Abstract
Diabetic retinopathy (DR) is the most common complication of diabetes and a major cause of new-onset blindness in the developed world. The present study aimed to examine the effect of kaempferol on high glucose-induced human retinal endothelial cells (HRECs) in vitro. The expression levels of various mRNAs and proteins were measured by reverse transcription-quantitative polymerase chain reaction (RT-qPCR) and western blotting, respectively. The target of kaempferol was determined using a luciferase reporter assay. In addition, HREC proliferation, migration and cell sprouting were determined using Cell Counting kit-8, wound scratch and tube formation assays, respectively. RT-qPCR and western blotting results showed that treatment with 30 mM glucose for 12, 24 and 48 h increased the expression level of estrogen-related receptor α (ERRα) mRNA and protein. The luciferase reporter assay demonstrated that kaempferol inhibited ERRα activity in HRECs. Compared with 5 mM normal glucose treatment, high (30 mM) glucose significantly promoted the proliferation, migration and tube formation of HRECs, which was antagonized by 10 and 30 µM kaempferol in a dose-dependent manner. Treatment with 30 mM glucose also increased the expression of vascular endothelial growth factor (VEGF) mRNA and protein, and the expression levels of VEGF mRNA and protein were suppressed by kaempferol (10 and 30 µM). Kaempferol (30 µM) treatment also increased the expression levels of thrombospondin 1 (TSP-1) and a disintegrin and metalloproteinase with thrombospondin motifs 1 (ADAMTS-1) mRNA; however, TSP-1 and ADAMTS-1 levels did not differ between high glucose and normal (5 mM) glucose conditions. The results of this study suggest that kaempferol targets ERRα and suppresses the angiogenesis of HRECs under high glucose conditions. Kaempferol may be a potential drug for use in controlling the progression of DR; however, in vivo studies are required to evaluate its efficacy and safety.
Keywords: diabetic retinopathy, human retinal endothelial cell, kaempferol, estrogen-related receptor α, angiogenesis, vascular endothelial growth factor
Introduction
Diabetic retinopathy (DR) is the most common complication of diabetes and the main cause of new-onset blindness in the developed world (1). This complication is a result of multiple pathogenic processes caused by hyperglycemia and the deregulation of insulin signalling pathways, which in turn causes neuro-retinal dysfunction and retinal microvascular degeneration (2,3). The early clinical signs of DR include microaneurysms and hemorrhages, while the later signs are narrowed, tortuous and irregular retinal blood vessels, due to the formation of abnormal new blood vessels at the back of the eye in proliferative DR (4). Although significant improvements have been made, no effective prevention or treatment for DR exists. Therefore, the development of novel and effective measures for the treatment and prevention of DR is necessary.
During the new blood vessel formation process, capillaries are formed when endothelial cells are stimulated to migrate, proliferate and invade the surrounding tissues (5). Various pro- and anti-angiogenic molecules regulate this process under normal conditions. When the regulatory balance is adversely affected, dysfunction of endothelial cells may occur. Among the angiogenic mediators, vascular endothelial growth factor (VEGF) is considered to be the main stimulating factor, which acts via promoting the migration and proliferation of vascular endothelial cells, and thereby stimulates the generation of new blood vessels (6). Endogenous inhibitors of angiogenesis include thrombospondin 1 (TSP-1) and a disintegrin and metalloproteinase with thrombospondin motifs 1 (ADAMTS-1), and their aberrant expression may contribute to the diabetes-related dysregulation of retinal vascular homeostasis and vasculopathies (7,8).
Estrogen-related receptor α (ERRα) belongs to a nuclear receptor superfamily characterized by their high levels of sequence identity to estrogen receptors, and the primary role of ERRα is in energy metabolism (9). A study has demonstrated that activation of the peroxisome proliferator-activated receptor g coactivator 1-α (PGC-1α)/ERRα pathway increases VEGF expression and angiogenesis in endothelial cells, which suggests that ERRα may be involved in the pathogenesis of DR (10). Kaempferol (3,4′,5,7-tetrahydoxyflavone), a commonly found dietary flavonoid, has been isolated from grapefruit, tea, broccoli and other plant sources (11). The anticancer effects of kaempferol have been demonstrated in previous studies (12,13), and kaempferol has been found to act as an ERRα inverse agonist, which inhibits cell growth in different cancer cell lines by antagonizing ERRα activity (14). Kaempferol has been shown to have an anti-angiogenic effect in ovarian cancer (15); however, whether kaempferol inhibits angiogenesis in DR is unclear. Therefore, the effect of kaempferol on the angiogenesis of retinal endothelial cells under high glucose conditions is worthy of investigation.
In the present study, it was demonstrated for the first time that high glucose treatment increased the expression level of ERRα mRNA and protein in human retinal endothelial cells (HRECs). Luciferase reporter and in vitro functional assays indicated that kaempferol inhibited ERRα activity and suppressed high glucose-induced cell proliferation, migration and tube formation. Further experiments revealed that kaempferol may exert its anti-angiogenesis effect by reducing VEGF expression and increasing TSP-1 and ADAMTS-1 expression.
Materials and methods
Cell culture
HRECs were purchased from ATCC (Manassas, VA, USA) and were cultured in a human microvascular endothelial medium (Cell Applications, Inc., San Diego, CA, USA) and were maintained at 37°C in a humidified 5% CO2 incubator. Experiments were performed using cells between passages 3 and 8.
