Abstract
Purpose
The apoptotic mechanisms responsible for secondary cone death in retinitis pigmentosa (RP) remain largely unknown. The cone-enriched apoptotic protease caspase-7 (Casp7) is thought to be triggered by endoplasmic reticulum (ER) stress and plays a pivotal role in mice deficient in the cone cyclic nucleotide-gated channels, a deficiency that causes achromatopsia in humans and in mice with autosomal dominant rhodopsin mutations, in particular the T17M mutation. Thus, we tested in two mouse models of RP whether the cone-enriched Casp7 plays a role during secondary cone death.
Methods
Casp7 knockout mice were crossed to two different RP mouse models with significantly different rod and cone death kinetics: the rd1 mouse model, which carries a mutation in the Pde6b gene, and the rhodopsin knockout mouse model (Rho-KO or Rho–/–). In both models, cone survival was assessed on retinal flat mounts by quantifying the percentage of cone arrestin staining over the retinal surface area. The analyses were performed at two different time points for each model.
Results
Loss of Casp7 did not alter cone survival in either of the two mouse models tested regardless of the time point analyzed. Rod survival was also not affected in either model nor did loss of Casp7 affect rod or cone function in a wild-type background as assessed with electroretinogram analyses.
Conclusions
Secondary cone death in retinitis pigmentosa is unlikely to be triggered by ER stress and is likely independent of Casp7 activity.
Introduction
Retinitis pigmentosa (RP) is an inherited photoreceptor degenerative disease that leads to blindness. The disease is often caused by mutations in rod photoreceptor (PR) specific genes resulting in initial loss of night vision. However, once a certain threshold of rod death is breached [1], secondary cone death follows leading to the loss of daylight, color, and high-acuity vision [2]. Understanding the underlying cause of secondary cone death may allow for the development of treatments that are applicable to all individuals with mutations in rod-specific genes. For example, the identification of a cell death mechanism could be exploited to prevent the execution of cone death itself.
Caspases belong to a family of cysteine proteases that control and execute apoptosis, which is a form of controlled cell death that leads to the removal of compromised cells within a tissue [3]. Caspases can be subdivided into initiator and executioner caspases and are generally activated by specific cell intrinsic or extrinsic signals or insults [4-6]. Thus, identifying a specific caspase as part of a cell death mechanism can give insights into the underlying cause for cell death. For example, we have previously proposed that secondary cone loss in RP is caused by a glucose and thus, NADPH, shortage in cones, which is elicited by structural changes induced by the loss of the overabundant rods [1]. By improving cell metabolism in cones through activation of the mammalian target of rapamycin complex 1 (mTORC1), we showed that cone survival is improved, and retinal NADPH levels are increased [1,7-10]. Consistent with that result, we found that loss of the NADPH-sensitive initiator Caspase-2 delays cone death in the rd1 mouse model of RP, a mouse model that carries a mutation in the rod PR specific phosphodiesterase 6-beta gene (PDE6b) [7,11]. Similarly, loss of the executioner Casp7 delays rod degeneration in the autosomal dominant Rhodopsin T17M mouse model of RP [12]. Interestingly, Casp7 is enriched in cones and expressed in the inner nuclear layer but is absent in adult rods [13]. However, in the case of the T17M mutant, which triggers endoplasmic reticulum (ER) stress and activation of the unfolded protein response (UPR), Casp7 is upregulated in rods [12,14]. Other autosomal dominant mutations in Rhodopsin, such as the S334ter and the P23H, have also been shown to lead to ER stress, yet the protective effect of loss of Casp7 in these mutants has not been tested [15,16]. Activation of Casp7 has also been shown to occur for some cone-specific mutations, such as mutations in cyclic nucleotide-gated channel subunits alpha 3 and beta 3 (CNGA3 and CNGB3) [17]. Mutation in either gene has also been associated with ER stress and activation of the UPR. The fact that Casp7 appears to be involved in rod and cone cell death when either cell experiences ER stress led us to test whether Casp7 may also play a role during the periods of secondary cone degeneration in RP, particularly because Casp7 is cone enriched and ER stress has been predicted to contribute to cone death in RP. Further, loss of caspase-2 did not completely prevent cone death; instead, the loss delayed cone death [7,13,18]. Thus, other yet unidentified cell death mechanisms are likely involved in triggering cone death in RP. Such a mechanism could involve ER stress–mediated activation of CASP7, because ER stress can also be triggered by increased oxidative stress, a condition known to be present during cone degeneration in RP and when alleviated, delays cone death [19-24].
