Abstract
Background
Many organisations promote eHealth applications as a feasible, low-cost method of addressing mental ill-health and stress amongst their employees. However, there are good reasons why the efficacy identified in clinical or other samples may not generalize to employees, and many Apps are being developed specifically for this group. The aim of this paper is to conduct the first comprehensive systematic review and meta-analysis evaluating the evidence for the effectiveness and examine the relative efficacy of different types of eHealth interventions for employees.
Methods
Systematic searches were conducted for relevant articles published from 1975 until November 17, 2016, of trials of eHealth mental health interventions (App or web-based) focused on the mental health of employees. The quality and bias of all identified studies was assessed. We extracted means and standard deviations from published reports, comparing the difference in effect sizes (Hedge’s g) in standardized mental health outcomes. We meta-analysed these using a random effects model, stratified by length of follow up, intervention type, and whether the intervention was universal (unselected) or targeted to selected groups e.g. “stressed”.
Results
23 controlled trials of eHealth interventions were identified which overall suggested a small positive effect at both post intervention (g = 0.24, 95% CI 0.13 to 0.35) and follow up (g = 0.23, 95% CI 0.03 to 0.42). There were differential short term effects seen between the intervention types whereby Mindfulness based interventions (g = 0.60, 95% CI 0.34 to 0.85, n = 6) showed larger effects than the Cognitive Behaviour Therapy (CBT) based (g = 0.15, 95% CI 0.02 to 0.29, n = 11) and Stress Management based (g = 0.17, 95%CI -0.01 to 0.34, n = 6) interventions. The Stress Management interventions however differed by whether delivered to universal or targeted groups with a moderately large effect size at both post-intervention (g = 0.64, 95% CI 0.54 to 0.85) and follow-up (g = 0.69, 95% CI 0.06 to 1.33) in targeted groups, but no effect in unselected groups.
Interpretation
There is reasonable evidence that eHealth interventions delivered to employees may reduce mental health and stress symptoms post intervention and still have a benefit, although reduced at follow-up. Despite the enthusiasm in the corporate world for such approaches, employers and other organisations should be aware not all such interventions are equal, many lack evidence, and achieving the best outcomes depends upon providing the right type of intervention to the correct population.
Introduction
Mental health problems in the workforce are common and have a substantial impact on employee wellbeing, productivity, absenteeism, compensation claims, and the social welfare systems [1–3]. Reported annual productivity losses to organisations and workforces caused by mental health conditions are estimated at $225US billion in the USA [4] and £13 billion in the UK [5].
The majority of mental ill-health seen in the workforce is due to common mental disorders, most notably, depression and anxiety [6–8], accounting for up to 12% of the Australian working population [9]. However, common mental disorders may go unnoticed in the workplace, as they can often be characterized as work stress or other stress related conditions [7]. More severe mental illness is less common in the workplace, due to lower levels of unemployment in those with severe mental illness [10].
Over the recent decades, organisations have increasingly recognised the importance of maximizing employee health, both for ethical reasons, to improve productivity, meet legislation changes and reduce their cost burden [11,12]. While physical health promotion interventions are well established in many workplaces [13], workplace mental health interventions have lagged. Despite mental illness now being the leading cause of work incapacity and sickness absence [14], and depression estimated to be the leading cause of disability at work by 2020 [15], a recent systematic meta-review found that there no workplace mental health interventions that could be considered evidence-based [16].
The past decade has seen an explosion in the delivery of eHealth interventions targeting common mental illnesses such as depression and anxiety, as well as those focused upon broader concepts of stress and distress [17] through Apps and via the Internet. The components of these interventions have included Cognitive Behavioural Therapy, Stress Management, Mindfulness approaches and Cognitive training. Some eHealth interventions offer fully unguided self-help programs while others involve supported guidance throughout and are thus more costly [18]. Their effectiveness has been examined in both general population and in clinical settings. Two previous systematic review and meta-analysis found that eHealth interventions delivered to general population could both reduce and prevent depression and anxiety [11,19]. Similar results were found in a systematic review and meta-analysis of eHealth interventions in a clinical setting [20].
Thus there is currently ample evidence for the short and long term benefits for eHealth delivered Cognitive Behavioural Therapy (CBT) for treating anxiety and depressive conditions in both general population and clinical settings [21–23], with greater improvement shown for those interventions that include guidance throughout the intervention period [21,24]. Evidence has also emerged for the effectiveness of Mindfulness based eHealth interventions in improving symptoms in both unselected and symptomatic people [25].
However, we know employed people differ systemically from both general or clinical populations used in most eHealth studies (in terms of symptom profile, risks, function and response [26]) Therefore, this evidence may not be generalisable to the occupational setting.
Many workplaces now provide employees with access to mental health assistance, usually through Employee Assistance Programs (EAPs), providing employees with a range of integrated services including short term counseling, management consultations, organisational and team interventions, often with aggregate reporting to the organisation [27]. EAPs are estimated to cost US workplaces up to US$40.00 per person [28]. To mitigate the cost of these, many organisations are now providing eHealth interventions and applications into their workplace health management systems for employees, either by creating their own programs for internal use or buying commercially available products [29,30]. However there is no guidance on whether eHealth interventions are effective in the workplace, or even whether they may cause harm [30]. Given this gap in the evidence we undertook a systematic review of the effectiveness of eHealth interventions delivered to employees through the workplace with the aim of informing organisations and employees that eHealth interventions targeting mental ill-health and work stress are safe and effective.
Methods
This work complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [31].
We aimed to identify all published, peer reviewed, clinical trials including randomized controlled trials (RCTs), controlled trials & pre/post trials using an eHealth intervention targeted at employees that reported outcomes on a standardized mental health measure of depression, anxiety and/or stress.
Eligibility criteria
Inclusion
We included only studies evaluating the outcome of an eHealth based intervention, defined as a therapeutic intervention delivered through a website, smartphone or tablet App, focused on the mental health of employees. Participants of the studies had to be in current paid employment and working age adults between 18 to 65 years of age. Included studies were peer-reviewed articles published in English.
Exclusion
Studies were excluded from the review if they focused on volunteer workers, unemployed participants, general or clinical population studies that did not mention being targeted to employees or in a workplace setting, examined non-mental health outcomes, or used telephone and/or email interventions only. Studies without a control group were also excluded from the meta-analysis.
Search strategy
A thorough literature search was conducted using the electronic databases MEDLINE, PsycINFO, Cochrane Register of Controlled Trials (CENTRAL) and EMBASE for relevant articles published from 1975 (the first eHealth intervention for employees was identified in 2004 [32]) until 17 November 2016. Keywords were searched relating to ‘workplace’ and ‘intervention’ and ‘outcome’ and ‘study design’ and an example of a search strategy for these databases is displayed in S1 Table. To increase coverage for relevant databases, we also manually screened the table of contents of the Journal of Medical Internet Research, Journal of Internet Interventions, Occupational and Environmental medicine and the Journal of Occupational Environmental Medicine, as well as the reference list of included studies.
Study selection criteria
Identification
After duplicates were removed, authors (ES) screened all titles and abstracts to identify potentially relevant studies. Abstracts and Full-text versions of potentially eligible studies were independently assessed by two investigators (ES and IC). Disagreements were adjudicated in conjunction with the senior author (NG).
Data collection and coding of outcomes
We collected the mean, and standard deviation (SD) of standardized measures of (dis)stress, depression and/or anxiety, and sample size (n) of participants in each arm (intervention and control) at baseline and each follow-up. Where studies used a number of measures, these were pooled as a single composite Mental Health outcome. When SDs were not reported, we contacted the authors. Three authors were contacted, and two of those responded with relevant data [33,34]. In one study [35] the SD could not be obtained from the paper or the authors; effect sizes for this study were derived from 2-tailed p-value for Group × Time interaction and sample sizes. One author did not respond and we were unable to obtain data so this study was excluded from the meta-analysis [36].
Where studies reported results of the same intervention in different papers (e.g., a post intervention and follow-up study), papers were grouped together and treated as one study and we used the first follow-up outcome point in the analysis.
We then categorized the studies by intervention type, in which three main types were identified from the primary paper as to the main component of the intervention: Cognitive Behavioural Therapy (CBT), Stress Management, and Mindfulness-based treatments, and by whether the intervention was given to unselected employees (universal) or targeted to those selected for higher symptom scores or another indication of poorer mental health (indicated). Sensitivity analysis results were also assessed by whether the intervention was unguided (self-help) or guided (feedback, rather than just technical support, as this is known to affect the outcome [37].
Quality assessment and risk of bias within studies
The quality of the identified studies was assessed using the Downs and Black checklist [38]. Specifically developed for public health, and used previously in similar reviews in the field [16], the Downs and Black checklist demonstrates good inter-rater reliability (r = 0.75) and strong criterion validity (r = 0.90) [11]. The checklist has 27-items to score within five sub categories: reporting, external validity, internal validity -assessing risk of bias & confounding, and power. The checklist was modified to simplify the power item to a score of either zero = no or one = yes based on whether the studies reported sufficient power to detect a clinically significant effect, as reported in previous studies [11,39]. The maximum score for the modified checklist was 28 with most items reporting on yes = one, no = zero or unable to determine = zero, with the exception of one question that used yes = two, partially = one, and no = zero. The first author (ES) individually scored each included paper. Scores were pooled into four categories as used in other reviews [11]: Excellent = 26 to 28, Good = 20 to 25, Fair = 15 to 19 and Poor = 14 and less. Any rated poor were reviewed by an independent research assistant and discrepancies adjudicated by the senior author (NG) and excluded.