Treatment of HRECs
For the time-dependence experiment, HRECs were treated with 30 mM glucose for 12, 24 or 48 h, and HRECs incubated in 5 mM normal glucose were used as a negative control. In the kaempferol treatment experiments, HRECs were divided into 5 mM normal glucose, 30 mM glucose, 30 mM glucose plus 10 µM kaempferol, and 30 mM glucose plus 30 µM kaempferol groups. The HRECs were split at 90% confluence and subcultured in 96-well plates or 6-well plates according to the appropriate assay conditions.
Chemicals, plasmids and transfection
Kaempferol and XTC-790 were purchased from Sigma-Aldrich (Merck KGaA, Darmstadt, Germany); pCMX-ERRα and pcDNA-PGC-1α plasmids and the respective plasmids (pCMX and pCDNA) used as negative controls were purchased from Generay Biotechnology Co., Ltd. (Shanghai, China). All transfections were conducted using Lipofectamine 2000 (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the manufacturer's instructions.
RNA preparation and reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis
Total RNA was isolated from the cells using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.). A TaqMan Reverse Transcription kit (Takara Biotechnology Co., Ltd., Dalian, China) was used to prepare cDNA from the ERRα, VEGF, TSP-1 and ADAMTS-1 RNA. qPCR was performed using a SYBR Green PCR kit (Takara Biotechnology Co., Ltd.) according to the manufacturer's instructions. GAPDH was used as an internal control. The primers for ERRα mRNA were: forward, 5′-TTCGGCGACTGCAAGCTC-3′ and reverse, 5′-CACAGCCTCAGCATCTTCAATG-3′; the primers for VEGF mRNA were: forward, 5′-TGCCATCCAATCGAGACCCTG-3′ and reverse, 5′-GGTGATGTTGGACTCCTCAGTG-3′; the primers for TSP-1 mRNA were: forward, 5′-GGTCGGCCTGCACTGTCACC-3′ and reverse, 5′-GGGGAAGCTGCTGCACTGGG-3′; the primers for ADAMTS-1 mRNA were: forward, 5′-CTCCGCCTGCACGCCTTTGA-3′ and reverse, 5′-ATCGCCATTCACGGTGCCGG-3′. Data were expressed as fold changes relative to GAPDH calculated based on the 2−∆∆Cq method (16).
Luciferase reporter assay
HRECs were seeded in a 96-well plate (1×104 cells/well), incubated for 24 h, and then co-transfected with pGL3-ERRE-Luci (reporter; Promega Corporation, Madison, WI, USA) and pMCX-ERRα with or without pcDNA-PGC-1α plasmids. Renilla luciferase plasmid (Promega Corporation) was used as an internal control. At 24 h after transfection, cells were treated with kaempferol (10 or 30 µM) or XTC-790 (15 µM) for 24 h and then harvested for luciferase assay. Luciferase activity was measured using a Dual-Luciferase Reporter Assay system (Promega Corporation).
Cell proliferation assay
HRECs (3×103) were seeded into each well of a 96-well plate and allowed to adhere for 24 h. When the cells were adherent to the bottom of the plate, they were cultured in serum-free medium for starvation for 24 h. The cells were then treated with glucose alone (5 and 30 mM) or 30 mM glucose with kaempferol (10 or 30 µM) for 24 h, and the proliferative activity was determined by Cell Counting kit-8 (CCK-8) assay (Beyotime Institute of Biotechnology, Haimen, China) according to the manufacturer's instructions. In brief, 10 µl CCK-8 was added to each well, and following incubation for 2 h, the absorbance at a wavelength of 450 nm was detected.
Cell migration assay
When the HRECs had grown to 90% confluence in 6-well plates, they were starved with serum-free medium for 12 h. When the HRECs were over-confluent, a 200-µl pipette tip was used to create a wound. The floating cells were removed by washing three times with sterile 1X phosphate-buffered saline. After this, the cells were incubated with serum-free media containing glucose alone (5 and 30 mM) or 30 mM glucose with kaempferol (10 or 30 µM) for 24 h, and then cultured in a 6-well plate at 37°C in an incubator with 5% CO2. The migration monolayer was photographed at 0, 12, 24 and 48 h. Photographic images of five fields were photographed for each well, and the migration distance was measured.
Tube formation assay
After thawing in a refrigerator at 4°C overnight, 60 µl Matrigel was added to a pre-cooled 96-well plate and then solidified by immediately placing the plate in a humidified CO2 incubator at 37°C for 30 min. HRECs that had been cultured with serum-free media containing glucose alone (5 and 30 mM) or 30 mM glucose with kaempferol (10 or 30 µM) for 24 h, were seeded immediately on the solidified Matrigel at a density of 1.5×104 cells/well. The plates were placed in a humidified atmosphere of 5% CO2 and 95% air at 37°C for 8 h. Images of the plates were captured, and the number of capillaries formed was qualitatively assessed using Image-Pro Plus 6.0 software (Media Cybernetics, Inc., Rockville, MD, USA).
