Abstract
Background
Sleep is intricately tied to emotional well-being, yet little is known about the reciprocal links between sleep and psychosocial experiences in the context of daily life.
Purpose
To evaluate daily psychosocial experiences (positive and negative affect, positive events, and stressors) as predictors of same-night sleep quality and duration, in addition to the reversed associations of nightly sleep predicting next-day experiences.
Methods
Daily experiences and self-reported sleep were assessed via telephone interviews for eight consecutive evenings in two replicate samples of U.S. employees (131 higher-income professionals and 181 lower-income hourly workers). Multilevel models evaluated within-person associations of daily experiences with sleep quality and duration. Analyses controlled for demographics, insomnia symptoms, the previous day’s experiences and sleep measures, and additional day-level covariates.
Results
Daily positive experiences were associated with improved as well as disrupted subsequent sleep. Specifically, positive events at home predicted better sleep quality in both samples, whereas greater positive affect was associated with shorter sleep duration among the higher-income professionals. Negative affect and stressors were unrelated to subsequent sleep. Results for the reversed direction revealed that better sleep quality (and, to a lesser degree, longer sleep duration) predicted emotional well-being and lower odds of encountering stressors on the following day.
Conclusions
Given the reciprocal relationships between sleep and daily experiences, efforts to improve well-being in daily life should reflect the importance of sleep.
Keywords: sleep, daily stress, positive events, positive affect, negative affect
Introduction
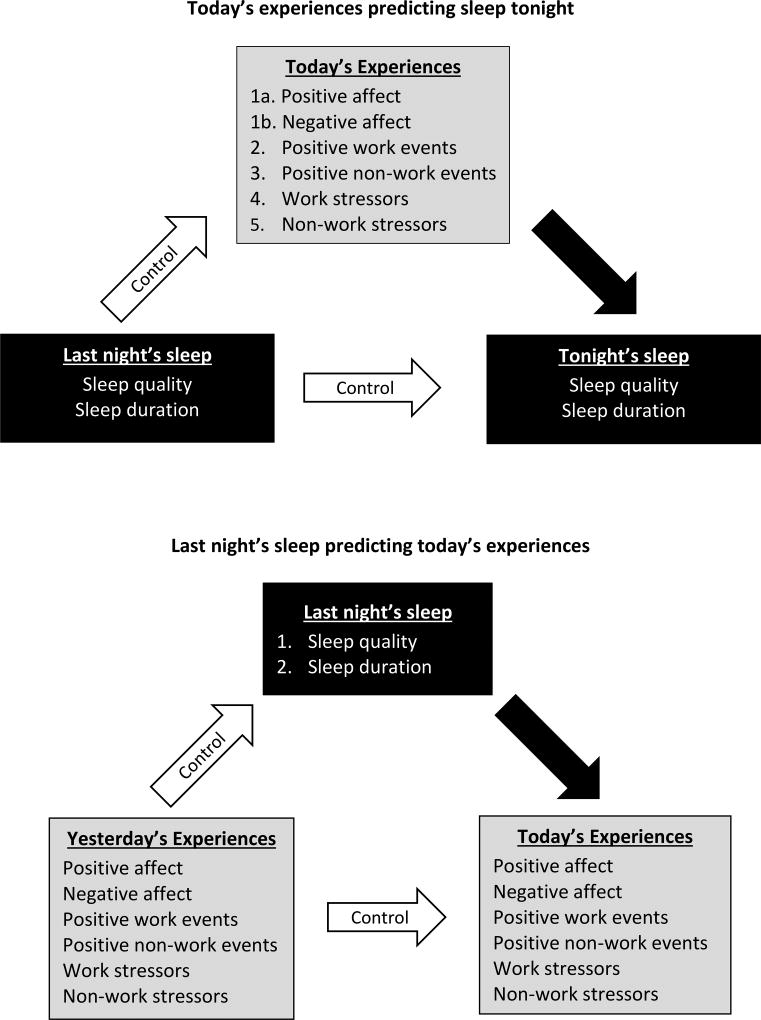
A large body of evidence has documented robust connections between sleep and emotional well-being (1,2). Much of the evidence linking sleep and emotions has been based on laboratory studies or single-administration measures that assess trait affect and typical sleep patterns (1,3). Naturally-occurring emotions, work and home demands, and sleep are far from static, however, and are marked by fluctuations within-persons from one day to the next (4–7). Day-to-day variations in psychosocial experiences may be linked to variations in sleep (e.g., Is sleep quality worse following a particularly negative day, relative to one’s average negative affect and sleep quality?) (8–15). Repeated measurements across short intervals, such as daily diaries, are ideal for examining within-person processes and for testing lagged and reciprocal associations between daily experiences and sleep (16). The current study evaluated the bidirectional associations of daily affect and events with self-reported sleep across one week in two replicate samples of middle-aged employees (Figure 1).
Figure 1. Conceptual model of reciprocal associations between daily experiences and nightly sleep.
In the top panel, the current day’s experiences are modeled as predictors of same-night sleep (black arrow), controlling for prior-night sleep (white arrows). In the bottom panel, prior-night sleep measures are modeled as predictors of current-day experiences (black arrow), controlling for prior-day experiences (white arrows).
Associations of work and non-work domains with subsequent sleep
Daily life is divided into three primary domains in employed adults—work, non-work, and sleep—that compete for resources as well as facilitate one another (17,18). The conservation of resources (COR) theory is a psychological framework (among other theories) that can be used to explain how stress at work and outside of work relates to sleep (19). COR theory posits that people strive to build and retain valued resources, which include conditions (e.g., work and family roles), objects (e.g., material goods), energies (e.g., time, mood, physical energy), and personal characteristics, e.g., optimism, (19,20). Psychological stress occurs when there is a potential for or actual loss of resources or when no resources are gained following resource investment (19). Based on COR theory, stressful events (for example, spousal disagreement about childcare responsibilities) are expected to threaten valued resources, such as marital quality (20). This threat of resource loss prompts individuals to expend resources to address the presence of a stressor (20), including borrowing time from sleep (17,21). For example, a within-person daily diary study of employed adults found that on days when work and family demands were higher than usual, participants subsequently spent less time sleeping to accommodate the increased demands (21). In addition to sleep duration, daytime stressors may contribute to impaired same-night sleep quality by increasing cognitive and somatic arousal, such as worry or muscle tension (22). As such, work and non-work demands—as well as their interface—have been linked to both poorer sleep quality and shorter sleep duration between-persons (17,23,24). Less research has examined the within-person associations of work and non-work stressors with sleep in the context of daily life (10,25,26). Given past research and propositions from COR theory, we hypothesized the following:
Hypothesis 1. Work stressors and non-work stressors will be associated with poorer same-night sleep quality and shorter sleep duration.
