Abstract
BACKGROUND
Hispanics are more likely than other racial/ethnic groups in the United States to be diagnosed with later stage of prostate cancer, yet they have lower prostate cancer mortality rates. The authors evaluated the impact of nativity and neighborhood-level Hispanic ethnic enclave on prostate cancer survival among Hispanics.
METHODS
A total of 35,427 Hispanic men diagnosed with invasive prostate cancer from 1995 through 2008 in the California Cancer Registry were studied; vital status data were available through 2010. Block group-level neighborhood measures were developed from US Census data. Stage-stratified Cox proportional hazards models were used to assess the effect of nativity and ethnic enclave on prostate cancer survival.
RESULTS
In models adjusted for neighborhood socioeconomic status and other individual factors, foreign-born Hispanics were found to have a significantly lower risk of prostate cancer survival (hazards ratio [HR], 0.81; 95% confidence interval [95% CI], 0.75–0.87). Living in an ethnic enclave appeared to modify this effect, with the survival advantage slightly more pronounced in the high ethnic enclave neighborhoods (HR, 0.78; 95% CI, 0.71–0.86) compared with low ethnic enclave neighborhoods (HR, 0.86; 95% CI, 0.76–0.98).
CONCLUSIONS
Despite lower socioeconomic status, Hispanic immigrants have better survival after prostate cancer than US-born Hispanics and this pattern was more striking among those living in ethnic enclaves. Identifying the modifiable individual and neighborhood-level factors that facilitate this survival advantage in Hispanic immigrants may help to inform specific interventions to improve survival among all patients.
Keywords: prostate neoplasm, Hispanic or Latino, socioeconomic status, Surveillance, Epidemiology, End Results (SEER), survival
INTRODUCTION
Of all major races and ethnicities, Hispanics are the most rapidly growing group in the United States, particularly in California, where the 14 million residents who are of Hispanic origin comprise more than one-third of the total California population.1,2 Hispanics are composed of a diverse population from many countries; however in California, the majority of foreign-born Hispanics immigrated from Mexico.3 Prostate cancer is the most commonly diagnosed cancer and accounts for > 25% of all new cancer cases among US Hispanic males.4,5
Compared with non-Hispanic (NH) white men, Hispanic men diagnosed with prostate cancer present with more advanced stage of disease, higher tumor grade, and elevated prostate-specific antigen levels,5–7 yet they experience lower prostate cancer-specific death rates,4,8–10 although this finding has not been consistently observed.11 Foreign-born Hispanics living in the United States experience a lower risk of death from prostate cancer than both NH whites and US-born Hispanics.9,12 Survival differences among Hispanic men do not appear to be entirely explained by treatment differences between NH white and Hispanic men,13,14 but may relate to lifestyle factors and degree of acculturation after migration to the United States.15,16 A spatial-temporal study performed in Texas found that Hispanics who resided in specific counties experienced an excess of prostate cancer mortality compared with those residing other counties, indicating that county-level or neighborhood-level clustering of sociodemographic factors may be associated with prostate cancer outcomes.8
The “Hispanic paradox” refers to the persistent pattern of Hispanic Americans having health outcomes that are paradoxically comparable to, or better than, their NH white counterparts although Hispanics have lower average socioeconomic status (SES). It has been postulated that this paradox reflects a survival advantage among foreign-born Hispanics, who in the United States predominantly reside in ethnic enclave communities (neighborhoods with higher concentrations of a particular ethnic group with ethnic-specific sociocultural mores) and who may experience culture-related health protective effects for a variety of disease outcomes. To the best of our knowledge, the current study is the first to investigate prostate cancer survival among Hispanics by nativity and ethnic enclave. Teasing apart the independent and joint effects of nativity, SES, and residence in ethnic enclaves may help us to better understand the apparent paradox in the improved survival, compared with NH white men, among Hispanic men diagnosed with prostate cancer, despite their having more advanced disease at the time of diagnosis.9,16,17
We examined prostate cancer survival among US-born and foreign-born Hispanics in the population-based California Cancer Registry (CCR) from 1995 to 2008. To our knowledge such an analysis has not been previously conducted in part due to missing data regarding birthplace for a sizable percentage (approximately 25%) of Hispanic cancer cases in CCR data.18,19 Therefore, through statistical imputation of nativity for cancer cases with missing birthplace and in combination with small-area (block group)–level data on neighborhood SES and ethnic enclave, we estimated prostate cancer survival among Hispanic men residing in California.
