Abstract
Objective
Because of the poor prognosis of ovarian cancer and concomitant distress, understanding contributors to positive well-being is critical. This study examines spiritual growth as a domain of posttraumatic growth and its contribution to longitudinal emotional outcomes in ovarian cancer.
Methods
Ovarian cancer patients (N=241) completed measures assessing spirituality (FACIT-SP-12; subscales: faith, meaning, and peace), depression (CESD), cancer-specific anxiety (IES), and total mood disturbance (TMD: POMS) prior to surgery and one-year post-surgery. Stressful life events in the year after diagnosis were measured at one-year post-surgery. Regressions examined the association between changes in spirituality and depression, anxiety, and TMD at one-year post surgery. Additionally, spiritual change was examined as a moderator of the effect of recent life events on mood.
Results
Increases in peace were related to lower depression (β=−.40, p<.001), anxiety (β= −.20, p=.004), and TMD (β= −.41, p<.001) at one-year. Changes in meaning and faith were unrelated to all outcomes. Additionally, changes in peace moderated the effect of stressful life events on depression (β= −.14, p=.027), anxiety (β= −.16, p=.05), and TMD (β= −.17, p=.01), such that those with a high number of life events paired with a decrease in peace experienced the worst psychological outcomes at one-year.
Conclusion
These findings suggest that the quality of peace may be the most adaptive facet of spiritual growth in cancer patients. Furthermore, changes in peace appear to moderate the effect of life events on psychological well-being.
Keywords: Ovarian cancer, spiritual well-being, posttraumatic growth, psycho-oncology, psychological adjustment
Introduction
Diagnosis and treatment of ovarian cancer often presents physical and emotional challenges, frequently leading to elevated levels of depression and anxiety compared to the general population.1 However, despite the frequency of distress in cancer survivors, a diagnosis of cancer can also have positive consequences, termed posttraumatic growth (PTG).2 Cancer survivors often report growth in several domains, including relationships, life goals/priorities, and sense of self, most often in the year after cancer diagnosis.3,4 PTG has predominantly been associated with lower depression and greater well-being,5 although not all studies are consistent.6
One commonly reported domain of PTG is spirituality, which can include both existential and religious elements.7,8 Many spiritual belief systems maintain that suffering can be transformative and help people make meaning out of their circumstances,9 with subsequent changes to one’s world view, goals and priorities, sense of self, and relationships.10 In the current paper, we examine longitudinal changes in spirituality as an indicator of PTG, where decreases in a sense of spirituality will be referred to as “spiritual decline,”10 while increases represent “spiritual growth.”
The construct of spirituality has been conceptualized as comprised of three components: meaning, peace, and faith.7 Meaning represents the cognitive aspect of spirituality, and may help maintain a sense of purpose and stability in the midst of life challenge. A sense of peace represents the affective aspect of spirituality, and may be experienced when an individual has reached acceptance of a particular life challenge and pursues meaningful goals. Faith is related to reliance on or adherence to particular spiritual beliefs and practices as a foundation for understanding the world.11 In studies of cancer patients, meaning and peace have typically been more strongly related to well-being than faith.11
Few studies have assessed longitudinal changes in spirituality after a cancer diagnosis. A national survey in the US indicates that patients with cancer report an increased role of spirituality and religion in their lives between pre-diagnosis and a median of 10 years post-diagnosis.12 Change in a sense of meaning/peace has been related to decreased depression over time in breast cancer patients after diagnosis and in hematopoetic cancer patients after stem cell transplantation.13,14 Another study of cancer patients about 3.5 years after diagnosis showed that greater changes in a sense of meaning/peace measured over one year were associated with better mental health and lower distress at follow-up, while faith was only related to perceived growth.15 No studies have examined differential effects of changes in meaning versus peace with respect to their effects on mood. Importantly, spirituality can decline after a trauma, as some people feel spiritually “lost” or that their faith is shaken.10 This is noteworthy, as lack of spiritual support is strongly associated with distress.16
Although the diagnosis of cancer represents a significant threat in itself, previously experienced stressful life events can impact an individual’s experience of overall distress and stress tolerance, thus increasing vulnerability to distress in response to a subsequent event.17 Our previous work has shown that non-cancer life events experienced in the year after diagnosis negatively impact quality of life (QOL) at one-year post-diagnosis, adjusting for mood outcomes.18 Potential moderators of this relationship can provide important insight into treatment targets. For example, social support has been found to moderate the effect of cancer-related stress on psychological sequelae.19 While PTG has been proposed to contribute to psychological well-being, it has been argued that it reflects the cognitive coping strategy of assimilation, in which one perceives benefits from cancer to maintain their sense of identity and/or to avoid cognitive dissonance.20 Thus, assessing the effects of actual PTG on the relationship between life stress and psychological outcomes can help elucidate the protective effects of growth after cancer diagnosis.