COR theory proposes that, in the absence of stressors, individuals will strive to build additional resources to offset the possibility of future loss (19). In the COR framework, positive events may lead to gains in resources (19,20). For example, a positive work event (e.g., accomplishing a difficult task) could result in increased resources such as greater self-efficacy, a pay raise, or workplace social support. These increased resources may, in turn, promote better physical health (27). Positive events occur more frequently than stressors in everyday life (28,29), yet few investigations have examined the associations between daily positive events and health. Between-person studies have shown that people who experience more frequent or more intense daily positive events tend to have lower levels of inflammation (28,30,31) and better subjective and polysomnography-assessed sleep (32), compared to people who have fewer or less-intense daily positive events. Based on this evidence, we hypothesized the following:
Hypothesis 2. Positive events at work and outside of work will be associated with better same-night sleep quality and longer sleep duration.
Asociations of sleep with next-day psychosocial experiences
In the COR framework, sleep is conceptualized as a resource (20). Inadequate sleep (i.e., low resource levels) is expected to increase vulnerability to further resource loss and diminish the ability to gain resources (e.g., reduced positive events) (20,33). Consistent with this notion, experimental sleep restriction has been shown to amplify affective, cardiovascular, and amygdala reactivity to negative stimuli and stressors (34,35). By contrast, several within-person studies have demonstrated that nights of adequate sleep were followed by days with better social interactions (13), affective recovery from negative events (36), and more appropriate emotional reactions to goal-enhancing and goal-disruptive events at work (15). We therefore hypothesized the following:
Hypothesis 3. Better sleep quality and longer sleep duration will be associated with lower odds of experiencing a work stressor or a non-work stressor on the following day.
Hypothesis 4. Better sleep quality and longer sleep duration will be associated with greater odds of experiencing a positive work or non-work event on the following day.
Bidirectional links between daily affect and sleep
Sleep is commonly believed to be important for emotional well-being the next day (13), and vice versa — good days precede a good night’s sleep (9,11,12). Indeed, at the within-person level, daily negative affect has been linked to more subsequent total wake time among participants with insomnia or bipolar disorder (12). Days with higher-than-usual positive affect were followed by longer self-reported total sleep time (11) and better sleep quality (9) in two samples of women, although elevated positive affect has also been linked to same-night sleep disturbance in participants with insomnia (12). In addition, within-person daily diary studies have provided support for the reversed relationship, such that better sleep quality (8,9,11,13,26,36), adequate sleep duration (9,26,37), and fewer insomnia symptoms (10) were predictive of next-day elevated positive affect and reduced negative affect. The current study extended previous research in several important ways: by explicitly testing both directions of association, by disaggregating between-person and within-person associations, by accounting for the confounding effects of prior-day measures, and by modeling positive and negative affect simultaneously to determine their unique contributions. Our final two hypotheses were as follows:
Hypothesis 5. Days of higher positive affect and lower negative affect will be associated with better same-night sleep quality and longer sleep duration.
Hypothesis 6. Better sleep quality and longer sleep duration will be associated with higher next-day positive affect and lower negative affect.
Methods
Design and participants
Study design
The data came from a larger study called the Work, Family, and Health Study, which was designed to examine the effects of workplace practices on the health of employees and their families in two multisite companies within the information technology (IT) and the extended care (nursing home) sectors (38). The IT company represented a higher-income, professional-level workforce, whereas the nursing care company was a lower-wage, hourly workforce. The two industries were examined as separate samples, rather than combined, due to important differences in demographics, socioeconomic status, job characteristics, and family structure (38–40). These meaningful differences between the samples permitted replication of the analyses linking daily experiences and sleep, as well as insight into how these daily processes may unfold differentially based on varying contextual and individual factors.
The present study uses baseline data collected by trained interviewers, who administered face-to-face computer-assisted personal interviews with employees in the workplace. Employees with children ages 9–17 living in the home were further eligible for family data collection, which included a daily diary study. To minimize the time interval between the workplace interview and the daily diary study, participants were given a 4-week period to initiate the daily assessments. The daily diary protocol consisted of telephone interviews for eight consecutive evenings, during which the participants answered questions about their emotions and experiences that day and about their sleep on the prior night. All participants provided written informed consent, and study procedures were approved by appropriate Institutional Review Boards.
IT employees
Participants were recruited from 56 “study groups” (clusters of employees and managers) in the IT division of a U.S. Fortune 500 organization. Of 1171 eligible employees, 823 (70%) enrolled in the study and completed the workplace interview. Of these, 206 were eligible for family data collection, and 148 were further eligible for the daily diary study after completing the initial home interview. The final sample size consisted of 131 IT employees who participated in the daily diary study (64% of 206 eligible for family data collection).
Extended care employees
Participants were recruited from 30 extended care facilities in six states. Employees were eligible if they normally worked a minimum of 22 hours per week in direct patient care. Those who exclusively worked night shifts were not eligible. Of 1783 eligible employees, 1523 (85%) completed the workplace interview. Of these, 373 had an age-eligible child for family data collection, and 257 were eligible for the daily diary study after completing the initial home interview. A final sample of 181 extended care employees participated in the daily diary study (49% of 373 eligible for family data collection).
Measures
Daily affect
Affect was assessed every day using items adapted from the Positive and Negative Affect Schedule (41). Participants reported how often they had experienced 10 positive emotions (interested, excited, strong, enthusiastic, proud, alert, inspired, determined, attentive, and active) and 10 negative emotions (distressed, upset, guilty, scared, hostile, irritable, ashamed, nervous, jittery, and afraid) using a 5-point rating scale (1 = none of the time, 2 = a little of the time, 3 = some of the time, 4 = most of the time, 5 = all of the time). Items were averaged to create subscale scores for daily positive and negative affect. The subscales had high internal consistency reliability: Cronbach’s α for positive affect was 0.91 in IT employees and 0.89 in extended care employees, and Cronbach’s α for negative affect was 0.83 in IT employees and 0.82 in extended care employees.
Daily positive events
Positive work-related and non-work events were assessed with two items. When participants indicated that they had worked at their primary job in the past 24 hours, they were asked about the occurrence of any positive work events: “Did you have an experience at your primary job that was particularly positive since this time yesterday?” Positive non-work (home) events were assessed with the question, “Since this time yesterday, did you have an experience at home that was particularly positive?” Response choices were yes (1) or no (0). This measure of daily positive events has previously been shown to predict daily affect, sleep, and physical health in other samples (28,42,43).
Daily stressors
Daily stressors were measured with an adapted version of the Daily Inventory of Stressful Events (44). This instrument is a semi-structured interview that asks whether the following stressors had occurred in the past 24 hours: (a) argument or disagreement, (b) avoided an argument, (c) network stressor (i.e., something happened to a co-worker, family, or friend that was stressful to the participant), (d) stressful demands (e.g., deadlines, childcare), and (e) any other stressor. These five types of stressors were assessed separately for the work domain and outside of work. Work stressors and non-work stressors were assigned a score of 1 if any work or non-work stressors occurred that day, respectively, whereas a score of 0 indicated no stressors.
Nightly sleep quality and duration
During telephone interviews each evening, participants answered questions adapted from the Pittsburgh Sleep Quality Index (45) about their sleep on the prior night. Sleep quality was assessed with the question, “How would you rate last night’s sleep quality overall?” Responses were scored as follows: 1 = very badly, 2 = badly, 3 = well, and 4 = very well. Sleep duration was assessed with the question, “How many hours did you sleep last night?”