MATERIALS AND METHODS
Study Population
California law mandates that cancer cases be reported to the population-based CCR, which is a participant in the National Cancer Institute’s Surveillance, Epidemiology, and End Results program and thus requires the highest level of data quality and accuracy, and is estimated to include > 99% of all invasive cancers diagnosed in the state of California. The CCR routinely collects patient data from medical records on personal characteristics at time of diagnosis (age, sex, race, ethnicity, and residence) as well as tumor characteristics (extent of disease, tumor characteristics, and first course of treatment). Through routine linkages with state and national databases, the CCR obtains and updates vital status and cause of death. Hispanic ethnicity was collected from medical records from inference based on additional information such as race and ethnicity of parents, maiden name, surname, and birthplace, or from death records.19,20 The North American Association of Central Cancer Registries’ Hispanic Identification Algorithm was used to improve the classification of Hispanic ethnicity.21
We identified 36,897 California residents of Hispanic ethnicity, regardless of race, newly diagnosed with first primary invasive prostate cancer (International Classification of Disease for Oncology, 3rd edition [ICD-O-3]22 site code C619) during the period from January 1, 1995 through December 31, 2008. We limited the study to those individuals with adenocarcinoma (ICD-O-3 morphology codes 8010 and 8140–8570). For each prostate cancer case, we obtained registry information routinely abstracted from the medical record such as age at diagnosis, stage at diagnosis (summarized as local/regional, advanced, or unknown), histological grade, and other clinical variables. In addition, address of residence at time of diagnosis was collected and geocoded by the CCR and used to assign each individual to a census block group.
We excluded subjects with missing or invalid survival time (n = 569) and those subjects whose address could not be accurately geocoded to a census block group (n = 901). The final population study size for analysis included 35,427 Hispanic men.
Variables
Nativity classification
Data regarding birthplace were available through the CCR for 60.2% of the identified cases. Statistical imputation using the subject’s Social Security number (SSN), which is indicative of the state and year of issuance, was used to estimate nativity for the 36.9% of cases with a known, valid SSN but unknown birthplace. Subjects who received their SSN before 20 years of age were considered US-born whereas those who received an SSN when they were aged ≥ 20 years were considered foreign-born. This age cutpoint was derived from a previous study of patients with cancer, comparing self-reported nativity with the registry data and by maximizing the predictive value and minimizing the misclassification based on receiver operating characteristic curves.23–25 The 2.9% of subjects with missing or invalid SSNs were assigned a nativity based on the age and nativity distribution of the overall sample.
Neighborhood ethnic enclave status
Neighborhood ethnic enclave was measured using a previously described index that used principal components analysis from the following 2000 Census block group variables: percentage linguistically isolated, percentage linguistically isolated who speak Spanish, percentage speaking limited English, percentage Spanish-speaking who spoke limited English, percentage of recent immigrants, percentage Hispanic, and percentage foreign-born.26 Each cancer case was assigned to a neighborhood ethnic enclave quintile based on the distribution across all census block groups in California. We dichotomized ethnic enclave into lower ethnic enclave (quintiles 1, 2, and 3) and higher ethnic enclave (quintiles 4 and 5) for statistical analysis.
Neighborhood SES
Neighborhood SES was measured using a previously described index that incorporates 2000 Census data regarding education, occupation, unemployment, household income, and poverty.27 Each cancer case was then assigned to a neighborhood SES quintile based on the distribution of SES across all census block groups in California. We dichotomized SES into lower SES (quintiles 1, 2, and 3) and higher SES (quintiles 4 and 5) for statistical analysis. Individual-level information regarding SES is not collected by the CCR.
Follow-up
Survival time, in months, was calculated from date of diagnosis to whichever of the following occurred first: 1) date of death due to prostate cancer; 2) date of last known contact; or 3) December 31, 2010 (the end of the study period). Subjects who were missing the month or day of the month for either diagnosis or follow-up were given the imputed month of July and the 15th day of the month, respectively (1.7% with missing month and 9.5%for whom the day of the month was missing). Deaths due to prostate cancer were identified from the underlying cause of death on the death certificate, according to the 9th28 or 10th29 revisions of the ICD codes (ICD-9 code 1859, ICD-10 code C61.9). Of the 25,653 individuals still alive at the end of the study period, 98.4% of US-born men had complete follow-up within the last 3 years (97% in the last year), whereas foreign-born men had slightly worse follow-up (96% within the past 3 years, 93% within the past year).