Methods
Animals
All procedures involving animals were in compliance with the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research and were approved by the Institutional Animal Care and Use Committees (IACUC) of the University of Massachusetts Medical School. Animals were maintained on a 12 h:12 h light-dark cycle with unrestricted access to food and water. Lighting conditions were kept constant in all cages, with illumination ranging between 10 and 15 lux. The Pde6b–/– (rd1, FVB strain), C57BL/6J, Casp7–/–, and Casp2–/– mice were purchased from Jackson Laboratories (Bar Harbor, ME) [11,25,26]. Because the FVB strain that carries the rd1 mutation is albino, it was first backcrossed to C57BL/6J for ten generations to generate the rd1_C57BL/6J line [7]. The Casp7–/– was already on a C57BL/6J, and the Rho–/– mice, which have been described previously by Janis Lem [27], are also maintained on a C57BL/6J background. However, to avoid any possible strain background differences and to be able to directly compare littermates, we first generated heterozygous Casp7 siblings (F1: e.g., Casp7–/+_Rho–/–) that were then crossed to each other to obtain the two (e.g., Casp7–/–_Rho–/– versus Rho–/–) of the three possible different genetic combinations of the F2 cross that were then used for analysis. For the triple loss of function of Casp7–/–_Casp2–/–_rd1, we generated the desired genotype, analyzed the data at 20 weeks of age, and compared the data to our previously published data for the Casp2–/–_rd1 genotype [7]. Genotyping was performed as described in the original publications. All mice were genotyped for absence of the rd8 allele with a mutation in the Crumbs 1 gene [28]. Electroretinography (ERG) was performed using the Espion E3 console in conjunction with the Color Dome (both sold by Diagnosys LLC, Lowell, MA) as described previously [29] with a minimum of six animals per genotype and age.
Histological methods
Antibody stainings on retinal flat mounts were performed as described previously [7,30]. CASP7 activity on retinal whole mounts was detected using the FAM-FLICA Caspase 3 & 7 Assay Kit (Cat# 93) from ImmunoChemistry Technologies (Bloomington, MN) as previously described [7] following the manufacturer’s instructions. The following primary antibodies and concentrations were used: rabbit α-cone arrestin (1:500; Cat# 15,282) from EMD Millipore (Now: MilliporeSigma, Burlington, MA), fluorescein-labeled peanut agglutinin lectin (PNA; 1:500; Cat# FL-1071) from Vector Laboratories (Burlingame, CA), and α-cleaved caspase 3 (1:300; Cat# 9662) from Cell Signaling (Danvers, MA). Nuclei were counterstained with 4´,6-diamidino-2-phenylindole (DAPI; Cat# 9542) from Sigma-Aldrich (Now: MilliporeSigma, Burlington, MA). All secondary antibodies (donkey) were purchased from Jackson ImmunoResearch (West Grove, PA) and were purified F(ab)2 fragments that displayed minimal cross-reactivity with other species. Quantification of cone survival was performed as previously described by calculating the surface area of the retina that is covered by the cone arrestin signal versus the entire retinal surface area to extrapolate the percentage of cone survival [1,7,9,31]. A minimum of six animals were used per genotype and age. Colocalization between the cone arrestin staining and the retinal surface area was calculated using CoLocalizer Pro software [32]. All images were acquired on a Leica DM5500 fluorescence microscope Leica (US Branch: Buffalo Grove, IL) equipped with an automated stage for tiling.
Molecular biology and cell culture methods
Protein extractions and western blot analysis were performed as described previously [7]. The following primary antibodies were used: rabbit α-caspase-7 (1:1,000; Cat# 9492) from Cell Signaling and mouse α-β-actin (1:2,000; Cat# A5316) from Sigma. To clone the Casp7 cDNA for overexpression Casp7 was amplified by PCR (For: 5’-GCG GCC GCC ACC ATG ACC GAT GAT CAG GAC TG-3’; Rev: 5’-CTA ACG GCT GAA GTA CAG CT-3’; PCR conditions: 95˚C for 2’; 25 times: 95˚C for 15’’, 53˚C for 30’’, 68˚C for 1’) with TaKaRa (US Branch: Mountain View, CA) LA Taq (Cat# RR002A) from a C57BL/6J retinal cDNA library that was generated as previously described [1]. The PCR product (994 bp) was sub-cloned into the p-GEMT-Easy vector (Cat# A1360) Promega (Madison, WI) and sequence verified. The Casp7 cDNA was then cloned into a recombinant adenoassociated virus (rAAV2) plasmid carrying a cytomegalovirus (CMV) promoter and the SV40 poly-adenylation site. The human embryonic kidney (HEK 293) cells were either treated with 100 nM rapamycin or transfected with Casp7 using PEI (Polyscience Inc, Warrington, PA; Cat# 23,966). For all conditions, cells were maintained in regular Dulbecco’s Modified Eagle Medium (DMEM; Cat# 11965092) containing 10% fetal bovine serum (FBS; Cat# 16140071) and a penicillin/streptomycin mixture (Cat# 15140122) all from Gibco by Life Technology (now Thermo Fisher Scientific; Grand Island, NY). Twelve hours post rapamycin treatment and 24 h post transfection with Casp7, protein extractions were performed as described [7].
Statistical analysis
The Student t test was used for statistical analyses. P values of less than 0.05 were considered statistically significant. None of the comparisons showed any statistically significant difference. All error bars represent the standard error of the mean (SEM).
