Abstract
Objective
To compare patterns of objectively measured moderate-to-vigorous physical activity (MVPA, ≥3.00 METs), light-intensity PA (LPA, 1.50–2.99 METs), and sedentary behavior (SB, <1.50 METs) in successful weight loss maintainers (WLM), normal weight controls (NC), and controls with overweight/obesity (OC).
Methods
Participants (18–65 years) were recruited in three groups: WLM (maintaining ≥13.6 kg weight loss for ≥1 year, n=30), NC (BMI matched to current BMI of WLM, n=33), and OC (BMI matched to pre-weight loss BMI of WLM, n=27) and wore the activPAL™ for one week.
Results
Compared to OC and NC, WLM spent more awake time in total MVPA (WLM: 9.6±3.9%, NC: 7.1±2.1%, OC 5.9±2.0%; p<0.01) and more time in sustained (≥10 minute) bouts of MVPA (WLM 39±33, NC 17±14, OC 9±11 minutes/day; p<0.01). Compared to OC, WLM and NC spent more awake time in LPA (WLM 29.6±7.9%, NC 29.1±8.3%, OC 24.8±6.7%; p=0.04) and less awake time sedentary (WLM 60.8±9.3%, NC 63.8±9.5%, OC 69.3±7.5%; p<0.01).
Conclusion
Results provide additional data supporting the important role of MVPA in weight loss maintenance, and suggest notable differences in LPA and SB between normal weight individuals and those with overweight/obesity. Increasing LPA and/or decreasing SB may be additional potential targets for weight management interventions.
Keywords: obesity, weight loss maintenance, physical activity epidemiology, light intensity physical activity, guidelines and recommendations
Introduction
High levels of moderate-to-vigorous physical activity (MVPA) are strongly associated with successful long-term weight loss maintenance (1–4) and current guidelines recommend 300 minutes/week of moderate intensity (or 150 minutes/week of vigorous intensity) to prevent weight gain and sustain weight loss (5, 6). However, the role of light-intensity physical activity (LPA) and sedentary behavior (SB) in weight management is less clear.
LPA is defined as activities that expend low levels of energy (1.50–2.99 Metabolic Equivalents; METs). A recent study of adults with overweight/obesity in a behavioral weight loss intervention found that increases in objectively measured LPA were associated with improved short-term (6 months) and long-term (18 months) weight loss (7), suggesting an important role for LPA in weight loss maintenance that deserves further exploration.
SB is defined as activities that expend very little energy (i.e. <1.50 METs) and is typically associated with sitting, reclining, or lying during waking hours (8). On average, Americans spend ~55% of awake time (7.7 hours/day) engaged in SB (9). SB is associated with several poor health outcomes, including increased risk of obesity (10–12) and weight gain (11, 13). However, the association between objectively measured SB and weight loss maintenance has not been evaluated.
Much of what is known about long-term weight loss maintenance comes from data collected from the National Weight Control Registry (NWCR), a prospective cohort study established in 1994. Entry criteria includes maintenance of a ≥13.6 kg weight loss for ≥1 year (14). NWCR members engage in high levels of MVPA (15, 16) and spend a minimal amount of time watching television, one of the most common types of SB (17). However, patterns of LPA and SB in individuals successful at long-term weight loss maintenance have never been objectively measured or compared to individuals of normal body weight and individuals with overweight/obesity.
The primary aim of this study was to compare free-living patterns of objectively measured MVPA, LPA, and SB in successful weight loss maintainers (WLM) to normal weight controls (NC) and controls with overweight/obesity (OC). We hypothesized WLM would have higher levels of MVPA and LPA and lower levels of SB as compared to both OC and NC.
Methods
Participants
This case control study was conducted at the University of Colorado Anschutz Medical Campus and approved by the Colorado Multiple Institutional Review Board. Participants were studied between October 2009 and August 2012 to assess PA over a range of seasons.
Participants were recruited through campus flyers and email announcements. To enhance recruitment of WLM, a recruitment letter was also sent to NWCR members in the Denver Metro area. Interested individuals underwent preliminary telephone screening to determine eligibility for one of three subject groups: Weight loss maintainers (WLM, maintaining ≥13.6 kg (30 lb) weight loss for ≥1 year, current BMI 18–28 kg/m2), normal weight controls (NC, BMI 18–28 kg/m2) with no history of overweight/obesity, and controls with overweight/obesity (OC, BMI >27 kg/m2). A nested subject selection procedure achieved similar group means for age, gender, and the desired BMI matching.
Individuals meeting preliminary eligibility criteria were invited to attend an in-person screening visit. After providing informed written consent, a health history and physical exam were completed. Individuals were excluded if they had any physical or medical condition that restricted PA (including diabetes, cardiovascular disease, cancer, and significant musculoskeletal, neurologic, or psychiatric disorders), had undergone bariatric surgery, were smokers, were not weight stable (>5 kg fluctuation in body weight over past 6 months), were taking weight loss medications or other medications known to affect appetite or metabolism, or were pregnant or lactating. Weight was measured with a calibrated digital scale (to the nearest 0.2 lbs) and height with a wall-mounted stadiometer (to the nearest 0.1 cm). Waist circumference was measured using a tape measure over the iliac crests. Eligible individuals were scheduled for a one-week PA monitoring period.
Assessment of Sedentary Behavior and Physical Activity
PA patterns were assessed using the activPAL™ activity monitor (PAL Technologies, Glasgow, Scotland). The activPAL™ is a small (23×43×5 mm) and lightweight (10 grams) device that uses accelerometer-derived information about thigh position to estimate time spent sitting/lying, standing, and stepping. The device is attached to the anterior thigh and is waterproofed by wrapping it in a nitrile sleeve, allowing for 24-hour measurement. Participants were asked to wear the device continuously for seven days. Data were considered valid and used for analysis if the device was worn for >10 hours/day on ≥4 days (including ≥2 weekdays and ≥1 weekend day).
