Abstract
Spondyloarthritis is a chronic inflammatory disease predominantly affecting joints of the axial skeleton. However, as many as 50% of patients with this disease may have extra-articular manifestations, which include uveitis; psoriasis; inflammatory bowel disease such as Crohn disease or ulcerative colitis; cardiovascular manifestations in the form of conduction abnormalities, atherosclerosis, or valvular heart disease; pulmonary involvement; and rarely renal involvement. Uveitis occurs in 25% to 40% of patients with spondyloarthritis. Management of uveitis is crucial to prevent morbidity caused by vision loss and secondary complications. Treatment ranges from local therapies to systemic drugs and varies depending on the severity and response to treatment. Categories of medical treatment include nonsteroidal anti-inflammatory agents, corticosteroids, and steroid-sparing agents. Biologic therapies such as antitumor necrosis factor agents act early in the disease process and have revolutionized the field of rheumatology, including management of uveitis. This review will focus on the management of ophthalmic manifestations in spondyloarthropathies.
INTRODUCTION
Spondyloarthritis (SpA) is a group of relatively common rheumatic diseases, with a prevalence of 1.5% to 2% in the general population.1,2 SpA constitutes ankylosing spondylitis, psoriatic arthritis, arthritis accompanying inflammatory bowel disease (eg, Crohn disease and ulcerative colitis), and reactive arthritis. Although SpA is mainly limited to joints, other organ systems of the human body can be involved. These extra-articular manifestations can involve the heart, lung, kidney, eye (uveitis), skin (psoriasis), gut, and nerves.1 The related manifestations can occur at anytime during the course of the disease or can be the presenting symptom, which is fairly common (20%–60%).3
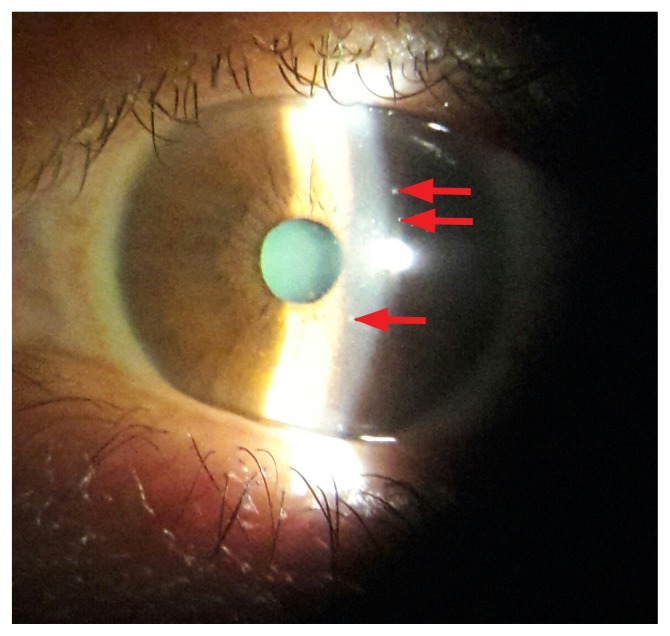
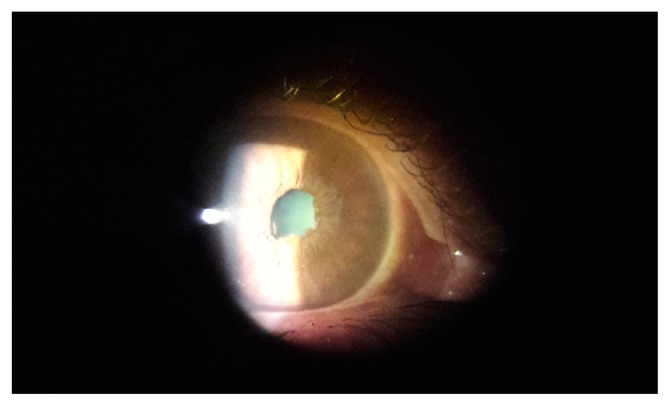
The term uveitis means any inflammation that affects the uveal tract (iris, ciliary body, and choroid). Uveitis can be broadly categorized as anterior uveitis, intermediate uveitis, posterior uveitis, or panuveitis. Anterior uveitis is the most frequently observed extra-articular manifestation of SpA and can be seen in up to 40% of patients.4 Unlike uveitis associated with spondyloarthropathies that are primarily unilateral, the phenotype of uveitis associated with inflammatory bowel disease and psoriatic arthritis is often bilateral. Uveitis related to SpA is acute in onset, unilateral, and recurrent and generally resolves without any sequelae when treated. Symptoms of uveitis include red eye, pain, photophobia, increased lacrimation, and visual blurring. On slit-lamp examination, iridocyclitis findings include keratic precipitates (Figure 1) along the endothelial surface of the cornea and cells in the anterior chamber. If treated, these precipitates resolve without any sequelae. However, uveitis has a chronic course if untreated and can lead to the following complications: Posterior synechiae (Figure 2), low visual acuity, cataract, secondary glaucoma, cystoid macular edema (CME), vitreitis, papillitis, and retinal vasculitis.5,6 Treatment options for uveitis include local as well as systemic therapies.