Results
Loss of Casp7 does not affect rod and cone function in a wild-type background
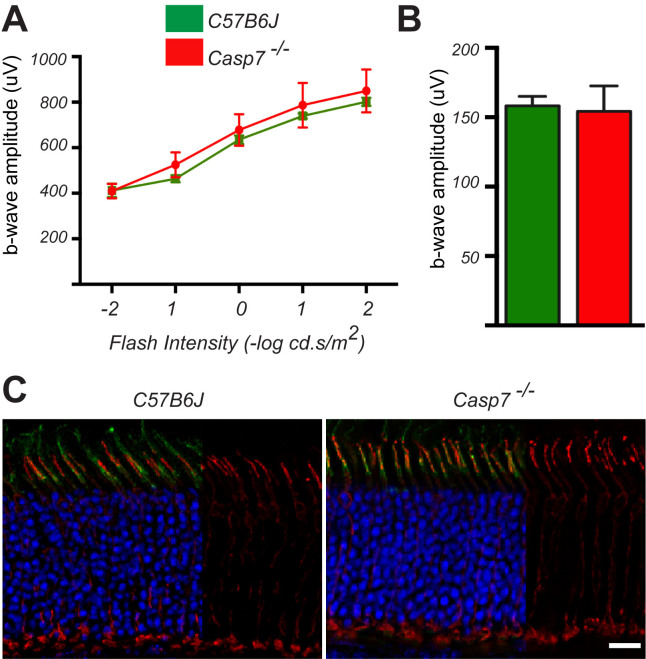
To study the long-term effect of Casp7 loss on secondary cone death in RP, we first assessed whether Casp7 loss alone has any negative effect on cones and rods in a wild-type background. The Casp-7–/– mice showed no appreciable difference in rod and cone function by 20 weeks of age when compared to the wild-type C57BL/6J mice (Figure 1A,B). The expression of cone-specific proteins, such as cone arrestin, was unchanged in the Casp7–/– mice, and the retinal structure appeared indistinguishable from that in the wild-type mice (Figure 1C) indicating that the loss of Casp7 has no overt effect on retinal development and function.
Figure 1.
Loss of Casp7 does not affect rod and cone function in a wild-type background. A, B: Electroretinogram (ERG) recordings at 20 weeks of age showing averages of b-wave amplitudes of scotopic ERGs over five different light intensities (A) and average of b-wave amplitudes of photopic ERGs (B) n=6 in A and B; Error bars: SEM. C: Immunofluorescence analysis on a cross section at 20 weeks of age showing normal expression of cone arrestin (red signal) and normal labeling of cone segment sheets with PNA (green signal). Blue: nuclear 4´,6-diamidino-2-phenylindole (DAPI). (Blue and green signals were removed from one third of each panel to better visualize the cone arrestin staining.) Scale bar: 20 μm.
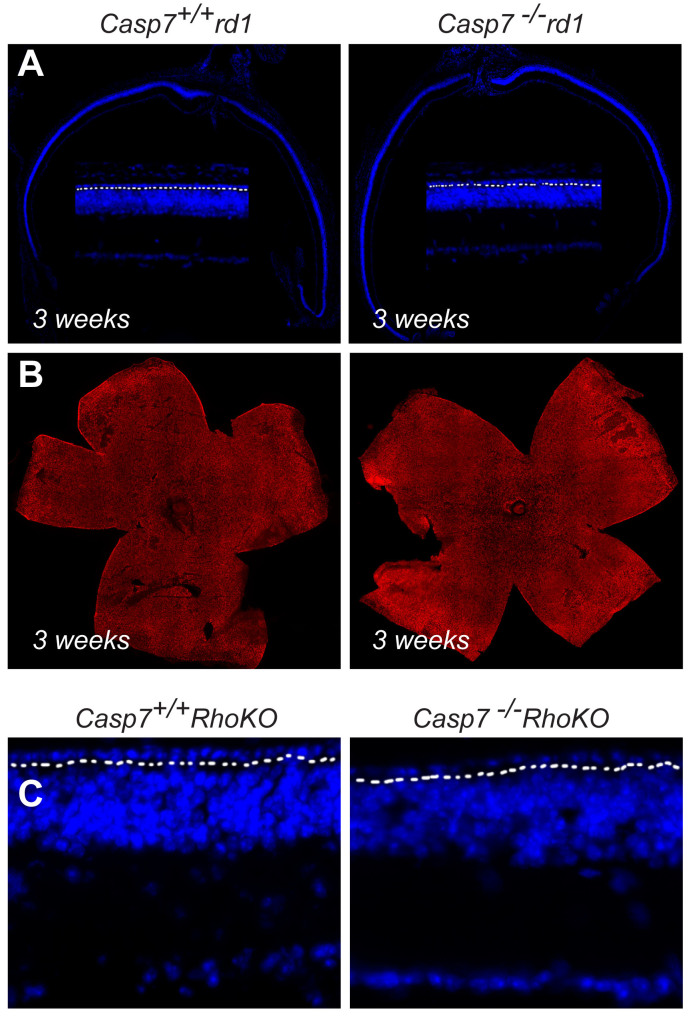
Casp7 loss does not alter rod survival in the rd1 and Rho-KO mouse models of RP
The endoplasmic reticulum stress induced Casp7 has been implicated in several autosomal dominant mouse models of RP [15,16], and the loss of this protein has been shown to delay rod death in the T17M rhodopsin mouse model of autosomal dominant RP [12]. Endoplasmic reticulum stress has also been proposed to contribute to retinal degeneration in the rd1 mouse model of retinal degeneration [18]. Because rod survival positively affects cone survival [1], we wanted to ensure that any effect of Casp7 loss on cones was not due to increased rod survival due to Casp7 loss in rods. Thus, we analyzed rod survival in rd1 and Rho-KO mice lacking Casp7 at 3 and 17 weeks of age, respectively. These time points were chosen as they coincide with the onset of cone death in these two mouse models of RP [1]. Therefore, any substantial increase in the number of surviving rods at the onset of cone death would inevitably delay cone death. Because at 3 and 17 weeks, respectively, the outer nuclear layer thickness in both models is reduced to one row of cells in the central retina, any difference in thickness would be clearly evident at those ages. No difference was seen in outer nuclear layer thickness on the retinal cross sections between the rd1 mice and the Casp7–/–_rd1 mice at 3 weeks of age indicating that rod survival was not altered in the absence of Casp7 (Figure 2A). Retinal flat mounts revealed a uniform distribution of cones as assessed with cone arrestin antibody staining consistent with 3 weeks being the onset of cone death (Figure 2B). Similarly, in the Casp7–/–_Rho-KO mice the outer nuclear layer was also reduced to one row of cells at 17 weeks of age indicating that also in the Rho-KO background the loss of CASP7 had no effect (Figure 2C). This is significantly different from what was seen in the T17M Rhodopsin mouse model where the thickness of the outer nuclear layer was three times wider [12]. In summary, loss of Casp7 did not affect rod survival in the rd1 and Rho-KO mouse models of RP.