The time-stamped “event” data file from the activPAL™ software was used to determine time spent sitting/lying, standing, and stepping per day. The activPAL™ has been validated for use in adults to distinguish between sitting/lying, standing, and stepping activities (18–21). The software uses a linear regression algorithm to 1) assign MET values for sitting/lying events (1.20 METs) and standing events (1.50 METs), and 2) assign MET values for stepping events using a cadence based algorithm. Several previous studies have validated the use of step cadence against indirect calorimetry to distinguish LPA and MVPA. This methodology has been reviewed in detail by Tudor-Locke and Rowe who reported a very high correlation (r=0.93) between mean step cadence and PA intensity assessed with indirect calorimetry based on five treadmill/overground walking studies (22). Stepping events were categorized into LPA (1.50–2.99 METs) and MVPA (≥3.00 METs) using 75 steps/minute as a threshold (75 steps/minute=3.00 METs). Lyden et al. (23) have recently reported very high accuracy for activPAL™ estimates of time in PA intensity category using this methodology. To control for differences in sleep time by expressing data in terms of percent awake time, we visually inspected the events data file to estimate time into bed at night and time out of bed in the morning using methods described previously (24).
A customized R program (www.r-project.org) was used to convert the event data file to a second-by-second data file to estimate additional metrics of SB (e.g. breaks in sedentary time, average duration of sedentary bouts, etc.) and time in PA intensity category (LPA and MVPA). MET-hours were computed by multiplying the MET value for each activity by the duration it was performed (in hours). Daily MET-hours were summed to compute total MET-hours/day. Total MVPA (minutes/day) was computed as the sum of time spent in MVPA (stepping events ≥3.00 METs). To assess whether levels of MVPA met the 2008 Physical Activity Guidelines for Americans (PAG) (6), which suggest activity be accumulated in bouts ≥10 minutes, we calculated “guideline MVPA” as the sum of minutes in bouts lasting at least 10 minutes where >80% of the entire bout was spent in ≥3.00 METs (5). Guideline MVPA was calculated as a) average minutes/day (total minutes/day spent in guideline MVPA bouts), b) average minutes/week (average minutes/day in guideline MVPA multiplied by 7), and c) number of discrete guideline MVPA bouts per day. LPA (minutes/day) was computed from standing and stepping events with a MET value between 1.50–2.99 METs. The following metrics of SB were computed during time spent awake: total sedentary time (total time spent in sitting/lying events), total breaks in sedentary time (number of times a sitting/lying event was followed by a standing or stepping event), sedentary break-rate (total number of breaks per total sedentary time in hours), time (minutes/day) in sedentary bouts ≥30 and ≥60 minutes, and number of discrete sedentary bouts ≥30 and ≥60 minutes per day.
Statistical Analysis
Statistical analyses were performed with SAS (version 9.4), with the type I error rate fixed at 0.05. Fisher’s exact tests compared categorical demographic characteristics across subject groups. The Shapiro-Wilk test determined normality of outcome measures. If the Shapiro-Wilk test p<0.05, data transformations were used. A square root transformation was used for minutes/day in guideline MVPA, percent of hours awake worn in LPA, total breaks in sedentary time, minutes/day in sedentary bouts ≥60 minutes, and number of sedentary bouts ≥30 minutes. A log transformation was used for guideline MVPA bouts, minutes/week in guideline MVPA, and break-rate. A Kruskal-Wallis test compared number of weekend and weekdays worn across subject group. For all other variables, one-way analysis of variance (ANOVA) examined the null hypothesis that samples in subject groups are drawn from populations with the same mean values. Omnibus F-test p-value is reported, followed by between subject group comparisons. Results are presented as mean ± SD unless otherwise stated. PA behavior was compared both in absolute minutes per day and as percent awake time (to account for differences in sleep time). A Pearson’s correlation coefficient examined correlations between total MVPA, LPA, sedentary time, and steps within subject group. Results were not corrected for multiple comparisons because we were not concerned with the universal null hypothesis that subject groups were identical on all variables (25). There was no a-priori power analysis for the outcomes variables in this secondary analysis. A sensitivity analysis was performed to ensure that seasonality during time of PA assessment did not impact between-group differences in PA patterns.
Results
Study Enrollment and Subject Characteristics
114 participants were screened, and 106 completed the study (Figure 1). 14 participants were missing data due to device malfunction or incorrect device placement and 2 participants did not meet valid monitoring period criteria (Figure 1), resulting in a final sample size of 90 participants (30 WLM, 33 NC, 27 OC). Groups were similar in regards to age, sex, and ethnicity (Table 1). Current BMI of WLM (23.7±2.4 kg/m2) was well matched to NC (22.7±2.0 kg/m2, p=0.22). Current BMI of OC (33.4±5.1 kg/m2) was well matched to the pre-weight loss maximum BMI of WLM (32.8±4.9 kg/m2, p=0.84). WLM were maintaining a weight loss of 26.3±11.6 kg for 9.5±10.2 years.
Figure 1.