Figure 1.
Keratic precipitates (arrows).
Figure 2.
Posterior synechiae.
EARLY DETECTION AND PREVENTION
When the presentation of uveitis is acute, early detection of the disease is possible. However, chronic forms of anterior uveitis are often asymptomatic and detected late. Regular eye check-ups can prevent vision-threatening complications of chronic anterior uveitis. A rheumatologist’s opinion should be obtained when systemic disease is suspected.
TREATMENT OPTIONS FOR UVEITIS IN SPONDYLOARTHRITIS
The goal of treatment of uveitis in SpA is resolution of symptoms by control of inflammation. In most cases, acute uveitis can resolve with treatment with local corticosteroids and mydriatics. If the symptoms do not resolve, an intraocular corticosteroid injection or a high oral dosage of prednisone (up to 60 mg daily) is required.
Treatment options can be divided into the following:
Topical therapies
Periocular corticosteroid injections
Intraocular (intravitreal) corticosteroids
Systemic nonsteroidal anti-inflammatory drugs (NSAIDs)
Systemic corticosteroids
Immunosuppressive drugs
Biologic therapy.
Topical Therapies
Topical corticosteroids are the first medicines to be used, in the form of eye drops or ointment. The ideal topical corticosteroid has properties of high anti-inflammatory activity and easy intraocular penetration.
Topical corticosteroids that are commonly used include the following:
Dexamethasone sodium phosphate and 0.1% alcohol solution, suspension, or ointment
Prednisolone acetate, 0.5% and 1% suspension
Fluorometholone and 0.1% alcohol suspension or ointment
Rimexolone, 1% suspension
Loteprednoletabonate, 0.5% suspension
Hydrocortisone acetate, 1% ointment
Fludrocortisone acetate, 0.1% ointment.
The dosage of administration may be a drop every 1 hour to 3 hours depending on severity (for severe inflammation, 1 drop is administered every 15 minutes to 30 minutes).7,8 Topical corticosteroids should be used with caution in patients with a history of intraocular infection.
Common complications of topical corticosteroids include transient or permanent elevation of intraocular pressure in susceptible individuals (glaucoma) and hastened cataract formation. Topical mydriatics are very useful and help by 1) relieving pain and photophobia by immobilizing the iris and 2) preventing adhesion of the iris to the anterior lens capsule (posterior synechiae), which can lead to elevated intraocular pressure and may lead to glaucoma.9
Corticosteroids selected by the ophthalmologist depends on the desired potency, ocular penetration of the medication, and its risk for intraocular pressure elevation from steroid response.
Mydriatic agents useful in the treatment of anterior uveitis include the following anticholinergic agents (sphincter muscle paralysis):
Atropine, 0.5%, 1%, and 2%
Homatropine, 2% and 5%
Scopolamine, 0.25%
Cyclopentolate, 0.5%, 1%, and 2%, and an adrenergic agonist (acting on the dilator muscle)
Phenylephrine, 2.5% and 10%.
Topical NSAIDs are another treatment option for uveitis. Although they have less potent anti-inflammatory properties than do corticosteroids, they have a possible role as adjunctive therapy.
Topical NSAIDs include the following:
Flurbiprofen, 0.03% solution
Diclofenac sodium, 0.1% solution
Ketorolac, 0.5% solution
Indomethacin, 0.5 to 1.0% suspension.