Figure 2.
Loss of Casp7 does not affect rod degeneration. A: Retinal cross section of 3-week-old Casp7+/+_rd1 and Casp7–/_–rd1 mice stained with 4´,6-diamidino-2-phenylindole (DAPI) showing no difference in the thickness of the outer nuclear layer in the central retina (n = 3 animals; the zoomed-in view shows one row of cells above the dotted line which separated the outer nuclear layer from the inner nuclear layer). B: Retinal flat mounts stained with cone arrestin (red signal) showing no difference in the distribution of cones at the onset of cone death (genotype and age same as in panel A). C: Retinal cross section of 17-week-old Casp7+/+_Rho-KO and Casp7–/–_Rho-KO mice showing no difference in the thickness of the outer nuclear layer in the central retina (n = 3 animals; the dotted line separates the outer nuclear layer from the inner nuclear layer).
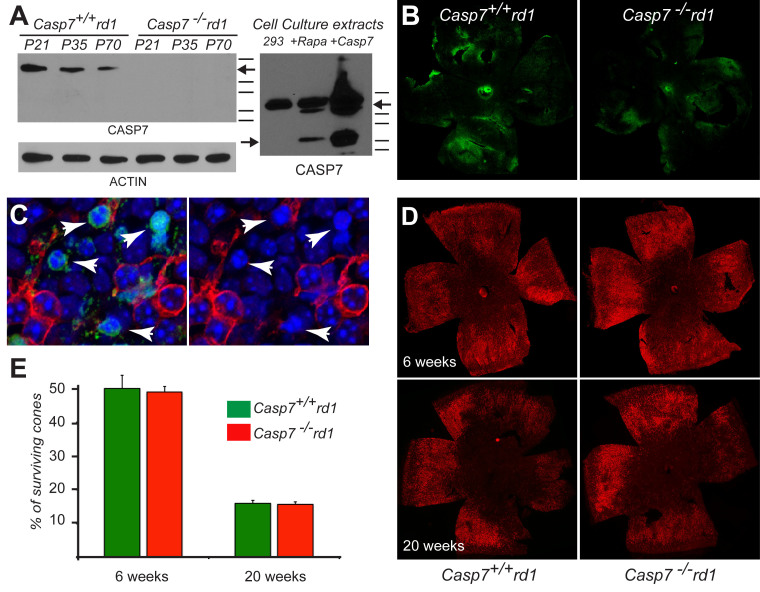
Secondary cone death in not affected by loss of Casp7 in the rd1 and Rho-KO mouse models of RP
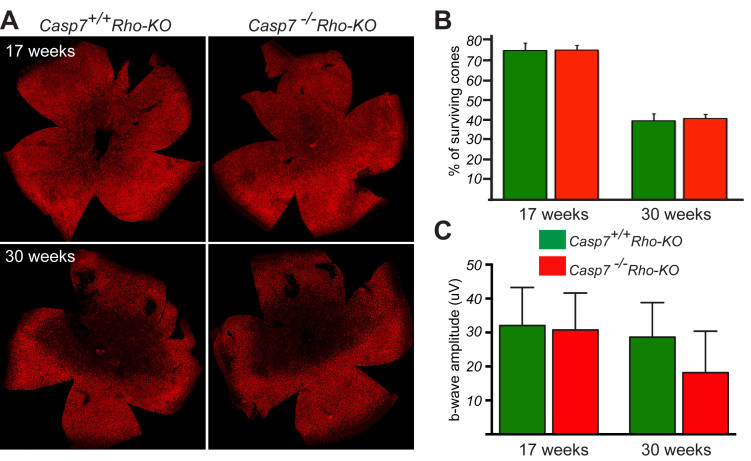
To determine whether Casp7 is activated in cones during the period of secondary cone death, we first used western blot analyses to test for cleaved Casp7. Executioner caspases are commonly activated by cleavage [33]; thus, the presence of a cleaved product is an indicator of an activated caspase. We did not detect any cleaved Casp7 in the rd1 mice (Figure 3A) although we readily identified the cleaved product in the HEK293 cells treated with rapamycin. However, Casp7 is the exception among the executioner caspases in that dimerization of Casp7 is sufficient for activation albeit at lower levels [34,35]. Consistent with that, overexpression of Casp7 in the HEK293 cells was sufficient to cause enough dimerization of Casp7 resulting in autocatalytic cleavage of the caspase (Figure 3A). Interestingly, the levels of CASP7 declined with the demise of cones over time consistent with it being enriched in cones. Alternatively, the decline could also be due to a decline in the number of cones in conjunction with an age-related decline in the inner nuclear layer and possibly in cones. To further test whether Casp7 was activated without cleavage, we used a fluorescein isothiocyanate (FITC)–labeled peptide with the target sequence of Casp7 (DEVD). The peptide becomes covalently bound to Casp7 only when the active site of the protease is formed. The fluorescent label thus allows determining if there is any in situ activity of Casp7 in cones. Although labeling of cones was seen in the 6-week-old rd1 mice, labeling was not abolished in the Casp7–/–_rd1 mice (Figure 3B). Interestingly, most of the labeled cell had a more condensed nucleus with almost no expression of the cone-specific protein cone arrestin consistent with the labeled cells undergoing apoptosis (Figure 3C). However, the same peptide can also bind to activated Casp3; thus, cross-reactivity cannot be excluded [36], although we were not able to detect any cleaved Casp3 in cones (data not shown) with an antibody that readily detected cleaved Casp3 in rods during the period of rod degeneration [1]. Finally, quantification of cone survival at 6 weeks and 20 weeks of age did not show any statistically significant difference between the rd1 mice and the rd1 mice with Casp7 loss (Figure 3D,E). Similarly, loss of Casp7 in the slower progressing Rho-KO mouse