Given the importance of protective resources in cancer and the dearth of research on longitudinal outcomes associated with PTG, a greater understanding of the adaptive value of PTG after diagnosis of ovarian cancer is warranted. The current study uses a prospective longitudinal design over the first year following ovarian cancer diagnosis and primary treatment to examine spiritual changes and their relationship to psychological outcomes. Furthermore, greater understanding of the effects of changes in spirituality on psychological well-being in the presence of life stress will clarify its potential value as a protective resource.
Methods
Participants and Procedures
Patients were recruited at a clinic visit before surgery for suspected ovarian cancer as part of a larger study on stress and tumor growth in ovarian cancer. Eligible patients included those with primary epithelial ovarian, peritoneal, or fallopian tube carcinomas and inclusion was confirmed following histological assessment. Participants were excluded from the study if they were less than 18 years old or had a tumor with low-malignant potential. For the larger study, patients were also excluded if they had recently used systemic corticosteroid medication or were diagnosed with immune-altering comorbidities. Psychosocial measures were completed 1–2 weeks prior to surgery and at one-year follow-ups. These analyses included 241 patients. All procedures were approved by institutional review boards at The University of Iowa (#200308061), Washington University, and University of Miami.
Measures
Demographics and clinical variables
Demographic variables including age, race, ethnicity, education, and income were collected at pre-surgery. Cancer stage, grade, and recurrence status were determined by medical chart review.
Spirituality
The FACIT-Sp 12 consists of 12 items measuring spirituality with 3 subscales of 4 items: meaning (e.g., “I have a reason for living”), peace (e.g., “I feel a sense of harmony within myself”), and faith (e.g., “I find comfort in my faith or spiritual beliefs”).7,8 To determine whether spirituality was best conceptualized in this sample as having 3 factors or 2 (with the meaning and peace subscales combined), confirmatory factor analysis was used. The 3-factor model had substantially better fit to the data. Thus, the 3 separate subscales were used. Reliability of these scales at pre-surgery was moderate, with Cronbach’s alphas of .73 (meaning), .82 (peace), and .83 (faith). At one-year, Cronbach’s alphas were .80 (meaning), .83 (peace) and .87 (faith).
Stressful life events
Life events were measured using a modified version of the Life Experiences Survey (LES)21 incorporating seventeen items, indicating major life events spanning domains of relationships, illness/death of family/close friends, work/finances, other illnesses, accidents/injuries, and safety concerns. An additional question was included for any major event not listed. Participants answered whether they had experienced each event in the last year and the sum of these was calculated. This questionnaire was given at the one-year follow-up, assessing the presence of life stressors the year after diagnosis, (Cronbach’s alpha=.65).
Depression
Depression was measured with the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item self-report scale, which has been shown to be reliable in cancer patients.22,23 Participants are asked to rate the frequency of certain experiences, e.g., “I felt sad.” The subscales of this questionnaire include vegetative, positive, negative, and interpersonal symptoms.22 (Cronbach’s alpha= .92 at one-year).
Cancer-specific anxiety
Intrusive thoughts (e.g. “I thought about it when I didn’t mean to”) and avoidance (e.g., “I tried not to talk about it”) were assessed with the Impact of Event Scale (IES).24 This 15-item scale has been used previously in cancer patients as a measure of anxiety symptoms associated with posttraumatic stress disorder.25 (Cronbach’s alpha= .89 at one-year).
