Abstract
Background:
Research from 2006 documented substantial variation in medication coverage for residents across Canada. Since then, some provinces have implemented major medication plan reforms. We aimed to update the information on publicly funded medication insurance plans available across Canada and to compare out-of-pocket costs across the country.
Methods:
We compared provincial medication insurance plans using data from public websites and other public source documents. Using 2 hypothetical clinical examples, we determined the amount and type of a patient's out-of-pocket costs for 5 different patient subtypes that varied based on medication burden, age and income.
Results:
Each province offers a plan to all residents. Cost-sharing is employed across all provinces. Some residents must pay a premium to receive insurance or must pay 100% of their medication costs until they reach a deductible amount, above which government funding covers a portion of medication costs. With the scenario of low medication burden (medication cost about $500), out-of-pocket costs ranged from $250 to $2100 for higher-income residents and from $0 to $700 for lower-income residents. With the scenario of high medication burden (medication cost about $1800), the corresponding ranges were $250-$2500 and $0-$1100. The variation was due to province of residence, age and income.
Interpretation:
Variations in out-of-pocket payments continue to exist across the provinces, with some groups facing high expenses. Further work is required to understand the impact of different cost-sharing mechanisms, develop policies to limit out-of-pocket expenses and improve provincial drug plans.
Although the Canada Health Act ensures universal coverage of medically necessary physician and hospital care, outpatient medications are not included in the act, and there is no requirement for provinces to provide outpatient medication coverage for all residents. As such, many studies have noted that Canada lacks universal medication insurance.1
In 2008, Demers and colleagues2 documented interprovincial differences in public medication plans accurate to December 2006 and examined the implications for patients through a series of hypothetical examples illustrating the amount of out-of-pocket expenditures by province. Between 2006 and November 2016, several provinces made major redesigns to their public medication insurance plans. Specifically, Saskatchewan, Newfoundland and Labrador, Nova Scotia and New Brunswick expanded drug coverage to include people under the age of 65 years. In addition, Saskatchewan, Quebec, Nova Scotia and New Brunswick modified the cost-sharing mechanisms within their plans for older adults (aged ≥ 65). No changes were made to the plans in Alberta, British Columbia, Manitoba or Ontario. Other studies have documented the variation in plan structures and the resulting out-of-pocket payments.3,4 However, clinical examples as a means to visualize and compare the out-of-pocket costs for a typical patient across the country were last published in 2008.2 Thus, we aimed to update the information on publicly funded medication insurance plans available across Canada and to compare out-of-pocket costs for Canadians across the country, based on medication burden, age and income. We provide illustrative examples to aid in understanding the current financial burden of typical patients and to identify the types of patients most likely to experience high out-of-pocket costs.
Methods
Data sources
We compared all provincial publicly funded medication plans. Data were extracted from public medication plan websites and other public source documents in November 2016. Data extraction was performed in duplicate by research associates trained in pharmaceutical policy and the design of publicly funded medication plans. Key data elements included the relevant policies and rules of insurance plans (including generic substitution and first-payer policies), populations covered by the publicly funded plans, and the cost-sharing mechanisms and cost-containment strategies used by each plan. A standardized data extraction form was used (Appendix 1, available at www.cmajopen.ca/content/5/4/E808/suppl/DC1). The data extracted were then sent to drug plan managers within each province (identified through the public websites and organizational charts of the ministries of health) to verify the accuracy of the data abstracted. Each drug plan manager was provided a detailed summary of the respective plan via email. Managers were asked to check a box ("Yes/no") to indicate whether the extracted data were accurate. If the data were not accurate, managers were asked to provide the corrected data with a reference that could be verified by the research team. The territories and federal plans were not included in this analysis as these jurisdictions have limited information available publicly.
Clinical scenarios
To assess the variation in out-of-pocket costs across the country, we purposively selected 2 clinical examples that are commonly seen by Canadian physicians but also represent a spectrum of medication burden: 1) a patient with hypothyroidism, osteoporosis, depression and anxiety (low medication burden) and 2) a patient with type 2 diabetes mellitus and coronary artery disease (high medication burden). For both examples, we asked 2 physicians to consider relevant guideline recommendations and list the medication regimen they would prescribe.