model of RP also did not result in any statistically significant difference in the distribution of cones at the onset of cone death, meaning at 17 weeks of age and at 30 weeks of age (Figure 4A,B). The 30 week time point, which is roughly equivalent to 10 weeks of age in the rd1 mouse model [1], was chosen as the second time point because by then cone death has progressed significantly in the Rho-KO. Cone function was also not changed although there was a slight reduction in the Casp7–/–_Rho-KO mice (Figure 4C). Overall, the data suggest that Casp7 likely does not contribute to secondary cone death in RP.
Figure 3.
Loss of Casp7 does not affect cone death in the rd1 mouse model of RP. A: Western blot analysis at postnatal (P) days 21, 35, and 70 with retinal extracts from Casp7+/+_rd1 and Casp7–/–_rd1 mice showing on the left no cleaved CASP7 protein in Casp7+/+_rd1 mice, a decline in the CASP7 protein over time, consistent with its enrichment in cones, and a lack of detectable CASP7 protein in Casp7–/–_rd1 mice. To the right, the western blot analysis with protein extracts from HEK293 cells show cleavage of the CASP7 protein after rapamycin treatment or overexpression of Casp7, indicating that the antibody is able to recognize the cleaved product and that dimerization by overexpression is sufficient to activate CASP7 (the lines on the right of both western blots indicate molecular weight markers in kDa; starting from the top line, their respective sizes are 37, 25, 20, 15, 10; arrows on right side of the western blot point to pro-CASP7 while the arrow on the left of the western blot points to the cleaved CASP7 product). B: Immunofluorescence on retinal flat mounts to detect active CASP7 (the green signal indicates the fluorescein isothiocyanate (FITC)–labeled CASP7 activity peptide) in the Casp7+/+_rd1 and Casp7–/–_rd1 mice. Because the FITC signal is still present in Casp7–/_–rd1 mice, the peptide is likely cross-reacting. C: Higher magnification of the assay in (B) showing that cone cells strongly labeled by the FITC CASP7 activity peptide (arrowheads) tend to have pyknotic nuclei and less cone arrestin immunoreactivity (red signal), suggesting that the peptide was labeling dying cones (blue: nuclear 4´,6-diamidino-2-phenylindole [DAPI]). D: Examples of retinal flat mounts of Casp7+/+_rd1 and Casp7–/–_rd1 mice stained for cone arrestin (red signal) expression at 6 and 20 weeks of age. E: Quantification of cone survival at 6 and 20 weeks of age showed no statistically significant improvement in cone survival upon loss of Caspase-7 in rd1 mice. (n=6 per genotype and time point; Error bars: SEM).
Figure 4.
Loss of Casp7 does not affect secondary cone death in Rho-KO mice. A: Examples of retinal flat mounts of Casp7+/+_Rho-KO and Casp7–/–_Rho-KO mice stained for cone arrestin (red signal) expression at the onset of cone death (17 weeks) and a later time point (30 weeks) that corresponds to roughly 10 weeks in rd1 mice. B: Quantification of cone survival at 17 and 30 weeks of age of Casp7+/+_Rho-KO and Casp7–/–_Rho-KO mice. No statistically significant improvement in cone survival is seen upon loss of Casp7. C: B-wave amplitudes of photopic electroretinogram recordings showed also no statistically significant improvement in cone function upon loss of Casp7. (n=6 per genotype and time point in B and C; Error bars: SEM).