Mood
The Profile of Mood States short-form (POMS-SF) is a 37-item measure in which participants rate their mood over the past week, with subscales for fatigue, vigor, tension/anxiety, depression/dejection, confusion, and anger/hostility.26 This scale has been validated in cancer patients.27 The total mood disturbance score, (TMD, the sum of all factors minus vigor), was used in this study as an overall measure of mood. (Cronbach’s alpha= .93 at one-year).
Statistical Analysis
Analyses used the Statistical Package for the Social Sciences v. 21 (SPSS, Armonk, NY). Distributions were examined for normality and outliers were removed. A priori covariates included cancer stage and recurrence status at one-year follow-up to control for the psychological effects of recurrence and disease severity on outcomes. Correlations examined relationships between demographic variables (age, education, income, race, and ethnicity) with psychological outcomes to assess for additional covariates. Age was significantly related to depression and TMD, and education was significantly related to anxiety and TMD; thus, age and education were included as covariates in all analyses.
Paired samples t-tests assessed changes in spirituality subscales from pre-surgery to one-year. Next, change scores were created, subtracting the pre-surgery measure from the one-year measure of each subscale. Finally, multiple regression analyses were used to examine the effect of these changes on depression, anxiety, and TMD at one-year. In addition to the above covariates, each regression model included pre-surgery scores of the relevant psychological outcome measured at pre-surgery. Change scores for all spirituality subscales were included simultaneously as predictors. To examine whether spiritual change buffered the effects of stressful life events on psychological outcomes at one-year, another set of multiple regression models included the main effects of spiritual change and life events along with their interaction, which was created with mean-centered variables. Unstandardized simple slopes were probed and plotted utilizing the “MODPROBE” SPSS macro.28
Results
Patient Characteristics
The mean age of participants was 59.2 years at study entry (see Table 1 for demographics). The patients in this sample were primarily white (95.1%), married/living with a partner (69.7%), and college-educated (32.2%). Most patients had stage III ovarian cancer (58.3%), and 85% had high grade tumors.
Table 1.
Demographic and clinical characteristics of participants (N=241)
| Characteristic | Mean (SD) |
|---|---|
|
| |
| Age (years) | 58.71 (11.16) |
|
| |
| N (%) | |
| Race (N=240) | |
| American Indian/Alaskan Native | 1 (.4) |
| Asian | 2 (.8) |
| Black/African American | 7 (2.9) |
| White | 230 (95.4) |
| Ethnicity (N=240) | |
| Non-Hispanic | 234 (97.5) |
| Hispanic | 6 (2.5) |
| Education (N=239) | |
| Less than high school graduate | 11 (4.6) |
| High school graduate | 75 (31.4) |
| Trade school/some college | 68 (28.5) |
| College graduate | 60 (25.1) |
| Postgraduate degree | 25 (10.5) |
| Relationship status | |
| Married, living with partner | 169 (70.1) |
| Single, separated, widowed, divorced | 72 (29.9) |
| Cancer stage | |
| I | 59 (24.5) |
| II | 23 (9.5) |
| III | 144 (59.8) |
| IV | 15 (6.2) |
| Grade | |
| Low | 35 (14.5) |
| High | 206 (85.5) |
| Histology | |
| Serous | 169 (70.1) |
| Endometrioid | 27 (11.2) |
| Mucinous | 6 (2.5) |
| Clear cell | 20 (8.3) |
| Other/unknown/missing | 19 (7.9) |
| Recurrence at one-year | |
| No | 204 (84.6) |
| Yes | 37 (15.4) |
Change in spirituality over time