As a further standardized measure we assessed Risk of Bias using the Cochrane Guidelines [40]. For this analysis five of the six items (sequence generation, allocation concealment, assessor blinding, incomplete outcome data and selective outcome reporting) were used to assess bias as all of the trials included in the Meta-analysis had only a wait list control group, and it would be impossible for participants and personnel to be blinded to the arm that they were randomized to (S1 Fig).
Statistical analysis
The summary measure was the standardized mean difference (SMD, calculated as Hedge’s g), of change in the effect sizes between baseline and each follow-up. A positive effect size (SMD) indicated that the intervention group had superior effects to the control group. Using standard measures of effect size, SMDs of 0.2 were considered small, 0.5 moderate, and 0.8 large [41]. Precision of effect sizes was estimated using 95% confidence interval (CI). Pooling of effect sizes across studies was done using random effects model in Comprehensive Meta-Analysis V3. Random effects analysis was used as we could not make the assumption that these studies represented a common effect as the different types of interventions delivered may result in large heterogeneity [42].
Analyses were conducted in three stages, first, we combined results of all studies to achieve a combined effect size at each time point, immediately post-intervention and at follow-up. We then estimated pooled effect sizes for each of the three intervention types (CBT, Stress Management, and Mindfulness based interventions). Studies targeting unselected employees were analysed separately from those targeting ‘symptomatic’ (selected) employees such as those having reported increased ‘stress’ or having a mental health condition at baseline measures indicated for intervention. Studies were then stratified using the post-intervention and follow-up combined SMD for each study in each sub-group.
Heterogeneity of real effects across studies was quantified using the I2 statistic to estimate the proportion observed variance not due to sampling error.
To assess small study effect (in the case where at least 10 studies were available for analysis) we used a funnel plot for the overall effects and each of the grouped intervention types which compared the outcome effects with their standard errors. We used Egger regression test to further examine asymmetry of the funnel plot [43] with a statistical significance based on a P-value less than 0.05. In the case where at least 10 studies were available for analysis and a small study effect was found we used a Duval and Tweedie trim and fill to quantify the magnitude of small study effect [44].
Results
Search results
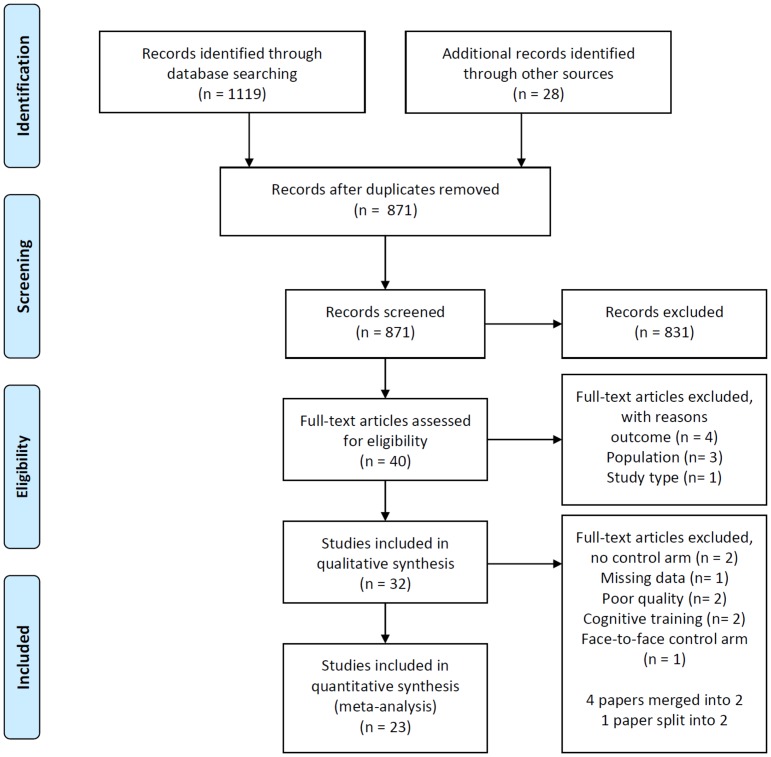
The search strategy identified a total of 1147 titles (Fig 1). After the removal of duplicates (n = 276), 871 titles and abstracts were reviewed by author (ES). Of those, 723 studies were excluded on the basis of the inclusion/exclusion criteria, leaving 108 studies potentially relevant to the research question. The 108 abstracts were examined by the two independent researchers (ES and IC), and 68 articles were excluded. Both researchers independently examined the full text of 40 articles, where a further 8 articles were excluded. The 32 remaining articles were identified as meeting criteria for quality assessment [32–37,45–71]. Four papers were identified as reporting on different follow-up periods and were merged [48,49] and [50,53]. After the quality assessment of all studies using the Down’ & Black Checklist, two studies were excluded from the analysis as they were found to be of ‘poor’ quality [45,55]. Two papers did not have a control group [56,57], and one study used a face-to-face control group [68]. One study [58] included two intervention groups, which were treated as two studies in the meta-analysis. The two intervention groups’ SMDs were computed and the mean (n) of the control group was evenly divided among each intervention group to ensure that control participants were only included once in the analysis. The two studies using cognitive training [59,60] were not included for the meta-analysis as the outcomes were not standardized mental health outcomes. One paper was excluded due to missing data [36]. This approach left 23 studies to be analysed in the meta-analysis, 22 of which were randomized controlled trials and a “controlled” trial [33].
Fig 1. Flow chart of studies selected.
Table 1 shows the details of each included intervention. Eleven studies were identified to have a CBT intervention [32,33,35,45–53,56,61], six studies described themselves as Stress Management [34,36,62–66], and six studies used Mindfulness-based approaches [57,58,67,69–71]. Of the CBT interventions, nine were web-based interventions while two were smartphone Apps. All of the Stress Management interventions were web-based interventions. Of the Mindfulness based interventions, five were web-based and one was on a smartphone App (Table 1).
Table 1. Studies included sorted firstly by intervention type and secondly by publication year.
| Study (ref #) | Type of intervention | Included in Meta-analysis | Targeted to symptomatic or high stressed participants? | Participants | Intervention, Duration + (n) | Control, n | Outcome(s) + Measure(s) | Baseline score (m,SD,n) | Post-intervention (from baseline) | Results—Post-intervention (m,SD,n) | Follow-up (from baseline) | Results—Follow-up (m,SD,n) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT based intervention | ||||||||||||
| Grime. (2004) (32)* | CBT | Yes | Yes | London, Occupational Health department. employees with >10 days sick leave in the past 6 months due to mental illness (n = 48) | ‘Beating the Blues’ a computerised CBT program for Depression and anxiety, 8 online sessions which last approximately an hour per week (n = 24) | WLC (n = 24) | Primary: Anxiety & Depression (HADS) | Intervention: Depression (7.96,3.43,24) Anxiety (11.75,3.87,24) Control: Depression (10.63,4.13,24) Anxiety (14.04,4.34,24) |
2 months | Depression Intervention (5.38, 3.93, 16) Control (8.61,3.86,23) Anxiety Intervention (10.13, 4.65,14) Control (12.00,4.31,23) |
3 months | Depression Intervention (5.00,4.12,13) Control (7.32,5.08,19) Anxiety Intervention (8.69,3.50,13) Control (9.47,5.26,19) |
| 6 months | Depression Intervention (5.07,4.57,14) Control (6.21,4.22,19) Anxiety Intervention (8.86,4.35,14) Control (9.16,4.37,19) |
|||||||||||
| Shimazu. et al. (2005) (45)* | CBT | Yes | No | Japan, any employee company wide in a construction machinery company (n = 225) | One-month web-based psycho-education based on social cognitive theory. Self-based program, 3 phases (5 chapters), (n = 112) | WLC (n = 113) | Primary: Stress (BJSQ) | Intervention: Stress (36.80,9.88,112) Control: Stress (38.30,9.39,113) |
5 weeks | Stress Intervention (35.70,5.68,105) Control (37.60,6.76,107) |
nil | not measured |
| Hasson. et al. (2005) (35)* ^ | CBT | Yes | No | Sweden, IT and media companies general employees (n = 317) | 12 month open access. Web-based self-help exercises—developed specifically for this study. Uses CBT techniques (n = 129) | WLC + info (n = 174) | Primary: Stress: (VAS) | Not reported | 12 months | Not reported | nil | not measured |
| Billings. et al (2008) # | CBT | Yes | No | USA, employees from a technology company on a health and activity promotion program (n = 309) | 3 month web-based. Participants could review sections more than once. Uses CBT—website is tailored around baseline answers for each participant depending on risks and needs (n = 154). | WLC (n = 155) | Primary: Stress: (symptoms of distress scale) Depression: (CES-D) Anxiety: (BAI) | Intervention: Stress (17.52,4.53,154) Depression (33.77,13.46,115) Anxiety (28.87,7.82,154) Control: Stress (16.81,3.78,155) Depression (32.15,10.08,155) Anxiety (27.98,7.43,155) |