Person-level covariates
Demographic covariates included age, gender (0 = female, 1 = male), and race (0 = non-White, 1 = White). Insomnia symptoms in the past month were assessed at the baseline workplace interview using two items from the Pittsburgh Sleep Quality Index (45). The items asked how often the participant could not fall asleep within 30 minutes and how often he/she woke up in the middle of the night or early morning (response options were 1 = never, 2 = less than once a week, 3 = one or twice a week, 4 = three or more times a week). The two items were summed, such that insomnia symptom scores ranged from 2 to 8. The study results were unchanged when we controlled for marital status. To keep the models parsimonious, marital status was not included as a covariate.
Day-level covariates
When examining day-lagged associations, the outcome variable measured on the prior day could be linked with both the prior-day predictors and the next-day outcome (Figure 1). For example, yesterday’s stressor may have been associated with impaired sleep last night, as well as greater odds of experiencing a stressor today. The association of sleep with next-day stressors should therefore be adjusted for prior-day stressors. Thus, in analyses for sleep predicting next-day psychosocial experiences, we controlled for the corresponding outcome measure of the psychosocial experiences from the prior day. Similarly, in models for daily experiences predicting sleep quality or duration, we controlled for the sleep measure on the prior night. Additional day-level covariates were the Day in Study (i.e., 0, 1, 2, …, 7) and Work Day (0 = no, 1 = yes), except for models predicting work events as outcomes (in which we only analyzed work days). To determine the unique contributions of positive versus negative affect, models predicting positive affect controlled for negative affect, and vice versa.
Data analysis
For descriptive purposes, differences in participant characteristics between IT and extended care employees were assessed using t-tests for continuous variables and chi-squared tests for categorical variables. Within-person correlations were computed as the ordinary correlation coefficients between the within-person deviations (Xdi − X̄·i) and (Ydi − Ȳ·i) (46). For the primary analyses, data were analyzed using multilevel models to account for the nesting of days within persons (PROC MIXED with maximum likelihood estimation in SAS 9.4). Multilevel linear models were used for continuous outcomes (affect and sleep), whereas multilevel logistic models were used for dichotomous outcomes (positive events and stressors). The first set of models tested daily experiences—positive and negative affect, positive work and non-work events, and work and non-work stressors—as predictors of same-night sleep quality and sleep duration. The second set of models evaluated the reversed associations, i.e., sleep quality and sleep duration predicting next-day experiences. The sample sizes for number of participants and for number of observation-days varied slightly due to the lagged design. Specifically, when testing daily experiences as predictors of same-night sleep, daily experiences for the final day were excluded from analyses because we did not have assessments of sleep that night. Likewise, when testing nightly sleep as a predictor of next-day experiences, the first day of observation was excluded because we could not control for prior-day experiences.
Although this study focused on within-person associations, the multilevel models included both between- and within-person levels of analysis (47). The between-person level of analysis evaluated differences between individuals (e.g., Did people with higher positive affect have longer sleep duration?). To test between-person effects, individuals’ scores were averaged across days, centered at the grand mean, and entered at Level 2. To test within-person effects, time-varying (daily) scores were centered at the person’s mean and entered at Level 1. Person-mean centering allowed us to interpret parameter estimates in terms of an individual’s deviation from his or her own average levels (For example, did a person’s sleep duration differ on days when their positive affect was higher than their average positive affect?). The following is an example equation of positive affect on day d as a function of person i’s sleep duration on the prior night (within-person) and his or her average sleep duration (between-person), controlling for prior-day positive affect and other covariates:
| (Level 1) |
| (Level 2) |
To reduce the risk of Type I error, p-values were corrected by applying the adjusted False Discovery Rate procedure (48) using PROC MULTTEST in SAS 9.4. P-values were corrected for 24 comparisons within each sample (i.e., 12 tests for 6 daily experiences predicting 2 sleep measures, and 12 tests for 2 sleep measures predicting 6 daily experiences). We presented the results based on the original significance levels and indicated changes that occurred after correcting for multiple comparisons.
Results
Sample characteristics
Table 1 describes key characteristics of the two samples. Participants (N = 131) from the IT industry completed a total of 869 daily interviews. The IT employees ranged in age from 29 to 63 years old (mean = 45 years). The sample was 45% female; 78% were college graduates; 70.2% were White, 1.5% Black or African American, 9.9% Asian Indian, 8.4% other Asian/Pacific Islander, 9.2% Hispanic, and 0.8% other races. In contrast, the sample of 181 employees in the extended care industry provided 1061 daily interviews. Participants ranged in age from 21 to 58 years old (mean = 39 years). Extended care employees were nearly all female (97%), were more ethnoracially diverse than the IT sample (63.5% White, 13.3% Black or African American, 14.4% Hispanic, and 8.8% other), and most reported high school or some college/technical school as the highest level of education attained. On average, extended care employees worked fewer hours per week (37 hours) than IT employees (46 hours), and they were less likely to be married or living with a partner (66%) compared to the IT sample (87%).
Table 1.
Percentage or mean (SD) for participant characteristics in IT and extended care employees
| Participant characteristic | IT employees (N = 131, Ndays = 869) |
Extended care employees (N = 181, Ndays = 1061) |
p |
|---|---|---|---|
| Age | 45.14 (6.32) | 38.64 (6.37) | <0.001 |
| Female | 45% | 97% | <0.001 |
| Race | <0.001 | ||
| White | 70.2% | 63.5% | |
| Black or African American | 1.5% | 13.3% | |
| Asian Indian | 9.9% | 0.5% | |
| Other Asian/Pacific Islander | 8.4% | 3.3% | |
| Hispanic | 9.2% | 14.4% | |
| Other race or >1 race | 0.8% | 5.0% | |
| Highest level of education | <0.001 | ||
| Some high school | 0% | 6% | |
| High school graduate | 2% | 30% | |
| Some college or technical school | 20% | 54% | |
| College graduate | 78% | 10% | |
| Hours worked per week | 45.89 (5.86) | 36.69 (8.10) | <0.001 |
| Married or cohabitating (vs. single) | 87% | 66% | <0.001 |
| Number of children at home | 2.11 (1.07) | 2.27 (1.11) | 0.19 |
| Daily experiences | |||
| Positive affect (range: 1–5) | 2.88 (0.68) | 2.88 (0.65) | 0.97 |
| Negative affect (range: 1–5) | 1.27 (0.25) | 1.39 (0.33) | <0.001 |
| Positive work event, % of days | 24% (27%) | 27% (32%) | 0.41 |
| Positive non-work event, % of days | 29% (27%) | 33% (31%) | 0.28 |
| Work stressor, % of days | 44% (30%) | 43% (35%) | 0.84 |
| Non-work stressor, % of days | 40% (29%) | 36% (27%) | 0.20 |
| Sleep variables | |||
| Sleep quality (range: 1–4) | 3.03 (0.41) | 2.97 (0.54) | 0.25 |
| Sleep duration, hours | 6.70 (0.87) | 6.49 (1.05) | 0.06 |
| Insomnia symptoms (range: 2–8) | 5.41 (1.51) | 5.72 (1.65) | 0.09 |
| Daily interviews completed | 7.71 (0.93) | 7.13 (1.62) | <0.001 |
Note. P-values for differences between IT and extended care employees were obtained from t-tests for continuous variables and chi-squared tests for categorical variables.