Faith, meaning, and peace were examined longitudinally to assess how reported spirituality changed from pre-surgery to one-year. Each subscale changed significantly over time (faith: t=−3.23, p=.001; meaning: t=2.99, p=.003; peace: t=−2.02, p<.001). Both faith and peace significantly increased from pre-surgery (faith: M=12.04, SD=3.81; peace: M=10.83, SD=3.61) to one-year (faith M=12.69, SD=3.63; peace M=11.7, SD=3.42). In contrast, meaning slightly decreased from pre-surgery levels (M=14.2, SD=2.23) to one-year (M=13.73, SD=2.78). These values are consistent with previous research examining norms in a large sample of adult cancer survivors.29
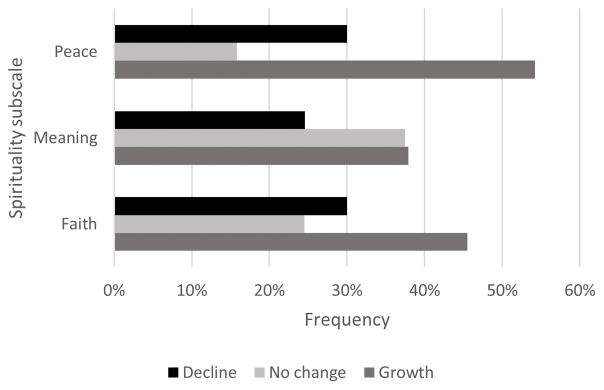
Though the average change over time was small, change scores for each subscale demonstrated substantial variability between individuals. Only 9% of the sample (N=22) remained stable on all spirituality subscales over time. Within each subscale, a significant portion of individuals reported changes over time (75% for faith, 62% for meaning, 84% for peace). There was substantial heterogeneity in these changes, with both decreases/decline and increases/growth in components of spirituality. Changes across all subscales with possible scores of 0–16, ranged from a decrease of 16 to an increase of 13. Frequencies of spiritual changes are displayed in Figure 1. Correlations and one-way ANOVAS were used to examine whether stage, recurrence, age, frequency of attendance at religious services, race, ethnicity, income, and education were related to these changes. Older age was significantly related to greater positive change in meaning (r=.14, p=.03). Additionally, race was related to changes in meaning (r=.19, p=.003); 10 participants who were not Caucasian reported a greater average decline in meaning (M=−2.7) than Caucasian participants (M=.38). All other relationships were not significant.
Figure 1.
Frequencies of change in spirituality subscales
Effect of spiritual change on psychological outcomes at one-year
Associations of spiritual change between diagnosis and one-year and psychological outcomes at one-year are displayed in Table 2. Women exhibiting increases in peace reported significantly lower depression (β =−.40, p<0.001), cancer-specific anxiety (β= −.20, p=.004), and TMD (β= −.41, p<0.001) at one-year, independent of age, stage, recurrence, education, and pre-surgery depression, anxiety, and mood disturbance. Changes in faith and meaning did not significantly predict depression, anxiety, or total mood disturbance at one-year, controlling for age, stage, education, recurrence, and pre-surgery levels of these measurements.
Table 2.
Regressions Examining One-year Outcomes from Spiritual Change and Moderation of Life Events by Change in Peace
| Outcome variables | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Depression | Anxiety | Total mood disturbance | ||||
|
| ||||||
| Predictor variables | B | p | β | P | β | P |
| Regressions predicting one-year outcomes by changes in spirituality | ||||||
| Step 1: Control Variables | ||||||
| Age | −.10 | .08 | −.16 | .008 | −.13 | .04 |
| Education | −.18 | .001 | −.17 | .004 | −.20 | .001 |
| Stage III/IV | −.09 | .13 | −.01 | .85 | −.06 | .29 |
| Recurrence at one-year | .08 | .19 | .03 | .68 | .04 | .49 |
| Pre-surgery dep/anx/mood | .52 | <0.001 | .50 | <.001 | .50 | <.001 |
| R2 | .31 | .31 | .36 | |||
| Step 2: Changes in spirituality | ||||||
| Change in faith | −.05 | .38 | −.11 | .08 | −.09 | .10 |
| Change in meaning | −.10 | .08 | .07 | .31 | −.001 | .99 |
| Change in peace | −.40 | <.001 | −.20 | .004 | −.407 | <.001 |
| R2 | .53 | .36 | .51 | |||
| Regressions examining moderation of life events by changes in peace* | ||||||
| Number of life events | .19 | .001 | .02 | .79 | .22 | <.001 |
| Change in peace | −.39 | <.001 | −.22 | <.001 | −.37 | <.001 |
| Life events* change in peace | −.11 | .027 | −.13 | .05 | −.13 | .01 |
Note: Stage III/IV is compared to stage I/II. Recurrence at 1-year is compared to no recurrence. Education coded for post-high school versus high school graduate and below.