Periocular Corticosteroid Injections
Periocular corticosteroid infiltration may be used in conditions when uveitis is associated with CME, in a noncompliant patient, or for very severe flare-ups with slow response to intensive topical treatment. (From 13% to 19% of the human leukocyte antigen-B27-positive uveitis cases are refractory to topical corticosteroids.) In some patients, uveitis may progress to a chronic condition. In this situation, periocular corticosteroid injection may be preferred to systemic corticosteroids.10 The approach used is either an inferior approach (orbital floor) or posterior sub-Tenon injection of depot steroid preparations (eg, triamcinolone acetonide, methylprednisolone acetate). Sen et al11 conducted a study that looked at effects and complications of periocular corticosteroid injections in uveitis. They found that periocular injections were effective in treating active intraocular inflammation, and the injections improved the reduced visual acuity attributed to macular edema in most patients. However, glaucoma is a potential complication of this technique, which is reported in up to 23% of patients receiving this treatment. Other possible complications include cataract formation, but this is less common than with systemic steroid administration.
Intraocular (Intravitreal) Corticosteroids
The intraocular route of steroid administration is used in the following cases: 1) anterior uveitis with CME unresponsive to other forms of therapy12 and 2) at the time of intraocular surgery in patients with high-risk anterior uveitis.
Intravitreal injection of triamcinolone acetonide in the dose of 4mg in 0.1mL is used.
Sustained-release fluocinolone implant, approved by the US Food and Drug Administration in 2005, can be used in the treatment of chronic noninfectious posterior uveitis.13 After its use, inflammation was well controlled in nearly all eyes after 34 weeks, and recurrence rates decreased by 90%, with 77% of patients able to discontinue systemic therapy and 96% able to discontinue treatment with local corticosteroid injections. Almost all phakic eyes developed cataract within 2 years after implantation. Glaucoma was seen in almost 75% of patients after 3 years, and 37% required filtering surgery. In the recently completed Multicenter Uveitis Steroid Treatment (MUST) trial, which is a 7-year extended follow-up of a randomized trial of patients with severe intermediate uveitis, posterior uveitis, or panuveitis, fluocinolone implant was compared with standard systemic therapy, which showed that systemic therapy had better visual acuity than those who received intravitreous fluocinolone acetonide implants.14 Thus systemic anti-inflammatory therapy is better than intravitreous fluocinolone acetonide implants in managing patients with uveitis.15,16 A biodegradable intraocular implant (Ozurdex) containing 700 μg of dexamethasone, approved by the US Food and Drug Administration, is used only for the treatment of macular edema caused by retinal vein occlusion.17 Preliminary study results suggest efficacy in the treatment of uveitic CME.17
Systemic Nonsteroidal Anti-Inflammatory Drugs
If the inflammation is mild and not controlled by topical agents, systemic NSAIDs are an additional option in management of uveitis. These medications reduce inflammation by inhibiting prostaglandins. Additionally, NSAIDs may reduce inflammation associated with CME (may accompany anterior uveitis).18 Fiorelli et al19 concluded from their study results that attacks of uveitis can be prevented, and the cumulative dose of steroids can be decreased with systemic NSAID therapy in patients with recurrent uveitis. Side effects of NSAIDs include stomach pain and heartburn; stomach ulcers; allergic reactions such as rashes, wheezing, and throat swelling; and liver or kidney problems.
Systemic Corticosteroids
Systemic corticosteroids are useful in situations of uveitis refractory to topical agents or NSAIDs and in cases of severe uveitis requiring immediate control of inflammation. High-dose oral steroids (1 mg/kg) may be used to suppress the inflammation initially, followed by a taper of the dosage. If the disease relapses using a tapering dosage of steroids or requires more than 10 mg of prednisone daily, immunosuppressive therapy should be considered. In a study by Howe et al,20 patients with uveitis required at least 12 months of steroid therapy for maintenance of remission of uveitis, and steroid therapy was associated with a high incidence (50%) of side effects. Also, 40% of those patients required steroid-sparing agents. Side effects of steroids include acne, blurred vision, cataracts, glaucoma, weight gain, and increased growth of body hair.
Immunosuppressive Therapy
Immunosuppressive therapy may be used in cases of recurrence of uveitis when the steroid dosage is tapered or when used as steroid-sparing agents. Before the start of therapy, the patient’s age, associated medical conditions, and type of family planning in both sexes must be assessed carefully.21
Indications for immunosuppressive agents (steroid sparing) in uveitis include the following:
Steroid-sparing therapy when the side effects of steroids are high
Uveitis nonresponsive to steroids
Uveitis in specific diseases, such as granulomatosis with polyangiitis, Behçet disease, and Vogt-Koyanagi Harada syndrome.