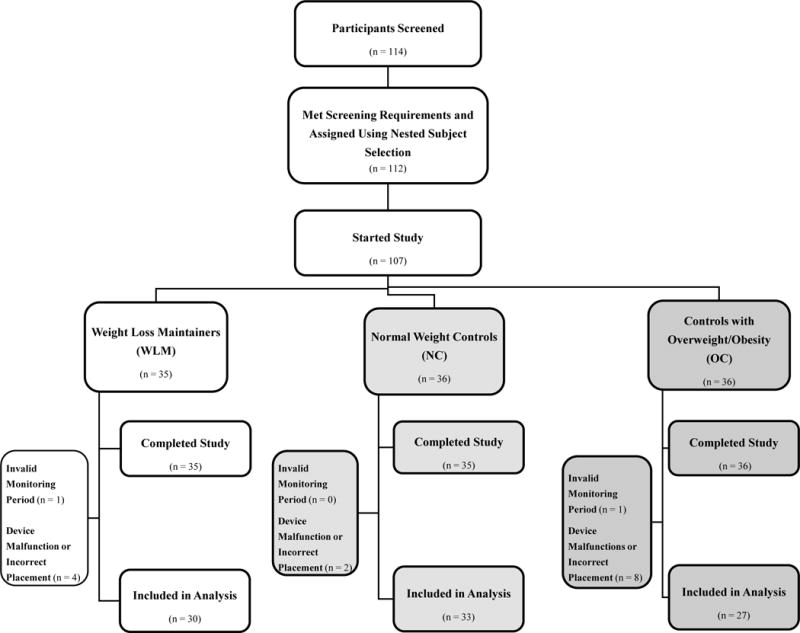
Study Enrollment
Table 1.
Baseline Characteristics of Study Participantsa
| Characteristic | WLM (n = 30) |
NC (n = 33) |
OC (n = 27) |
Overall p-value |
|---|---|---|---|---|
| Age (y) [Mean ± SD] | 44.8 ± 11.8 | 46.8 ± 13.8 | 47.1 ± 11.0 | 0.74 |
|
| ||||
| Anthropometric Measures [Mean ± SD] | ||||
| Weight (kg) | 68.1 ± 11.0b | 64.1 ± 11.0 | 93.2 ± 18.7 | <0.01 |
| Height (cm) | 169.0 ± 9.1 | 167.4 ± 9.8 | 166.6 ± 8.7 | 0.61 |
| BMI (kg/m2) | 23.7 ± 2.4b | 22.7 ± 2.0b | 33.4 ± 5.1 | <0.01 |
| Waist Circumference (cm) | 83.1 ± 7.3b | 82.6 ± 7.1b | 112.2 ± 39.7 | <0.01 |
| Maximum Weight (kg)d | 93.7 ± 15.9c | 68.5 ± 11.8b | 99.5 ± 21.9 | <0.01 |
| Minimum Weight (kg)e | 63.3 ± 11.3c | 57.2 ± 9.9b | 65.4 ± 15.3 | 0.03 |
| Maximum BMI (kg/m2) | 32.8 ± 4.9b, c | 24.3 ± 2.1b | 35.6 ± 6.1 | <0.01 |
| Maximum Weight Ever Lost (kg) | 26.3 ± 11.6b, c | 6.1 ± 5.1b | 12.2 ± 8.2 | <0.01 |
| Weight Loss Maintenance Duration (y) | 9.5 ± 10.2 | n/a | n/a | n/a |
|
| ||||
| Sex, Male [n, (%)] | 8 (27%) | 9 (27%) | 4 (15%) | 0.47 |
|
| ||||
| Ethnicity [n, (%)] | 0.13 | |||
| Hispanic/Latino | 0 (0%) | 4 (12%) | 3 (11%) | |
| Not Hispanic/Latino | 30 (100%) | 29 (88%) | 24 (89%) | |
|
| ||||
| Race [n, (%)] | 0.03 | |||
| White | 30 (100%) | 29 (88%) | 23 (85%) | |
| Black/African American | 0 (0%) | 1 (3%) | 4 (15%) | |
| Asian | 0 (0%) | 2 (6%) | 0 (0%) | |
| Not Reported | 0 (0%) | 1 (3%) | 0 (0%) | |
Fisher’s Exact Test used for categorical variables; Continuous variables analyzed using one-way ANOVA. Significant p values (alpha <0.05) indicated in bold. Body Mass Index (BMI); Weight Loss Maintainers (WLM); Normal Weight Controls (NC); Controls with Overweight/Obesity (OC).
Significantly different from OC (p<0.05).
Significantly different from NC (p<0.05).
Excluding pregnancy.
After age 18 and excluding illness.
Wear Time and Sleep Parameters
Median number of weekend days (2 days) and weekdays (4 days) worn, mean sleep time (8 hours), and mean wake time (16 hours) were similar across groups. There was a non-significant trend for longer sleep time in OC as compared to WLM and NC (Table 2). Thus, PA behavior was expressed both in absolute minutes/day and as percent awake time. WLM were more likely to be assessed in the Spring/Summer versus Fall/Winter the seasons as compared to NC and OC (see Supplementary Information, Table S1). There was no difference in PA behavior within subject group between Spring/Summer vs. Fall/Winter seasons (Table S2). In addition, when seasonality was added to the ANOVA model for total MVPA, guideline MVPA, LPA, sedentary time, and steps, results did not change (Table S3).
Table 2.