Western blot analysis
HRECs were lysed in SDS lysis buffer containing protease inhibitor (Sigma-Aldrich; Merck KGaA), and the protein concentration was measured using a Bio-Rad Protein Assay kit (Bio-Rad Laboratories, Inc., Hercules, CA, USA) according to the manufacturer's instructions. Proteins were then separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and transferred to a polyvinylidene fluoride membrane. The membrane was incubated with the following primary antibodies: Mouse anti-ERRα (1:1,500; sc-65718; Santa Cruz Biotechnology, Inc., Dallas, TX, USA), rabbit anti-VEGF (1:2,000; no. 2463; Cell Signalling Technology, Inc., Boston, MA, USA), and mouse anti-β-actin (1:6,000; ab8226; Abcam, Cambridge, MA, USA) at 4°C overnight. Membranes were then incubated with the horseradish peroxidase-conjugated secondary antibodies (1:4,000; ab6728; Abcam) at room temperature for 1 h. After further incubation with the enhanced chemiluminescence substrate (Bio-Rad Laboratories, Inc., Hercules, CA, USA), the membranes were exposed using a ChemoDoc XRS detection system (Bio-Rad Laboratories, Inc.). The band intensities were analysed by the Image Lab v.6.0 software (Bio-Rad Laboratories, Inc.).
Statistical analysis
All statistical analysis was performed using GraphPad Prism 6 (GraphPad. Software, Inc., La Jolla, CA, USA). Data are presented as the mean ± standard deviation; and differences among the treatment groups were compared by one-way analysis of variance followed by Dunnett's multiple comparison test, or unpaired t-test as appropriate. P<0.05 was considered to indicate a statistically significant difference.
Results
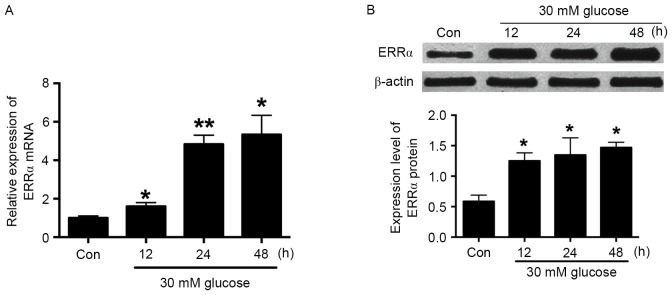
Effect of high glucose on ERRα mRNA and protein expression in HRECs
RT-qPCR was conducted to evaluate the ERRα mRNA expression in HRECs following treatment with 30 mM glucose for 12, 24 and 48 h. The results showed that glucose (30 mM) significantly increased ERRα mRNA expression in a time-dependent manner (Fig. 1A). The effect of 30 mM glucose on ERRα protein expression was evaluated by western blot analysis, and similar results were obtained; this concentration of glucose also increased ERRα protein expression in a time-dependent manner (Fig. 1B). As treatment with 30 mM glucose for 24 h significantly increased ERRα expression at the mRNA and protein levels, a 24-h treatment time was selected for high glucose treatment in the following experiments.
Figure 1.
High glucose (30 mM) increases the expression of ERRα. After HRECs had been treated with 30 mM glucose for 12, 24 and 48 h, (A) reverse transcription-quantitative polymerase chain reaction was performed to measure the expression level of ERRα mRNA and (B) western blotting was performed to determine the expression level of ERRα protein. All values represent the mean ± standard deviation (n=3). *P<0.05 and **P<0.01 vs. Con. HREC, human retinal endothelial cell; ERRα, estrogen-related receptor α; Con, control (5 mM glucose).
Effects of kaempferol on the activity of ERRα
Kaempferol has been shown to inhibit ERRα activity in cancer cells (12). In the present study, whether kaepmferol is able to inhibit ERRα in HRECs was investigated. The luciferase reporter assay showed that HREC cells co-transfected with pCMX-ERRα and pcDNA-PGC-1α plasmids had a higher luciferase activity comparing with that of the HRECs transfected with only one plasmid (Fig. 2); kaempferol and XTC-790 treatment each significantly reduced the luciferase activity in cells co-transfected with pCMX-ERRα and pcDNA-PGC-1α plasmids compared with the untreated co-transfected control, and kaempferol exhibited the inhibitory effect in a concentration-dependent manner (Fig. 2). These results indicate that kaempferol inhibits ERRα activity in HRECs.
Figure 2.
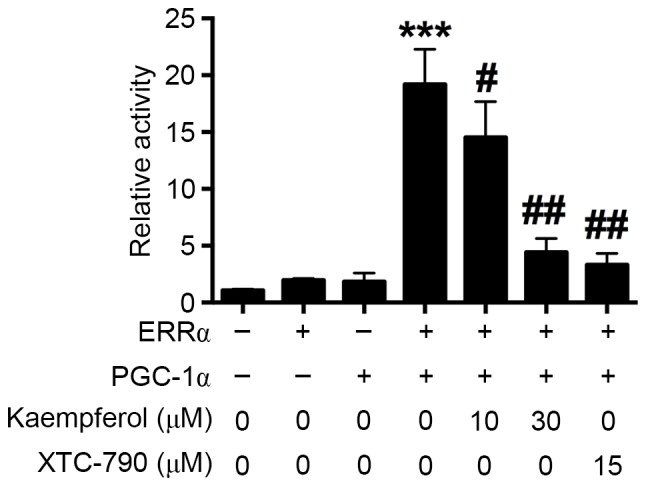
Kaempferol (10 and 30 µM) inhibits ERRα. HRECs were transfected with the plasmids pCMX-ERRα and/or pcDNA-PGC-1α together with reporter pGL3-ERRE-Luc and control Renilla luciferase plasmid, and cells were then treated with kaempferol or XTC-790 for 24 h prior to harvesting for luciferase assays. All values represent the mean ± standard deviation (n=3). #P<0.05, ##P<0.01 and ***P<0.001 vs. the HRECs transfected with only one plasmid. HREC, human retinal endothelial cell; ERRα, estrogen-related receptor α; PGC-1α, proliferator-activated receptor g coactivator 1-α.