3 months | Stress Intervention (16.03,4.18,113) Control (16.50,4.35,132) Depression Intervention (31.60,13.33,113) Control (31.57,10.56,132) Anxiety Intervention (27.54,7.53,113) Control (27.30,6.19,132) |
nil | not measured |
| Lappalainen. et al. (2013) (46) * ^ | CBT | Yes | Yes | Finland, males aged 28-58yrs with exhaustion, stress symptoms, or sleeping problems (n = 23) | ‘P4Well′, 3 month novel CBT intervention Delivered via multiple channels, including 3 group meetings, Internet/Web portal, mobile phone applications, and personal monitoring devices. (n = 11) | WLC (n = 12) | Primary: Depression–(BDI 21-item) | Intervention: Depression (14.64,7.61,11) Control: Depression (13.33,9.24,12) |
3 months | Depression Intervention (6.20,3.30,11) Control (9.30,7.10,12) |
6 months | Depression Intervention (6.20,3.30,11) Control not measured |
| Boiler. et al. (2014) (47)* ^ | CBT | Yes | No | Netherland, Nurses and allied health professionals general employees (n = 423) | Based on screening results participants were offered a tailored web-based interventions ranging from 4 to 8 weeks (n = 212) | WLC (n = 211) | Primary: Depression (BSI), Secondary: Anxiety (BSI) | Intervention: Depression (0.31,0.32,212) Anxiety (0.21,0.24,212) Control: Depression (0.30,0.35,212) Anxiety (0.25,0.32,211) |
3 months | Depression Intervention (0.24,0.32,143) Control (0.26,0.35,82) Anxiety Intervention (0.16,0.24,143) Control (0.19,0.30,82) |
6 months | Depression Intervention (0.22,0.31,138) Control (0.29,0.35,70) Anxiety Intervention (0.17,0.24,138) Control (0.22,0.32,70) |
| Geraedts. et al. (2014) (two papers 48 & 49)* ^ | CBT | Yes | Yes | Netherland, employees from banking companies with elevated Depression (n = 231) | Web-based guided self-help intervention, called Happy@Work, 6 weekly sessions consisted of problem solving techniques and CBT, complete an assessment each week to move on (n = 116) | WLC (n = 115) | Primary: Depression (CES-D), Secondary: anxiety (HADS) | Intervention: Depression (25.70,7.50,116) Anxiety (10.60,3.80,116) Control: Depression (26.10,7.00,116) Anxiety (10.20,3.20,116) |
2 months | Depression Intervention (15.80,10.60,116) Control (18.30,9.10,115) Anxiety Intervention (7.60,3.80,116) Control (8.30,3.60,115) |
12 months | Depression Intervention (15.70,11.30,116) Control (16.20,10.70,115) Anxiety Intervention (6.80,4.10,116) Control (6.80,4.00,115) |
| Imamura. et al. (2014) & (2015) (two papers 50 & 53) * ^ | CBT | Yes | Yes | Japan, IT employees with no Major Depressive Disorder in last month or treated for mental health problems in last month (n = 762) | 6 week internet-based computerized CBT. 6 lessons, one lesson per week, approx. 30 mins each. Each lesson had homework. Given 10 weeks to complete study in whole (n = 381). | WLC + info (n = 381) | Primary: Depression (BDI-21), Secondary: stress (K6), anxiety (DASS) | Intervention: Stress (5.60,4.60,381) Depression (11.90,8.00,381) Anxiety (88.00,21.50,381) Control: Stress (5.60,4.70,381) Depression (11.80,8.00,381) Anxiety (87.40,20.90,381) |
3 months | Stress Intervention (5.60,4.60,270) Control (5.80,4.70,336) Depression Intervention (10.70,8.60,270) Control (11.70,8.30,336) Anxiety Intervention (87.40,21.70,270) Control (88.50,20.90,336) |
6 months | Stress Intervention (5.70,4.80,272) Control (6.40,5.10,320) Depression Intervention (11.30,9.60,272) Control (12.10,8.70,320) Anxiety Intervention (84.90,23.30,272) Control (87.00,22.80,320) |
| 12 months | Stress Intervention (5.40,4.70,239) Control (5.80,4.70,272) Depression Intervention (11.20,9.40,239) Control (11.60,9.00,272) |
|||||||||||
| Mori. et al. (2014) (51) * ^ | CBT | Yes | No | Japan, IT employees, system engineers with high computer literacy (n = 168) | 4-week intervention with homework. A Web-Based Training Program using CBT. 150 minute group class—participants use web based entries to log daily stresses (n = 85) | WLC (n = 83) | Primary: Psychological distress (K6). | Intervention: Stress (4.70,4.50,85) Control: Stress (4.80,4.50,83) |
1 month | Stress Intervention (4.20,4.90,85) Control (5.00,4.80,83) |
6 months | Stress Intervention (4.60,5.10,85) Control (5.63,5.00,83) |
| Phillips. et al. (2014) (52) * | CBT | Yes | Yes | UK, transport, health and communications sectors who reported issues with difficulty in some tasks at work (n = 637) | 5 week web-based intervention ‘MoodGYM’ five one hour long modules containing CBT skills for preventing and coping with Depression (n = 318) | WLC + info (n = 319) | Primary: Depression (PHQ-9), and (Generalized Anxiety Disorder GAD) | Intervention: Stress (19.90,8.00,318) Depression (14.50,5.40,318) Anxiety (13,50.4.00,318) Control: Stress (20,70.7.00,319) Depression (14.60,5.60,319) Anxiety (13.20,5.00,319) |
6 weeks | Stress Intervention (16.00,9.10,171) Control (16.50,8.60,188) Depression Intervention (9.90,6.10,164) Control (10.20,6.00,176) Anxiety Intervention (9.50,6.00,166) Control (10.20,5.70,181) |
3 months | Stress Intervention (15.00,10.10,102) Control (15.90,8.60,129) Depression Intervention (9.30,6.90,97) Control (10.30,6.90,122) Anxiety Intervention (8.40,6.40,98) Control (10.10,6.50,123) |
| Takechi. et al. (2015) (56) $ | CBT | No, no control group | No | Japan, Manufacturing company, general employees (n = 81) | 10-week single group study, CBT exercise program workbook focusing on dysfunctional thoughts and problem solving, followed by 10 weeks of at home exercises. | nil | Primary: Psychological distress (K6). | Intervention: Stress (4.39,3.70,81) |
10 weeks | Stress Intervention (3.53,2.70,44) |
Nil | not measured |
| Birney. et al. (2016) (61)* | CBT | Yes | Yes | USA, Employees with mild to moderate depressive symptoms (n = 300) | 6 weeks CBT mobile phone app “MoodHacker” (n = 150) | WLC (n = 150) | Primary: Depression (PHQ-9) | Intervention: Depression (13.20,4.30,150) Control: Depression (13.60,3.80,150) |
10 weeks | Depression Intervention (8.80,5.10,130) Control (9.50,5.00,141) |
Nil | not measured |
| Stress Management Interventions | ||||||||||||
| Cook. et al. (2007) (62)* | Stress Mx | Yes | No | USA, human resource employees (n = 419) | Web-based multimedia health promotion program ‘Health Connection’ for the workplace offering guidance on stress management (n = 209) | WLC + info (n = 210) | Primary: Stress | Intervention: Stress (14.21,4.90,209) Control: Stress (15.05,4.60,210) |
3 months | Stress Intervention (13.70,4.90,209) Control (14.30,4.50,210) |
nil | not measured |
| Eisen. et al. (2008) (36)* | Stress Mx | No, face-to-face control group | No | manufacturing company general employees (n = 257) | 2 week online intervention: two sessions online stress management program (n = 123) | completing identical intervention instructor led workshop (n = 134) | Stress: (Occupational Stress inventory, OSI-R) | Intervention: Stress (45.80,14.90,123) Control: Stress (42.90,20.50,134) |
2 weeks | Stress Intervention (38.30,9.30,24) Control (21.70,15.20,75) |
1 month | Stress Intervention (33.30,16.30,15) Control (21.10,14.50,48) |
| Cook. et al. (2015) (34)* | Stress Mx | Yes | No | USA, Employees aged 50–68 years global IT company (n = 278) | ‘HealthyPast50’ is a web-based. Open access for 3 months, 5 modules on stress and mood management, healthy eating, active lifestyle, and smoking (n = 138) | WLC (n = 140) | Primary: Stress (The Ultimate Stress Management, Self-Assessment, and Coping Guide) | Intervention: Stress (3.24,0.50,138) Control: Stress (3.20,0.40,140) |
3 months | Stress Intervention (3.30,0.50,109) Control (3.34,0.50,130) |
nil | not measured |