Various immunosuppressive drugs that can be useful in uveitis include methotrexate, mycophenolate mofetil, azathioprine, cyclosporine, tacrolimus, and cyclophosphamide. Methotrexate blocks the formation of purines and pyrimidines within the cell, thus inhibiting cell growth. It also induces T-cell apoptosis, modifies the B-cell response, and inhibits cytokine production. In a study by Samson et al,22 it was found that methotrexate could control uveitis in 76% of patients at a mean dose of 12.3 mg/wk.
In a multicenter retrospective study called Systemic Immunosuppressive Therapy for Eye Diseases (SITE), 384 patients were treated with methotrexate or cyclosporine for inflammatory eye disease including uveitis.23 It was found that 66% of patients receiving methotrexate and 52% on a regimen of cyclosporine achieved complete remission of inflammation, including uveitis within a year while allowing a dose reduction of oral steroids. Thus, this study suggests that methotrexate is more effective than cyclosporine in managing uveitis. However, methotrexate is also associated with some adverse effects, such as mouth ulcers, diarrhea, bone marrow suppression, and liver problems (eg, drug-induced hepatitis).
A review published by Hesselink and associates24 concluded that cyclosporine is an effective second-line agent but should be used with caution because of its high incidence of adverse effects.
In evidence by case reports of six patients with posterior uveitis treated with tacrolimus, Sloper and colleagues25 concluded that tacrolimus is useful in the treatment of sight-threatening posterior uveitis resistant to cyclosporine therapy.
Mycophenolate mofetil has been shown to be useful in management of uveitis. In the SITE study, 236 patients with ocular inflammation including uveitis received mycophenolate mofetil; 73% achieved control of inflammation (including uveitis) within 1 year, and 55% experienced a steroid-sparing effect.26
Similar results were seen with azathioprine in the SITE study.27 Of 145 patients treated with azathioprine, 62% achieved inflammation control, and 47% experienced a steroid-sparing effect. Azathioprine was most useful in patients with intermediate uveitis.
The SITE study also demonstrated that 76% of 215 patients receiving cyclophosphamide achieved control of ocular inflammation, with 61% demonstrating a steroid-sparing effect.28
Side effects of immunosuppressants include infection, sterility with alkylating agents, hypertension, dyslipidemia, renal dysfunction, and bone marrow suppression.
Biologic Therapy
Biologic medicines are a relatively newer group of medications that have revolutionized the management of SpA and have also been useful in the treatment of uveitis. These drugs target cytokines or their inflammatory signaling pathways. Biologics are useful in treating refractory uveitis.
Biologics, especially tumor necrosis factor (TNF) inhibitors, have shown remarkable results in the treatment of uveitis. The various TNF blockers that are available include golimumab, infliximab, etanercept, adalimumab, and certolizumab. Biosimilar molecules are also available as Infimab (biosimilar of infliximab), Exemptia or Adfrar (biosimilar of adalimumab), and Intacept or Etacept (biosimilar of etanercept).
Infliximab is a chimeric monoclonal antibody that acts on both circulating and membrane-bound TNF-α. In the treatment of uveitis in ankylosing spondylitis, the TNF inhibitors infliximab and adalimumab decrease the rate of recurrences and reduce the incidence of uveitis.29–31 Infliximab has been shown to be highly efficacious in uveitis in patients with juvenile idiopathic arthritis (JIA), as demonstrated in retrospective studies.32,33
An observational study of golimumab in SpA-associated refractory uveitis has shown positive results.34
It is important to note that etanercept is not associated with improvement in inflammatory uveitis. In 2006, Guignard et al35 showed that etanercept was ineffective in the treatment of uveitis. In a prospective, open-label, multicenter study (median = 13 months), patients with JIA and uveitis initially responded to etanercept36; however, only half of respondents had sustained improvement at 1 year. It was found that etanercept was associated with severe side effects that disappeared after discontinuation of etanercept therapy.