Statistical Analysis
We used Cox proportional hazards models stratified by stage of disease (local/regional, advanced, unknown) and adjusted for age to assess the effect of nativity on prostate cancer-specific survival. Stratified Cox models allow the baseline hazard to vary within the different stage strata while assuming that the general relationship between survival and nativity remains the same, yielding 1 set of parameter estimates from a global model. The hazards ratio (HR) and 95% confidence intervals (95% CI) were estimated comparing foreign-born with US-born individuals. Because we were interested in examining the effect of neighborhood ethnic enclave on the relationship between survival and nativity, after testing the 2-way interaction, we computed models within the 2 levels of ethnic enclave. We then adjusted these models for year of diagnosis, marital status, histological grade, surgery, radiotherapy, hormone therapy, and neighborhood SES.
We found minimal spatial clustering of prostate cancer cases at the block group level; 65% of block groups had only 1 or 2 cases, 92% had ≤ 5 cases, and 99% had ≤ 10 cases. The proportional hazards assumption was assessed by analysis of the scaled Schoenfeld residuals and no significant violations were observed.
RESULTS
Sociodemographic and clinical characteristics of the cases are shown in Table 1 by nativity and stratified by neighborhood ethnic enclave. The case population had a higher percentage of foreign-born (56%) individuals who were slightly older at the time of diagnosis compared with US-born individuals, especially within low ethnic enclaves. Foreign-born Hispanics were more likely to be diagnosed with disease of both advanced stage and advanced grade. Foreign-born Hispanics were more likely to undergo surgery or hormone therapy and less likely to receive radiotherapy. Foreign-born Hispanics were more likely to live in high ethnic enclave neighborhoods (72.2% vs 49.9% of US-born) and less likely to live in higher SES neighborhoods (21.1% vs 33.2% of US-born).
TABLE 1.
Demographic and Clinical Characteristics of Hispanic Men With Prostate Cancer Unstratified and Stratified by Ethnic Enclave: California, 1995 to 2008a
| Unstratified | High Ethnic Enclave | Low Ethnic Enclave | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Variable | US-Born (n = 15,530) % |
Foreign-Born (n = 19,897) % |
US-Born (n = 7748) % |
Foreign-Born (n = 14,360) % |
US-Born (n = 7782) % |
Foreign-Born (n = 5537) % |
| Age at diagnosis, y | ||||||
| <60 | 22.1 | 19.2 | 19.2 | 18.9 | 25.0 | 20.0 |
| 60–69 | 37.6 | 37.9 | 37.6 | 38.0 | 37.5 | 37.7 |
| ≥70 | 40.3 | 42.9 | 43.2 | 43.1 | 37.5 | 42.3 |
| Marital status at diagnosis | ||||||
| Married | 69.5 | 71.2 | 66.1 | 70.2 | 72.8 | 73.8 |
| Never married | 9.0 | 8.1 | 10.1 | 8.7 | 7.9 | 6.4 |
| Previously married | 13.8 | 11.5 | 15.0 | 11.7 | 12.6 | 10.9 |
| Unknown | 7.7 | 9.2 | 8.8 | 9.4 | 6.7 | 8.9 |
| Stage | ||||||
| Localized | 80.0 | 76.8 | 78.6 | 76.0 | 81.3 | 79.0 |
| Regional | 10.7 | 11.7 | 10.4 | 11.7 | 11.1 | 11.6 |
| Advanced | 5.3 | 5.9 | 6.2 | 6.3 | 4.4 | 4.9 |
| Unknown | 4.0 | 5.6 | 4.8 | 6.0 | 3.2 | 4.5 |
| Tumor grade | ||||||
| I | 4.3 | 4.6 | 4.7 | 5.0 | 3.8 | 3.7 |
| II | 58.7 | 56.6 | 58.4 | 56.4 | 59.0 | 57.2 |
| III | 32.5 | 33.7 | 31.9 | 33.7 | 33.1 | 33.7 |
| IV | 0.2 | 0.4 | 0.3 | 0.4 | 0.2 | 0.3 |
| Unknown | 4.3 | 4.7 | 4.7 | 4.5 | 3.9 | 5.1 |
| Surgery | ||||||
| Yes | 42.0 | 42.8 | 40.8 | 43.5 | 43.1 | 41.1 |
| No | 57.9 | 57.0 | 59.1 | 56.4 | 46.7 | 58.6 |
| Unknown | 0.1 | 0.2 | 0.1 | 0.1 | 0.2 | 0.3 |
| Radiotherapy | ||||||
| Yes | 32.7 | 28.9 | 31.3 | 27.8 | 34.1 | 31.6 |
| No | 67.3 | 71.1 | 68.6 | 72.2 | 65.9 | 68.3 |
| Unknown | 0.0 | 0.0 | 0.1 | 0.0 | 0.0 | 0.1 |
| Hormone therapy | ||||||
| Yes | 29.6 | 32.1 | 31.1 | 32.6 | 28.1 | 31.1 |
| No | 69.3 | 66.8 | 67.8 | 66.4 | 70.8 | 67.9 |
| Unknown | 1.1 | 1.1 | 1.1 | 1.0 | 1.1 | 1.0 |
| Neighborhood SES, quintile | ||||||
| 1 (lowest) | 21.6 | 36.2 | 38.9 | 48.3 | 4.3 | 4.8 |
| 2 | 23.1 | 24.9 | 32.5 | 29.3 | 13.7 | 13.4 |
| 3 | 22.2 | 17.8 | 19.5 | 15.5 | 24.8 | 23.9 |
| 4 | 18.3 | 12.5 | 7.0 | 5.4 | 29.6 | 30.9 |
| 5 | 14.9 | 8.6 | 2.1 | 1.5 | 27.6 | 27.0 |
Abbreviations: SES, socioeconomic status.