The samples were comparable in their assessments of daily experiences and sleep, except extended care employees had higher negative affect than IT employees (Table 1). Participants reported positive work events on approximately one-fourth of interview days and positive non-work events on nearly one-third of days. Work stressors occurred on over 40% of days and non-work stressors occurred on 36–40% of days. The average sleep quality score of approximately 3 indicated that the participants slept “well.” Extended care employees reported sleeping an average of 6 hours and 30 minutes, whereas IT employees reported sleeping 6 hours and 42 minutes. Insomnia symptoms in the past month—that is, sleep onset latency >30 minutes and waking in the middle of the night or early morning—occurred nearly once or twice per week (corresponding with a composite score of about 6).
Within-person correlations for daily experiences and sleep
Table 2 shows within-person correlations and intraclass correlation coefficients (ICC; between-person level variance/total variance) among the variables of interest. Between-person correlations are provided in Supplementary Table 1. For both samples, the ICCs indicated that 60–65% of the variance in daily positive affect and 42% of the variance in daily negative affect were due to between-person differences. Most of the variance in positive events, stressors, and sleep were attributable to day-to-day differences within individuals. Specifically, between-person differences accounted for only 26–33% of variance in positive events, 20–26% for stressors, and 25–33% for sleep quality and duration.
Table 2.
Within-person correlations between prior-night sleep and current-day experiences
| Variable | Positive affect |
Negative affect |
Positive work event |
Positive non- work event |
Work stressors |
Non-work stressors |
Sleep quality |
Sleep duration |
|---|---|---|---|---|---|---|---|---|
| Industry 1 replicate (131 IT employees) | ||||||||
| Positive affect | 0.65 | |||||||
| Negative affect | −0.10** | 0.42 | ||||||
| Positive work event | 0.09* | 0.08* | 0.26 | |||||
| Positive non-work event | 0.10** | −0.02 | 0.17*** | 0.28 | ||||
| Work stressors | 0.06 | 0.30*** | 0.11** | 0.02 | 0.22 | |||
| Non-work stressors | −0.02 | 0.23*** | 0.13*** | 0.06* | 0.13*** | 0.26 | ||
| Sleep quality | 0.13*** | −0.17*** | 0.03 | 0.05 | −0.11* | −0.07* | 0.25 | |
| Sleep duration | 0.10** | −0.10** | 0.04 | 0.06† | −0.13** | −0.002 | 0.43*** | 0.32 |
| Industry 2 replicate (181 extended care employees) | ||||||||
| Positive affect | 0.60 | |||||||
| Negative affect | −0.22*** | 0.42 | ||||||
| Positive work event | 0.13*** | 0.05 | 0.31 | |||||
| Positive non-work event | 0.09** | −0.02 | 0.27*** | 0.33 | ||||
| Work stressors | 0.01 | 0.24*** | 0.03 | 0.04 | 0.24 | |||
| Non-work stressors | −0.08* | 0.31*** | 0.06 | 0.05† | 0.12** | 0.20 | ||
| Sleep quality | 0.16*** | −0.13*** | 0.21*** | 0.04 | −0.10* | −0.14*** | 0.33 | |
| Sleep duration | 0.06+ | −0.09** | 0.03 | 0.05† | −0.03 | −0.11*** | 0.45*** | 0.26 |
Note.Diagonals (bold) show intraclass correlation coefficients (ICC = between-person level variance/total variance) of the variable. Correlations for IT employees were based on Ndays = 862 for affect and non-work events and Ndays = 505 for work events. Correlations for extended care employees were based on Ndays = 1060 for affect and non-work events and Ndays = 410 for work events. Affect was rated on a 1 (none of the time) to 5 (all of the time) scale. Positive events and stressors were coded as yes (1) or no (0). Sleep quality was rated 1 (very badly) to 4 (very well). Sleep duration was reported in hours.
p < 0.001,
p < 0.01,
p < 0.05,
p < 0.10
Within-person correlations for daily experiences and sleep were small to moderate in magnitude. The two samples showed fairly similar patterns of correlations, albeit with several differences. Nights of better sleep quality were correlated with elevated next-day higher positive affect, lower negative affect, and reduced odds of work and non-work stressors in both samples. In extended care employees, better sleep quality was also associated with higher odds of experiencing a positive work event on the following day. Longer sleep duration was correlated with better next-day emotional well-being in both samples, reduced odds of a work stressor in IT employees, and reduced odds of a non-work stressor in extended care employees.
Daily experiences predicting same-night sleep quality and duration
Supplementary Figure 1 summarizes results for both within- and between-person levels of analysis. On days when IT employees experienced higher-than-usual positive affect (i.e., a 1-point change), they subsequently slept 15 minutes less than their average sleep duration (unstandardized B coefficient = −0.253 hours; upper half of Table 3). Positive non-work events (i.e., at home) predicted better-than-usual sleep quality in both samples (B = 0.119 for IT employees, B = 0.151 for extended care employees). By contrast, the occurrence of a positive work event was linked to poorer same-night sleep quality among extended care employees (B = −0.181; lower half of Table 3), although this association was not significant after correcting for multiple comparisons. Contrary to our hypotheses, daily negative affect and stressors were not predictive of same-night sleep measures in either sample.
Table 3.
Daily experiences predicting same-night sleep quality and duration in 2 employee samples
| Models with daily affect or events as predictors |
Ndays | Sleep Quality Unstd. B (95% CI) |
Sleep Duration Unstd. B (95% CI) |
|---|---|---|---|
| Industry 1 replicate (131 IT employees) | |||
| 1. Affect model | 864 | ||
| 1a. Positive affect | −0.088 (−0.180, 0.005)† | −0.253 (−0.433, −0.074)**a | |
| 1b. Negative affect | −0.028 (−0.190, 0.134) | −0.155 (−0.468, 0.158) | |
| 2. Positive work event | 626 | −0.051 (−0.193, 0.090) | −0.205 (−0.469, 0.060) |
| 3. Positive non-work event | 867 | 0.119 (0.009, 0.228)*b | 0.176 (−0.039, 0.390) |
| 4. Work stressor | 625 | −0.021 (−0.141, 0.098) | 0.003 (−0.220, 0.226) |
| 5. Non-work stressor | 867 | 0.036 (−0.068, 0.140) | 0.045 (−0.158, 0.248) |
| Industry 2 replicate (181 extended care employees) | |||
| 1. Affect model | 1058 | ||
| 1a. Positive affect | −0.002 (−0.091, 0.086) | 0.109 (−0.088, 0.305) | |
| 1b. Negative affect | 0.022 (−0.108, 0.152) | 0.0178 (−0.273, 0.309) | |
| 2. Positive work event | 640 | −0.181 (−0.346, −0.015)*c | −0.170 (−0.528, 0.189) |
| 3. Positive non-work event | 1059 | 0.151 (0.034, 0.269)*b | 0.205 (−0.056, 0.467) |
| 4. Work stressor | 641 | −0.010 (−0.151, 0.132) | 0.097 (−0.207, 0.401) |
| 5. Non-work stressor | 1061 | 0.033 (−0.075, 0.141) | −0.037 (−0.276, 0.201) |
Note.Daily experiences were each tested in separate models as predictors of same-night sleep quality or duration, controlling for between-person effects of the daily experience variable. Models also controlled for age, gender, race (White vs. non-White), day in study (Day 0, Day 1, …, Day 7), work day (yes/no), insomnia in the past month, and prior night sleep measure (prior night sleep quality or duration).
