvard University Press; 2001. [Google Scholar]
- Rothbart MK, Derryberry D. Development of individual differences in temperament. In: Lamb ME, Brown AL, editors. Advances in Developmental Psychology. Vol. 1. Hillsdale, NJ: Erlbaum; 1981. pp. 37–86. [Google Scholar]
- Rouse MH, Goodman SH. Perinatal depression influences on negative affectivity: Timing, severity, and co-morbid anxiety. Infant Behavior & Development. 2014;37:739–751. doi: 10.1016/j.infbeh.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarason IG, Sarason B, Shearin E, Pierce G. A brief measure of social support: practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4:497–510. [Google Scholar]
- Seifer R, Sameroff AJ, Anagnostopolou R, Elias PK. Mother-infant interaction during the first year: Effects of situation, maternal mental illness, and demographic factors. Infant Behavior & Development. 1992;15:405–426. [Google Scholar]
- Seifer R, Schiller M, Sameroff AJ, Resnick S, Riordan K. Attachment, maternal sensitivity, and infant temperament during the first year of life. Developmental Psychology. 1996;32:12–25. [Google Scholar]
- Sharpley C, Rogers H. Preliminary validation of the abbreviated Spanier Dyadic Adjustment Scale: Some psychometric data regarding a screening test of marital adjustment. Educational and Psychological Measurement. 1984;44:1045–1050. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Sroufe LA, Egeland B, Carlson EA, Collins WA. The development of the person: The Minnesota study of risk and adaptation from birth to adulthood. New York: Guilford; 2005. [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Pariante CM. Effects of perinatal mental disorders on the fetus and child. The Lancet. 2014;384:1800–1819. doi: 10.1016/S0140-6736(14)61277-0. [DOI] [PubMed] [Google Scholar]
- Tronick E, Beeghly M. Infants’ meaning-making and the development of mental health problems. American Psychologist. 2011;66:107–119. doi: 10.1037/a0021631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA, Weinstock LM, Tolejko N. Marriage and Depression. In: Keyes CLM, Goodman SH, editors. Women and Depression: A Handbook for the Social, Behavioral, and Biomedical Sciences. NY: Cambridge University Press; 2006. pp. 219–240. [Google Scholar]
- Yen IH, Kaplan GA. Poverty area residence and changes in depression and perceived health status: evidence from the Alameda County Study. International Journal of Epidemiology. 1999;28:90–94. doi: 10.1093/ije/28.1.90. [DOI] [PubMed] [Google Scholar]