Effects of kaempferol on glucose-induced cell proliferation, migration and tube formation of HRECs
An in vitro CCK-8 assay was carried out to examine the proliferative ability of HRECs after the cells had been treated with glucose (30 mM) alone or in combination with 10 or 30 µM kaempferol for 24 h. The results showed that 30 mM glucose treatment significantly increased the proliferation of HRECs compared with 5 mM glucose treatment, and the proliferation of HRECs induced by 30 mM glucose was inhibited by concurrent treatment with 30 µM kaempferol (Fig. 3A).
Figure 3.
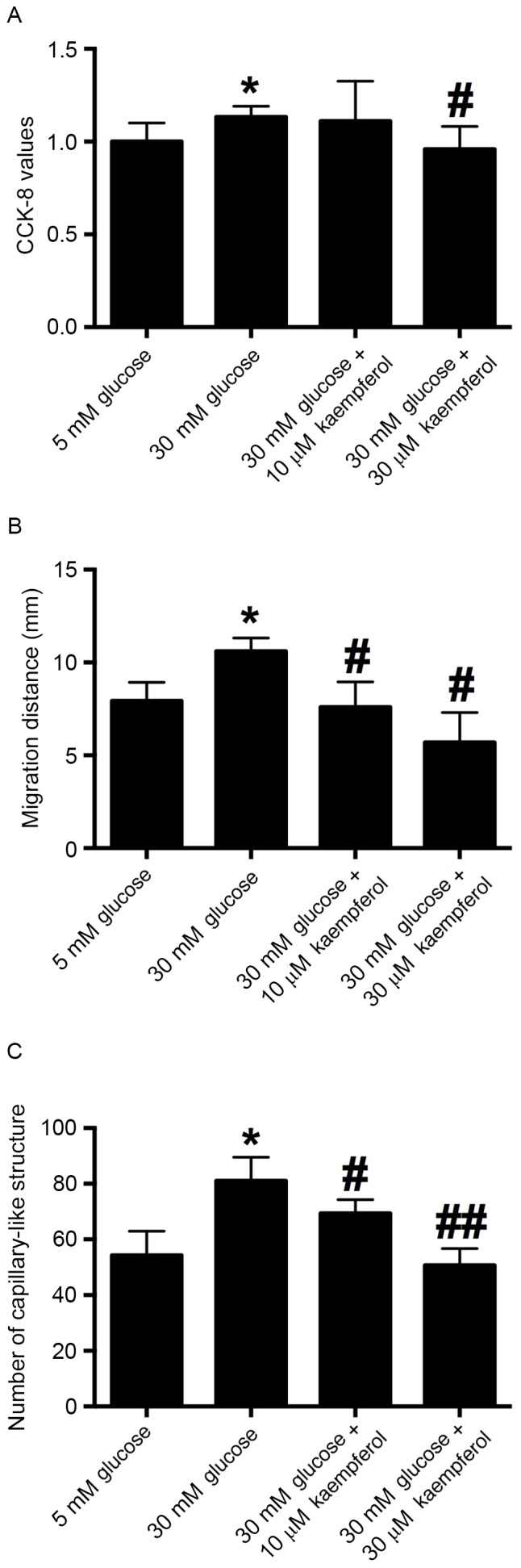
Kaempferol suppresses glucose (30 mM)-induced proliferation, migration and tube formation of HRECs. After HRECs had been treated with glucose (30 mM) alone or in combination with kaempferol (10 or 30 µM) for 24 h, (A) a CCK-8 assay was performed to assess cell proliferation, (B) wound scratch assay was performed to measure cell migration, and (C) Matrigel assay was performed to assess tube formation. All values represent the mean ± standard deviation (n=3). *P<0.05 vs. the 5 mM glucose group; #P<0.05 and ##P<0.01 vs. the 30 mM glucose group. HREC, human retinal endothelial cell; CCK-8, Cell Counting kit-8.
A wound scratching assay was conducted to examine whether kaempferol was able to modulate the glucose-induced migration of HRECs. The results showed that 30 mM glucose significantly accelerated the wound closure compared with that in the 5 mM glucose treatment group. Treatment with kaempferol (10 or 30 µM) significantly inhibited the migration of HRECs induced by 30 mM glucose compared with that in the 30 mM glucose group (Fig. 3B). These results indicate that kaempferol inhibits the high glucose-induced migration of HRECs.
To examine the effect of glucose (30 mM) and kaempferol (10 or 30 µM) on angiogenesis, the tube formation of HRECs was evaluated by Matrigel assay. The results showed that 30 mM glucose significantly increased the number of capillary-like structures compared with that in the 5 mM glucose treatment group. HRECs treated with kaempferol (10 and 30 µM) had fewer capillary-like structures compared with the high glucose-treatment group (Fig. 3C). The results suggest that kaempferol inhibits high glucose-induced tube formation.