Follow-up through December 31, 2010.
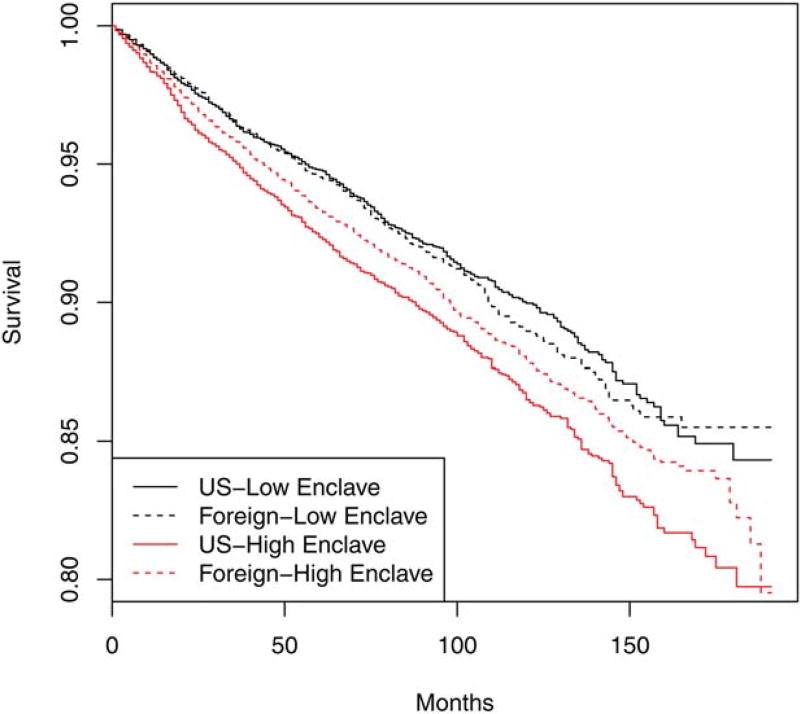
The unadjusted relationship between nativity and survival, stratified by ethnic enclave, for prostate cancer survival can be seen in the Kaplan-Meier curves shown in Figure 1. Overall, Foreign-born Hispanics living in a high ethnic enclave area were found to have better prostate cancer survival than their US-born counterparts; however, within low ethnic enclave areas, the survival curves were comparable between foreign-born and US-born Hispanics. The HRs of the fully adjusted Cox proportional hazards models for foreign-born Hispanics compared with US-born Hispanics are shown in Table 2. In these stage-stratified, age-adjusted models, foreign-born Hispanics had significantly better survival (HR, 0.81; 95% CI, 0.75–0.87). Ethnic enclave modified this effect (interaction P value of 0.009), with the survival advantage being more pronounced in the high ethnic enclave compared with low ethnic enclave neighborhoods. The HRs remained roughly the same after adjustment for significant personal and tumor characteristics as well as neighborhood SES.
Figure 1.
Kaplan-Meier survival curves are shown for the unadjusted relationship between nativity and ethnic enclave for California Hispanic men diagnosed with prostate cancer from 1995 through 2008.
TABLE 2.