Comparison of activPAL™ Parameters (Mean ± SD) across Subject Groupa
| ictivPAL™ Parameter | WLM (n=30) |
NC (n=33) |
OC (n=27) |
p-value, Omnibus F test | p-value, WLM:NC | p-value, WLM:OC | p-value, NC:OC |
|---|---|---|---|---|---|---|---|
| Wear Time and Sleep | |||||||
| Sleep Time (hours/day) | 7.7 ± 1.5 | 7.9 ± 1.1 | 8.3 ± 1.3 | 0.21 | 0.49 | 0.08 | 0.25 |
| Wake Time (hours/day) | 16.3 ± 1.5 | 16.1 ± 1.1 | 15.7 ± 1.3 | 0.21 | 0.49 | 0.08 | 0.25 |
|
| |||||||
| MVPA and LPA | |||||||
| Total MVPA (min/day) | 95 ± 40 | 69 ± 20 | 56 ± 20 | <0.01 | <0.01 | <0.01 | 0.07 |
| Total MVPA (% hours awake worn) | 9.6 ± 3.9 | 7.1 ± 2.1 | 5.9 ± 2.0 | <0.01 | <0.01 | <0.01 | 0.09 |
| Guideline MVPA (min/day)b | 39 ± 33 | 17 ± 14 | 9 ± 11 | <0.01 | <0.01 | <0.01 | 0.04 |
| Guideline MVPA (min/week) | 272 ± 234 | 117 ± 100 | 63 ± 76 | <0.01 | 0.01 | <0.01 | 0.18 |
| Guideline MVPA Bouts (count/day)c | 1.4 ± 1.2 | 0.7 ± 0.6 | 0.4 ± 0.5 | <0.01 | 0.01 | <0.01 | 0.12 |
| MET-Hours/day | 26.2 ± 3.3 | 24.7 ± 2.0 | 23.3 ± 2.2 | <0.01 | 0.02 | <0.01 | 0.03 |
| LPA (min/day) | 290 ± 82 | 281 ± 85 | 234 ± 68 | 0.02 | 0.68 | 0.01 | 0.02 |
| LPA (% hours awake worn)b | 29.6 ± 7.9 | 29.1 ± 8.3 | 24.8 ± 6.7 | 0.04 | 0.79 | 0.02 | 0.03 |
|
| |||||||
| Sedentary Behavior | |||||||
| Sedentary Time (min/day) | 596 ± 105 | 617 ± 102 | 654 ± 79 | 0.08 | 0.40 | 0.03 | 0.14 |
| Sedentary Time (% of hours awake worn) | 60.8 ± 9.3 | 63.8 ± 9.5 | 69.3 ± 7.5 | <0.01 | 0.19 | <0.01 | 0.02 |
| Sedentary Bouts ≥30 min (min/day) | 300 ± 99 | 309 ± 111 | 346 ± 93 | 0.20 | 0.73 | 0.09 | 0.16 |
| Sedentary Bouts ≥30 min (count/day)b | 5.3 ± 1.8 | 5.3 ± 1.5 | 6.1 ± 1.4 | 0.08 | 0.86 | 0.04 | 0.06 |
| Sedentary Bouts ≥60 min (min/day)b | 143 ± 68 | 154 ± 89 | 169 ± 80 | 0.50 | 0.78 | 0.26 | 0.34 |
| Sedentary Bouts ≥60 min (count/day) | 1.5 ± 0.7 | 1.6 ± 0.7 | 1.8 ± 0.8 | 0.24 | 0.88 | 0.13 | 0.16 |
| Sedentary Breaks (count/day)b | 57.6 ± 13.1 | 58.0 ± 11.0 | 52.1 ± 10.9 | 0.11 | 0.84 | 0.09 | 0.05 |
| Sedentary Break-rate (break count/sedentary time in hours)c | 6.08 ± 2.21 | 5.74 ± 1.17 | 4.84 ± 1.14 | 0.01 | 0.75 | 0.01 | 0.01 |
|
| |||||||
| Postural Allocation and Steps | |||||||
| Standing Time (min/day) | 249 ± 73 | 245 ± 78 | 205 ± 63 | 0.04 | 0.82 | 0.02 | 0.03 |
| Stepping Time (min/day) | 135 ± 48 | 105 ± 28 | 85 ± 25 | <0.01 | <0.01 | <0.01 | 0.03 |
| Steps (count/day) | 12,256 ± 5,095 | 9,047 ± 2,703 | 7,072 ± 2,346 | <0.01 | <0.01 | <0.01 | 0.04 |
Results from one-way ANOVA. Significant p values (alpha <0.05) indicated in bold. Weight Loss Maintainers (WLM); Normal Weight Controls (NC); Controls with Overweight/Obesity (OC). Light-Intensity-Physical Activity (LPA); Moderate-to-Vigorous Intensity Physical Activity (MVPA).
Results from one-way ANOVA using a square root transformation, but data presented using untransformed mean ± SD.
Results from one-way ANOVA using a log transformation, but data presented using untransformed mean ± SD.
MVPA
Compared to NC and OC, WLM spent more time in total and guideline MVPA, engaged in more bouts of guideline MVPA, accumulated more MET-hours of PA (Table 2), and spent a greater percent of time awake in MVPA (Figure 2). Extrapolating to a 1-week period for comparison to current PA guidelines, WLM engaged in more minutes/week of guideline MVPA compared to NC and OC (WLM: 272±234, NC: 117±100, OC: 63±76 minutes/week; Table 2).
Figure 2.
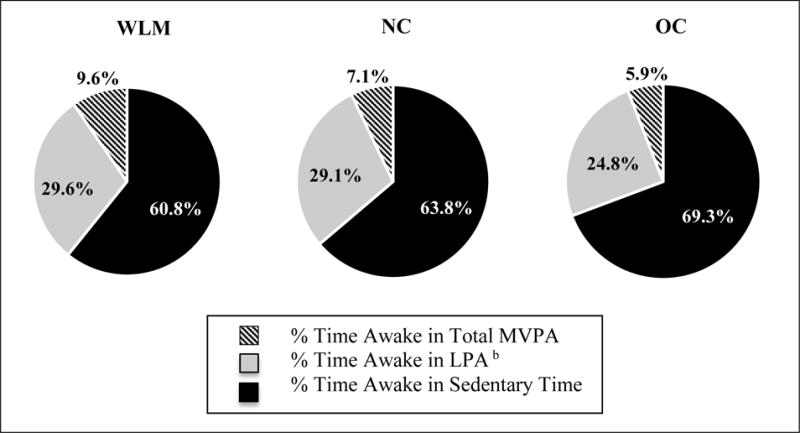
Proportion of Awake Time Spent in SB, LPA, and Total MVPA across Subject Groupa
aResults from one-way ANOVA reported; total n=90 (WLM: 30, NC: 33, OC: 27).
bResults from one-way ANOVA using a square root transformation, but data presented using untransformed mean ± SD.