Effects of high glucose and kaempferol on VEGF, ADAMTS-1 and TSP-1 mRNA expression in HRECs
To examine whether high glucose and kaempferol induce changes in VEGF, ADAMTS-1 and TSP-1 mRNA expression in HRECs, RT-qPCR was conducted. The expression of VEGF mRNA was significantly increased by treatment with 30 mM glucose compared with that with 5 mM glucose, and kaempferol (10 and 30 µM) significantly antagonized the glucose-induced increase in VEGF mRNA expression (Fig. 4A). ADAMTS-1 and TSP-1 mRNA levels did not differ significantly between the 5 and 30 mM glucose groups, while kaempferol treatment increased the expression of ADAMTS-1 and TSP-1 mRNA in the HRECs (Fig. 4B and C).
Figure 4.
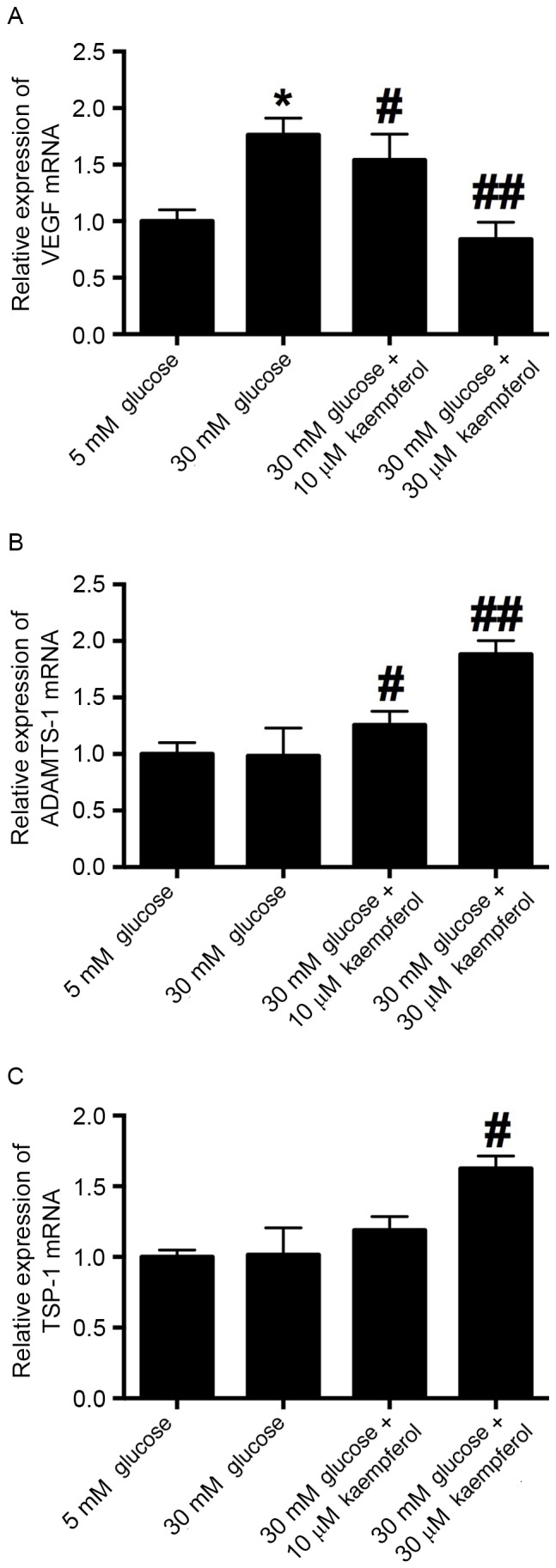
Effects of kaempferol on the expression of pro- and anti-angiogenic factors. After HRECs had been treated with glucose (30 mM) alone or in combination with kaempferol (10 or 30 µM) for 24 h, reverse transcription-quantitative polymerase chain reaction was performed to determine the mRNA expression levels of (A) VEGF, (B) ADAMTS-1 and (C) TSP-1. All values represent the mean ± standard deviation (n=3). *P<0.05 vs. the 5 mM glucose group; #P<0.05 and ##P<0.01 vs. the 30 mM glucose group. HREC, human retinal endothelial cell; VEGF, vascular endothelial growth factor; ADAMTS-1, a disintegrin and metalloproteinase with thrombospondin motifs 1; TSP-1, thrombospondin 1.
Effects of high glucose and keampferol on VEGF protein in HRECs
Western blotting results demonstrated that 30 mM glucose increased the expression of VEGF protein compared with that in the 5 mM glucose group, and kaempferol (10 and 30 µM) significantly antagonized the high glucose-induced increase in expression (Fig. 5).
Figure 5.