Stratified Cox Proportional Hazards Model by Nativity for Hispanic Men With Prostate Cancer, Unstratified and Stratified by Ethnic Enclave: California, 1995 to 2008a
| Cancer-Specific Survival | |||
|---|---|---|---|
|
|
|||
| Variable | Unstratified HR (95% CI) | High Ethnic Enclave HR (95% CI) | Low Ethnic Enclave HR (95% CI) |
| Nativity | |||
| US born | 1.00 | 1.00 | 1.00 |
| Foreign born | 0.81 (0.75–0.88) | 0.78 (0.71–0.86) | 0.86 (0.76–0.98) |
| Age | 1.04 (1.03–1.05) | 1.04 (1.03–1.05) | 1.05 (1.04–1.06) |
| Marital status | |||
| Married | 1.00 | 1.00 | 1.00 |
| Never married | 1.13 (1.00–1.28) | 1.17 (1.01–1.35) | 1.02 (0.80–1.29) |
| Previously married | 1.15 (1.04–1.28) | 1.13 (1.00–1.27) | 1.21 (1.02–1.43) |
| Unknown | 0.91 (0.79–1.05) | 0.89 (0.75–1.06) | 0.96 (0.75–1.23) |
| Tumor grade | |||
| I | 0.74 (0.57–0.96) | 0.76 (0.55–1.03) | 0.68 (0.41–1.13) |
| II | 1.00 | 1.00 | 1.00 |
| III | 2.66 (2.42–2.91) | 2.66 (2.38–2.98) | 2.65 (2.26–3.10) |
| IV | 2.82 (2.04–3.90) | 3.16 (2.20–4.56) | 2.02 (0.98–4.15) |
| Unknown | 3.18 (2.80–3.60) | 3.26 (2.80–3.80) | 2.97 (2.37–3.71) |
| Surgery | |||
| No | 1.00 | 1.00 | 1.00 |
| Yes | 0.74 (0.66–0.82) | 0.75 (0.66–0.85) | 0.69 (0.57–0.84) |
| Unknown | 1.62 (0.88–2.97) | 1.29 (0.53–3.15) | 2.21 (0.94–5.18) |
| Radiotherapy | |||
| No | 1.00 | 1.00 | 1.00 |
| Yes | 0.83 (0.76–0.91) | 0.87 (0.78–0.97) | 0.79 (0.67–0.92) |
| Unknown | 2.16 (0.47–9.95) | 3.49 (0.40–30.5) | 1.41 (0.16–12.3) |
| Hormone therapy | |||
| No | 1.00 | 1.00 | 1.00 |
| Yes | 1.73 (1.58–1.90) | 1.70 (1.52–1.91) | 1.76 (1.50–2.06) |
| Unknown | 1.07 (0.77–1.47) | 1.05 (0.71–1.55) | 1.02 (0.56–1.85) |
| Neighborhood SES | |||
| High | 1.00 | 1.00 | 1.00 |
| Low | 1.13 (1.05–1.22) | 1.12 (1.01–1.25) | 1.10 (0.94–1.29) |
Abbreviations: 95% CI, 95% confidence interval; HR, hazards ratio; SES, socioeconomic status.
Follow-up through December 31, 2010.
To account for the possibility that many of the foreign-born Hispanics diagnosed with advanced disease may have left the country and thus their deaths may not have been captured by the registry, we performed a sensitivity analysis assuming that these individuals had died (n = 47). In the fully adjusted model, the survival results changed a small amount toward the null (HR, 0.84; 95% CI, 0.78–0.90). Because only 4.4% of cases with localized/regional stage among foreign-born Hispanics, died of prostate cancer, we believed that limiting the sensitivity analysis to the cases with advanced disease was a reasonable assumption.
DISCUSSION
Given the overall SES disadvantage of Hispanic Americans compared with NH white Americans, it remains unclear why Hispanic Americans appear to consistently experience better outcomes across several health indicators relative to NH whites.15,30–33 Studies on Hispanic populations are distinctively well positioned to investigate whether migration-related factors may help to describe these paradoxical patterns.12 Of particular interest, the Hispanic paradox has been attributed to better health outcomes specific to foreign-born Hispanics and indeed, previous studies have demonstrated that foreign-born Hispanics may possess certain culturally related health protective effects against cancer mortality.9,17,31 To evaluate whether clinical or neighborhood-level social factors may help to explain nativity-related differences in survival after a diagnosis of prostate cancer among Hispanic men, we used data from the large population-based CCR enhanced with neighborhood-level measures of ethnic enclave and SES.
To the best of our knowledge, the current study is the first to evaluate prostate cancer survival differences among Hispanics by ethnic enclave status. These findings support the growing body of evidence suggesting that prostate cancer survival among Hispanic men varies by nativity and acculturation-related factors.8,9 Singh et al demonstrated the importance of nativity for Hispanic Americans, demonstrating a more favorable covariate-adjusted prostate cancer-specific risk of death among US Hispanic immigrants.9 For acculturation-related factors, a spatial scan conducted in Texas indicated that clustering of lifestyle factors by county of residence was associated with prostate cancer mortality.8 The current study extends these findings by jointly investigating the effects of nativity and residence in an ethnic enclave and demonstrating that, within the Hispanic American population, foreign-born individuals have an even greater survival advantage than US-born individuals. Neighborhood ethnic enclave status appeared to modify that effect, strengthening the nativity association in high ethnic enclave neighborhoods.