p < 0.001,
p < 0.01,
p < 0.05,
p < 0.10
Effect remained significant at p < 0.05 after correcting for multiple comparisons
Effect was marginally significant at p < 0.08 after correcting for multiple comparisons
Effect was not significant after correcting for multiple comparisons (corrected p = 0.12)
Nightly sleep quality and duration predicting next-day experiences
After nights when sleep quality was better than usual, both IT and extended care employees had elevated positive affect and lower odds of experiencing stressors on the following day (Table 4). Better sleep quality was also associated with lower next-day negative affect among IT employees (upper half of Table 4), as well as nearly threefold greater odds of experiencing a positive event at work among extended care employees (odds ratio = 2.930; lower half of Table 4). Following nights when sleep duration was longer than usual, IT employees had higher positive affect and lower odds of a work stressor. As indicated in Table 4, the significant results for sleep quality and sleep duration as predictors of next-day experiences remained significant (p < 0.05) or marginally significant (p < 0.08) after correcting for multiple comparisons. Contrary to hypotheses, nightly sleep duration in IT employees was not related to next-day negative affect, positive events, or non-work stressors. Nightly sleep duration did not predict any measure of experiences on the following day among extended care employees.
Table 4.
Nightly sleep predicting next-day experiences in 2 employee samples
| Sleep predictors (each cell is a separate model) |
Positive affect Unstd. B (95% CI) |
Negative affect Unstd. B (95% CI) |
Positive work event OR (95% CI) |
Positive non-work event OR (95% CI) |
Work stressor OR (95% CI) |
Non-work stressor OR (95% CI) |
|---|---|---|---|---|---|---|
| Industry 1 replicate (131 IT employees) | ||||||
| Ndays = 862 | Ndays = 862 | Ndays = 505 | Ndays = 869 | Ndays = 505 | Ndays = 869 | |
| 1. Sleep quality | 0.094 (0.035, 0.154)**a | −0.051 (−0.080, −0.021)***a | 1.000 (0.652, 1.533) | 1.104 (0.810, 1.503) | 0.616 (0.422, 0.899)*a | 0.737 (0.556, 0.977)*b |
| 2. Sleep duration | 0.041 (0.009, 0.074)*a | −0.004 (−0.020, 0.012) | 1.206 (0.920, 1.580) | 1.042 (0.879, 1.234) | 0.766 (0.608, 0.964)*b | 1.031 (0.886, 1.199) |
| Industry 2 replicate (181 extended care employees) | ||||||
| Ndays = 1060 | N days = 1060 | Ndays = 410 | N days = 1060 | N days = 410 | N days = 1060 | |
| 1. Sleep quality | 0.124 (0.075, 0.173)***a | −0.022 (−0.055, 0.010) | 2.930 (1.705, 5.035)***a | 1.079 (0.826, 1.408) | 0.668 (0.442, 1.011)† | 0.721 (0.568, 0.915)**a |
| 2. Sleep duration | 0.016 (−0.008, 0.039) | −0.005 (−0.019, 0.010) | 1.051 (0.839, 1.316) | 1.029 (0.911, 1.163) | 0.883 (0.722, 1.080) | 0.910 (0.813, 1.020) |
Note.Sleep quality and sleep duration were tested in separate models as predictors of each daily experience outcome. Models also controlled for age, gender, race (White vs. non-White), day in study (Day 0, Day 1, …, Day 7), work day (yes/no), insomnia in the past month, and outcome variable (e.g., affect, positive event, stressor) measured on the prior day. The positive affect analyses included additional covariates for prior- and same-day negative affect, and the negative affect analyses included covariates for prior- and same-day positive affect.
p < 0.001,
p < 0.01,
p < 0.05,
p < 0.10
Effect remained significant at p < 0.05 after correcting for multiple comparisons
Effect was marginally significant at p < 0.08 after correcting for multiple comparisons
Between-person associations of daily experiences and sleep
Because our study focused on within-person associations, we provide only a brief overview of between-person findings here. Readers interested in the full results may refer to Supplementary Tables 2 and 3 (IT and extended care employees, respectively) for analyses of daily experiences predicting same-night sleep, as well as Supplementary Tables 4 and 5 for analyses of nightly sleep predicting next-day experiences.
The between-person level of analysis assessed whether a person’s average daily experiences (aggregated across days) were related to his or her average sleep measures. Unlike the within-person level of analysis, between-person associations were not lagged or directional. In both samples, individuals with higher average negative affect and lower positive affect tended to have poorer sleep quality. People who experienced more frequent stressors reported poorer sleep quality and shorter sleep duration, compared to those who encountered fewer stressors.
Discussion
Stress and emotions are robustly associated with sleep, yet less is known about the reciprocal relationships between sleep and psychosocial experiences in the context of everyday life. The purpose of this study was to evaluate daily psychosocial experiences as predictors of same-night sleep quality and duration, in addition to the reversed associations of nightly sleep predicting next-day experiences. We found limited support for our hypotheses regarding daily experiences as predictors of same-night sleep: positive affect and positive events were associated with better as well as poorer subsequent sleep, whereas negative affect and stressors were unrelated to same-night sleep. The results showed more support for nightly sleep quality as a predictor of next-day experiences, including higher positive affect and reduced odds of encountering stressors in both samples, lower negative affect in IT employees, and greater odds of positive work events in extended care employees. In line with COR theory, the current study suggests that adequate sleep is a resource that may facilitate further resource gain (e.g., positive affect and positive events) and guard against resource loss and stress (19,20,33). Taken together, these findings support the reciprocal roles of sleep with psychosocial experiences in everyday life and highlight the importance of examining these processes within individuals.