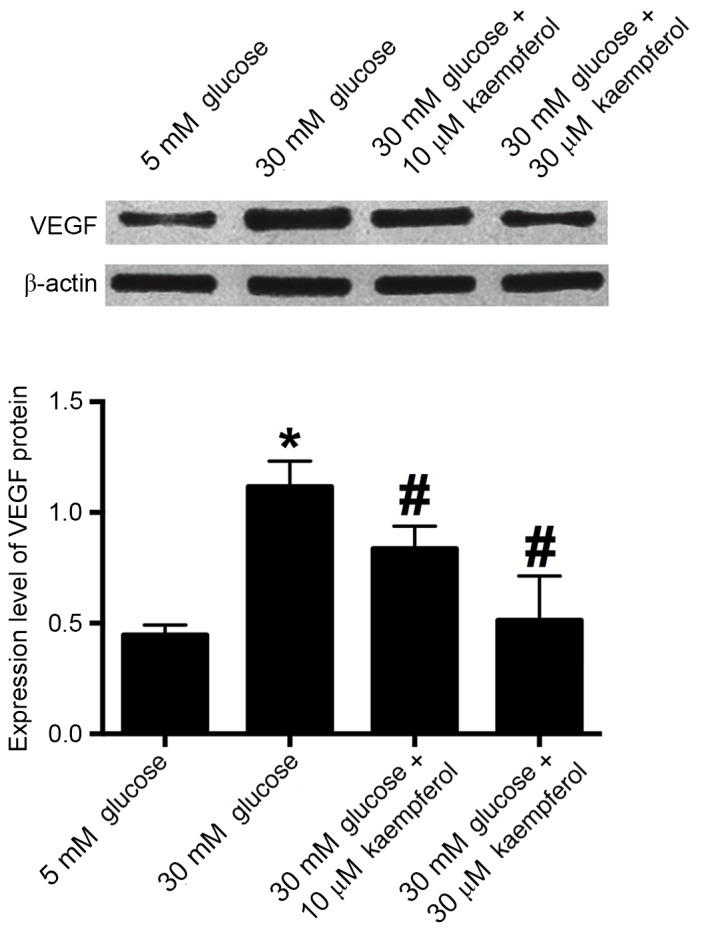
Kaempferol (10 and 30 µM) inhibited glucose (30 mM)-induced VEGF expression. After HRECs had been treated with glucose (30 mM) alone or in combination with kaempferol (10 or 30 µM) for 24 h, western blotting was performed to determine the VEGF protein expression level. All values represent the mean ± standard deviation (n=3). *P<0.05 vs. the 5 mM glucose group; #P<0.05 vs. the 30 mM glucose group. HREC, human retinal endothelial cell; VEGF, vascular endothelial growth factor.
Discussion
The present study demonstrated for the first time that high glucose treatment increases the expression of ERRα at the mRNA and protein levels in HRECs. Luciferase reporter and in vitro functional assays indicated that kaempferol was able to inhibit ERRα activity and suppress the high glucose-induced cell proliferation, migration and tube formation. Further experiments suggested that kaempferol may exert its anti-angiogenic effect via the downregulation of VEGF and upregulation of ADAMTS-1 and TSP-1.
The development of DR is largely attributed to high glucose levels, which generate cellular stress, cause injury to vascular pericytes and endothelial cells, and induce the development of abnormal capillaries (17). Endothelial cells play a key role in regulating vascular tone, and dysfunction of these cells is crucial for the development of DR (18). In the present study, HRECs were used to simulate the pathogenesis of DR under high glucose condition; and high glucose treatment for 24 h was shown to increase the proliferation, migration and tube formation of HRECs. The high glucose-induced migration and tube formation of HRECs have been well documented in previous reports (19–21). However, the effect of high glucose on the proliferation of HRECs found in these studies has varied. Yuan et al demonstrated that treatment of HRECs with 30 mM glucose for 48 h increased the proliferation of HRECs compared with 5 mM glucose treatment (18), while two other studies indicated that treatment with 30 mM glucose for 24 and 72 h failed to increase the proliferation of HRECs (20,22). Differences in cell lines and culture times have been suggested as a cause of the discrepancy. The increase in the proliferation of HRECs following treatment with 30 mM glucose for 24 h was only ~5% in our study, and the effect was very marginal; thus, further investigation may be required to elucidate the effect of high glucose levels on these cells.
ERRα has roles in energy metabolism, and various biosynthetic pathways, and is a key hypoxic growth regulator (23). However, the role of ERRα in the pathogenesis of DR is largely unknown. PGC-1α, a co-activator of ERRα, has been shown to regulate VEGF and angiogenesis in a HIF-independent manner (24). Activation of the PGC-1α/ERRα pathway by baicalin has been shown to increase VEGF expression and angiogenesis (10). More importantly, it has also been found that PGC-1α affects both glucose metabolism and angiogenesis in multiple myeloma cells by regulating VEGF and GLUT-4 (25). In the present study, high glucose treatment was demonstrated to increase the expression of EERα at the mRNA and protein levels. Collectively, these data may indicate a potential role for EERα in DR. Kaempferol has been shown to be an ERRα inverse agonist that is able to inhibit cell growth by antagonizing ERRα (14), and its anticancer effect has also been recognized (12,13). However, its role in DR has not previously been reported. In the present study, a luciferase reporter assay demonstrated that kaempferol inhibited ERRα in HRECs, which suggests that the effects of kaempferol may be mediated via the targeting of ERRα. To further elucidate the effect of kaempferol on the pathogenesis of DR, in vitro functional experiments were conducted, which showed that kaempferol suppressed the high glucose-induced proliferation, migration and tube formation of HRECs. Kaempferol has previously been shown to inhibit angiogenesis and VEGF expression in human ovarian cancer cells via an ERK-NFkB-cMyc-p21 pathway (15); Liang et al demonstrated that kaempferol suppressed angiogenesis through inhibiting VEGF receptor 2 expression, and this effect was enhanced by fibroblast growth factor (FGF) inhibition in a transgenic zebrafish model (26). On the basis of these findings, it may be suggested that ERRα could be involved in the pathogenesis of DR, and that kaempferol might be a useful tool for inhibiting angiogenesis in DR.