Previous studies have suggested that lifestyle factors including diet, physical activity, body mass index, smoking history, and social support may mediate the observed overall survival benefit experienced by Hispanic immigrants.15,33–38 Data from the 2000 National Health Interview Survey indicate that Hispanics with less English language use were more adherent to multiple health behavior recommendations such as tobacco and alcohol use and fruit and vegetable consumption.36 Likewise, ethnic enclaves may reflect the extent to which Hispanic communities maintained the traditional, more healthful, lifestyle factors of their home countries before immigration. Ethnic enclaves may also confer more coethnic social support and networks, a mechanism that has been hypothesized as an explanation for the Hispanic paradox. Indeed, studies have identified a range of health advantages for Hispanic immigrants living in ethnic enclaves26,39 and also among Hispanics of lower SES.40 Models of acculturation and acculturative stress have been developed to conceptualize processes by which Hispanic immigrants may become integrated or separated from the US host society and the associated health effects of those processes.41 Qualitative research provides a more descriptive picture of how ethnic enclaves may act as support systems not only to maintain Hispanic cultural mores but also to shield immigrants from exposure to the possible effects of stigmatizing messages that exist in the racial dynamics in the United States.15 Our novel findings of better survival among foreign-born Hispanics in ethnic enclaves directs future research into possible protective factors unexplained by clinical factors and neighborhood SES, as well as to what extent these factors may help to explain observed survival differences (eg, diet, physical activity, social support, tangible support, translator assistance, and community resources). Moreover, further etiologic research is warranted to tease apart the independent and joint effects and mechanisms of lifestyle factors underlying the dynamics between nativity and ethnic enclave status that may help to inform interventions for improving cancer survivorship outcomes.
The strengths of the current study include the large, population-based data set; complete nativity information based on a validated imputation method; and incorporation of small-area–level neighborhood factors. However, similar to all population-based cancer registry analyses, it lacked detailed individual-level data regarding risk factors and was limited by some degree of missing data and/or nonstandardized assessment of Hispanic race/ethnicity and nativity constituting the basis for cancer registry abstraction.19,20,42 For race/ethnicity, a previous study from the Greater Bay Area Cancer Registry, a subset of the CCR, found that compared with self-report, the sensitivity and positive predictive value for Hispanics were moderate (70%–90%)43; however, Hispanic classification was likely improved in this study with the application of an algorithm to enhance classification based on surnames, given names, and birthplace.21 For nativity, another Greater Bay Area Cancer Registry report demonstrated that when registry birthplace was recorded, it was highly accurate,18 including high accuracy for death certificates.44 Our measurement of nativity relied on imputation for the 40% of patients with prostate cancer for whom registry data regarding birthplace were missing.
The current study findings of survival differences may also have been biased by the “healthy immigrant” hypothesis, the phenomenon of migrants entering the United States with healthier baseline characteristics,33,45–47 or by the “salmon effect,” in which migrants with serious illnesses return home to their birth countries to die.32,48,49 Due to the lack of detailed individual-level prostate cancer risk factor information available in the registry setting, we were unable to account for the possible impact of the healthy immigrant hypothesis. However, we demonstrated statistically that the salmon migration effect would not have likely biased our results by performing a sensitivity analysis in which all foreign-born patients with disease of advanced stage and who were lost to follow-up were assumed to be dead; this slightly shifted our results toward the null, but our findings remained statistically significant. An additional limitation inherent to cancer registry analyses is residual confounding by factors for which we lack information or detailed information, including detailed treatment and comorbidities.13,14,50
Conclusions
Despite the tendency toward a later stage of prostate cancer at the time of diagnosis and a greater likelihood of living in lower SES neighborhoods and Hispanic ethnic enclaves, foreign-born Hispanics were found to have better survival after prostate cancer than US-born Hispanics, a finding that is consistent with the Hispanic paradox. Further research is needed to examine the reasons for the observed paradox, because identifying factors that facilitate this survival advantage in Hispanic immigrants may improve survival for all men with prostate cancer.