For both clinical examples, we simulated 5 different age and income levels to illustrate variations in the provincial medication plan coverage. Specifically, we considered how a patient's age (< 65 yr or ≥ 65 yr), household income (above or below low-income cut-offs) and social assistance beneficiary status affected out-of-pocket cost (Box 1). We selected these age and income cut-offs because several provinces have different plans for people aged 65 years or more and low-income households. We did not consider any specialized plans that target high-cost drugs such as transplantation, major surgery, or palliative or cancer drugs.
Box 1: Clinical examples and patient demographic profiles considered.
Clinical overview
1. Case 1: patient with hypothyroidism, osteoporosis, depression and anxiety currently taking levothyroxine (75 µg daily), alendronate sodium (70 mg weekly), lorazepam (1 mg nightly) and escitalopram (20 mg daily); approximate medication cost $500
2. Case 2: patient with type 2 diabetes mellitus and coronary artery disease currently taking atorvastatin (40 mg daily), carvedilol (12.5 mg twice daily), irbesartan (150 mg daily), clopidogrel (75 mg daily), nitroglycerine (0.4 mg/h transdermally every 12 h), metformin (1000 mg twice daily) and insulin glargine (50 units subcutaneously twice daily); approximate medication cost $1800
Patient demographic profiles
1. Social assistance beneficiary: 35-year-old who is receiving social assistance benefits
2. Lower-income adult aged ≥ 65 yr: 67-year-old with an annual after-tax income of $14 000 who receives Old Age Supplement and Guaranteed Income Supplement
3. Higher-income adult aged ≥ 65 yr: 72-year-old with an annual after-tax income of $55 000 including Canada Pension Plan benefits and private pensions
4. Lower-income adult aged < 65 yr: 52-year-old with an annual after-tax income of $14 000
5. Higher-income adult aged < 65 yr: 45-year-old with an annual after-tax income of $55 000
Calculation of out-of-pocket costs
For each clinical example and patient demographic profile, we calculated the annual patient-borne out-of-pocket costs based on the eligibility rules and regulations of the applicable provincial insurance plan. We coded the rules of the plan into an Excel spreadsheet, with the coding verified by a duplicate reviewer for accuracy. Any disagreement in coding was resolved by consensus. Each component of the total cost (i.e., deductible, copayment and premium) was reported separately. We assumed that all prescriptions were dispensed in 3-month supplies, as most provinces allow a maximum of 100 days per dispense. We used the 2016 Alberta medication prices for all provinces.5 This approach ensured that we were able to attribute differences in out-of-pocket costs to the plan design as opposed to different absolute medication prices negotiated by provinces with pharmaceutical companies. We added the province-specific dispensing fee to the total cost of each prescription. All costs are expressed in 2016 Canadian dollars.
Ethics approval
Because this study did not involve human subjects, ethics approval was not sought.
Results
Comparison of medication plans across Canada
All provinces have generic payment rules that generally state that the provincial payer will pay only the amount for generic equivalents, where available. With the exception of Quebec, all provinces use multiple medication insurance plans, ranging from 5 (Manitoba, Nova Scotia, and Newfoundland and Labrador) to 27 (Prince Edward Island) (Table 1). All provinces have generous plans for social assistance beneficiaries that leave patients with no or about $2-$5 in out-of-pocket expenditures. All of the provinces have different plans for those aged less than 65 years and those aged 65 years or more except Manitoba and BC (which is in the process of phasing out its age-based plan). Some provinces rely on premium-based systems, whereas others use some mix of copayments and deductibles to cost-share with beneficiaries. In general, the amount of out-of-pocket expenditures paid by Canadians varies by medication burden and/or income level except within Alberta (Appendix 1). Other characteristics of the plans that vary across Canada include the adoption of first-payer policy (BC, Alberta, Saskatchewan, Ontario and Quebec) and the mandatory requirement to carry medication insurance (Quebec).
Table 1: Summary of characteristics of publicly funded medication plans across Canadian provinces*.
| Province | No. of plans | Common target populations and whether coverage is subject to a premium | Government first payer | ||
|---|---|---|---|---|---|
| General population | Older adults† | Social assistance/low-income | |||
| British Columbia | 10 | Yes | Born before 1939 | Yes | Yes |
| Alberta | 10 | Premiums | Yes | Yes | Yes |
| Saskatchewan | 11 | Yes | Yes | Yes | Yes |
| Manitoba | 5 | Yes | Same as general population | Yes | No |
| Ontario | 7 | Yes | Yes | Yes | Yes |
| Quebec‡ | 1 | Premiums | Premiums | Yes | Yes |
| New Brunswick | 13 | Premiums | Low-income/premiums for others | Yes | No |
| Nova Scotia | 5 | Yes | Premiums | Yes | No |
| Prince Edward Island | 27 | Combination of plans§ | Yes | Yes | Unclear |
| Newfoundland and Labrador | 5 | Yes | Yes | Yes | Yes |
*All provinces have generic payment rules.