There was no support in either sample for our hypothesis that work and non-work stressors would be linked with poorer same-night sleep quality and shorter sleep duration (Hypothesis 1). Our results differed from those of several previous within-person investigations. For example, a study of 50 participants found that feelings of stress and worry at bedtime predicted poorer self-reported sleep quality across 42 days (49). In a community sample of 67 participants tracked for three weeks, both the frequency and subjective impact of daily stressors were associated with greater pre-sleep cognitive and somatic arousal, which in turn, predicted poorer self-reported sleep quality and efficiency (22). However, other studies have produced mixed findings regarding the link between daily stressors and sleep (14,25). A 2-week study of 145 healthy young women demonstrated that, following days with higher-than-usual stressors, actigraphic sleep efficiency was better whereas subjective sleep quality was worse (14). In addition, a study of Danish employees found bidirectional associations of daily work and family stressors with poorer sleep as reported on the awakening index of the Karolinska Sleep Questionnaire (e.g., exhausted at awakening, non-refreshing sleep), yet daily stressors were unrelated to the disturbed sleep index (e.g., difficulty falling asleep, disturbed/restless sleep) (25). The inconsistencies in the literature might be due, at least in part, to differences in sleep characteristics and measures, such as subjective versus objective measures (14) and differences between self-report questionnaires (22,25,49). There are also meaningful differences in the stress constructs under investigation, including the occurrence of daily stressors (14,22,25), subjective ratings of daytime stress (14,22), and stress at bedtime (25,49).
We found partial support—and an unexpected result—for our prediction that daily positive events will be related to better same-night sleep (Hypothesis 2). Positive events at home were associated with better subsequent sleep quality in both industries; this was in line with the theoretical proposition that positive events may signify or lead to increased resources that, in turn, promote health (19,33). The only existing within-person study of daily positive events and sleep demonstrated a similar pattern, such that positive home events across 2 days were marginally associated with lower self-reported sleep disturbance (25). Surprisingly, we found that positive work events predicted poorer sleep quality among extended care employees. These sleep disruptions may have been due to amplified emotions such as excitement (43), recurrent thoughts about the positive events, and increased physiological reactivity. The correlation between positive work events and same-day positive affect was somewhat stronger among extended care employees than in IT employees, raising the possibility that the positive work events encountered by extended care employees were relatively more activating. Also contrary to our hypothesis, there were no associations between positive events and sleep duration. Because the participants were employed and had children, sleep duration was likely dictated by family and work schedules and was perhaps less susceptible to minor events. Additional work is needed to examine subjective aspects of daily positive events (e.g., emotional responses, appraisals), in addition to evaluating positive events as potential buffers in the association between stressors and sleep.
Our next pair of hypotheses focused on the reversed direction of association: Are better sleep quality and longer sleep duration associated with reduced odds of experiencing stressors (Hypothesis 3) and greater odds of encountering positive events (Hypothesis 4) on the following day? After correcting for multiple comparisons, sleep duration was again not significantly associated with stressors or positive events. Better sleep quality, on the other hand, predicted lower odds of work stressors in IT employees and non-work stressors in extended care employees. Better sleep quality also predicted greater odds of positive work events among extended care employees. These results were consistent with a previous study that linked poorer self-reported sleep quality to greater odds of experiencing work and family stressors on the following day, as well as marginally lower odds of positive work events (25). It is important to note that the current analyses focused on whether stressors and positive events occurred (i.e., exposure), but not emotional reactivity or appraisals of the events. Prior investigations have shown that nights of adequate sleep were followed by less affective reactivity to daily stress in college students (50) and more affective recovery from stressors among women with fibromyalgia (36). Thus, future research should seek to delineate the roles of sleep in exposure, reactivity, and recovery for daily events.
Several prior studies have reported bidirectional relationships between daily affect and sleep (11,12,51), but our results did not support the prediction that higher positive affect and lower negative affect would be linked with better same-night sleep quality and longer sleep duration (Hypothesis 5). Contrary to our hypothesis, on days when positive affect was higher than usual, IT employees subsequently slept 15 minutes less than usual. This unexpected result was consistent with a previous finding, in which greater positive affect in the evening was linked with more total wake time among individuals with insomnia (12). Although between-person differences in positive affect and positive events are often described as protective factors for health (28,32,52–54), our study suggests that positive aspects of daily life were not entirely beneficial for sleep at the within-person level. Daily positive affect and events may be associated with transient disruptions in sleep when they occur at greater frequency or intensity than one’s usual level.
The most consistent pattern of results emerged for Hypothesis 6, in which better sleep quality predicted next-day higher positive affect in both samples. Among IT employees only, longer sleep duration was also associated with higher positive affect, and better sleep quality predicted reduced negative affect. These findings were concordant with other within-person studies, which have shown that affect was more strongly linked to prior-night sleep than to subsequent sleep (8–10,13,26,36,37). For example, a 14-day study of community-dwelling older adults found that nights of better subjective sleep quality or less reported wake time were associated with higher positive affect and lower negative affect on the following day (8). Our findings were also in line with previous evidence suggesting that sleep may be more robustly linked with positive affect than with negative affect in daily life (9,11,55). Thus, the current study supported existing findings on the day-to-day associations of sleep with stress and affect, and we extended the literature in several ways. First, we examined a broader range of positive and stressful events, rather than focusing solely on affect. Next, due to the intensive nature of data collection, previous studies have primarily used small samples. We sought to replicate our findings in two samples of employed, middle-aged adults that differed widely in demographics, socioeconomic status, and the nature of their work. Lastly, we were stringent in our analytic approach by controlling for the outcome variable measured on the prior day, by testing both positive and negative affect in the same models to determine their independent associations, and by disaggregating within-person and between-person associations (47).
Potential mechanisms
Pathways between daily psychosocial experiences and sleep may differ depending on the causal direction. When considering poor sleep as a predictor of next-day events, it was unclear whether people were objectively experiencing more stressors and fewer positive events or whether their perceptions had changed. Sleep-deprived individuals show greater negative affect than rested controls following exposure to a mild experimental stressor but not in response to a high-intensity stressor, suggesting that sleep deprivation lowers the threshold at which a person experiences an event as stressful (56). Neuroimaging evidence points to the loss of functional connectivity between the amygdala and medial prefrontal cortex as a neural pathway linking sleep deprivation to negative emotional reactivity (35). Investigations of the mechanisms linking sleep to next-day experiences should be expanded beyond experimental sleep deprivation to include naturally-occurring variations in sleep.
Daily stressors may impair subsequent sleep through greater emotional, physiological, or cognitive arousal. For example, higher daytime stress is associated with elevated pre-sleep somatic and cognitive arousal (e.g., muscle tension, racing thoughts), which in turn are linked to poorer same-night sleep efficiency and quality (14,22). To our knowledge, no studies have identified mechanisms whereby positive affect or positive events are linked to subsequent sleep.