Acknowledgments
FUNDING SUPPORT
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should be inferred.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
References
- 1.Ennis SR, Rios-Vargas M, Albert NG. 2010 Census Briefs. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. The Hispanic Population: 2010. [Google Scholar]
- 2.Humes KR, Jones NA, Ramirez RR. 2010 Census Briefs. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. An Overview: Race and Hispanic Origin and the 2010 Census. [Google Scholar]
- 3.Malone N, Baluja K, Costanzo J, Davis C. Census 2000 Brief. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2003. The Foreign-Born Population: 2000. [Google Scholar]
- 4.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 5.O’Brien K, Cokkinides V, Jemal A, et al. Cancer statistics for Hispanics, 2003. CA Cancer J Clin. 2003;53:208–226. doi: 10.3322/canjclin.53.4.208. [DOI] [PubMed] [Google Scholar]
- 6.Rosser CJ, Kuban DA, Levy LB, et al. Clinical features and treatment outcome of Hispanic men with prostate cancer following external beam radiotherapy. J Urol. 2003;170:1856–1859. doi: 10.1097/01.ju.0000092880.23660.de. [DOI] [PubMed] [Google Scholar]
- 7.Hoffman RM, Gilliland FD, Eley JW, et al. Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2001;93:388–395. doi: 10.1093/jnci/93.5.388. [DOI] [PubMed] [Google Scholar]
- 8.Hsu CE, Mas FS, Miller JA, Nkhoma ET. A spatial-temporal approach to surveillance of prostate cancer disparities in population subgroups. J Natl Med Assoc. 2007;99:72–80. 85–87. [PMC free article] [PubMed] [Google Scholar]
- 9.Singh GS, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91:392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du XL, Fang S, Coker AL, et al. Racial disparity and socioeconomic status in association with survival in older men with local/regional stage prostate carcinoma. Cancer. 2006;106:1276–1285. doi: 10.1002/cncr.21732. [DOI] [PubMed] [Google Scholar]
- 11.White A, Coker AL, Du XL, Eggleston KS, Williams M. Racial/ethnic disparities in survival among men diagnosed with prostate cancer in Texas. Cancer. 2011;117:1080–1088. doi: 10.1002/cncr.25671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eschbach K, Stimpson JP, Kuo Y, Gooewin JS. Mortality of foreign-born and US-born Hispanic adults at younger ages: a reexamination of recent patterns. Am J Public Health. 2007;97:1297–1304. doi: 10.2105/AJPH.2006.094193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Underwood W, DeMonner S, Ubel P, Fagerlin A, Sanda MG, Wei JT. Racial/ethnic disparities in the treatment of localized/regional prostate cancer. J Urol. 2004;171:1504–1507. doi: 10.1097/01.ju.0000118907.64125.e0. [DOI] [PubMed] [Google Scholar]
- 14.Latini DM, Elkin EP, Cooperberg MR, et al. Differences in clinical characteristics and disease-free survival for Latino, African American, and non-Latino white men with localized prostate cancer. Cancer. 2006;106:789–795. doi: 10.1002/cncr.21675. [DOI] [PubMed] [Google Scholar]
- 15.Viruell-Fuentes E. Beyond acculturation: immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007;65:1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Eschbach K, Mahnken JD, Goodwin JS. Neighborhood composition and incidence of cancer among Hispanics in the United States. Cancer. 2005;103:1036–1044. doi: 10.1002/cncr.20885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eschbach K, Kuo YF, Goodwin JS. Ascertainment of Hispanic ethnicity on California death certificates: implications for the explanation of the Hispanic mortality advantage. Am J Public Health. 2006;96:2209–2215. doi: 10.2105/AJPH.2005.080721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez SL, Glaser SL. Quality of cancer registry birthplace data for Hispanics living in the United States. Cancer Causes Control. 2005;16:713–723. doi: 10.1007/s10552-005-0694-7. [DOI] [PubMed] [Google Scholar]
- 19.Clegg L, Reichman M, Hankey B, et al. Quality of race, Hispanic ethnicity, and immigrant status in population-based cancer registry data: implications for health disparity studies. Cancer Causes Control. 2007;18:177–187. doi: 10.1007/s10552-006-0089-4. [DOI] [PubMed] [Google Scholar]
- 20.Gomez SL, Le GM, West DW, Satariano WA, O’Connor L. Hospital policy and practice regarding the collection of data on race, ethnicity, and birthplace. Am J Public Health. 2003;93:1685–1688. doi: 10.2105/ajph.93.10.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NAACCR Latino Research Group. NAACCR Guideline for Enhancing Hispanic/Latino Identification: Revised NAACCR Hispanic/Latino Identification Algorithm [NHIA v2] Springfield, IL: North American Association of Central Cancer Registries; 2005. [Google Scholar]
- 22.Fritz A, Percy C, Jack A, et al., editors. International Classification of Diseases for Oncology. 3. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 23.Gomez SL, Quach T, Horn-Ross PL, et al. Hidden breast cancer disparities in Asian women: disaggregating incidence rates by ethnicity and migrant status. Am J Public Health. 2010;100(suppl 1):S125–S131. doi: 10.2105/AJPH.2009.163931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Block G, Matanoski GM, Seltser RS. A method for estimating year of birth using social security number. Am J Epidemiol. 1983;118:377–395. doi: 10.1093/oxfordjournals.aje.a113645. [DOI] [PubMed] [Google Scholar]