Discussion
We set out to understand whether Casp7 is involved in facilitating secondary cone death during the periods of cone degeneration in RP. Because Casp7 is cone enriched and has been shown to play a role in PRs that experience ER stress, and ER stress has been proposed to be a contributing factor to PR death in RP, Casp7 was chosen as a rational candidate to identify additional cell death mechanisms that contribute to secondary cone death in RP [12,13,16-18]. Although we were able to detect activated Casp7 with the FITC-labeled activity-peptide assay, we did not identify any cleaved CASP7 protein product nor was the peptide-activity assay negative in the Casp7–/–_rd1 background. Because the same peptide sequence used here also recognizes activated CASP3, cross-reactivity to CASP3 cannot be excluded [36]. However, we failed to detect activated CASP3 in cones with immunofluorescence although in our previously published work the antibody was able to detect activated CASP3 during the periods of rod degeneration [1]. This does not exclude that the FITC-labeled peptide-activity assay may have reacted with low levels of activated CASP3. Alternatively, the chemically activated FITC-labeled peptide could have reacted with other proteases or protein degradation products produced during the cell death process, because labeling with the FITC-labeled peptide was preferentially seen in cells undergoing apoptosis. We favor this hypothesis over cross-reactivity with CASP3, because although CASP3 and CASP7 were for a long time believed to be functionally redundant, more and more research indicates that there are clear functional differences in vivo and regarding substrate recognition, indicating that these two proteases occupy distinct non-redundant roles within the cell death machinery [36-40].
We previously identified Casp2 as the first caspase that plays a pivotal role during the periods of secondary cone death in RP [7]. Thus, if Casp7 plays any role in secondary cone death, one could envision that in the absence of Casp7 cones increase CASP2 activity. Such a scenario could offer an explanation for the cross-reactivity of the FITC-labeled peptide and the fact that loss of Casp7 did not result in improved cone survival. To determine whether in the absence of Casp7 Casp2 plays a more prominent role in secondary cone cell death, we also generated the double loss of function in an rd1 background and analyzed cone survival at 20 weeks of age, when we saw a clear improvement in our previously published data in the absence of Casp2 [7]. However, although at 20 weeks of age concomitant loss of Casp2 and Casp7 in an rd1 background resulted in improved cone survival when compared to the loss of Casp7 alone (30.9%±2.90% versus 15.7%±1.00%, respectively), the double loss of function did not result in a statistically significant improvement in cone survival when compared to our previously published data [7] with the loss of Casp2 alone (31.5%±1.00%), suggesting that Casp2 does not compensate for the lack of Casp7.
The rd1 mouse model of RP is one of the fastest degenerating mouse models used to study the disease. Thus, it is quite possible that some mechanisms of cone cell death may be quite specific to this model and not apply to slower models of cone degeneration. To address this issue, we also used the much slower degenerating mouse model of RP, the Rho-KO mouse. Nonetheless, there was no difference in cone degeneration in the Rho-KO mouse model in the absence or presence of Casp7. In summary, Casp7 is either not involved in secondary cone death in RP or the effect of Casp7 is negligible. This is surprising given that Casp7 is expressed in cones and is absent from rods, albeit rods are perfectly capable of upregulating Casp7 under stress conditions that cause ER stress [12,14]. This raises the question, why would cones express Casp7 rather than upregulating it when needed? One possible explanation could be that CASP7 can cleave CASP12. In its uncleaved form, CASP12 can bind CASP1 and thus prevent CASP1-mediated activation of proinflammatory cytokines, such as interleukin (IL)-1β and IL-18 [41]. Thus, the presence of CASP7 in cones could accelerate the release of proinflammatory cytokines from cones after ischemia, light damage, or infection. However, the present findings allow us only to conclude that CASP7 is not required for secondary cone death in RP suggesting that under these conditions cone death is unlikely due to an increase in ER stress. Additionally, the findings suggest that the mechanism(s) used to execute secondary cone death in RP may be the same across all disease-causing mutations that are in genes exclusively expressed in rods, meaning the mechanisms are independent of the rod death kinetics.
Acknowledgments
We would like to thank Janis Lem for the Rho-KO mice. We acknowledge Eric Baehrecke, Francis Chan, Daryl Bosco, Hemant Khanna, Lolita Petit and Marina Zieger for insightful discussions and critical reading of the manuscript. This work was supported in part by grants from the NIH R01EY023570.