†Aged 65 years or more unless otherwise noted.
‡All residents are mandated to have insurance (private or public).
§Has a variety of disease- and medication-based plans for those under 65 years of age.
Clinical examples
People receiving social assistance do not pay out of pocket in 6 provinces: BC, Alberta, Manitoba, Quebec, Prince Edward Island, and Newfoundland and Labrador. In the remaining provinces, those receiving social assistance pay lower amounts for their prescription medications than do older and younger adults. For the scenario of low medication burden (annual medication cost $500), the out-of-pocket payments ranged from $32 to $80 annually across the provinces. For the scenario of high medication burden (annual medication cost $1800), the range of out-of-pocket expenses across the provinces was $64 to $160 annually.
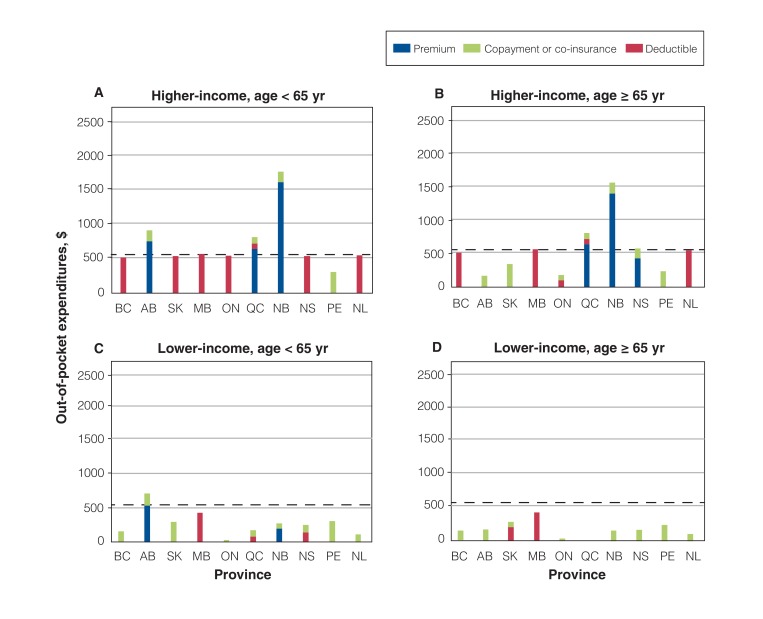
In the scenario of low medication burden, out-of-pocket costs varied from $250 to $2100 for those with an income of $55 000 (Figure 1, A and B) and from $0 to $700 for those with an income of $14 000 (Figure 1, C and D). The out-of-pocket costs were generally lower for older adults than for younger adults and for lower-income residents than for those with higher incomes. There were several provincial outliers, particularly those that use premiums (Alberta [younger adults], Quebec and New Brunswick [older adults]). Owing to the premium costs in these provinces, residents with a low medication burden were found to potentially contribute more than their actual medication costs.
Figure 1.
Out-of-pocket expenditures for medications for the scenario of low medication burden, by province. The horizontal line at $500 represents the annual medication cost. The difference between the height of the bar, excluding premiums, and the horizontal line is the amount the government pays.