| Ebert. et al. (2014) (63)* ^ | Stress Mx | Yes | Yes | German, teachers with elevated depressive symptoms currently employed (n = 150) | 6 weeks, 5 lessons, based on problem solving techniques, internet-based problem-solving training (iPST), one lesson per week and practice problem solving skills between each lesson (n = 75) | WLC (n = 75) | Primary: depressive symptoms (CES-D), Secondary: stress (PSQ) | Intervention: Stress (0.66,0.15,75) Depression (22.76,9.20,75) Control: Stress (0.67,0.14,75) Depression (22.80,9.15,75) |
7 weeks | Stress Intervention (0.55,0.20,75) Control (0.62,0.17,75) Depression Intervention (22.81,9.15,75) Control (21.20,8.37,75) |
3 months | Stress Intervention (0.48,0.27,75) Control (0.56,0.25,75) Depression Intervention (15.37,8.40,75) Control (19.87,14.00,75) |
| 6 months | Stress Intervention (0.53,0.20,75) Control (0.60,0.16,75) Depression Intervention (14.53,13.80,75) Control (19.91,10.42,75) |
|||||||||||
| Umanodan. et al. (2014) (64)* | Stress Mx | Yes | No | Japan, general employees in a manufacturing company (n = 266) | 6 week Computer based stress management training (SMT) 6 lessons (one per week)—self paced. 2-phased learning process (n = 142) | WLC (n = 121) | Primary: Stress (BJSQ) | Intervention: Stress (2.00,0.50,142) Control: Stress (2.10,0.56,121) |
9 weeks | Stress Intervention (1.90,0.45,142) Control (2.00,0.55,121) |
19 weeks | Stress Intervention (2.00,0.04,142) Control (2.00,0.55,121) |
| Stansfeld, S., et al. (2015) (65)* ^ | Stress Mx | Yes | No | UK, manager and general employees of the NHS Mental Health Trust (n = 275) | Online health promotion program based around understanding stress through a series of linked topics with case examples. Six fortnightly modules for 3 months (n = 216) | WLC (n = 59) | psychological distress (GHQ-12) | Intervention: Stress (2.80,3.50,216) Control: Stress (3.20,3.40,59) |
3 months | Stress Intervention (2.90,3.50,216) Control (2.90,3.40,59) |
nil | not measured |
| Heber. et al. (2016) (66)* ^ | Stress Mx | Yes | Yes | Germany, mainly recruited by a large health insurance company of highly stressed employees (n = 264) | 7 sessions. 1–2 sessions per week. web-based Internet stress management interventions (iSMI) problem solving, emotion regulation strategies + booster session (n = 132) | WLC (n = 132) | Primary: Stress (PSS). Secondary: Depression (CES-D, HADS) | Intervention: Stress (25.90,3.90,132) Depression (23.34,8.50,132) Anxiety (11.20,3.30,132) Control: Stress (25.15,3.96,132) Depression (23.77,7.60,132) Anxiety (10.70,3.40,132) |
7 weeks | Stress Intervention (17.90,6.17,132) Control (22.90,6.10,132) Depression Intervention (15.60,9.10,132) Control (21.40,8.80,132) Anxiety Intervention (7.80,3.90,132) Control (10.30,3.50,132) |
6 months | Stress Intervention (16.08,6.00,132) Control (22.10,5.80,132) Depression Intervention (13.80,7.70,132) Control (31.50,8.50,132) Anxiety Intervention (6.73,3.40,132) Control (9.65,3.60,132) |
| Mindfulness Based Interventions | ||||||||||||
| Glück. et al. (2011) (67)* | Mindfulness based | Yes | No | Austria, Germany & Switzerland General employees of universities, car dealership, broadcasting station, and health care consulting companies in (n = 50) | web based mindfulness training 13 days two modules each module lasted for 6 days with 20 mins per day (n = 28) | WLC (n = 21) | Primary: Stress (PSQ) | Intervention: Stress (40.06,16.40,28) Control: Stress (35.10,13.40,21) |
2 weeks | Stress Intervention (34.40,15.00,26) Control (34.72,15.35,18) |
3 months | Stress Intervention (27.90,11.20,19) Control group not tested |
| Wolever. et al. (2012) (68)* | Mindfulness based | No, face-to-face control group | Yes | USA, insurance carrier employees with elevated stress levels (n = 96) | 12 week online interventions lasted 1hr per week (n = 52) | In person mindfulness training (n = 44) | Primary: Stress (PSS), Secondary: Depression (CES-D) | Intervention: Stress (24.50,0.50,52) Depression (19.60,1.30,52) Control: Stress (24.85,0.53,44) Depression (20.00,1.40,44) |
3 months | Stress Intervention (14.90,0.80,52) Control (16.94,0.86,44) Depression Intervention (11.10,1.20,52) Control (14.23,1.30,44) |
nil | not measured |
| Ahtinen. et al. (2013) (57)$ | Mindfulness based | No, no control group | No | Finland, general employees from a technology University (n = 15) | 4 week mobile phone app intervention “Oiva” mental wellness training app. With 4 intervention modules to be taken weekly | nil | Primary: Stress (PSS) | Intervention: Stress (3.10,0.20,15) |
1 month | Stress Intervention (2.50,0.10,15) |
nil | not measured |
| Aikens. et al. (2014) (69)* | Mindfulness based | Yes | No | USA, general employees (n = 90) | 7 week web-based online mindfulness training program. 1 hour per week modules (n = 44) | WLC (n = 45) | Primary: Stress (PSS-14) | Intervention: Stress (24.50,6.30,44) Control: Stress (24.80,8.16,45) |
7 weeks | Stress Intervention (18.00,7.00,36) Control (23.30,8.50,42) |
6 months | Stress Intervention (18.80,6.70,31) Control (19.81,7.40,32) |
| Ly. et al. (2014) (70)* | Mindfulness based | Yes | No | Sweden, middle managers or have staff responsibilities in the private sector (n = 73) | 6 week smartphone app mindfulness based. 6 modules one for each week. each module had an audio lecture, text & exercises (n = 36) | WLC (n = 37) | Primary: Stress (PSS-14). | Intervention: Stress (24.30,8.30,36) Control: Stress (24.50,5.90,37) |
6 weeks | Stress Intervention (19.50,7.30,36) Control (23.30,8.00,37) |
nil | not measured |
| Mak. et al. (2015) (58)* | Mindfulness based | Yes | No | China, University staff—general employees (n = 321) | two arm intervention: 8 week online mindfulness training, one lesson per week that took 23–30 (107) | WLC (n = 107) | Primary: Stress (PSS-10), Depression, Anxiety (DASS-21) | Intervention: Stress (1.70,0.60,107) Depression (6.10,6.30,107) Anxiety (6.70,5.20,107) Control: Stress (1.63,0.70,55) Depression (5.47,7.60,55) Anxiety (6.20,8.00,55) |
2 months | Stress Intervention (1.65,0.50,58) Control (1.62,0.70,48) Depression Intervention (5.70,6.80,58) Control (5.60,7.70,48) Anxiety Intervention (6.60,5.40,58) Control (5.70,7.30,48) |
3 months | Stress Intervention (1.70,0.50,44) Control (1.63,0.70,24) Depression Intervention (6.80,7.20,44) Control (5.90,8.12,24) Anxiety Intervention (7.30,6.40,44) Control (5.70,7.60,24) |
| the second group had the identical training plus HAPA (health action process approach) to test enhanced efficacy (n = 107) | Intervention: Stress (1.80,0.60,107) Depression (6.95,7.70,107) Anxiety (7.50,6.60,107) Control: Stress (1.63,0.70,54) Depression (5.47,7.60,54) Anxiety (6.20,8.00,54) |
Stress Intervention (1.70,0.60,58) Control (1.62,0.70,48) Depression Intervention (6.50,7.40,58) Control (5.60,7.70,48) Anxiety Intervention (6.30,6.60,58) Control (5.70,7.30,48) |
Stress Intervention (1.70,0.60,37) Control (1.63,0.70,24) Depression Intervention (6.90,7.70,37) Control (5.90,8.12,24) Anxiety Intervention (6.50,6.60,37) Control (5.70,7.60,24) |
|||||||||
| Allexandre. et al. (2016) (71)* | Mindfulness based | Yes | No | USA, General employees from a corporate call centre (n = 91) | 8 week web-based educational program based on mindfulness meditation. 1 session per week (n = 54) | WLC (n = 37) | Primary: Stress (PSS-10) | Intervention: Stress (25.60,5.40,54) Control: Stress (25.40,5.70,37) |
2 months | Stress Intervention (19.80,7.60,30) Control (24.00,7.20,25) |
4 months | Stress Intervention (19.40,7.70,27) Control (22.50,7.20,20) |
| Cognitive/Assertion Training Interventions | ||||||||||||
| Abbott. et al. (2009) (59)* | Cognitive training | No, cognitive training | No | Australian Industrial organisation general employees (n = 53) | Internet-based program teaching resilience through cognitive training. 7 core modules (n = 26) | WLC (n = 27) | Primary: Depression, Anxiety, Stress: (DASS-21) | Intervention: Stress (10.70,7.40,26) Depression (5.30,5.10,26) Anxiety (2.30,2.20,26) Control: Stress (7.60,6.90,27) Depression (3.78,5.40,27) Anxiety (2.07,2.80,27) |