Adalimumab is a fully human monoclonal anti-TNF-α antibody. A prospective, nonrandomized study in 14 children with recalcitrant uveitis found improvement of anterior uveitis in 81% of patients with JIA.37
There have been reports of exacerbation of uveitis with TNF blockers, especially etanercept. A French national surveillance and English case reports have reported the association between TNF-α inhibitors and uveitis, with 31 and 121 cases, respectively. In these series, etanercept was associated with new-onset uveitis in 23 cases (74%) and 103 cases (85%), respectively.38 There were also 3 cases of new-onset uveitis with adalimumab therapy and 5 cases with infliximab therapy.39
Abatacept, a fusion molecule that inhibits costimulation, has also been shown to control uveitis; however, the data are limited to case reports and case series only.40
Because rituximab and intravenous immunoglobulins have been shown to be useful in refractory uveitis in Behçet disease41 and JIA,42 they may be effective in uveitic patients with SpA.
The effectiveness of other biologics, such as interleukin-17 inhibitors, must be tested. Tocilizumab, an interleukin-6 inhibitor, has been demonstrated to control refractory uveitis of various causes, including JIA and Behçet disease.43,44
Use of biologic therapy in patients with noninfectious uveitis can be in the group of patients with an inadequate response to or tolerance to conventional immunotherapy.
Side effects of biologic therapy include the risk of allergic reactions (including anaphylaxis, which may be life-threatening), infusion reactions, risk of worsening infection, and reactivation of old infections such as tuberculosis or diseases such as multiple sclerosis, and can even lead to lymphoma.
CONCLUSION
Uveitis is a relatively common extra-articular manifestation of SpA. An ophthalmology referral should be sought by the treating rheumatologist, and collaboration must begin as early as possible to diagnose and treat associated eye manifestations such as uveitis, which may be refractory to topical therapy. Systemic corticosteroids, immunosuppressive drugs, or biologics in various combinations may be required to induce remission. The prognosis is usually excellent with topical treatment alone for acute anterior uveitis; however, topical corticosteroids have limited penetration in the treatment of posterior uveitis. The indications for immunosuppressive drugs are typically refractory uveitis, involvement of the posterior pole, or high tendency toward recurrence or chronicity. CME may be a posterior pole finding but does not signify posterior uveitis, so CME is not an indication for prescribing immunosuppressive agents.
Universe
Who would believe that so small a space could contain the images of all the universe?
— Leonardo da Vinci, 1452–1519, Italian Renaissance polymath
Acknowledgment
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Poddubnyy D, Rudwaleit M. Early spondyloarthritis. Rheum Dis Clin North Am. 2012 May;38(2):387–403. doi: 10.1016/j.rdc.2012.04.007. DOI: https://doi.org/10.1016/j.rdc.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Helmick CG, Felson DT, Lawrence RC, et al. National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part 1. Arthritis Rheum. 2008 Jan;58(1):15–25. doi: 10.1002/art.23177. DOI: https://doi.org/10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- 3.Carron P, Van Praet L, Jacques P, Elewaut D, Van den Bosch F. Therapy for spondyloarthritis: The role of extra-articular manifestations (eye, skin) Rheum Dis Clin North Am. 2012 Aug;38(3):583–600. doi: 10.1016/j.rdc.2012.08.017. DOI: https://doi.org/10.1016/j.rdc.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 4.Martin TM, Smith JR, Rosenbaum JT. Anterior uveitis: Current concepts of pathogenesis and interactions with the spondyloarthropathies. Curr Opin Rheumatol. 