Limitations and Future Directions
Several limitations should be considered when interpreting these findings. First, prior-night sleep was assessed during telephone interviews on the following evening. The gap in time between waking and the sleep assessment introduced the possibility that other factors during the day may have interfered with the participants’ recall and perceptions of prior-night sleep. Common method bias also may have contributed to the results for prior-night sleep as a predictor of current-day experiences. In addition, self-reported sleep quality and duration were each measured with only a single item, which may have been less reliable and valid than multiple-item scales. Future research would be strengthened by using more comprehensive assessments of subjective sleep in the morning, as well as objective measures of sleep (e.g., actigraphy, polysomnography). Second, multiple statistical tests were conducted and may have increased the risk of Type I error. However, we sought to reduce the risk of Type I error by replicating the findings across two independent samples and by correcting for the false discovery rate. There were some similar patterns in results across both samples, particularly with regard to sleep quality as a predictor of next-day positive affect and stressors. It is therefore less likely that the significant findings were due to chance alone. Third, one week of data was appropriate for examining associations of sleep and psychosocial experiences lagged by one day; however, there were not enough days of observation to test longer lags (i.e., consecutive nights of poor sleep or accumulated stress). Fourth, this observational study provided evidence of temporal ordering and associations, but not causal direction. Interventions to improve sleep, family life, or workplace practices would be better suited for testing causal effects. Finally, caution should be taken in generalizing these results to other samples, such as those with psychological disorders or sleep disturbances.
Conclusion
Based on over 1900 daily interviews from employees in the IT and extended care industries, daily psychosocial experiences and nightly sleep had reciprocal influences. The within-person associations—particularly for sleep quality as a predictor of next-day experiences—were replicated in two samples that differed in socioeconomic backgrounds, job characteristics, and family structure. Our results suggest the possibility that efforts to improve sleep quality may promote better mood, engender positive events, and reduce stressors across work and personal contexts. This study underscores the important bidirectional contributions of psychological and contextual factors in everyday life for sleep health.
Supplementary Material
References
- 1.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: A focus on insomnia. Sleep Med Rev. 2010 Aug;14(4):227–38. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein AN, Walker MP. The Role of Sleep in Emotional Brain Function. Annu Rev Clin Psychol. 2014;10(1):679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull. 2009 Sep;135(5):731–48. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mezick EJ, Matthews KA, Hall M, Kamarck TW, Buysse DJ, Owens JF, et al. Intra-individual variability in sleep duration and fragmentation: Associations with stress. Psychoneuroendocrinology. 2009 Oct;34(9):1346–54. doi: 10.1016/j.psyneuen.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-Individual Daily and Yearly Variability in Actigraphically Recorded Sleep Measures: the CARDIA Study. Sleep. 2007 Jun 1;30(6):793–6. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Åkerstedt T, Garefelt J, Richter A, Westerlund H, Magnusson Hanson LL, Sverke M, et al. Work and Sleep—A Prospective Study of Psychosocial Work Factors, Physical Work Factors, and Work Scheduling. SLEEP. 2015 Jul 1;38(7):1129–36. doi: 10.5665/sleep.4828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eid M, Diener E. Intraindividual variability in affect: Reliability, validity, and personality correlates. J Pers Soc Psychol. 1999;76(4):662–76. [Google Scholar]
- 8.McCrae CS, McNamara JPH, Rowe MA, Dzierzewski JM, Dirk J, Marsiske M, et al. Sleep and affect in older adults: using multilevel modeling to examine daily associations. J Sleep Res. 2008;17(1):42–53. doi: 10.1111/j.1365-2869.2008.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wild-Hartmann JA de, Wichers M, Bemmel AL van, Derom C, Thiery E, Jacobs N, et al. Day-to-day associations between subjective sleep and affect in regard to future depression in a female population-based sample. Br J Psychiatry. 2013 Jun 1;202(6):407–12. doi: 10.1192/bjp.bp.112.123794. [DOI] [PubMed] [Google Scholar]
- 10.Scott BA, Judge TA. Insomnia, Emotions, and Job Satisfaction: A Multilevel Study. J Manag. 2006 Oct 1;32(5):622–45. [Google Scholar]
- 11.Kalmbach DA, Pillai V, Roth T, Drake CL. The interplay between daily affect and sleep: a 2-week study of young women. J Sleep Res. 2014;23(6):636–45. doi: 10.1111/jsr.12190. [DOI] [PubMed] [Google Scholar]
- 12.Talbot LS, Stone S, Gruber J, Hairston IS, Eidelman P, Harvey AG. A test of the bidirectional association between sleep and mood in bipolar disorder and insomnia. J Abnorm Psychol. 2012;121(1):39–50. doi: 10.1037/a0024946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Totterdell P, Reynolds S, Parkinson B, Briner RB. Associations of sleep with everyday mood, minor symptoms and social interaction experience. Sleep. 1994 Aug;17(5):466–75. doi: 10.1093/sleep/17.5.466. [DOI] [PubMed] [Google Scholar]
- 14.Winzeler K, Voellmin A, Schäfer V, Meyer AH, Cajochen C, Wilhelm FH, et al. Daily stress, presleep arousal, and sleep in healthy young women: a daily life computerized sleep diary and actigraphy study. Sleep Med. 2014 Mar;15(3):359–66. doi: 10.1016/j.sleep.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 15.Zohar D, Tzischinsky O, Epstein R, Lavie P. The effects of sleep loss on medical residents’ emotional reactions to work events: a cognitive-energy model. Sleep. 2005 Jan;28(1):47–54. doi: 10.1093/sleep/28.1.47. [DOI] [PubMed] [Google Scholar]
- 16.Almeida DM. Resilience and Vulnerability to Daily Stressors Assessed via Diary Methods. Curr Dir Psychol Sci. 2005;14(2):64–8. [Google Scholar]
- 17.Crain TL, Hammer LB, Bodner T, Kossek EE, Moen P, Lilienthal R, et al. Work–family conflict, family-supportive supervisor behaviors (FSSB), and sleep outcomes. J Occup Health Psychol. 2014;19(2):155. doi: 10.1037/a0036010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawson KM, Davis KD, McHale SM, Hammer LB, Buxton OM. Daily positive spillover and crossover from mothers’ work to youth health. J Fam Psychol. 2014;28(6):897. doi: 10.1037/fam0000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. Am Psychol. 1989;44(3):513–24. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- 20.ten Brummelhuis LL, Bakker AB. A resource perspective on the work–home interface: The work– home resources model. Am Psychol. 2012;67(7):545–56. doi: 10.1037/a0027974. [DOI] [PubMed] [Google Scholar]
- 21.Barnes CM, Wagner DT, Ghumman S. Borrowing from Sleep to Pay Work and Family: Expanding Time?Based Conflict to the Broader Nonwork Domain. Pers Psychol. 2012;65(4):789–819. [Google Scholar]