LPA
WLM and NC spent more total time in LPA (WLM: 290±82, NC: 281±85, OC: 234±68 minutes/day; Table 2) and spent more percent time awake in LPA as compared to OC (~30% vs. ~25%, respectively) (Figure 2).
Sedentary Behavior
Both WLM and NC spent less percent time awake sedentary (Table 2, Figure 2) and had a higher sedentary break rate as compared to OC (Table 2). There was a trend for a between-group difference across subject groups in total sedentary time (WLM: 596±105, NC: 617±102, OC: 654±79 minutes/day) and number of sedentary bouts ≥30 minutes/day, with WLM and NC having a lower number of bouts ≥30 minutes/day compared to OC (Table 2). There were no between-group differences in any other SB metrics.
Postural Allocation and Steps
Compared to OC, both WLM and NC spent more minutes standing per day. Compared to both NC and OC, WLM spent more time stepping and achieved more average steps per day (Table 2).
Correlations between Physical Activity and Sedentary Time Categories
Sedentary time and LPA were negatively correlated within all subject groups. Steps and total MVPA were strongly positively correlated within all subject groups. Within NC, but not WLM or OC, LPA was positively (and sedentary time was negatively) correlated with total MVPA and steps (Table 3). In all groups combined, LPA was positively correlated (and sedentary time was negatively correlated) with total MVPA (LPA: r=0.36 versus sedentary time: r=−0.36), and steps (LPA: r=0.40 versus sedentary time: r=−0.39) and negatively correlated with sedentary time (r=−0.69), with all correlations significant at p<0.05 (data not shown).
Table 3.
Correlations between Physical Activity, Sedentary Time, and Steps Within Subject Groupsa
| Total MVPA (min/day) |
LPA (min/day) |
Sedentary Time (min/day) |
Steps (count/day) |
|
|---|---|---|---|---|
|
| ||||
| WLM | ||||
| Total MVPA (min/day) | 1.00 | 0.228 (p=0.23) | −0.205 (p=0.28) | 0.99 (p<0.01) |
| LPA (min/day) | 0.228 (p=0.23) | 1.00 | −0.630 (p<0.01) | 0.26 (p=0.16) |
| Sedentary Time (min/day) | −0.205 (p=0.28) | −0.630 (p<0.01) | 1.00 | −0.25 (0.17) |
| Steps (count/day) | 0.99 (p<0.01) | 0.26 (p=0.16) | −0.25 (0.17) | 1.00 |
| NC | ||||
| Total MVPA (min/day) | 1.00 | 0.517 (p<0.01) | −0.542 (p<0.01) | 0.99 (p<0.01) |
| LPA (min/day) | 0.517 (p<0.01) | 1.00 | −0.766 (p<0.01) | 0.49 (p<0.01) |
| Sedentary Time (min/day) | −0.542 (p<0.01) | −0.766 (p<0.01) | 1.00 | −0.53 (p<0.01) |
| Steps (count/day) | 0.99 (p<0.01) | 0.49 (p<0.01) | −0.53 (p<0.01) | 1.00 |
| OC | ||||
| Total MVPA (min/day) | 1.00 | 0.333 (p=0.09) | −0.233 (p=0.24) | 0.99 (p<0.01) |
| LPA (min/day) | 0.333 (p=0.09) | 1.00 | −0.531 (p<0.01) | 0.36 (p=0.07) |
| Sedentary Time (min/day) | −0.233 (p=0.24) | −0.531 (p<0.01) | 1.00 | −0.27 (p=0.17) |
| Steps (count/day) | 0.99 (p<0.01) | 0.36 (p=0.07) | −0.27 (p=0.17) | 1.00 |
Results from Pearson Correlation with significant r and p values (alpha <0.05) indicated in bold. Weight Loss Maintainers (WLM); Normal Weight Controls (NC); Controls with Overweight/Obesity (OC). Light-Intensity Physical Activity (LPA); Moderate-to-Vigorous Intensity Physical Activity (MVPA).
Discussion
This study is the first to objectively assess multiple components of free-living activity behavior (MVPA, LPA, SB, postural allocation, and steps) in successful weight loss maintainers (WLM), as compared to individuals with normal body weight (NC) and individuals with overweight/obesity (OC). Consistent with previous studies, our results suggest that successful WLM achieve higher levels of MVPA as compared to non-weight reduced individuals (NC and OC). We also show that individuals of normal body weight (NC and WLM) achieve higher levels of LPA and lower levels of SB as compared to individuals with overweight/obesity (OC), suggesting that increasing LPA and/or decreasing SB may be additional potential targets for weight management interventions.
WLM engaged in two-fold greater minutes/day of guideline MVPA as compared to NC and four-fold greater minutes/day of guideline MVPA as compared to OC. Differences between subject groups in total MVPA appear to have been driven primarily by differences in minutes of guideline MVPA as we have observed previously (15). Results from the current study confirm results from previous observational studies (15, 16, 26–29) as well as previous randomized trials reporting on the association between MVPA and long-term (18 month) weight loss (7, 30–32). Furthermore, these results are consistent with a previous study by our group (15) that compared MVPA (assessed with the RT3 accelerometer) in a sample of WLM (n=26) to NC (n=30) and OC (n=34) studied from 2004–2006. Time spent in guideline MVPA by subject group observed in that study (15) shows a similar pattern to the results we observed in the current study using the activPAL™, with WLM spending the most time of the three groups in guideline MVPA, followed by NC, and then OC. Taken together, these results suggest WLM may require higher levels of guideline MVPA to maintain a normal body weight after weight loss as compared to non-reduced individuals, as has been previously suggested (15, 16, 31).