2002 Jul;14(4):337–41. doi: 10.1097/00002281-200207000-00001. DOI: https://doi.org/10.1097/00002281-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol. 2005 Jul-Aug;50(4):364–88. doi: 10.1016/j.survophthal.2005.04.003. DOI: https://doi.org/10.1016/j.survophthal.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez A, Akova YA, Pedroza-Seres M, Foster CS. Posterior segment ocular manifestations in patients with HLA-B27-associated uveitis. Ophthalmology. 1994 Jul;101(7):1267–74. doi: 10.1016/s0161-6420(94)31179-1. DOI: https://doi.org/10.1016/s0161-6420(94)31179-1. [DOI] [PubMed] [Google Scholar]
- 7.Muñoz-Fernández S, Martín-Mola E. Uveitis. Best Pract Res Clin Rheumatol. 2006 Jun;20(3):487–505. doi: 10.1016/j.berh.2006.03.008. DOI: https://doi.org/10.1016/j.berh.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Havener WH. Ocular pharmacology. 5th ed. St Louis, MO: CV Mosby; 1983. pp. 383–5. [Google Scholar]
- 9.Trevisani VF, Mattos KT, Esteves RF, Olialves SM, Andrade LE. Autoantibodies specificity in acute anterior uveitis according to the presence of the HLA-B27 allele. Ocul mmunol nflamm. 2001 Dec;9(4):231–42. doi: 10.1076/ocii.9.4.231.3952. DOI: https://doi.org/10.1076/ocii.9.4.231.3952. [DOI] [PubMed] [Google Scholar]
- 10.Catania LJ. Primary care of the anterior segment. 2nd ed. Norwalk, CT: Appleton & Lange; 1995. pp. 371–2. [Google Scholar]
- 11.Sen HN, Vitale S, Gangaputra SS, et al. Periocular corticosteroid injections in uveitis: Effects and complications. Ophthalmology. 2014 Nov;121(11):2275–86. doi: 10.1016/j.ophtha.2014.05.021. DOI: https://doi.org/10.1016/j.ophtha.2014.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Androudi S, Letko E, Meniconi M, Papadaki T, Ahmed M, Foster CS. Safety and efficacy of intravitreal triamcinolone acetonide for uveitic macular edema. Ocul mmunol nflamm. 2005 Apr-Jun;13(2–3):205–12. doi: 10.1080/09273940590933511. DOI: https://doi.org/10.1080/09273940590933511. [DOI] [PubMed] [Google Scholar]
- 13.Jaffe GJ. Reimplantation of a fluocinoloneacetonide sustained drug delivery implant for chronic uveitis. Am J Ophthalmol. 2008 Apr;145(4):667–75. doi: 10.1016/j.ajo.2007.11.008. DOI: https://doi.org/10.1016/j.ajo.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Multicenter Uveitis Steroid Treatment Trial Research Group. Kempen JH, Altaweel MM, Holbrook JT, Jabs DA, Sugar EA. The multicenter uveitis steroid treatment trial: Rationale, design, and baseline characteristics. Am J Ophthalmol. 2010 Apr;149(4):550–61. doi: 10.1016/j.ajo.2009.11.019. DOI: https://doi.org/10.1016/j.ajo.2009.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sugar EA, Venugopal V, Thorne JE, et al. Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group. Ophthalmology. 2017 Nov;124(11):1662–9. DOI: https://doi.org/10.1016/j.ophtha.2017.05.015. [Google Scholar]
- 16.Writing Committee for the Multicenter Uveitis Steroid Treatment (MUST) Trial and Follow-up Study Research Group. Kempen JH, Altaweel MM, Holbrook JT, Sugar EA, Thorne JE, Jabs DA. Association between long-lasting intravitreous fluocinolone acetonide implant vs systemic anti-inflammatory herapy and visual acuity at 7 years among patients with intermediate, posterior, or panuveitis. JAMA. 2017 May 16;317(19):1993–2005. doi: 10.1001/jama.2017.5103. DOI: https://doi.org/10.1001/jama.2017.5103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kupperman BD, Blumenkranz MS, Haller JA, et al. Randomized controlled study of an intravitreous dexamethasone drug delivery system in patients with persistent macular edema. Arch Ophthalmol. 2007 Mar;125(3):309–17. doi: 10.1001/archopht.125.3.309. DOI: https://doi.org/10.1001/archopht.125.3.309. [DOI] [PubMed] [Google Scholar]
- 18.Foster CS, Vitale AT. Diagnosis and treatment of uveitis. 2nd ed. New Delhi, India: Jaypee Brothers Medical Publishers Ltd; 2013. [Google Scholar]