- 22.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003 Apr;65(2):259–67. doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- 23.Burgard SA, Ailshire JA. Putting work to bed: Stressful experiences on the job and sleep quality. J Health Soc Behav. 2009 Dec;50(4):476–92. doi: 10.1177/002214650905000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkman LF, Buxton O, Ertel K, Okechukwu C. Managers’ practices related to work–family balance predict employee cardiovascular risk and sleep duration in extended care settings. J Occup Health Psychol. 2010;15(3):316–29. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garde AH, Albertsen K, Persson R, Hansen ÅM, Rugulies R. Bi-Directional Associations Between Psychological Arousal, Cortisol, and Sleep. Behav Sleep Med. 2012 Jan 1;10(1):28–40. doi: 10.1080/15402002.2012.636272. [DOI] [PubMed] [Google Scholar]
- 26.Sonnentag S, Binnewies C, Mojza EJ. “Did you have a nice evening?” A day-level study on recovery experiences, sleep, and affect. J Appl Psychol. 2008;93(3):674–84. doi: 10.1037/0021-9010.93.3.674. [DOI] [PubMed] [Google Scholar]
- 27.Uchino BN. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. J Behav Med. 2006 Jun 7;29(4):377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 28.Sin NL, Graham-Engeland JE, Almeida DM. Daily positive events and inflammation: Findings from the National Study of Daily Experiences. Brain Behav Immun. 2015;43:130–8. doi: 10.1016/j.bbi.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zautra AJ, Affleck GG, Tennen H, Reich JW, Davis MC. Dynamic approaches to emotions and stress in everyday life: Bolger and Zuckerman reloaded with positive as well as negative affects. J Pers. 2005;73(6):1511–38. doi: 10.1111/j.0022-3506.2005.00357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jain S, Mills PJ, Von Känel R, Hong S, Dimsdale JE. Effects of perceived stress and uplifts on inflammation and coagulability. Psychophysiology. 2007;44(1):154–60. doi: 10.1111/j.1469-8986.2006.00480.x. [DOI] [PubMed] [Google Scholar]
- 31.Bajaj A, John-Henderson NA, Cundiff JM, Marsland AL, Manuck SB, Kamarck TW. Daily social interactions, close relationships, and systemic inflammation in two samples: Healthy middle-aged and older adults. Brain Behav Immun. 2016 Jun 8; doi: 10.1016/j.bbi.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tomfohr L, Ancoli-Israel S, Pung MA, Natarajan L, Dimsdale JE. Uplifts and sleep. Behav Sleep Med. 2011;9(1):31–7. doi: 10.1080/15402002.2011.533992. [DOI] [PubMed] [Google Scholar]
- 33.Hobfoll SE. Conservation of Resources Theory: Its implication for stress, health, and resilience. In: Folkman S, editor. The Oxford Handbook of Stress, Health, and Coping. New York, NY: Oxford University Press; 2011. pp. 127–47. [Google Scholar]
- 34.Franzen PL, Gianaros PJ, Marsland AL, Hall MH, Siegle GJ, Dahl RE, et al. Cardiovascular reactivity to acute psychological stress following sleep deprivation. Psychosom Med. 2011 Oct;73(8):679–82. doi: 10.1097/PSY.0b013e31822ff440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoo S-S, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep—a prefrontal amygdala disconnect. Curr Biol. 2007;17(20):R877–8. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Hamilton NA, Affleck G, Tennen H, Karlson C, Luxton D, Preacher KJ, et al. Fibromyalgia: The role of sleep in affect and in negative event reactivity and recovery. Health Psychol. 2008;27(4):490–7. doi: 10.1037/0278-6133.27.4.490. [DOI] [PubMed] [Google Scholar]
- 37.Wrzus C, Wagner GG, Riediger M. Feeling good when sleeping in? Day-to-day associations between sleep duration and affective well-being differ from youth to old age. Emotion. 2014;14(3):624–8. doi: 10.1037/a0035349. [DOI] [PubMed] [Google Scholar]
- 38.Bray JW, Kelly EL, Hammer LB, Almeida DM, Dearing JW, King RB, et al. An Integrative, Multilevel, and Transdisciplinary Research Approach to Challenges of Work, Family, and Health. Methods Rep RTI Press. 2013:1–38. doi: 10.3768/rtipress.2013.mr.0024.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kossek EE, Hammer LB, Kelly EL, Moen P. Designing Work, Family & Health Organizational Change Initiatives. Organ Dyn. 2014 Jan;43(1):53–63. doi: 10.1016/j.orgdyn.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly EL, Moen P, Oakes JM, Fan W, Okechukwu C, Davis KD, et al. Changing Work and Work-Family Conflict Evidence from the Work, Family, and Health Network. Am Sociol Rev. 2014;79(3):485–516. doi: 10.1177/0003122414531435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 42.Charles ST, Luong G, Almeida DM, Ryff C, Sturm M, Love G. Fewer ups and downs: Daily stressors mediate age differences in negative affect. J Gerontol B Psychol Sci Soc Sci. 2010;65B(3):279–86. doi: 10.1093/geronb/gbq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ong AD, Exner-Cortens D, Riffin C, Steptoe A, Zautra A, Almeida DM. Linking stable and dynamic features of positive affect to sleep. Ann Behav Med. 2013;46(1):52–61. doi: 10.1007/s12160-013-9484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events: an interview-based approach for measuring daily stressors. Assessment. 2002;9(1):41–55. doi: 10.1177/1073191102091006. [DOI] [PubMed] [Google Scholar]
- 45.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 46.Snijders TA, Bosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. 2. SAGE; 2011. [Google Scholar]
- 47.Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol. 2011;62:583–619. doi: 10.1146/annurev.psych.093008.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. J Educ Behav Stat. 2000;25(1):60–83. [Google Scholar]
- 49.Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep--a study of day-to-day covariation across six weeks. Sleep Med. 2012 Jun;13(6):674–9. doi: 10.1016/j.sleep.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 50.Flueckiger L, Lieb R, Meyer AH, Witthauer C, Mata J. The importance of physical activity and sleep for affect on stressful days: Two intensive longitudinal studies. Emotion. 2016;16(4):488–97. doi: 10.1037/emo0000143. [DOI] [PubMed] [Google Scholar]
- 51.van Zundert RMP, van Roekel E, Engels RCME, Scholte RHJ. Reciprocal Associations Between Adolescents’ Night-Time Sleep and Daytime Affect and the Role of Gender and Depressive Symptoms. J Youth Adolesc. 2015;44(2):556–69. doi: 10.1007/s10964-013-0009-3. [DOI] [PubMed] [Google Scholar]
- 52.Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, et al. Association of enjoyable leisure activities with psychological and physical well-being. Psychosom Med. 2009;71(7):725. doi: 10.1097/PSY.0b013e3181ad7978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ong AD, Kim S, Young S, Steptoe A. Positive affect and sleep: A systematic review. Sleep Med Rev. 2016 Jul 25; doi: 10.1016/j.smrv.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 54.Sin NL, Moskowitz JT, Whooley MA. Positive Affect and Health Behaviors Across 5 Years in Patients With Coronary Heart Disease: The Heart and Soul Study. Psychosom Med. 2015;77(9):1058–66. doi: 10.1097/PSY.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bower B, Bylsma LM, Morris BH, Rottenberg J. Poor reported sleep quality predicts low positive affect in daily life among healthy and mood-disordered persons. J Sleep Res. 2010;19(2):323–32. doi: 10.1111/j.1365-2869.2009.00816.x. [DOI] [PubMed] [Google Scholar]
- 56.Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EL, et al. Sleep deprivation and stressors: Evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. 2012;12(5):1015–20. doi: 10.1037/a0026871. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.