Regressions examining moderation of life events by changes in peace included all control variables from regressions above.
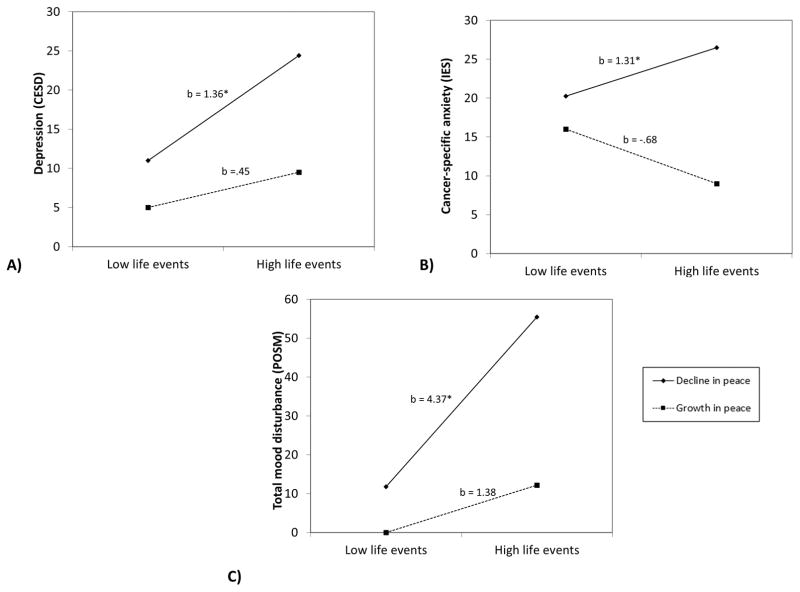
Spiritual change as a moderator of life events
Because change in peace was the only significant predictor of psychological outcomes, this subscale was examined as a potential moderator of the relationship between life events and these outcomes. Results for these analyses are presented in Table 2. Change in peace significantly moderated the effect of life stress on depression (β= −.11, p=.027), anxiety (β= −.16, p=.05), and TMD (β= −.13, p=.01) adjusting for all covariates described above. The effect of life stress on each outcome variable was then calculated at different levels of change in peace (1 SD above/below the mean). The effect of life stress on depression and total mood disturbance was significant when calculated at the average value of change in peace (depression: b=.90, p<.001; TMD: b=2.88, p<.001) and at 1 SD below the mean for change in peace (depression: b=1.36, p<.0001; TMD: b=2.88, p=.0001), indicating that, for those with little change or decreases in peace from pre-surgery to one-year, having more stressful life events was related to greater depression and TMD at one-year. Similarly, the effect of life stress on anxiety was significant at 1 SD below the mean change in peace (b=1.31, p=.005), indicating that life stress was related to greater anxiety at one-year only in those who had decreases in peace over time. On the other hand, the deleterious effect of life stress on mood outcomes was not significant when paired with an increase in peace over time, indicating that positive changes in peace acted as a buffer against life stress. This interaction is shown in Figure 2 at 1 SD above/below the mean for change in peace and at the highest and lowest values for number of stressful life events.
Figure 2.