10 weeks | Stress Intervention (9.70,6.00,26) Control (1.56,2.40,27) Depression Intervention (4.70,4.90,26) Control (3.70,5.30,27) Anxiety Intervention (2.30,2.20,26) Control (6.30,4.90,27) |
nil | not measured |
| Borness. et al. (2013) (60)* | Cognitive training | No, cognitive training | No | Australian Public Sector general employees (n = 135) | 16 week of online Cognitive Training based around, memory, attention, language, executive function, program is called ‘Spark!’ with three 20 minute sessions per week (n = 67) | active control program (n = 68) general knowledge information | Primary: Stress (JSS, Secondary: Depression, Anxiety, DASS-42) | Intervention: Stress (10.70,6.70,67) Depression (6.20,6.20,67) Anxiety (5.40,5.60,67) Control: Stress (11.00,8.80,68) Depression (7.40,6.80,68) Anxiety (6.60,5.80,68) |
4 months | Stress Intervention (10.90,7.90,58) Control (5.80,8.20,62) Depression Intervention (7.30,6.90,58) Control (6.80,7.60,62) Anxiety Intervention (6.20,7.10,58) Control (6.60,11.50,62) |
nil | not measured |
| Yamagishi. et al. (2007) (54)$ | Assertion training | No, poor quality + no control group | No | Japan, shift nurses (n = 25) | web-based assertion training (70 minutes) ‘Internet navigware’: pre, post & follow-up. Training was accessible for 3 weeks (n = 25) | nil | Primary: Stress, Depression–(JSBQ) | Intervention: Stress (2.21,0.73,25) Depression (38.52,9.31,25) |
3 weeks | Stress Intervention (2.11,0.72,25) Depression Intervention (36.84,8.81,25) |
1 months | Stress Intervention (2.01,0.77,25) Depression Intervention (37.44,10.74,25) |
| Yamagishi. et al. (2008) (55)* | Assertion training | No, poor quality | No | Japanese shift working Nurses (n = 60) | 9 weeks sixty minute web-based training was provided weekly (n = 30) | WLC (n = 30) | Primary: Stress, Anxiety, Depression—JSBQ) | Intervention: Stress (2.54,0.67,30) Depression (1.85,0.70,30) Anxiety (2.18,0.80,30) Control: Stress (2.35,0.80,30) Depression (1.89,0.90,30) Anxiety (2.03,0.80,30) |
5 weeks | Stress Intervention (2.58,0.60,30) Control (2.79,0.80,30) Depression Intervention (1.93,0.70,30) Control (2.04,0.80,30) Anxiety Intervention (2.26,0.70,30) Control (2.33,0.80,30) |
9 weeks | Stress Intervention (2.60,0.70,30) Control (2.67,0.70,30) Depression Intervention (1.71,0.50,30) Control (1.78,0.60,30) Anxiety Intervention (2.00,0.69,30) Control (2.10,0.80,30) |
Key:
* Randomised controlled trial,
# Controlled Trial,
$ Pre-intervention post-intervention,
^ Guided,
Questionnaires used: Hospital Anxiety Depression Scale (HADS), Brief Job Stress Questionnaire (BJSQ), Centre of Epidemiologic Studies Depression scale (CES-D), Beck Anxiety Inventory (BAI), Visual Analogue Scale (VAS), Beck’s Depression Inventory (BDI-21), Brief Symptom Inventory (BSI), Kessler 6 (K6), Depression Anxiety Stress Scales DASS, 21 & 42), Patient Health Questionnaire-9 (PHQ-9), Work and Social Adjustment Scale (WSAS), Perceived Stress Scale (PSS, 10 &14), Patient Satisfaction Questionnaire (PSQ), General Health Questionnaire (GHQ-12), Job satisfaction Survey (JSS), Job Stress Burnout (JSBQ)
Meta-analysis results
Overall effect of employee eHealth interventions compared to control conditions
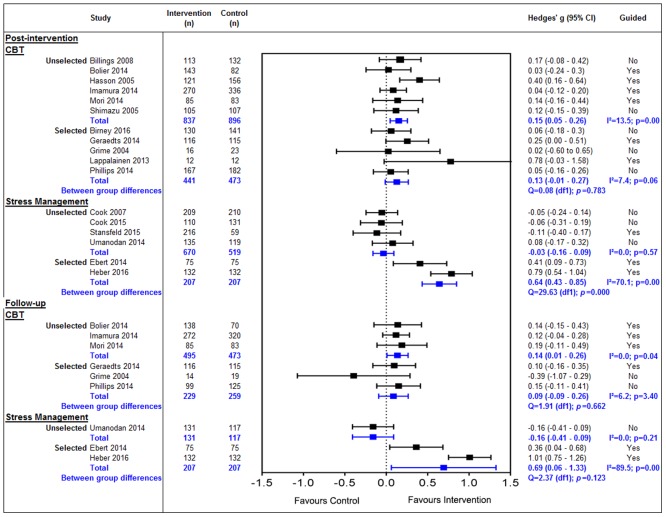
For the 23 trials identified (Fig 2), there was a small, significant positive overall effect post intervention (g = 0.24, 95% CI 0.13 to 0.35, p = <0.00). However, moderate to large heterogeneity was detected (I2 = 67.6%), and there was a significant difference between the effect of intervention types (Q = 9.82 (df2), p = <0.00).
Fig 2. Effect of eHealth interventions in the workplace.
When stratified by intervention type, CBT (n = 11) showed a very small, significant positive effect size and virtually no heterogeneity (g = 0.15, 95% CI 0.02 to 0.29, p = 0.03, I2 = 1.9%). Mindfulness based interventions (n = 6) showed a moderate to large positive effect size and no heterogeneity (g = 0.60, 95% CI 0.34 to 0.85, p = <0.00, I2 = 0.0%). Stress Management interventions (n = 6) had a non-significant small positive effect size with large heterogeneity (g = 0.17, 95% CI -0.01 to 0.34, p = 0.07, I2 = 86.8%).
At follow-up, there was an overall small significant positive effect (g = 0.23, 95% CI 0.03 to 0.42, p = 0.02) and again moderate to large heterogeneity was detected (I2 = 77.7%). When stratified by intervention type, CBT interventions (n = 6) did not maintain the post-intervention effect (g = 0.09, 95% CI -0.18 to 0.36, p = 0.52, I2 = 0.0%). Mindfulness intervention still showed a small positive, but not statistically significant effect (g = 0.32, 95% CI -0.09 to 0.73, p = 0.12, I2 = 0.0%). Stress Management interventions (n = 3) showed a moderate statistically significant positive effect, however large heterogeneity was detected (g = 0.40, 95% CI 0.04 to 0.77, p = 0.03, I2 = 95.1%). There was no significant difference between the intervention types detected (Q = 2.11 (df2), p = 0.35).
Universal vs targeted interventions
There were no differences in the effect of CBT (Fig 3) at post-intervention for unselected (n = 6) (g = 0.15, 95% CI 0.05 to 0.26, p = 0.00, I2 = 13.5%) or selected (n = 5) (g = 0.13, 95% CI -0.01 to 0.27, p = 0.06, I2 = 7.4%). This continued into follow-up for unselected (n = 3) (g = 0.14, 95% CI 0.01 to 0.26, p = 0.04, I2 = 0.0%) and selected (n = 3) (g = 0.09, 95% CI -0.09 to 0.26, p = 3.40, I2 = 6.2%).
Fig 3. Sub-group analysis of the effect of eHealth interventions in the workplace.
However, the effect of Stress Management interventions differed between selected and unselected employees at both post-intervention and follow-up. Interventions delivered to an unselected group (n = 4) showed a very small non-significant negative post-intervention effect (g = -0.03, 95% CI -0.16 to 0.09, p = 0.57, I2 = 0.0%) whereas, interventions given to a selected group showed a moderate to large significant effect reflected in the significant difference between these two groups at post-intervention (Q = 29.63 (df1), p< = 0.01) and high heterogeneity (g = 0.64, 95% CI 0.43 to 0.85, p = 0.00, I2 = 70.1%), we can also see that At follow-up there was only study in an unselected group showing a small non-significant negative effect (g = -0.16, 95% CI -0.41 to 0.09, p = 0.21, I2 = 0.0%). In contrast interventions in selected groups continued to show a significant moderate to large effect size, however large heterogeneity was detected (g = 0.69, 95% CI 0.06 to 1.33, p = 0.00, I2 = 89.5%). All Mindfulness-based interventions were aimed at unselected employees in the studies.
Small study effect
The funnel plots (S2 Fig) of the 23 studies included in the meta-analysis at post-intervention (Panel A in S2 Fig) showed significant asymmetry (Egger’s intercept = 2.53, p = 0.01). After conducting a trim and fill analysis six studies were imputed; there was an adjusted effect size, which was statistically significant (g = 0.12, 95% CI = 0.01 to 0.25) suggesting greater effect in smaller studies (Panel B in S2 Fig). There was no significant asymmetry in the 13 studies at follow-up (Egger’s intercept = 0.32, p = 0.83) (Panel C in S2 Fig). The only sub-group that had more than 10 studies was post-intervention selected CBT (n = 11) (Panel D in S2 Fig), which showed no significant asymmetry (Egger’s intercept = 1.05, p = 0.27)
Overview of efficacy of intervention type and moderators of efficacy across each mental health outcome
A summary of all of the outcomes is visually presented in Table 2, a matrix showing each Hedge’s g effect size for each intervention and each moderator. Overall, there is evidence for the unselected and guided CBT in reducing overall symptoms, which appears to be due to the effects on depression and stress, but not anxiety. The overall effects of unselected and unguided CBT were maintained at follow up, mainly due to the follow up effects of CBT on stress.
Table 2. Overview of efficacy (Hedge’s g) and moderators of each mental health outcome.