References
- 1.Punzo C, Kornacker K, Cepko CL. Stimulation of the insulin/mTOR pathway delays cone death in a mouse model of retinitis pigmentosa. Nat Neurosci. 2009;12:44–52. doi: 10.1038/nn.2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet. 2006;368:1795–809. doi: 10.1016/S0140-6736(06)69740-7. [DOI] [PubMed] [Google Scholar]
- 3.Earnshaw WC, Martins LM, Kaufmann SH. Mammalian caspases: structure, activation, substrates, and functions during apoptosis. Annu Rev Biochem. 1999;68:383–424. doi: 10.1146/annurev.biochem.68.1.383. [DOI] [PubMed] [Google Scholar]
- 4.Salvesen GS, Dixit VM. Caspases: intracellular signaling by proteolysis. Cell. 1997;91:443–6. doi: 10.1016/s0092-8674(00)80430-4. [DOI] [PubMed] [Google Scholar]
- 5.Thornberry NA, Lazebnik Y. Caspases: enemies within. Science. 1998;281:1312–6. doi: 10.1126/science.281.5381.1312. [DOI] [PubMed] [Google Scholar]
- 6.Bao Q, Shi Y. Apoptosome: a platform for the activation of initiator caspases. Cell Death Differ. 2007;14:56–65. doi: 10.1038/sj.cdd.4402028. [DOI] [PubMed] [Google Scholar]
- 7.Venkatesh A, Ma S, Le YZ, Hall MN, Ruegg MA, Punzo C. Activated mTORC1 promotes long-term cone survival in retinitis pigmentosa mice. J Clin Invest. 2015;125:1446–58. doi: 10.1172/JCI79766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zoncu R, Efeyan A, Sabatini DM. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol. 2011;12:21–35. doi: 10.1038/nrm3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Venkatesh A, Ma S, Punzo C. TSC but not PTEN loss in starving cones of retinitis pigmentosa mice leads to an autophagy defect and mTORC1 dissociation from the lysosome. Cell Death Dis. 2016;7:e2279. doi: 10.1038/cddis.2016.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Usui S, Oveson BC, Lee SY, Jo YJ, Yoshida T, Miki A, Miki K, Iwase T, Lu L, Campochiaro PA. NADPH oxidase plays a central role in cone cell death in retinitis pigmentosa. J Neurochem. 2009;110:1028–37. doi: 10.1111/j.1471-4159.2009.06195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bowes C, Li T, Danciger M, Baxter LC, Applebury ML, Farber DB. Retinal degeneration in the rd mouse is caused by a defect in the beta subunit of rod cGMP-phosphodiesterase. Nature. 1990;347:677–80. doi: 10.1038/347677a0. [DOI] [PubMed] [Google Scholar]
- 12.Choudhury S, Bhootada Y, Gorbatyuk O, Gorbatyuk M. Caspase-7 ablation modulates UPR, reprograms TRAF2-JNK apoptosis and protects T17M rhodopsin mice from severe retinal degeneration. Cell Death Dis. 2013;4:e528. doi: 10.1038/cddis.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corbo JC, Myers CA, Lawrence KA, Jadhav AP, Cepko CL. A typology of photoreceptor gene expression patterns in the mouse. Proc Natl Acad Sci USA. 2007;104:12069–74. doi: 10.1073/pnas.0705465104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunte MM, Choudhury S, Manheim JF, Shinde VM, Miura M, Chiodo VA, Hauswirth WW, Gorbatyuk OS, Gorbatyuk MS. ER stress is involved in T17M rhodopsin-induced retinal degeneration. Invest Ophthalmol Vis Sci. 2012;53:3792–800. doi: 10.1167/iovs.11-9235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shinde VM, Sizova OS, Lin JH, LaVail MM, Gorbatyuk MS. ER stress in retinal degeneration in S334ter Rho rats. PLoS One. 2012;7:e33266. doi: 10.1371/journal.pone.0033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorbatyuk MS, Knox T, LaVail MM, Gorbatyuk OS, Noorwez SM, Hauswirth WW, Lin JH, Muzyczka N, Lewin AS. Restoration of visual function in P23H rhodopsin transgenic rats by gene delivery of BiP/Grp78. Proc Natl Acad Sci USA. 2010;107:5961–6. doi: 10.1073/pnas.0911991107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thapa A, Morris L, Xu J, Ma H, Michalakis S, Biel M, Ding XQ. Endoplasmic Reticulum Stress-associated Cone Photoreceptor Degeneration in Cyclic Nucleotide-gated Channel Deficiency. J Biol Chem. 2012;287:18018–29. doi: 10.1074/jbc.M112.342220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang LP, Wu LM, Guo XJ, Tso MO. Activation of endoplasmic reticulum stress in degenerating photoreceptors of the rd1 mouse. Invest Ophthalmol Vis Sci. 2007;48:5191–8. doi: 10.1167/iovs.07-0512. [DOI] [PubMed] [Google Scholar]
- 19.Xiong W, MacColl Garfinkel AE, Li Y, Benowitz LI, Cepko CL. NRF2 promotes neuronal survival in neurodegeneration and acute nerve damage. J Clin Invest. 2015;125:1433–45. doi: 10.1172/JCI79735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Punzo C, Xiong W, Cepko CL. Loss of daylight vision in retinal degeneration: are oxidative stress and metabolic dysregulation to blame? J Biol Chem. 2012;287:1642–8. doi: 10.1074/jbc.R111.304428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Komeima K, Rogers BS, Campochiaro PA. Antioxidants slow photoreceptor cell death in mouse models of retinitis pigmentosa. J Cell Physiol. 2007;213:809–15. doi: 10.1002/jcp.21152. [DOI] [PubMed] [Google Scholar]