Effect of non-cancer life stressors on A) depression, B) anxiety, and C) total mood disturbance moderated by changes in peace over time, with simple slopes at 1 SD above/below the mean of changes in peace. *p≤.05
Discussion
The current study examined change in spirituality (i.e., change in self-reported sense of peace, meaning, or faith) in women with ovarian cancer in the first year post-diagnosis and its relationship with mood outcomes at one-year post-diagnosis. In the current sample, each facet of spirituality significantly changed from pre-surgery to one-year. Additionally, there was significant heterogeneity in the percentage of women who reported no change, growth in spirituality, or decline in spirituality. Greater increases in peace during the year after diagnosis were associated with better adjustment at follow-up, as indicated by lower depression, anxiety, and total distress, while changes in faith and meaning were unrelated to these outcomes. Furthermore, change in peace moderated the influence of life events on mood. Women with a high number of life events during the year after diagnosis who experienced a decline in the domain of peace were most likely to report higher depression, anxiety, and overall mood disturbance. This study highlights the importance of spirituality to psychological outcomes, and supports theories of PTG that suggest actual posttraumatic changes can have positive impacts on well-being.2
Because a sense of peace is considered the affective component of spirituality, it may be the facet of spirituality most closely associated with psychological well-being. Peace has previously been shown to have a stronger relationship with mental health and QOL than faith or meaning.7 A sense of peace and harmony may be related to meaning-in-life through action, and engaging in meaning-based behaviors may be a mechanism influencing well-being.30 Faith, the adherence to specific beliefs and practices as a foundation for understanding the world, may indirectly influence outcomes through its influence on other facets of spirituality, as faith may provide meaning and bring about peace. Consistent with this notion, previous studies have shown that peace and meaning mediate the relationship between faith and QOL.31 Lastly, it may be that the overall level of faith and meaning foster positive adjustment to cancer, while changes in these domains (growth or decline) are unrelated to psychological well-being. Much more remains to be understood regarding contextual importance of the specific aspects of spirituality. Future research should examine how each facet of spirituality relates to specific behaviors and coping strategies, as this may reflect mechanisms underlying their protective effects. Furthermore, more research should examine which contextual factors influence the effects of changes in spirituality. For example, a patient with poor social support may benefit more from increases in faith if it leads to increased involvement in their church community.
Our research has previously shown that non-cancer stressful life events have a negative impact on QOL at one-year.18 The current study found that changes in peace may act as a moderator of the relationship between life events and mood outcomes; in particular, spiritual growth can serve as a buffer against effects of life stress. Consequently, decline in a sense of peace may be risk factor that increases vulnerability to the negative effects of stressful life events. Previous research has found that a decreased sense of spirituality after a cancer diagnosis is more related to depression and negative affect than increases in spirituality.10 In fact, a sense of peace, even in the context of terminal illness, has been related to lower psychological distress and better advanced care outcomes.32 Future research should examine the function of changes in a sense of peace in the context of different types of life stressors, as well as a variety of illnesses and severity.
Clinical Implications
Several interventions have been shown to increase PTG,33,34 though none have been specifically targeted increasing a sense of peace among cancer patients. Additionally, some interventions have focused on meaning-making,35 as well as exploration of spirituality through specific coping and emotion regulation skills.36 However, these interventions did not examine peace separately from meaning, which the current findings indicate may be an important distinction. Mindfulness-based interventions have also shown positive effects on psychological well-being in patients with cancer.37 Interventions that target acceptance and values-based behavior are likely to help foster a sense of peace.38 Given the current findings, future research should examine whether increasing a sense of peace as an intervention target, particularly in those with many life stressors, can increase psychological well-being in cancer patients and survivors.
Limitations
Because the baseline assessment occurred when the patient was anticipating a potential cancer diagnosis, it may not fully reflect patient characteristics during a non-crisis state. The current sample was relatively homogenous in demographic characteristics, limiting generalizability to other populations. Additionally, as this study only followed patients until one-year, we may not have captured the full extent of changes in spirituality, as meta-analyses have shown that positive changes increase over time.5 Though we did not find any consistent clinical correlates of spiritual change, this may be related to measurement timing. For example, patients with poor treatment outcomes (e.g., early recurrences) may have a different trajectory of changes in spirituality that may not have been captured at one-year. Future research should explore changes over a longer time period.
Despite these limitations, this study has a number of strengths. Studies examining PTG as an outcome often measure perceived growth, asking participants at one measurement how much they believe they have changed as a result of a specific event, using a retrospective self-report measure such as the Posttraumatic Growth Inventory (PTGI).39 In fact, studies have found minimal correlation between actual growth in the component constructs of PTG and the PTGI assessment.40 Instead, we utilized measures of spirituality over time instead of measures of retrospective, perceived growth, thus providing potentially more accurate information about the relationship between these aspects of PTG and outcomes. Furthermore, this method assesses spiritual decline along with growth. Lastly, most of the patients in our study had advanced stage ovarian cancer, the most lethal of gynecologic cancers. This is an understudied population in cancer research.