| Post-Intervention | Overall | Depression | Anxiety | Stress | Follow-up | Overall | Depression | Anxiety | Stress | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 0.24** (n = 23) | 0.25** (n = 12) | 0.21 (n = 10) | 0.30** (n = 18) | Overall | 0.23* (n = 13) | 0.21 (n = 9) | 0.21 (n = 8) | 0.35** (n = 10) | ||||
| All Interventions | Population | Targeted | 0.31** (n = 7) | 0.31** (n = 7) | 0.33* (n = 4) | 0.42* (n = 3) | All Interventions | Population | Targeted | 0.32* (n = 5) | 0.28 (n = 5) | 0.32 (n = 4) | 0.53* (n = 3) |
| Untargeted | 0.21** (n = 16) | 0.18 (n = 5) | 0.11 (n = 6) | 0.28** (n = 15) | Untargeted | 0.16 (n = 8) | 0.12 (n = 4) | 0.10 (n = 4) | 0.25 (n = 7) | ||||
| Support | Guided | 0.27** (n = 9) | 0.34** (n = 6) | 0.29 (n = 4) | 0.29 * (n = 6) | Support | Guided | 0.32 * (n = 6) | 0.32* (n = 5) | 0.33 (n = 4) | 0.45 * (n = 4) | ||
| Unguided | 0.22 ** (n = 14) | 0.14 (n = 6) | 0.12 (n = 6) | 0.32** (n = 12) | Unguided | 0.11 (n = 7) | 0.00 (n = 4) | 0.03 (n = 4) | 0.26 (n = 6) | ||||
| Risk of bias | High | 0.20** (n = 13) | 0.17 (n = 4) | 0.23 (n = 3) | 0.23* (n = 9) | Risk of bias | High | 0.11 (n = 5) | 0.13 (n = 2) | 0.11 (= 2) | 0.12 (n = 3) | ||
| Low | 0.29** (n = 10) | 0.29** (n = 8) | 0.19 (n = 7) | 0.37** (n = 9) | Low | 0.31* (n = 8) | 0.24 (n = 7) | 0.25 (n = 6) | 0.45** (n = 7) | ||||
| CBT | Population | Targeted | 0.13 (n = 5) | 0.11 (n = 5) | 0.15 (n = 3) | 0.05 (n = 1) | CBT | Population | Targeted | 0.09 (n = 3) | 0.04 (n = 3) | 0.15 (n = 3) | 0.09 (n = 1) |
| Untargeted | 0.15** (n = 6) | 0.12* (n = 3) | 0.06 (n = 3) | 0.19** (n = 5) | Untargeted | 0.14* (n = 3) | 0.13 (n = 2) | 0.10 (n = 2) | 0.15* (n = 2) | ||||
| Support | Guided | 0.18** (n = 6) | 0.16* (n = 4) | 0.10 (n = 3) | 0.18 (n = 3) | Support | Guided | 0.13* (n = 4) | 0.11 (n = 3) | 0.11 (n = 3) | 0.15* (n = 2) | ||
| Unguided | 0.10 (n = 5) | 0.07 (n = 4 | 0.08 (n = 3) | 0.14 (n = 3) | Unguided | 0.08 (n = 2) | 0.07 (n = 2) | 0.13 (n = 2) | 0.09 (n = 1) | ||||
| Risk of bias | High | 0.18** (n = 7) | 0.14 (n = 4) | 0.14 (n = 2) | 0.24** (n = 3) | Risk of bias | High | 0.14 (n = 3) | 0.12 (n = 2) | 0.11 (n = 2) | 0.19 (n = 1) | ||
| Low | 0.10 (n = 4) | 0.10 (n = 4) | 0.08 (n = 4) | 0.10 (n = 3) | Low | 0.11 (n = 3) | 0.09 (n = 5) | 0.12 (n = 3) | 0.13 (n = 2) | ||||
| Mindfulness | Population | Targeted | - | - | - | - | Mindfulness | Population | Targeted | - | - | - | - |
| Untargeted | 0.59** (n = 6) | 0.34* (n = 2) | 0.21 (n = 3) | 0.68** (n = 6) | Untargeted | 0.31* (n = 4) | 0.04 (n = 2) | 0.11 (n = 2) | 0.45** (n = 4) | ||||
| Support | Guided | - | - | - | - | Support | Guided | - | - | - | - | ||
| Unguided | 0.59** (n = 6) | 0.34* (n = 2) | 0.21 (n = 3) | 0.68** (n = 6) | Unguided | 0.31* (n = 4) | 0.04 (n = 2) | 0.11 (n = 2) | 0.45** (n = 4) | ||||
| Risk of bias | High | 0.65** (n = 3) | - | 0.51 (n = 1) | 0.64** (n = 3) | Risk of bias | High | 0.43 (n = 1) | - | - | 0.43 (n = 1) | ||
| Low | 0.54** (n = 3) | 0.34 * (n = 2) | 0.06 (n = 2) | 0.72** (n = 3) | Low | 0.26 (n = 3) | 0.04 (n = 2) | 0.11 (n = 2) | 0.48* (n = 3) | ||||
| Stress Management | Population | Targeted | 0.64** (n = 2) | 0.63** (n = 2) | 0.83** (n = 1) | 0.64** (n = 2) | Stress Management | Population | Targeted | 0.70* (n = 2) | 0.65* (n = 2) | 1.0** (n = 1) | 0.75 (n = 2) |
| Untargeted | -0.03 (n = 4) | - | - | -0.04 (n = 4) | Untargeted | -0.16 (n = 1) | - | - | -0.16 (n = 1) | ||||
| Support | Guided | 0.37* (n = 3) | 0.63** (n = 2) | 0.83** (n = 1) | 0.38 (n = 3) | Support | Guided | 0.70* (n = 2) | 0.65* (n = 2) | 1.0** (n = 1) | 0.75 (n = 2) | ||
| Unguided | -0.01 (n = 3) | - | - | -0.1 (n = 3) | Unguided | -0.16 (n = 1) | - | - | -016 (n = 1) | ||||
| Risk of bias | High | -0.03 (n = 3) | - | - | -0.03 (n = 3) | Risk of bias | High | -0.16 (n = 1) | - | - | -0.16 (n = 1) | ||
| Low | 0.38* (n = 3) | 0.63** (n = 2) | 0.83** (n = 1) | 0.39 (n = 3) | Low | 0.70* (n = 2) | 0.65* (n = 2) | 1.0 ** (n = 1) | 0.75 (n = 2) | ||||
P = <0.05*
P = <0.001**
Mindfulness in unselected and unguided formats had a moderate to large effect size (g = 0.59) in reducing overall symptoms, a small to moderate effect in reducing depression (g = 0.34), and a large effect size (g = 0.68) in reducing stress. Unguided and unselected Mindfulness had a small to moderate effect on overall symptoms at follow up, with a large effect on stress.
Stress Management in selected formats had a large effect size (g = 0.64) and moderate effects when guided (g = 0.37) in reducing overall symptoms, a large effect in reducing depression (g = 0.63), anxiety (g = 0.83) and stress (g = 0.64). These results continued at post-intervention however the effect on Stress Management was no longer significant.
Discussion
This study provides the first comprehensive review of the published evidence for the effectiveness of a range of work-based eHealth interventions addressing the mental health of employees.
Our results were drawn from 32 trials, testing a range of online and mobile applications utilizing Cognitive Behavioural techniques, Stress Management based approaches, and Mindfulness based interventions, 23 studies were suitable for the meta-analysis.
Overall pooled eHealth interventions showed a small significant positive effect at post intervention and follow-up for reducing overall mental health (depression, anxiety and stress) in both universal and selected employees which is similar to a recent review of eHealth interventions for general population [19], providing further evidence for potential use on eHealth interventions as a low cost, alternative to face-to-face interventions for employees [4]. However, this result showed large heterogeneity, which is examined in our sub-group analysis. There is evidence of a small study effect in the overall 23 studies at post-intervention, a possible cause for this is the clinical heterogeneity between the participants in the large and small studies, the smaller studies were targeted at the selected group (n = 1328 participants) so that a favourable outcome of the selected group may be expected compared to the larger amount of participants in the universal studies (n = 2922) [72].
As planned, sub-group analyses were performed on selected and universal interventions. Mindfulness interventions were all universal and unguided interventions, and resulted in a moderately large and statistically significant effect size at post intervention, this result has a potential to make a meaningful change when considered on a population level and is a contrary result to previous findings for interventions delivered to a universal population. Previous research indicates that large effect sizes are unlikely to be found in interventions delivered to general populations who may not be unwell [19, 73]. However, this appeared to be relatively short lived with a halved effect size at follow-up.
There was no difference between universal and targeted CBT interventions, although, previous evidence suggests that selected interventions may be more effective than universal interventions [20,74,75]. Both groups showed very small if any effect at post-intervention or follow-up, indicating that CBT interventions appeared not to have any statistical benefits either universal or targeted working populations which seems to differ from large results seen in both universal [76] and clinical [77], populations. This could be due to recent evidence that shows employed people differ systemically from the general or clinical in terms of symptom profile, function and response [26]. It may also be that the setting, with propensity for perverse incentives, or perceived coercion by employers may not be an effective therapeutic milieu.
In contrast, eHealth Stress Management interventions did appear to have benefits when used in a selected fashion e.g. amongst those reporting increased stress, showing a moderately large effect at post-intervention and a moderate effect size follow-up however, large heterogeneity was detected showing that the two selected studies had a significant difference in what can assume is the sample size as the follow-up length and intervention designs were both very similar. Importantly, when the same type of Stress Management based eHealth interventions were used in unselected (universal) employees, there was no effect compared to wait list controls. Only one study reported a follow up and suggested psychological harm, which may, if replicated, be another example of well-meaning intentions going awry, as some believe to occur with psychological debriefing [78]. It is not clear why a Stress Management intervention would not be effective when used on an unselected population, though it may relate to the dangers of providing non-help seeking populations with too much information, leading them to feel more anxious and vulnerable, as suggested by the authors of these studies[79], or could reflect intra-study effects e.g. differential drop out.
The outcome measures were then analysed separately by means of mental health condition.
We can see evidence for workplace eHealth interventions that are targeted and guided with low risk of bias reducing depression overall at post-intervention. There is no evidence to suggest that any eHealth intervention in the workplace have any effect on reducing anxiety level or symptoms at either post-intervention or follow-up. For stress levels it is evident that Stress Management interventions are most effective at post-intervention. It is evident that where a high risk of bias is found: in overall interventions, CBT and Mindfulness are all due to stress outcomes, it is unclear why, but this may be due to the different self-reporting measures used to report stress.
Strengths and limitations
The main strengths of this review are the detailed systematic search strategy, the clearly defined inclusion and exclusion criteria and the assessment of the quality of the studies. There are a number of potential limitations, first, despite widespread use, the number of studies examining eHealth interventions in the workplace was surprisingly small with only 23 studies able to be included in the meta-analysis and for some of the subgroups there were too few to draw strong conclusions. Second, although some of the studies had clearly defined the intervention type, e.g. reporting only using CBT approaches, other interventions prioritised one approach in a more eclectic intervention, e.g. using “Mindfulness with aspects of Stress Management”, and we had to group these studies into that dominant intervention basis. However the high heterogeneity of differences of true effects when all these eHealth interventions were combined was reduced substantially when analysed by intervention type, sometimes to zero, supporting this grouping. Where a study had several outcome measures, we decided to pool them into one ‘overall mental health’ combined category, however Table 2 shows the outcome specific moderators and each level of efficacy in the intervention groups and overall. As self-reported measures were used in all studies, our conclusions are limited to self-reported reduction of symptoms rather than a clinical diagnosis. Finally, initial screening of some titles for exclusion was only completed by one author.