Angiogenesis is a complex and multistep process, and when the regulatory mechanism for angiogenesis is unbalanced, dysfunction may occur. VEGF is considered to mediate the abnormal angiogenesis that occurs in response to high glucose (6). Various studies have indicated that high glucose stimulates VEGF secretion (27), and the findings of the present study are consistent with this. The results of the present study indicated that kaempferol significantly antagonized the high glucose-induced increase in VEGF expression at the mRNA and protein levels, which suggests that kaempferol exerts an anti-angiogenic effect via the suppression of VEGF expression. Whether kaempferol has an effect on the expression of the anti-angiogenic molecules, TSP-1 and ADAMTS-1, which are constitutively present in HRECs, was then investigated. These molecules can inhibit vascular development (28,29). ADAMTS-1 acts on TSP-1, causing it to release anti-angiogenic polypeptides (30). TSP-1 deficiency has been found to exacerbate the pathogenesis of diabetic retinopathy (7). At high concentrations, ADAMTS-1 has been shown to inhibit the endothelial migration induced by combined treatment with VEGF and basic FGF (31). In the present study, it was found that kaempferol increased the expression of TSP-1 and ADAMTS-1 mRNA in HRECs under high glucose conditions. These results suggest that kaempferol suppressed the high glucose-induced angiogenesis of HRECs by regulating pro-angiogenic and anti-angiogenic factors.
In conclusion, the findings of the present study suggest that kaempferol inhibits ERRα and reduces the high glucose-induced proliferation, migration and tube formation of HRECs via the regulation of pro- and anti-angiogenic factors. The results suggest that kaempferol is potentially useful as a drug to control the progression of DR. However, in vivo studies are required to evaluate its efficacy and safety.
Acknowledgements
The present study was supported by the Innovative Research Program of Shenzhen City (grant no. JYJ201304011).
References
- 1.Yu DY, Cringle SJ, Su EN, Yu PK, Jerums G, Cooper ME. Pathogenesis and intervention strategies in diabetic retinopathy. Clin Exp Ophthalmol. 2001;29:164–166. doi: 10.1046/j.1442-9071.2001.00409.x. [DOI] [PubMed] [Google Scholar]
- 2.Hendrick AM, Gibson MV, Kulshreshtha A. Diabetic Retinopathy. Prim Care. 2015;42:451–464. doi: 10.1016/j.pop.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Wan TT, Li XF, Sun YM, Li YB, Su Y. Recent advances in understanding the biochemical and molecular mechanism of diabetic retinopathy. Biomed Pharmacother. 2015;74:145–147. doi: 10.1016/j.biopha.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Osaadon P, Fagan XJ, Lifshitz T, Levy J. A review of anti-VEGF agents for proliferative diabetic retinopathy. Eye (Lond) 2014;28:510–520. doi: 10.1038/eye.2014.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoo SY, Kwon SM. Angiogenesis and its therapeutic opportunities. Mediators Inflamm. 2013;2013:127170. doi: 10.1155/2013/127170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Distler JH, Hirth A, Kurowska-Stolarska M, Gay RE, Gay S, Distler O. Angiogenic and angiostatic factors in the molecular control of angiogenesis. Q J Nucl Med. 2003;47:149–161. [PubMed] [Google Scholar]
- 7.Sorenson CM, Wang S, Gendron R, Paradis H, Sheibani N. Thrombospondin-1 deficiency exacerbates the pathogenesis of diabetic retinopathy. J Diabetes Metab. 2013;(Suppl 12) doi: 10.4172/2155-6156.S12-005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basile DP, Fredrich K, Chelladurai B, Leonard EC, Parrish AR. Renal ischemia reperfusion inhibits VEGF expression and induces ADAMTS-1, a novel VEGF inhibitor. Am J Physiol Renal Physiol. 2008;294:F928–F936. doi: 10.1152/ajprenal.00596.2007. [DOI] [PubMed] [Google Scholar]
- 9.Ranhotra HS. The estrogen-related receptor alpha: The oldest, yet an energetic orphan with robust biological functions. J Recept Signal Transduct Res. 2010;30:193–205. doi: 10.3109/10799893.2010.487493. [DOI] [PubMed] [Google Scholar]
- 10.Zhang K, Lu J, Mori T, Smith-Powell L, Synold TW, Chen S, Wen W. Baicalin increases VEGF expression and angiogenesis by activating the ERR{alpha}/PGC-1{alpha} pathway. Cardiovasc Res. 2011;89:426–435. doi: 10.1093/cvr/cvq296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olszewska MA. New validated high-performance liquid chromatographic method for simultaneous analysis of ten flavonoid aglycones in plant extracts using a C18 fused-core column and acetonitrile-tetrahydrofuran gradient. J Sep Sci. 2012;35:2174–2183. doi: 10.1002/jssc.201200287. [DOI] [PubMed] [Google Scholar]