- 25.Shimizu H, Ross RK, Bernstein L, Yatani R, Henderson BE, Mack TM. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br J Cancer. 1991;63:963–966. doi: 10.1038/bjc.1991.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keegan TH, Quach T, Shema S, Glaser SL, Gomez SL. The influence of nativity and neighborhoods on breast cancer stage at diagnosis and survival among California Hispanic women. BMC Cancer. 2010;10:603. doi: 10.1186/1471-2407-10-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12:703–711. doi: 10.1023/a:1011240019516. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. International Classification of Diseases. Geneva, Switzerland: World Health Organization; 1980. 9th Revision. [Google Scholar]
- 29.World Health Organization. International Classification of Diseases. Geneva, Switzerland: World Health Organization; 1992. 10th Revision. [Google Scholar]
- 30.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the ”salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hayes-Bautista D. Hispanic health: how healthy is the fastest growing population of the United States? Ethn Dis. 2002;12:459. [PubMed] [Google Scholar]
- 32.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 2):68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- 33.Peek MK, Cutchin MP, Salinas JJ, et al. Allostatic load among non- Hispanic whites, non-Hispanic blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. Am J Public Health. 2009;100:940–946. doi: 10.2105/AJPH.2007.129312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blue L, Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: the role of smoking. Int J Epidemiol. 2011;40:786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Efstathiou JA, Bae K, Shipley WU, et al. Obesity and mortality in men with locally advanced prostate cancer. Cancer. 2007;110:2691–2699. doi: 10.1002/cncr.23093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oh A, Dodd K, Ballard-Barbash R, Perna F, Berrigan D. Language use and adherence to multiple cancer preventive health behaviors among Hispanics. J Immigrant Minority Health. 2011;13:849–859. doi: 10.1007/s10903-011-9456-7. [DOI] [PubMed] [Google Scholar]
- 37.Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic paradox. Sleep. 2011;34:1021–1031. doi: 10.5665/SLEEP.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Waldstein A. Popular medicine and self-care in a Mexican migrant community: toward an explanation of an epidemiological paradox. Med Anthropol. 2010;29:71–107. doi: 10.1080/01459740903517386. [DOI] [PubMed] [Google Scholar]
- 39.Cagney KA, Browning CR, Wallace DM. The Latino paradox in neighborhood context: the case of asthma and other respiratory conditions. Am J Public Health. 2007;97:919–925. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Turra CM, Goldman N. Socioeconomic differences in mortality among U.S. adults: insights into the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2007;62:S184–S192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- 41.Caplan S. Latinos, acculturation, and acculturative stress: a dimensional concept analysis. Policy Polit Nurs Pract. 2007;8:93–106. doi: 10.1177/1527154407301751. [DOI] [PubMed] [Google Scholar]
- 42.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Inconsistencies between self-reported ethnicity and ethnicity recorded in a health maintenance organization. Ann Epidemiol. 2005;15:71–79. doi: 10.1016/j.annepidem.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 43.Gomez S, Glaser S. Misclassification of race/ethnicity in a population-based cancer registry (United States) Cancer Causes and Control. 2006;17:771–781. doi: 10.1007/s10552-006-0013-y. [DOI] [PubMed] [Google Scholar]
- 44.Gomez SL, Glaser SL. Quality of birthplace information obtained from death certificates for Hispanics, Asians, and Pacific Islanders. Ethn Dis. 2004;14:292–295. [PubMed] [Google Scholar]
- 45.Akresh IR, Frank R. Health selection among new immigrants. Am J Public Health. 2008;98:2058–2064. doi: 10.2105/AJPH.2006.100974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crimmins EM, Soldo BJ, Kim JK, Alley DE. Using anthropometric indicators for Mexicans in the United States and Mexico to understand the selection of migrants and the “hispanic paradox”. Soc Biol. 2005;52:164–177. doi: 10.1080/19485565.2005.9989107. [DOI] [PubMed] [Google Scholar]
- 48.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 49.Turra C, Elo I. The impact of salmon bias on the Hispanic mortality advantage: new evidence from social security data. Popul Res Policy Rev. 2008;27:515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barocas DA, Penson DF. Racial variation in the pattern and quality of care for prostate cancer in the USA: mind the gap. BJU Int. 2010;106:322–328. doi: 10.1111/j.1464-410X.2010.09467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]