Conclusion
This review demonstrated the evidence that certain types of eHealth interventions delivered to employees via their workplace can be effective at reducing mental health and stress symptoms although the evidence base is affected by a small study effect that seems to inflate effectiveness. If an eHealth intervention is to be offered to all employees, in a universal fashion, then Mindfulness approaches appear to have a stronger effect than the other types. There is little to recommend Stress Management approaches delivered to the whole workforce, and one study suggests that providing this type of intervention may even be harmful. In contrast the use of Stress Management eHealth interventions by workers who are reporting high levels of stress may have a positive effect, despite few studies. Thus although eHealth interventions are now popular and widely promoted in workplaces it appears that some caution is required in their advocacy and uptake and more evidence is needed on the effectiveness, targeting, implementation and potential risks of these new technologies.
Several considerations for future research and practice for delivering eHealth interventions to employees are evident. First, it is important to consider what the intended populations needs from the interventions to ensure the greatest potential for benefit, for example, the diverse mental health status of the employees should be considered, and where possible interventions should be offered that best fit a range of symptoms which may entail more than one application. Second, it is important to select interventions on the basis of available evidence, as some intervention types may have little or no effect on the intended outcome or may even be potentially harmful. Third, it is important for organisations that are providing interventions to their employees consider both the effectiveness of the interventions and design features to ensure that they can be applied to both universal and selected groups of people, and to be aware that not all employees would benefit from the same type of intervention. Fourth, more research is needed in the form of randomised controlled trials to understand which type of interventions would best benefit different types of employees and mental health conditions, especially Mindfulness interventions that are guided and targeting symptomatic employees, as there is no current evidence for this group.
Supporting information
(PDF)
(TIF)
(TIF)
(PDF)
(XLSX)
Acknowledgments
ES, IC, SH & NG are supported in partnership with beyondblue with donations from the Movember Foundation. AL is supported by NHMRC-ARC Dementia Research Development Fellowship. RAC is funded by an Australian Research Council Future Fellowship.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
ES, IC, SH & NG are supported in partnership with beyondblue with donations from the Movember Foundation. AL is supported by NHMRC-ARC Dementia Research Development Fellowship. RAC is funded by an Australian Research Council Future Fellowship.
References
- 1.PricewaterhouseCoopers. (2014) Creating a mentally healthy workplace Return on investment analysis. Final Report. Retrieved from https://www.headsup.org.au/docs/default-source/resources/beyondblue_workplaceroi_finalreport_may-2014.pdf
- 2.Glozier N. Mental ill health and fitness for work. Occup Environ Med 2002; 59:714–20. doi: 10.1136/oem.59.10.714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvey SB, Henderson M, Lelliott P, Hotopf M. Mental health and employment: much work still to be done. Br J Psychiatry, 2009; 194(3):201–203 doi: 10.1192/bjp.bp.108.055111 [DOI] [PubMed] [Google Scholar]
- 4.Stewart W, Ricci J, Chee E, & Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American productivity audit. Journal of Occupational & Environmental Medicine, 2003; 45(12), 1234–1246. [DOI] [PubMed] [Google Scholar]
- 5.Black C. Working for a healthier tomorrow Dame Carol Black’s Review of the health of Britain’s working age population. Department of Work and Pensions; 2008. [Google Scholar]
- 6.Harvey S, Modini M, & Joyce S, Milligan-Saville JS, Tan L, Mykletun A. et al. Can work make you mentally ill? A systematic meta-review of work related risk factors for common mental health problems. Occup Environ Med 2017;74(4):301–310 doi: 10.1136/oemed-2016-104015 [DOI] [PubMed] [Google Scholar]
- 7.Knudsen A, Harvey S, Mykletun A, and Overland S Common mental disorders and long-term sickness absence in a general working population. The Hordaland Health Study. Acta Psychiatr Scand 2013;127:287–97. doi: 10.1111/j.1600-0447.2012.01902.x [DOI] [PubMed] [Google Scholar]
- 8.Knudsen A, Overland S, Aakvaag HF, Harvey SB, Hotopf M and Mykletun A. Common mental disorders and disability pension award: seven year follow-up of the HUSK study. J Psychosom Res 2010;69:59–67 doi: 10.1016/j.jpsychores.2010.03.007 [DOI] [PubMed] [Google Scholar]
- 9.Harvey Samuel B, Deady Mark, Wang Min-Jung, Mykletun Arnstein, Butterworth Peter, Christensen Helen and Mitchell Philip B. Is the prevalence of mental illness increasing in Australia? Evidence from national health surveys and administrative data, 2001–2014. Med J Aust 2017; 206 (11): 490–493 [DOI] [PubMed] [Google Scholar]
- 10.Harvey S, Modini M, Christensen H, & Glozier N. Severe mental illness and work: What can we do to maximise the employment opportunities for individuals with psychosis? Australian & New Zealand Journal of Psychiatry (2013);47: (5):421–4. [DOI] [PubMed] [Google Scholar]
- 11.Tan L, Wang M.-J, Modini M, Joyce S, Mykletun A, Christensen H. et al. Preventing the development of depression at work: A systematic review and meta-analysis of universal interventions in the workplace. MBC Medicine, 2014; 12, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence: Workplace health promotion: how to encourage employees to be physically active NICE Public Health Guidance 13. 2008, London, UK: National Institute for Health and Clinical Excellence. [Google Scholar]
- 13.Brunton G, Dickson K, Khatwa M, Caird J, Oliver S, Hinds K.et al. , (2016) Developing evidence informed, employer-led workplace health. London: EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London. [Google Scholar]
- 14.Henderson M, Harvey S, Overland S, Mykletun A, & Hotopf M: Work and common psychiatric disorders. J R Soc Med. 2011, 104: 198–207. doi: 10.1258/jrsm.2011.100231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mathers CD, Loncar D: Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joyce S, Modini M, Christensen H, Mykletun A, Bryant R, Mitchell PB. et al. Workplace interventions for common mental disorders: a systematic meta-review, Psychological Medicine, 2016;46(4), 683–697 doi: 10.1017/S0033291715002408 [DOI] [PubMed] [Google Scholar]
- 17.Harrison V, Proudfoot J, Wee P, Parker G, Pavlovic DH, Manicavasagar V. Mobile mental health: review of the emerging field and proof of concept study. J Ment Health 2011; 20:509–524. doi: 10.3109/09638237.2011.608746 [DOI] [PubMed] [Google Scholar]
- 18.Andersson G, Hesser H, Veilord A, Svedling L, Andersson F, Sleman O. et al. Randomised controlled non-inferiority trial with 3-year follow-up of Internet-delivered versus face-to-face group cognitive behavioural therapy for depression. Journal of Affective Disorders, 2013; 151(3), 986–994. doi: 10.1016/j.jad.2013.08.022 [DOI] [PubMed] [Google Scholar]
- 19.Deady M, Choi I, Calvo R, Glozier N, Christensen H, & Harvey S. ‘eHealth interventions for the prevention of depression and anxiety in the general population: A systematic review and meta-analysis’. BMC Psychiatry, 2017;17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richards D, & Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin. Psychol. Rev, 2012; (32) 329–342 [DOI] [PubMed] [Google Scholar]
- 21.Andrews G, Cuijpers P, Craske M, McEvoy P, Titov N. Computer Therapy for the Anxiety and Depressive Disorders Is Effective, Acceptable and Practical Health Care: A Meta-Analysis. PLoS ONE 5, 2010. (10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.So M, Yamaguchi S, Hashimoto S, Sado M, Furukawa T & McCrone P, Is computerised CBT really helpful for adult depression?-A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry 2013, 13:113 doi: 10.1186/1471-244X-13-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilbody S, Littlewood E, Hewitt C, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial, BMJ, 2015;351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrews G, Cuijpers P, Carlbring P, Riper H, Hedman E, Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry 2014;13:288–295 doi: 10.1002/wps.20151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spijkerman M, Pots W, Bohlmeijer E. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology 2016;102:(45) 114. [DOI] [PubMed] [Google Scholar]
- 26.McIntyre RS, Florea I, Tonnoir B, Loft H, Lam RW, Christensen MC. Efficacy of Vortioxetine on Cognitive Functioning in Workinf Patients with Major Depressive Disorder. Journal Clinical Psychiatry, 2017;78:115–121 [DOI] [PubMed] [Google Scholar]
- 27.Flanagan P, & Ots J. EAP counselling: Outcomes, impact & return on investment 2011.