- 19.Fiorelli VM, Bhat P, Foster CS. Nonsteroidal anti-inflammatory therapy and recurrent acute anterior uveitis. Ocul mmunol nflamm. 2010 Apr;18(2):116–20. doi: 10.3109/09273941003587558. DOI: https://doi.org/10.3109/09273941003587558. [DOI] [PubMed] [Google Scholar]
- 20.Howe LJ, Stanford MR, Edelsten C, Graham EM. The efficacy of systemic corticosteroids in sight-threatening retinal vasculitis. Eye (Lond) 1994;8(Pt 4):443–7. doi: 10.1038/eye.1994.105. DOI: https://doi.org/10.1038/eye.1994.105. [DOI] [PubMed] [Google Scholar]
- 21.Siddique SS, Shah R, Suelves AM, Foster CS. Road to remission: A comprehensive review of therapy in uveitis. Expert Opin Investig Drugs. 2011 Nov;20(11):1497–515. doi: 10.1517/13543784.2011.617741. DOI: https://doi.org/10.1517/13543784.2011.617741. [DOI] [PubMed] [Google Scholar]
- 22.Samson CM, Waheed N, Baltatzis S, Foster CS. Methotrexate therapy for chronic noninfectious uveitis: Analysis of a case series of 160 patients. Ophthalmology. 2001 Jun;108(6):1134–9. doi: 10.1016/s0161-6420(01)00576-0. DOI: https://doi.org/10.1016/s0161-6420(01)00576-0. [DOI] [PubMed] [Google Scholar]
- 23.Gangaputra S, Newcomb CW, Liesegang TL, et al. Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study. Methotrexate for ocular inflammatory diseases. Ophthalmology. 2009 Nov;116(11):2188–98.e1. doi: 10.1016/j.ophtha.2009.04.020. DOI: https://doi.org/10.1016/j.ophtha.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hesselink DA, Baarsma GS, Kuijpers RW, van Hagen PM. Experience with cyclosporine in endogenous uveitis posterior. Transplant Proc. 2004 Mar;36(2 Suppl):372S–377S. doi: 10.1016/j.transproceed.2004.01.003. DOI: https://doi.org/10.1016/j.transproceed.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Sloper CM, Powell RJ, Dua HS. Tacrolimus (FK506) in the treatment of posterior uveitis refractory to cyclosporine. Ophthalmology. 1999 Apr;106(4):723–8. doi: 10.1016/S0161-6420(99)90156-2. DOI: https://doi.org/10.1016/s0161-6420(99)90156-2. [DOI] [PubMed] [Google Scholar]
- 26.Daniel E, Thorne JE, Newcomb CW, et al. Mycophenolatemofetil for ocular inflammation. Am J Ophthalmol. 2010 Mar;149(3):423–32.e1–2. doi: 10.1016/j.ajo.2009.09.026. DOI: https://doi.org/10.1016/j.ajo.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang JJ, Gaudio PA. Ocular inflammatory disease and uveitis manual: Diagnosis and treatment. Baltimore, MD: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 28.Pujari SS, Kempen JH, Newcomb CW, et al. Cyclophosphamide for ocular inflammatory diseases. Ophthalmology. 2010 Feb;117(2):356–65. doi: 10.1016/j.ophtha.2009.06.060. DOI: https://doi.org/10.1016/j.ophtha.2009.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levy-Clarke G, Nussenblatt R. Does anti-TNF therapy decrease the incidence of anterior uveitis in patients with ankylosing spondylitis? Nat Clin Pract Rheumatol. 2006 Feb;2(2):72–3. doi: 10.1038/ncprheum0097. DOI: https://doi.org/10.1038/ncprheum0097. [DOI] [PubMed] [Google Scholar]
- 30.van der Horst-Bruinsma IE, Nurmohamed MT. Management and evaluation of extra-articular manifestations in spondyloarthritis. Ther Adv Musculoskelet Dis. 2012 Dec;4(6):413–22. doi: 10.1177/1759720X12458372. DOI: https://doi.org/10.1177/1759720x12458372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braun J, Baraliakos X, Listing J, Sieper J. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheum. 2005 Aug;52(8):2447–51. doi: 10.1002/art.21197. DOI: https://doi.org/10.1002/art.21197. [DOI] [PubMed] [Google Scholar]
- 32.Rajaraman RT, Kimura Y, Li S, Haines K, Chu DS. Retrospective case review of pediatric patients with uveitis treated with infliximab. Ophthalmology. 2006 Feb;113(2):308–14. doi: 10.1016/j.ophtha.2005.09.037. DOI: https://doi.org/10.1016/j.ophtha.2005.09.037. [DOI] [PubMed] [Google Scholar]