Conclusions
This study furthers the understanding of PTG in cancer patients, particularly in the domain of spirituality. Specifically, an increased sense of peace is most related to better psychological outcomes and also buffers the impact of stressful life events on psychological outcomes. These findings have implications for screening individuals who may benefit from interventions and for identifying the most important intervention targets. Future work should continue to examine changes in spirituality over time and their relationships with psychological and contextual factors.
Acknowledgments
This research was supported in part by NIH grants CA104825 and CA140933 to SL and a supplement to LD.
Footnotes
Financial Disclosures: Premal H. Thaker, consulting or advisory role for Incyte, travel/accommodations/expenses from Intuitive Surgical
References
- 1.Roland KB, Rodriguez JL, Patterson JR, Trivers KF. A literature review of the social and psychological needs of ovarian cancer survivors. Psychooncology. 2013;22(11):2408–2418. doi: 10.1002/pon.3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tedeschi RG, Calhoun LG. Trauma & Transformation: Growing in the Aftermath of Suffering. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 3.Tallman Ba, Altmaier E, Garcia C. Finding benefit from cancer. J Couns Psychol. 2007;54(4):481–487. doi: 10.1037/0022-0167.54.4.481. [DOI] [Google Scholar]
- 4.Danhauer SC, Case LD, Tedeschi R, et al. Predictors of posttraumatic growth in women with breast cancer. Psychooncology. 2013;22(12):2676–2683. doi: 10.1002/pon.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helgeson VS, Reynolds Ka, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- 6.Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Heal Psychol. 2004;23(1):16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- 7.Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR. A 3-factor model for the FACIT-Sp. Psychooncology. 2008;17:908–916. doi: 10.1002/pon. [DOI] [PubMed] [Google Scholar]
- 8.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy--Spiritual Well-Being Scale (FACIT-Sp) Ann Behav Med. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 9.Cadell S, Regehr C, Hemsworth D. Factors contributing to posttraumatic growth: a proposed structural equation model. Am J Orthopsychiatry. 2003;73(3):279–287. doi: 10.1037/0002-9432.73.3.279. [DOI] [PubMed] [Google Scholar]
- 10.Cole BS, Hopkins CM, Tisak J, Steel JL, Carr BI. Assessing spiritual growth and spiritual decline following a diagnosis of cancer: Reliability and validity of the spiritual transformation scale. Psychooncology. 2008;17(2):112–121. doi: 10.1002/pon. [DOI] [PubMed] [Google Scholar]
- 11.Visser A, Garssen B, Vingerhoets A. Spirituality and well-being in cancer patients: A review. Psychooncology. 2010;19:565–572. doi: 10.1002/pon. [DOI] [PubMed] [Google Scholar]
- 12.Costanzo ES, Ryff CD, Singer BH. Psychosocial adjustment among cancer survivors: Findings from a national survey of health and well-being. Heal Psychol. 2009;28(2):147–156. doi: 10.1037/a0013221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avis NE, Levine B, Naughton MJ, Case LD, Naftalis E, Van Zee KJ. Age-related longitudinal changes in depressive symptoms following breast cancer diagnosis and treatment. Breast Cancer Res Treat. 2013;139(1):199–206. doi: 10.1007/s10549-013-2513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leeson LA, Nelson AM, Rathouz PJ, et al. Spirituality and the recovery of quality of life following hematopoietic stem cell transplantation. Heal Psychol. 2015;34(9):920–928. doi: 10.1037/hea0000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yanez B, Edmondson D, Stanton AL, et al. Facets of spirituality as predictors of adjustment to cancer: Relative contributions of having faith and finding meaning. J Consult Clin Psychol. 2009;77(4):730–741. doi: 10.1037/a0015820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agarwal J, Powers K, Pappas L, et al. Correlates of elevated distress thermometer scores in breast cancer patients. Support Care Cancer. 2013;21(8):2125–2136. doi: 10.1007/s00520-013-1773-z. [DOI] [PubMed] [Google Scholar]