- 22.Komeima K, Rogers BS, Lu L, Campochiaro PA. Antioxidants reduce cone cell death in a model of retinitis pigmentosa. Proc Natl Acad Sci USA. 2006;103:11300–5. doi: 10.1073/pnas.0604056103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu L, Oveson BC, Jo YJ, Lauer TW, Usui S, Komeima K, Xie B, Campochiaro PA. Increased expression of glutathione peroxidase 4 strongly protects retina from oxidative damage. Antioxid Redox Signal. 2009;11:715–24. doi: 10.1089/ars.2008.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shen J, Yang X, Dong A, Petters RM, Peng YW, Wong F, Campochiaro PA. Oxidative damage is a potential cause of cone cell death in retinitis pigmentosa. J Cell Physiol. 2005;203:457–64. doi: 10.1002/jcp.20346. [DOI] [PubMed] [Google Scholar]
- 25.Zandy AJ, Lakhani S, Zheng T, Flavell RA, Bassnett S. Role of the executioner caspases during lens development. J Biol Chem. 2005;280:30263–72. doi: 10.1074/jbc.M504007200. [DOI] [PubMed] [Google Scholar]
- 26.Bergeron L, Perez GI, Macdonald G, Shi L, Sun Y, Jurisicova A, Varmuza S, Latham KE, Flaws JA, Salter JC, Hara H, Moskowitz MA, Li E, Greenberg A, Tilly JL, Yuan J. Defects in regulation of apoptosis in caspase-2-deficient mice. Genes Dev. 1998;12:1304–14. doi: 10.1101/gad.12.9.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lem J, Krasnoperova NV, Calvert PD, Kosaras B, Cameron DA, Nicolo M, Makino CL, Sidman RL. Morphological, physiological, and biochemical changes in rhodopsin knockout mice. Proc Natl Acad Sci USA. 1999;96:736–41. doi: 10.1073/pnas.96.2.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mattapallil MJ, Wawrousek EF, Chan CC, Zhao H, Roychoudhury J, Ferguson TA, Caspi RR. The Rd8 mutation of the Crb1 gene is present in vendor lines of C57BL/6N mice and embryonic stem cells, and confounds ocular induced mutant phenotypes. Invest Ophthalmol Vis Sci. 2012;53:2921–7. doi: 10.1167/iovs.12-9662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma S, Venkatesh A, Langellotto F, Le YZ, Hall MN, Ruegg MA, Punzo C. Loss of mTOR signaling affects cone function, cone structure and expression of cone specific proteins without affecting cone survival. Exp Eye Res. 2015;135:1–13. doi: 10.1016/j.exer.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Venkatesh A, Ma S, Langellotto F, Gao G, Punzo C. Retinal gene delivery by rAAV and DNA electroporation. Curr Protoc Microbiol 2013; Chapter 14:Unit 14D 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zieger M, Punzo C. Improved cell metabolism prolongs photoreceptor survival upon retinal-pigmented epithelium loss in the sodium iodate induced model of geographic atrophy. Oncotarget. 2016;7:9620–9633. doi: 10.18632/oncotarget.7330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zinchuk V, Wu Y, Grossenbacher-Zinchuk O, Stefani E. Quantifying spatial correlations of fluorescent markers using enhanced background reduction with protein proximity index and correlation coefficient estimations. Nat Protoc. 2011;6:1554–67. doi: 10.1038/nprot.2011.384. [DOI] [PubMed] [Google Scholar]
- 33.Boatright KM, Renatus M, Scott FL, Sperandio S, Shin H, Pedersen IM, Ricci JE, Edris WA, Sutherlin DP, Green DR, Salvesen GS. A unified model for apical caspase activation. Mol Cell. 2003;11:529–41. doi: 10.1016/s1097-2765(03)00051-0. [DOI] [PubMed] [Google Scholar]
- 34.Berger AB, Witte MD, Denault JB, Sadaghiani AM, Sexton KM, Salvesen GS, Bogyo M. Identification of early intermediates of caspase activation using selective inhibitors and activity-based probes. Mol Cell. 2006;23:509–21. doi: 10.1016/j.molcel.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 35.Denault JB, Bekes M, Scott FL, Sexton KM, Bogyo M, Salvesen GS. Engineered hybrid dimers: tracking the activation pathway of caspase-7. Mol Cell. 2006;23:523–33. doi: 10.1016/j.molcel.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 36.Walsh JG, Cullen SP, Sheridan C, Luthi AU, Gerner C, Martin SJ. Executioner caspase-3 and caspase-7 are functionally distinct proteases. Proc Natl Acad Sci USA. 2008;105:12815–9. doi: 10.1073/pnas.0707715105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Larner SF, Hayes RL, McKinsey DM, Pike BR, Wang KK. Increased expression and processing of caspase-12 after traumatic brain injury in rats. J Neurochem. 2004;88:78–90. doi: 10.1046/j.1471-4159.2003.02141.x. [DOI] [PubMed] [Google Scholar]
- 38.Le DA, Wu Y, Huang Z, Matsushita K, Plesnila N, Augustinack JC, Hyman BT, Yuan J, Kuida K, Flavell RA, Moskowitz MA. Caspase activation and neuroprotection in caspase-3- deficient mice after in vivo cerebral ischemia and in vitro oxygen glucose deprivation. Proc Natl Acad Sci USA. 2002;99:15188–93. doi: 10.1073/pnas.232473399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nicolini G, Rigolio R, Miloso M, Bertelli AA, Tredici G. Anti-apoptotic effect of trans-resveratrol on paclitaxel-induced apoptosis in the human neuroblastoma SH-SY5Y cell line. Neurosci Lett. 2001;302:41–4. doi: 10.1016/s0304-3940(01)01654-8. [DOI] [PubMed] [Google Scholar]
- 40.Eguchi R, Tone S, Suzuki A, Fujimori Y, Nakano T, Kaji K, Ohta T. Possible involvement of caspase-6 and −7 but not caspase-3 in the regulation of hypoxia-induced apoptosis in tube-forming endothelial cells. Exp Cell Res. 2009;315:327–35. doi: 10.1016/j.yexcr.2008.10.041. [DOI] [PubMed] [Google Scholar]
- 41.Scott AM, Saleh M. The inflammatory caspases: guardians against infections and sepsis. Cell Death Differ. 2007;14:23–31. doi: 10.1038/sj.cdd.4402026. [DOI] [PubMed] [Google Scholar]