- 12.Chen AY, Chen YC. A review of the dietary flavonoid, kaempferol on human health and cancer chemoprevention. Food Chem. 2013;138:2099–2107. doi: 10.1016/j.foodchem.2012.11.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim SH, Choi KC. Anti-cancer effect and underlying mechanism (s) of kaempferol, a phytoestrogen, on the regulation of apoptosis in diverse cancer cell models. Toxicol Res. 2013;29:229–234. doi: 10.5487/TR.2013.29.4.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Fang F, Huang Z, Wang Y, Wong C. Kaempferol is an estrogen-related receptor alpha and gamma inverse agonist. FEBS Lett. 2009;583:643–647. doi: 10.1016/j.febslet.2009.01.030. [DOI] [PubMed] [Google Scholar]
- 15.Luo H, Rankin GO, Juliano N, Jiang BH, Chen YC. Kaempferol inhibits VEGF expression and in vitro angiogenesis through a novel ERK-NFκB-cMyc-p21 pathway. Food Chem. 2012;130:321–328. doi: 10.1016/j.foodchem.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 17.Dagher Z, Park YS, Asnaghi V, Hoehn T, Gerhardinger C, Lorenzi M. Studies of rat and human retinas predict a role for the polyol pathway in human diabetic retinopathy. Diabetes. 2004;53:2404–2411. doi: 10.2337/diabetes.53.9.2404. [DOI] [PubMed] [Google Scholar]
- 18.Yuan L, Hu J, Luo Y, Liu Q, Li T, Parish CR, Freeman C, Zhu X, Ma W, Hu X, et al. Upregulation of heparanase in high-glucose-treated endothelial cells promotes endothelial cell migration and proliferation and correlates with Akt and extracellular-signal-regulated kinase phosphorylation. Mol Vis. 2012;18:1684–1695. [PMC free article] [PubMed] [Google Scholar]
- 19.Chen X, Li J, Li M, Zeng M, Li T, Xiao W, Li J, Wu Q, Ke X, Luo D, et al. KH902 suppresses high glucose-induced migration and sprouting of human retinal endothelial cells by blocking VEGF and PIGF. Diabetes Obes Metab. 2013;15:224–233. doi: 10.1111/dom.12008. [DOI] [PubMed] [Google Scholar]
- 20.Chen Z, Liu G, Xiao Y, Lu P. Adrenomedullin22-52 suppresses high-glucose-induced migration, proliferation, and tube formation of human retinal endothelial cells. Mol Vis. 2014;20:259–269. [PMC free article] [PubMed] [Google Scholar]
- 21.Hayashi JN, Ito H, Kanayasu T, Asuwa N, Morita I, Ishii T, Murota S. Effects of glucose on migration, proliferation and tube formation by vascular endothelial cells. Virchows Arch B Cell Pathol Incl Mol Pathol. 1991;60:245–252. doi: 10.1007/BF02899553. [DOI] [PubMed] [Google Scholar]
- 22.Premanand C, Rema M, Sameer MZ, Sujatha M, Balasubramanyam M. Effect of curcumin on proliferation of human retinal endothelial cells under in vitro conditions. Invest Ophthalmol Vis Sci. 2006;47:2179–2184. doi: 10.1167/iovs.05-0580. [DOI] [PubMed] [Google Scholar]
- 23.Zou C, Yu S, Xu Z, Wu D, Ng CF, Yao X, Yew DT, Vanacker JM, Chan FL. ERRalpha augments HIF-1 signalling by directly interacting with HIF-1α in normoxic and hypoxic prostate cancer cells. J Pathol. 2014;233:61–73. doi: 10.1002/path.4329. [DOI] [PubMed] [Google Scholar]
- 24.Arany Z, Foo SY, Ma Y, Ruas JL, Bommi-Reddy A, Girnun G, Cooper M, Laznik D, Chinsomboon J, Rangwala SM, et al. HIF-independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC-1alpha. Nature. 2008;451:1008–1012. doi: 10.1038/nature06613. [DOI] [PubMed] [Google Scholar]
- 25.Cao D, Zhou H, Zhao J, Jin L, Yu W, Yan H, Hu Y, Guo T. PGC-1α integrates glucose metabolism and angiogenesis in multiple myeloma cells by regulating VEGF and GLUT-4. Oncol Rep. 2014;31:1205–1210. doi: 10.3892/or.2014.2974. [DOI] [PubMed] [Google Scholar]
- 26.Liang F, Han Y, Gao H, Xin S, Chen S, Wang N, Qin W, Zhong H, Lin S, Yao X, Li S. Kaempferol identified by zebrafish assay and fine fractionations strategy from dysosma versipellis inhibits angiogenesis through VEGF and FGF pathways. Sci Rep. 2015;5:14468. doi: 10.1038/srep14468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Betts-Obregon BS, Vellanki S, Buikema J, Tsin AT, Wright K. Effect of glucose on retinal endothelial cell viability and VEGF secretion. HSOA J Cell Biol Cell Metabol. 2016;3 pii: 008. [PMC free article] [PubMed] [Google Scholar]
- 28.DiPietro LA, Nebgen DR, Polverini PJ. Downregulation of endothelial cell thrombospondin 1 enhances in vitro angiogenesis. J Vasc Res. 1994;31:178–185. doi: 10.1159/000319585. [DOI] [PubMed] [Google Scholar]
- 29.Sun Y, Huang J, Yang Z. The roles of ADAMTS in angiogenesis and cancer. Tumour Biol. 2015;36:4039–4051. doi: 10.1007/s13277-015-3461-8. [DOI] [PubMed] [Google Scholar]
- 30.Lee NV, Sato M, Annis DS, Loo JA, Wu L, Mosher DF, Iruela-Arispe ML. ADAMTS1 mediates the release of antiangiogenic polypeptides from TSP1 and 2. EMBO J. 2006;25:5270–5283. doi: 10.1038/sj.emboj.7601400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krampert M, Kuenzle S, Thai SN, Lee N, Iruela-Arispe ML, Werner S. ADAMTS1 proteinase is up-regulated in wounded skin and regulates migration of fibroblasts and endothelial cells. J Biol Chem. 2005;280:23844–23852. doi: 10.1074/jbc.M412212200. [DOI] [PubMed] [Google Scholar]