- 33.Tynjälä P, Lindahl P, Honkanen V, Lahdenne P, Kotaniemi K. Infliximab and etanercept in the treatment of chronic uveitis associated with refractory juvenile idiopathic arthritis. Ann Rheum Dis. 2007 Apr;66(4):548–50. doi: 10.1136/ard.2006.058248. DOI: https://doi.org/10.1136/ard.2006.058248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miserocchi E, Modorati G, Pontikaki I, Meroni PL, Gerloni V. Long-term treatment with golimumab for severe uveitis. Ocul Immunol Inflamm. 2014 Apr;22(2):90–5. doi: 10.3109/09273948.2013.844265. DOI: https://doi.org/10.3109/09273948.2013.844265. Erratum in: Ocul Immunol Inflamm 2015 Jun;23(3):266. DOI: https://doi.org/10.3109/09273948.2015.1051909. [DOI] [PubMed] [Google Scholar]
- 35.Guignard S, Gossec L, Salliot C, et al. Efficacy of tumour necrosis factor blockers in reducing uveitis flares in patients with spondylarthropathy: A retrospective study. Ann Rheum Dis. 2006 Dec;65(12):1631–4. doi: 10.1136/ard.2006.052092. DOI: https://doi.org/10.1136/ard.2006.052092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quartier P, Taupin P, Bourdeaut F, et al. Efficacy of etanercept for the treatment of juvenile idiopathic arthritis according to the onset type. Arthritis Rheum. 2003 Apr;48(4):1093–101. doi: 10.1002/art.10885. DOI: https://doi.org/10.1002/art.10885. [DOI] [PubMed] [Google Scholar]
- 37.Vazquez-Cobian LB, Flynn T, Lehman TJ. Adalimumab therapy for childhood uveitis. J Pediatr. 2006 Oct;149(4):572–5. doi: 10.1016/j.jpeds.2006.04.058. DOI: https://doi.org/10.1016/j.jpeds.2006.04.058. [DOI] [PubMed] [Google Scholar]
- 38.Wendling D, Paccou J, Berthelot JM, et al. New onset of uveitis during anti-tumor necrosis factor treatment for rheumatic diseases. Semin Arthritis Rheum. 2011 Dec;41(3):503–10. doi: 10.1016/j.semarthrit.2011.05.005. DOI: https://doi.org/10.1016/j.semarthrit.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 39.Seider N, Beiran I, Scharf J, Miller B. Intravenous immunoglobulin therapy for resistant ocular Behçet’s disease. Br J Ophthalmol. 2001 Nov;85(11):1287–8. doi: 10.1136/bjo.85.11.1287. DOI: https://doi.org/10.1136/bjo.85.11.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wendling D, Paccou J, Berthelot JM, et al. CRI. New onset of uveitis during anti-tumor necrosis factor treatment for rheumatic diseases. Semin Arthritis Rheum. 2011 Dec;41(3):503–10. doi: 10.1016/j.semarthrit.2011.05.005. DOI: https://doi.org/10.1016/j.semarthrit.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Birolo C, Zannin ME, Arsenyeva S, et al. Comparable efficacy of abatacept used as first-line or second-line biological agent for severe juvenile idiopathic arthritis-related uveitis. J Rheumatol. 2016;43(11):2068–73. doi: 10.3899/jrheum.151389. DOI: https://doi.org/10.3899/jrheum.151389. [DOI] [PubMed] [Google Scholar]
- 42.Heiligenhaus A, Miserocchi E, Heinz C, Gerloni V, Kotaniemi K. Treatment of severe uveitis associated with juvenile idiopathic arthritis with anti-CD20 monoclonal antibody (rituximab) Rheumatology (Oxford) 2011 Aug;50(8):1390–4. doi: 10.1093/rheumatology/ker107. DOI: https://doi.org/10.1093/rheumatology/ker107. [DOI] [PubMed] [Google Scholar]
- 43.Tappeiner C, Heinz C, Ganser G, Heiligenhaus A. Is tocilizumab an effective option for treatment of refractory uveitis associated with juvenile idiopathic arthritis? J Rheumatol. 2012 Jun;39(6):1294–5. doi: 10.3899/jrheum.120010. DOI: https://doi.org/10.3899/jrheum.120010. [DOI] [PubMed] [Google Scholar]
- 44.Hirano T, Ohguro N, Hohki S, et al. A case of Behçet’s disease treated with a humanized anti-interleukin-6 receptor antibody, tocilizumab. Mod Rheumatol. 2012 Apr;22(2):298–302. doi: 10.1007/s10165-011-0497-5. DOI: https://doi.org/10.3109/s10165-011-0497-5. [DOI] [PubMed] [Google Scholar]