We also observed higher levels of LPA and lower levels of SB in individuals maintaining a normal body weight (both NC and WLM) as compared to individuals with overweight/obesity (OC), which may have important implications for prevention of weight gain (primary prevention) or prevention of weight regain after weight loss (secondary prevention). On average, WLM were engaging in ~56 minutes/day more LPA and ~58 minutes/day less sedentary time as compared to OC. NC were engaging in ~47 minutes/day more LPA and ~38 minutes/day less sedentary time as compared to OC. There was an inverse correlation between time spent sedentary and time spent in LPA. Individuals with higher LPA had lower levels of sedentary time (overall r=−0.686, p<0.01), qualitatively similar (although less strong) to correlations reported in Healy et al. (r=−0.96) (33).
Our results regarding SB are consistent with prior observational data (11, 12, 34), which suggest a potential role for reducing SB to support body weight regulation. For example, a cross-sectional study of 1,422 NWCR members provided evidence that avoidance of watching television (the most common type of SB) was associated with successful weight loss maintenance, independent of self-reported MVPA (17). Our results regarding LPA are novel, as there is currently limited epidemiological evidence on the association between LPA and body weight. To our knowledge, only one other study has evaluated the association between objectively measured LPA and weight loss maintenance. Jakicic et al. (7) examined data from 260 women with overweight/obesity enrolled in an 18-month behavioral weight loss program and found that those who achieved 10% weight loss at 18 months demonstrated greater increases in objectively measured LPA. While these findings are intriguing, it is not clear whether higher levels of LPA and lower levels of SB are protective against weight gain or whether weight gain causes LPA to decrease and SB to increase.
WLM accumulated the most steps/day and spent the most time stepping, followed by NC, and then OC, suggesting that achieving a high number of steps/day may play an important role in the prevention of weight gain and weight regain after weight loss. Our results are consistent with Nakata et al. (35) who found that individuals in the highest quartile of weight loss 2 years after a 6-month intervention significantly increased their step count (by ~2,607 steps/day) compared to the lowest quartile of weight loss. In addition WLM and NC spent ~1.2 fold greater minutes/day standing as compared to OC, suggesting that increasing time spent standing may help individuals maintain a normal body weight. Furthermore, in the Nurses’ Health Study (11), time spent standing or walking at home was associated with a 23% lower risk of obesity (p<0.01). Breaking up sedentary time by increasing time spent standing and stepping may be an important additional recommendation for individuals seeking weight management. As Healy et al. (36) suggest, even activities as minimal as standing, rather than sitting, have been shown to result in substantial increases in total daily energy expenditure.
It is important to recognize that relative differences in MVPA between groups in our study were more dramatic than relative differences in LPA or SB, suggesting that the observed differences in MVPA are likely to play a larger role in weight loss maintenance compared to LPA. For example, when comparing WLM to OC, the relative between-group differences in total MVPA (~70%) were much higher than the relative between-group differences in LPA (~24%) or sedentary time (~9%). The estimated energetic effect of the additional 56 minutes/day of total LPA observed in WLM as compared to OC (56 minutes/day × LPA MET range of 1.50–2.99 METs = 84–167 MET-minutes/day) is generally less than the estimated energetic effect of the additional 39 minutes of total MVPA observed in WLM as compared to OC (39 minutes × MVPA MET range of 3.0–10.0 METs = 117–390 MET-minutes/day). However, the calculated ranges demonstrate that the exact energetic benefits depend on the mean intensity of the LPA and MVPA performed.
While the energetic benefits of increasing MVPA are greater than an equivalent increase in duration of LPA, these benefits will not be accrued unless individuals actually achieve and sustain higher levels of MVPA. Increasing MVPA is a goal that is difficult for many adults with overweight/obesity to achieve, even when supported by a behavioral weight loss program (31, 32). Interventions to increase LPA and/or decrease SB may be more practical and universal across different settings (including home and the workplace), and may be more acceptable. Thus, interventions to increase LPA and/or decrease SB may ultimately promote greater energetic benefits than interventions designed to increase MVPA due to a greater level of adherence. Increasing LPA and/or decreasing SB may provide additional health benefits and contribute to weight management due to the cumulative energetic effects of LPA accrued throughout the day as well as the metabolic benefits that may occur with reductions in sedentary time (36). A recent study concluded that in a group of sedentary adults, minimal intensity PA (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of MVPA when energy expenditure is comparable (37), indicating that LPA may play a larger role in metabolic health than previously thought. An uncontrolled, observational study found that in participants with overweight/obesity who completed a behavioral weight loss program (mean±SD weight loss 6.7±8.7 kg), enrollment in a 6-month fitness program focused on increasing both light-intensity (gardening, light housework) and moderate-intensity PA (walking), limited weight regain (38), indicating that the addition of LPA to MVPA recommendations may help promote long-term weight loss maintenance. Owen et al. noted that, “Every minute of sedentary time replaced with LPA would expend 1 additional kilocalorie (calculated assuming 1.50 vs. 2.30 METs for a person weighing 72 kg),” revealing the potential for several health improvements with a recommendation such as this (36, 39). As suggested first by Healy et al. (40), replacing SB with LPA may be a successful, additional approach to improving weight management. A practicable recommendation may be to replace one hour of SB with one hour of LPA every day. However, well-designed, prospective, interventional trials are needed to evaluate the effectiveness of interventions to increase LPA and/or decrease SB (in addition to or instead of meeting current guidelines for MVPA) during weight loss/weight loss maintenance to better understand the effectiveness of these recommendations as a weight management strategy.