- 28.Dunning M, (2014 Jan 5). Employee assistance programs underutilized by employees. Retrieved from http://www.businessinsurance.com/article/20140105/NEWS03/301059979
- 29.Birgit W, Horn A, Maercker A. Internet-based versus face-to-face cognitive-behavioral intervention for depression: A randomized controlled non-inferiority trial. Journal of Affective Disorders, 2013. [DOI] [PubMed] [Google Scholar]
- 30.Ahthes E, Mobile mental-health apps have exploded onto the market, but few have been thoroughly tested. Pocket Psychiatry, Nature, 2016;532(7) [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097 doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grime P, Computerized cognitive behavioural therapy at work: a randomised controlled trial in employees with recent stress-related absenteeism. Occupational Medicine 2004;54:353–359 doi: 10.1093/occmed/kqh077 [DOI] [PubMed] [Google Scholar]
- 33.Billings D, Royer F, Hendrickson A, Dove D, A web-based approach to managing stress and mood disorders in the workforce. Journal of Occupational and Environmental Medicine, 2008;50(8): 960–968. doi: 10.1097/JOM.0b013e31816c435b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook R, Hersch R, Schlossberg D, Leaf S. A Web-based health promotion program for older workers: Randomized controlled trial. Journal of medical Internet research, 2015. 17(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hasson D, Anderberg U, Töres T, Arnetz B Psychophysiological effects of a web-based stress management system: A prospective, randomized controlled intervention study of IT and media workers. BMC Public Health. 2005; 5: 78 doi: 10.1186/1471-2458-5-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eisen K, Allen G, Bollash M, Pescatello L. Stress management in the workplace: A comparison of a computer-based and in-person stress management intervention. Computers in Human Behavior. 2008. 24(2): 486–496 [Google Scholar]
- 37.Andersson G, Cuijpers P, Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cognitive Behaviour Therapy 2009; 38:4. [DOI] [PubMed] [Google Scholar]
- 38.Downs SH, Black N: The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998, 52: 377–384. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Samoocha D, Bruinvels D, Elbers N, Anema J, van der Beek A: Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010, 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higins J, Green S, editors Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. [Google Scholar]
- 41.Cohen J, Statistical Power Analysis for Behavioural Sciences, Hillsdale, NJ: Lawrence Erlbaum Associates; 1988(2). [Google Scholar]
- 42.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. Oxford, United Kingdom: The Cochrane Collaboration; 2009. [Google Scholar]
- 43.Rothstein H, Sutton A, Borenstein M. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. Chichester, United Kingdom: John Wiley & Sons Ltd, 2005. [Google Scholar]
- 44.Duval S, Tweedie R: Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in met-analysis. Biometrics, 2000:56:455–463. [DOI] [PubMed] [Google Scholar]
- 45.Shimazu A, Irimajiri H, Sakamoto M, Amano S, Effects of web-based psychoeducation on self-efficacy, problem solving behavior, stress responses and job satisfaction among workers: a controlled clinical trial. Journal of Occupational Health, 2005;47(5): 405–13. [DOI] [PubMed] [Google Scholar]
- 46.Lappalainen P, Kaipainen K, Lappalainen K, Hoffrén R, Myllymaki T, Linnunen ML. et al. Feasibility of a personal health technology-based psychological intervention for men with stress and mood problems: randomized controlled pilot trial. JMIR Research Protocols, 2013; 2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boiler L, Ketelaar S, Nieuwenhuijsen K, Smeets O, Gartner F, Sluiter J. Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: A cluster-randomized controlled trial. Internet Interventions 1, 2014;196–204 [Google Scholar]
- 48.Geraedts A, Kleiboer AM, Twisk J, Wiezer NM, van Mechelen W, Cuijpers P.Long-term results of a web-based guided self-help intervention for employees with depressive symptoms: randomized controlled trial. Journal of medical Internet research, 2014;16(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geraedts A, Wiezer N, van Mechelen W, Cuijpers P, Short-term effects of a web-based guided self-help intervention for employees with depressive symptoms: randomized controlled trial. Journal of medical Internet research, 2014;16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Imamura K, Kawakami N, Furukawa T, Matsuyama Y, Shimazu A, Umanodan R. et al. Effects of an Internet-based cognitive behavioral therapy (iCBT) program in Manga format on improving subthreshold depressive symptoms among healthy workers: a randomized controlled trial. PLoS ONE, 2014;9(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mori M, Taajima M, Kimura R, Sasaki N, Somemura H, Ito Y. et al. A Web-Based Training Program Using Cognitive Behavioral Therapy to Alleviate Psychological Distress Among Employees: Randomized Controlled Pilot Trial. JMIR research protocols, 2014. 3(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Phillips R, Schneider J, Molosankwe I, Leese M, Foroushani PS, Grime P. et al. Randomized controlled trial of computerized cognitive behavioural therapy for depressive symptoms: effectiveness and costs of a workplace intervention. Psychological Medicine, 2014;44(4): 741–52. doi: 10.1017/S0033291713001323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Imamura K, Kawakami N, Furukawa T, Matsuyama Y, Shimazu A, Umanodan R. et al. Does Internet-based cognitive behavioral therapy (iCBT) prevent major depressive episode for workers? A 12-month follow-up of a randomized controlled trial. Psychological medicine, 2015;45(09): 1907–1917. [DOI] [PubMed] [Google Scholar]
- 54.Yamagishi M, Kobayashi T, Nagami M, Shimazu A, Kageyama T. Effect of web-based assertion training for stress management of Japanese nurses. Journal of Nursing Management, 2007. 15(6): 603–607. doi: 10.1111/j.1365-2834.2007.00739.x [DOI] [PubMed] [Google Scholar]
- 55.Yamagishi M, Nakamura Y, Effects of web-based career identity training for stress management among Japanese nurses: a randomized control trial. Journal of Occupational Health, 2008. 50(2): 191–193. [DOI] [PubMed] [Google Scholar]
- 56.Takechi S, Kikuchi T, Horisawa S, Nakagawa A, Yoshimura, Mimura M. Effectiveness of a Cognitive Behavioral Therapy-Based Exercise Program for Healthy Employees. Advances in Physical Education, 2015;5(4): 263 [Google Scholar]
- 57.Ahtinen A, Mattila E, Valkkynen P, Kaipainen K, Vanhala T, Ermes M. et al. Mobile mental wellness training for stress management: Feasibility and design implications based on a one-month field study. JMIR Mhealth Uhelath, 2013; 1(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mak W, Chan A, Cheung E, Lin C, Ngai K, Enhancing Web-based mindfulness training for mental health promotion with the health action process approach: Randomised controlled trial. Journal of Medical Internet Research, 2015; 17(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abbott J-A, Klein B, Hamilton C, Rosenthal A. The impact of online resilience training for sales managers on wellbeing and performance. Sensoria: A Journal of Mind, Brain & Culture, 2009. 5(1): 89–95. [Google Scholar]
- 60.Borness C, Crawford J, Valenzuela M. Putting brain training to the test in the workplace: a randomized, blinded, multisite, active-controlled trial. PLoS ONE [Electronic Resource], 2013. 8(3): p. e59982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Birney A, Gunn R, Russell J, Ary D. MoodHacker mobile wen app with email for adults to self-manage mild-to-moderate depression: Randomized controlled trial. JMIR Mhealth Uhelath, 2016;4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cook R, Hersch R, Back A, Hendrickson A. A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. Journal of Medical Internet Research, 2007. 9(2): e17 doi: 10.2196/jmir.9.2.e17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ebert D, Lehr D, Boss L, Riper H, Cuijpers P, Andersson G. et al. Efficacy of an internet-based problem-solving training for teachers: Results of a randomized controlled trial. Scandinavian Journal of Work, Environment & Health, 2014. 40(6): 582–596 [DOI] [PubMed] [Google Scholar]
- 64.Umanodan R, Minami M, Kawakami N. Effects of computer-based stress management training on psychological well-being and work performance in japanese employees: a cluster randomized controlled trial. Industrial Health, 2014. 52(6): 480–91. doi: 10.2486/indhealth.2013-0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stansfeld S, Kerry S, Chamdola T. Russell J, Berney L, Hounsome N. et al. Pilot study of a cluster randomised trial of guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: GEM study. BMJ Open 2015;5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Heber E, Lehr D, Ebert D, Berking M, Riper H. Web-Based and Mobile Stress Management Intervention for Employees: A Randomized Controlled Trial. Journal of medical Internet research, 2016. 18(1): 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Glück T, Maercker A, A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry 2011; 11:175 doi: 10.1186/1471-244X-11-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA. et al. Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. Journal of occupational health psychology, 2012. 17(2): 246–258. doi: 10.1037/a0027278 [DOI] [PubMed] [Google Scholar]
- 69.Aikens K, Astin J, Pelletier K, Levanovich K, Baase CM, Park YY. et al. Mindfulness goes to work. JOEM, 2014;56(7). [DOI] [PubMed] [Google Scholar]
- 70.Ly K, Asplund K, Andersson G. Stress management for middle managers via an acceptance and commitment-based smartphone application: a randomized controlled trial. Internet Interventions, 2014. 1(3): 95–101. [Google Scholar]
- 71.Allexandre D, Bernstein A, Walker E, Hunter J, Roizen MF, and Morledge TJ. A web-based mindfulness stress management program in a corporate call center. A randomized clinical trial to evaluate the added benefit of onsite group. JOEM, 2016; 58(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwarzer G, Carpenter J, Rücker G. (2015) Small-Study Effects in Meta-Analysis In: Meta-Analysis with R. Use R!. Springer, Cham [Google Scholar]
- 73.Rose G. The strategy of prevention medicine. Oxford: Oxford University Press; 1994. [Google Scholar]
- 74.Schröder J, Berger T, Westermann S, Klein JP, Moritz S. Internet interventions for depression: new developments. Dialogues in Clinical Neuroscience. 2016;18(2):203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, McLoone J. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol. 2006;74(1):66:66 doi: 10.1037/0022-006X.74.1.66 [DOI] [PubMed] [Google Scholar]
- 76.Spek V, Cuijpers P, Nyklicek I, Smits N, Riper H, Keyzer J. et al. One-year follow-up results of a randomized controlled clinical trial on internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years. Psychol Med. 2008;38(5):635–9 doi: 10.1017/S0033291707002590 [DOI] [PubMed] [Google Scholar]
- 77.Andrews G, Cuijpers P, Craske M, McEvoy P, & Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS ONE, 2010;5 (10), [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wessely S & Deahl M. Psychological debriefing is a waste of time (in debate). Br J Psychiatry; 2003. 183:12–14. [DOI] [PubMed] [Google Scholar]
- 79.Wessely S, Bryant RA, Greenberg N, Earnshaw M, Sharpley J, Hughes JH. et al. Does psychoeducation help prevent Post Traumatic Psychological Distress? Psychiatry: Interpersonal and Biological Processes 2008; 71, 4, 287–302 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(TIF)
(TIF)
(PDF)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.