- 17.Fava Ga, Guidi J, Semprini F, Tomba E, Sonino N. Clinical assessment of allostatic load and Clinimetric criteria. Psychother Psychosom. 2010;79(5):280–284. doi: 10.1159/000318294. [DOI] [PubMed] [Google Scholar]
- 18.Lutgendorf SK, Slavich GM, Degeest K, et al. Non-cancer life stressors contribute to impaired quality of life in ovarian cancer patients. Gynecol Oncol. 2013;131(3):667–673. doi: 10.1016/j.ygyno.2013.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carpenter KM, Fowler JM, Maxwell GL, Andersen BL. Direct and buffering effects of social support among gynecologic cancer survivors. Ann Behav Med. 2010;39:79–90. doi: 10.1007/s12160-010-9160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sumalla EC, Ochoa C, Blanco I. Posttraumatic growth in cancer: Reality or illusion? Clin Psychol Rev. 2009;29(1):24–33. doi: 10.1016/j.cpr.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: Development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46(5):932–946. doi: 10.1037/0022-006X.46.5.932. [DOI] [PubMed] [Google Scholar]
- 22.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 23.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) J Psychosom Res. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 24.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer: A conceptual and empirical review. Clin Psychol Rev. 2002;22(4):499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- 26.Shacham S. A shortened version of the Profile of Mood States. J Pers Assess. 1983;47(3):305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- 27.Baker F, Denniston M, Zabora J, Polland A, Dudley WN. A POMS short form for cancer patients: Psychometric and structural evaluation. Psychooncology. 2002;11(4):273–281. doi: 10.1002/pon.564. [DOI] [PubMed] [Google Scholar]
- 28.Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav Res Methods. 2009;41(3):924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- 29.Munoz AR, Salsman JM, Stein KD, Cella D. Reference values of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being: A report from the American Cancer Society’s studies of cancer survivors. Cancer. 2015;121(11):1838–1844. doi: 10.1002/cncr.29286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am Psychol. 2001;56(3):218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salsman JM, Yost KJ, West DW, Cella D. Spiritual well-being and health-related quality of life in colorectal cancer: A multi-site examination of the role of personal meaning. Support Care Cancer. 2011;19(6):757–764. doi: 10.1007/s00520-010-0871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ray A, Block SD, Friedlander RJ, Zhang B, Maciejewski PK, Prigerson HG. Peaceful awareness in patients with advanced cancer. J Palliat Med. 2006;9(6):1359–1368. doi: 10.1089/jpm.2006.9.1359. [DOI] [PubMed] [Google Scholar]
- 33.Antoni MH, Lehman JM, Kilbourn KM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Heal Psychol. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 34.Stanton AL, Danoff-Burg S, Sworowski LA, et al. Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. J Clin Oncol. 2002;20(20):4160–4168. doi: 10.1200/JCO.2002.08.521. [DOI] [PubMed] [Google Scholar]
- 35.Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology. 2010;19(1):21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garlick M, Wall K, Corwin D, Koopman C. Psycho-spiritual integrative therapy for women with primary breast cancer. J Clin Psychol Med Settings. 2011;18(1):78–90. doi: 10.1007/s10880-011-9224-9. [DOI] [PubMed] [Google Scholar]
- 37.Feros DL, Lane L, Ciarrochi J, Blackledge JT. Acceptance and Commitment Therapy (ACT) for improving the lives of cancer patients: A preliminary study. Psychooncology. 2013;22(2):459–464. doi: 10.1002/pon.2083. [DOI] [PubMed] [Google Scholar]
- 38.Karekla M, Constantinou M. Religious coping and cancer: Proposing an acceptance and commitment therapy approach. Cogn Behav Pract. 2010;17(4):371–381. doi: 10.1016/j.cbpra.2009.08.003. [DOI] [Google Scholar]
- 39.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 40.Frazier P, Tennen H, Gavian M, Park C, Tomich P, Tashiro T. Does self-reported posttraumatic growth reflect genuine positive change? Psychol Sci. 2009;20(7):912–919. doi: 10.1111/j.1467-9280.2009.02381.x. [DOI] [PubMed] [Google Scholar]