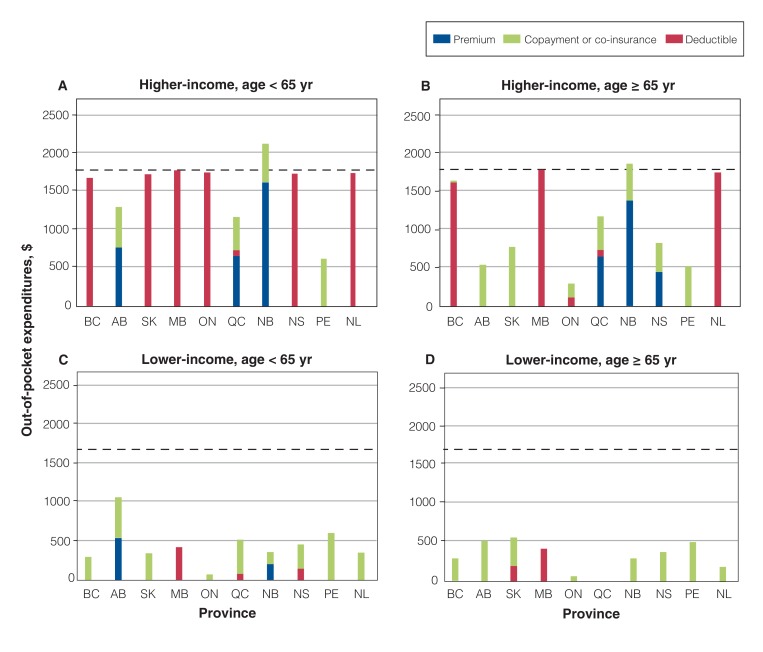
In the scenario of high medication burden, out-of-pocket costs ranged $250 to $2500 for higher-income residents (Figure 2, A and B) and from $0 to $1100 for lower-income residents (Figure 2, C and D). In all provinces except Alberta, patient income level or, in some cases, income-to-medication-burden ratio, is used to determine cost-sharing.
Figure 2.
Out-of-pocket expenditures for medications for the scenario of high medication burden, by province. The horizontal line at $1800 represents the annual medication cost. The difference between the height of the bar, excluding premiums, and the horizontal line is the amount the government pays.
Interpretation
All Canadian provinces have publicly funded medication insurance plans that are available to all residents. However, those with incomes of $55 000 or more may not receive any financial support for their medications from the government insurance plans. The use of age-based plans and income-based medication coverage varies across the country. In addition, each province, and occasionally the different plans within a province, use a variety of cost-sharing mechanisms. This variation leads to different out-of-pocket costs for the same type of patient, depending on the province of residence.
Only a few provincial medication plans use premiums. A reliance on premiums may lead to situations in which it is advantageous to remain uninsured, such as when one's medication burden, even when paying 100% of the cost, remains less than the cost of premiums and copayments. This insurance selectivity may lead to an unbalanced risk pool in the insurance market and may leave the publicly funded plans' insuring only those at highest risk (or with greatest expense). To address this issue, Quebec has instituted a mandatory insurance policy, although publications assessing the impact of this policy are lacking.6,7 Further study assessing the implications of mandatory insurance for private insurance, public support for legislative changes and the impact on out-of-pocket costs would be required before other provinces consider adopting mandatory insurance.
It remains unclear which form of cost-sharing has less impact on adherence or is preferred by patients. Several systematic reviews on cost-sharing have been published.8-11 However, the conclusions have been limited to documenting the association between increased out-of-pocket costs and lower medication use; the authors have not been able to compare across mechanisms of cost-sharing. The limited published data reporting on cost-sharing mechanisms comes from the United States, where the relation between health insurance cost-sharing mechanisms, not medication insurance, is arguably different.12,13
Our findings are particularly relevant given the current discussion in the academic literature regarding the need for a system of national pharmacare to replace the current patchwork system of pharmaceutical insurance in Canada.14 National pharmacare is defined as public coverage of medically necessary prescription drugs on universal terms and conditions across Canada, including limited patient copayments and a basic list of medications available for all Canadians.15 Recent research has shown that national pharmacare could reduce private insurers' costs by $8.2 billion and increase the costs to public plans by $1 billion, thus achieving a total reduction on medication spending of $7.3 billion.15 These savings would be achieved through the creation of a larger market share, thus enabling negotiation of lower drug prices. The analysis also assumes that a larger market would also be better able to promote better medication selection and that co-insurance would be maintained. Although the savings that could be achieved are very attractive, it is important to consider national pharmacare within the current context and options that exist for provinces to lower drug prices. If the federal government included prescription medication access within legislation such as the Canada Health Act, this would compel a minimum standard within medication insurance funded by the provincial governments. Establishing a minimum standard would likely close the gap between the out-of-pocket payments faced by the same type of patients in different provinces.
Limitations
This study is limited by the complexity of the multitude of public medication insurance plans in each province (with the exception of Quebec). We gathered information from publicly available sources (i.e., provincial websites) to obtain accurate and up-to-date information on each medication plan, but specifics regarding how each province administers its plans was not uniformly available. Although we tried to be comprehensive with our clinical cases and age and demographic profiles, it is difficult to represent all possible combinations of the important contributing variables, especially given the large number of plans available in certain provinces. Of particular note, we considered only the standard population-based plans across the provinces. Many provinces also have a variety of specialized programs that support patients with exceptional needs such as palliative care and high-cost medications, those with infectious diseases and those with cancer. Other studies have reported on these plans,16,17 but this was not the focus of our study.