Our study has some limitations. Because of the observational study design, we were unable to assess causality. Increasing MVPA and LPA and decreasing SB may be behavioral strategies that aid in maintaining a normal body weight. However, reverse causality may exist – as people gain weight, they may become less active (and more sedentary) because activity becomes more difficult. It is possible that the intensity of some activities was misclassified by the activPAL™ cadence based algorithm. Our study results may not be generalizable as our study population is relatively small, predominantly female (77%), white (91%), and non-Hispanic/Latino (92%). However, 24-hour objective assessment of multiple components of free-living activity allowed us to detect important distinctions in patterns of activity between successful weight loss maintainers, normal weight individuals, and individuals with overweight/obesity, a novel aspect of our study.
Conclusion
We observed significantly higher levels of MVPA in individuals maintaining a weight loss (WLM) as compared to non-weight reduced individuals (NC and OC), providing additional objective data to suggest that weight-reduced individuals may require a greater level of MVPA to maintain a normal body weight than individuals not maintaining a weight loss. Our results also suggest that individuals of a normal body weight (WLM and NC) engage in significantly more LPA and less SB as compared to their counterparts with overweight/obesity (OC). While the energetic benefits of increasing MVPA are likely greater than increasing LPA, current intervention current strategies to increase MVPA are only modestly successful. Increasing LPA and/or decreasing SB may be additional potential targets for weight management interventions and should be tested in prospective studies.
Supplementary Material
STUDY IMPORTANCE QUESTIONS.
What is already known about this subject?
High levels of moderate-to-vigorous intensity physical activity (MVPA, ≥3.00 METs) are strongly correlated with successful long-term weight loss maintenance.
The association between objectively measured sedentary behavior (SB, <1.50 METs), and light-intensity physical activity (LPA, 1.50–2.99 METs) with body weight is less clear.
What does your study add?
This study is the first to objectively assess multiple components of free-living activity behavior (MVPA, LPA, SB, postural allocation, and steps) in successful weight loss maintainers, as compared to individuals with normal body weight and individuals with overweight/obesity.
We observed significantly higher levels of MVPA in individuals maintaining a weight loss (WLM) as compared to non-weight reduced individuals (NC and OC), providing additional objective data to suggest that weight-reduced individuals may require a greater level of MVPA to maintain a normal body weight than individuals not maintaining a weight loss.
The observed patterns of LPA and SB in this study suggest that both individuals successful at weight loss maintenance and individuals maintaining a normal body weight spend significantly more awake time in LPA and significantly less awake time sedentary compared to individuals with overweight/obesity.
Acknowledgments
We would like to thank all of our study participants as well as Dr. Rena Wing for providing access to the NWCR to assist with recruitment of study participants.
FUNDING: This work was supported by grants from the National Institutes of Health: NIH K23 DK078913, P30 DK048520, and NIH UL1 TR001082 as well as the American Heart Association: AHA 16PRE29660012.
Footnotes
DISCLOSURE: KL is currently a consultant for PAL Technologies, the company that manufactures the activPAL™ device. JO and HW report stock options from Retrofit, and are partners in Shakabuku LLC, companies who provide weight management services, outside the submitted work; JO and HW have been issued a patent on the “Energy Gap”. HW accepts personal fees as an advisory board member for Atkins, a low-carbohydrate weight loss program.
AUTHOR CONTRIBUTIONS: VC, HW, and JH conceived of and designed the study. VC, HW, and JH obtained funding. VC wrote the protocol and acquired the data. KL cleaned and identified additional activity metrics with the activPAL™ data. ZP and DO performed the statistical analysis. DO, KL, ZP, JH, EM, and VC interpreted the data. DO and VC drafted the manuscript. DO generated tables and figures. All authors were involved in writing and revising the manuscript and approved the final version of the manuscript.
Supporting Information
We have provided supporting information about our sensitivity analysis to examine whether seasonality impacted physical activity (PA) behavior in our study. We categorized March-August into the Spring/Summer season and September-February into the Fall/Winter season based on season categories for Denver, CO (1). Weight loss maintainers (WLM) were more likely to have PA behavior assess in the Spring/Summer seasons versus Fall/Winter as compared to normal weight controls (NC) and controls with overweight/obesity (OC) based on results from a Chi-Square test (p=0.01; see Table S1). However, there was no difference in total MVPA (minutes/day), guideline MVPA (minutes/day), LPA (minutes/day), sedentary time (minutes/day), or steps (count/day) in the Spring/Summer season as compared to the Fall/Winter season within each group, based on a two-samples t-test (p>0.05; see Table S2). In addition, when seasonality was added to the ANOVA model for total MVPA, guideline MVPA, LPA, sedentary time, and steps, results did not change (see Table S3). Therefore, we are not concerned that seasonality impacted PA behavior in this analysis.