Conclusion
The delivery of pharmaceutical insurance in Canada is a patchwork, with each province having separate medication insurance plans. This leads to variations in out-of-pocket payments across the provinces. Further research is required to understand the impact of different cost-sharing mechanisms, develop policies to limit out-of-pocket expenses and improve provincial drug plans.
Supplementary Material
Footnotes
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/5/4/E808/suppl/DC1.
References
- 1.Barnieh L, Clement F, Harris A, et al. A systematic review of cost-sharing strategies used within publicly-funded drug plans in member countries of the Organisation for Economic Co-operation and Development. PLoS One. 2014;9:e90434. doi: 10.1371/journal.pone.0090434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demers V, Melo M, Jackevicius C, et al. Comparison of provincial prescription drug plans and the impact on patients' annual drug expenditures. CMAJ. 2008;178:405–9. doi: 10.1503/cmaj.070587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daw JR, Morgan SG. Stitching the gaps in the Canadian public drug coverage patchwork? A review of provincial pharmacare policy changes from 2000 to 2010. Health Policy. 2012;104:19–26. doi: 10.1016/j.healthpol.2011.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coombes ME, Morgan SG, Barer ML, et al. Who's the fairest of them all? Which provincial pharmacare model would best protect Canadians against catastrophic drug costs? Healthc Q. 2004; 7(Suppl 13-9) doi: 10.12927/hcq.2004.17236. [DOI] [PubMed] [Google Scholar]
- 5.Interactive drug benefit list. Edmonton: Alberta Health; 2017. [accessed 2016 Nov. 15]. Available https://www.ab.bluecross.ca/dbl/idbl_main1.html.
- 6.Pomey MP, Forest PG, Palley HA, et al. Public/private partnerships for prescription drug coverage: policy formulation and outcomes in Quebec's universal drug insurance program, with comparisons to the Medicare prescription drug program in the United States. Milbank Q. 2007;85:469–98. doi: 10.1111/j.1468-0009.2007.00496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C, Li Q, Sweetman A, et al. Mandatory universal drug plan, access to health care and health: evidence from Canada. J Health Econ. 2015;44:80–96. doi: 10.1016/j.jhealeco.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Gemmill MC, Thomson S, Mossialos E. What impact do prescription drug charges have on efficiency and equity? Evidence from high-income countries. Int J Equity Health. 2008;7:12. doi: 10.1186/1475-9276-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298:61–9. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kesselheim AS, Huybrechts KF, Choudhry NK, et al. Prescription drug insurance coverage and patient health outcomes: a systematic review. Am J Public Health. 2015;105:e17–30. doi: 10.2105/AJPH.2014.302240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann BS, Barnieh L, Tang K, et al. Association between drug insurance cost sharing strategies and outcomes in patients with chronic diseases: a systematic review. PLoS One. 2014:e89168. doi: 10.1371/journal.pone.0089168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waters TM, Chang CF, Cecil WT, et al. Impact of high-deductible health plans on health care utilization and costs. Health Serv Res. 2011;46:155–72. doi: 10.1111/j.1475-6773.2010.01191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reddy SR, Ross-Degnan D, Zaslavsky AM, et al. Impact of a high-deductible health plan on outpatient visits and associated diagnostic tests. Med Care . 2014;52:86–92. doi: 10.1097/MLR.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan SG, Li W, Yau B, et al. Estimated effects of adding universal public coverage of an essential medicines list to existing public drug plans in Canada. CMAJ. 2017;189:E295–302. doi: 10.1503/cmaj.161082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgan SG, Law M, Daw J, et al. Estimated cost of universal public coverage of prescription drugs in Canada. CMAJ. 2015;187:491–7. doi: 10.1503/cmaj.141564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hanley GE, Morgan S. Chronic catastrophes: exploring the concentration and sustained nature of ambulatory prescription drug expenditures in the population of British Columbia, Canada. Soc Sci Med. 2009;68:919–24. doi: 10.1016/j.socscimed.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Weymann D, Smolina K, Gladstone EJ, et al. High-cost users of prescription drugs: a population-based analysis from British Columbia, Canada. Health Serv Res. 2017;52:697–719. doi: 10.1111/1475-6773.12492. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.