References
- 1.Catenacci VA, Wyatt HR. The role of physical activity in producing and maintaining weight loss. Nature clinical practice. Endocrinology & metabolism. 2007;3(7):518–529. doi: 10.1038/ncpendmet0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jakicic JM. The effect of physical activity on body weight. Obesity. 2009;17(Suppl 3):S34–38. doi: 10.1038/oby.2009.386. [DOI] [PubMed] [Google Scholar]
- 3.Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1997;21(10):941–947. doi: 10.1038/sj.ijo.0800499. [DOI] [PubMed] [Google Scholar]
- 4.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Progress in cardiovascular diseases. 2014;56(4):441–447. doi: 10.1016/j.pcad.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acsm’s guidelines for exercise testing and prescription. Wolters Kluwer/Lippincott Willams & Wilkins Health; 2014. p. 456. [Google Scholar]
- 6.Services. USDoHaH. 2008 physical activity guidelines for americans: Be active, health and happy! Services HaH. ix. Washington, DC: U.S Dept of Heath and Human Services; 2008. p. 61. [Google Scholar]
- 7.Jakicic JM, Tate DF, Lang W, et al. Objective physical activity and weight loss in adults: The step-up randomized clinical trial. Obesity. 2014;22(11):2284–2292. doi: 10.1002/oby.20830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: The population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the united states, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids. 2003;38(2):103–108. doi: 10.1007/s11745-003-1038-4. Epub 2003/05/08. [DOI] [PubMed] [Google Scholar]
- 11.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. Jama. 2003;289(14):1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 12.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. American journal of preventive medicine. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Chaput JP, Klingenberg L, Astrup A, Sjodin AM. Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12(5):e12–20. doi: 10.1111/j.1467-789X.2010.00772.x. [DOI] [PubMed] [Google Scholar]
- 14.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. The American journal of clinical nutrition. 1997;66(2):239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 15.Catenacci VA, Grunwald GK, Ingebrigtsen JP, et al. Physical activity patterns using accelerometry in the national weight control registry. Obesity. 2011;19(6):1163–1170. doi: 10.1038/oby.2010.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phelan S, Roberts M, Lang W, Wing RR. Empirical evaluation of physical activity recommendations for weight control in women. Medicine and science in sports and exercise. 2007;39(10):1832–1836. doi: 10.1249/mss.0b013e31812383c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raynor DA, Phelan S, Hill JO, Wing RR. Television viewing and long-term weight maintenance: Results from the national weight control registry. Obesity. 2006;14(10):1816–1824. doi: 10.1038/oby.2006.209. [DOI] [PubMed] [Google Scholar]
- 18.Godfrey A, Culhane KM, Lyons GM. Comparison of the performance of the activpal professional physical activity logger to a discrete accelerometer-based activity monitor. Med Eng Phys. 2007;29(8):930–934. doi: 10.1016/j.medengphy.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40(12):992–997. doi: 10.1136/bjsm.2006.030262. Epub 2006/09/19. doi: bjsm.2006.030262 [pii] 10.1136/bjsm.2006.030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Medicine and science in sports and exercise. 2011;43(8):1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 21.Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40(9):779–784. doi: 10.1136/bjsm.2006.027276. Epub 2006/07/11. doi: bjsm.2006.027276 [pii] 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tudor-Locke C, Rowe DA. Using cadence to study free-living ambulatory behaviour. Sports medicine. 2012;42(5):381–398. doi: 10.2165/11599170-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Lyden K, Keadle SK, Staudenmayer J, Freedson PS. The activpal tm accurately classifies activity intensity categories in healthy adults. Medicine and science in sports and exercise. 2016 doi: 10.1249/MSS.0000000000001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Berg JD, Willems PJ, van der Velde JH, et al. Identifying waking time in 24-h accelerometry data in adults using an automated algorithm. J Sports Sci. 2016;34(19):1867–1873. doi: 10.1080/02640414.2016.1140908. [DOI] [PubMed] [Google Scholar]
- 25.Perneger TV. What’s wrong with bonferroni adjustments. Bmj. 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGuire MT, Wing RR, Klem ML, Hill JO. Behavioral strategies of individuals who have maintained long-term weight losses. Obesity research. 1999;7(4):334–341. doi: 10.1002/j.1550-8528.1999.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 27.Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the national weight control registry. American journal of preventive medicine. 2014;46(1):17–23. doi: 10.1016/j.amepre.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 28.Weinsier RL, Hunter GR, Desmond RA, Byrne NM, Zuckerman PA, Darnell BE. Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight. The American journal of clinical nutrition. 2002;75(3):499–504. doi: 10.1093/ajcn/75.3.499. [DOI] [PubMed] [Google Scholar]
- 29.Westerterp KR, Plasqui G. Physically active lifestyle does not decrease the risk of fattening. PLoS One. 2009;4(3):e4745. doi: 10.1371/journal.pone.0004745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women: A randomized trial. Jama. 2003;290(10):1323–1330. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- 31.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Archives of internal medicine. 2008;168(14):1550–1559. doi: 10.1001/archinte.168.14.1550. discussion 1559–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? The American journal of clinical nutrition. 2007;85(4):954–959. doi: 10.1093/ajcn/85.4.954. [DOI] [PubMed] [Google Scholar]
- 33.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: The australian diabetes, obesity and lifestyle study (ausdiab) Diabetes care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 34.Healy GN, Winkler EAH, Brakenridge CL, Reeves MM, Eakin EG. Accelerometer-derived sedentary and physical activity time in overweight/obese adults with type 2 diabetes: Cross-sectional associations with cardiometabolic biomarkers. Plos One. 2015;10(3) doi: 10.1371/journal.pone.0119140. ARTN e0119140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakata Y, Okada M, Hashimoto K, Harada Y, Sone H, Tanaka K. Weight loss maintenance for 2 years after a 6-month randomised controlled trial comparing education-only and group-based support in japanese adults. Obesity facts. 2014;7(6):376–387. doi: 10.1159/000369913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes care. 2008;31(4):661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 37.Duvivier BMFM, Schaper NC, Bremers MA, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. Plos One. 2013;8(2) doi: 10.1371/journal.pone.0055542. ARTN e55542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villanova N, Pasqui F, Burzacchini S, et al. A physical activity program to reinforce weight maintenance following a behavior program in overweight/obese subjects. International journal of obesity. 2006;30(4):697–703. doi: 10.1038/sj.ijo.0803185. [DOI] [PubMed] [Google Scholar]
- 39.Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: Emerging evidence for a new health risk. Mayo Clin Proc. 2010;85(12):1138–1141. doi: 10.4065/mcp.2010.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes care. 2007;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


