Abstract
PURPOSE
To evaluate the sealing performance of Hybrid Coat and its influence on the shear bond strength of five dentin surface cements.
MATERIALS AND METHODS
Six premolars were pretreated to expose the dentin surface prior to the application of Hybrid Coat. The microscopic characteristics of the dentinal surfaces were examined with scanning electron microscopy (SEM). Then, 40 premolars were sectioned longitudinally, and 80 semi-sections were divided into a control group (untreated) and a study group (treated by Hybrid Coat). Alloy restoration was bonded to the teeth specimen using five different cements. Shear bond strength was measured by the universal testing machine. The fracture patterns and the adhesive interface were observed using astereomicroscope.
RESULTS
SEM revealed that the lumens of dentinal tubules were completely occluded by Hybrid Coat. The Hybrid Coat significantly improved the shear bond strength of resin-modified glass ionomer cement (RMGIC) and resin cement (RC) but weakened the performance of zinc phosphate cement (ZPC), zinc polycarboxylate cement (ZPCC) and glass ionomer cement (GIC).
CONCLUSION
Hybrid Coat is an effective dentinal tubule sealant, and therefore its combined use with resin or resin-modified glass ionomer cements can be applied for the prostheses attachment purpose.
Keywords: Hybrid Coat, Cement, Shear Bond Strength
INTRODUCTION
Indirect fabrications, including onlay, inlay, crown and bridge restorations, were necessary in dental practices. The conduct of these procedures needed enough preparation space, and as a consequence, the damage to sound dentin as well as the exposure of dentinal tubules was unavoidable. The dentinal tubules were fluid-filled and indirectly contacted with pulpal nerve endings. Some external stimulus, such as low temperature, chemical substance, and mechanical action would cause the excitation of pulpal nerve fibers, thus leading to the nerve cell membrane depolarization and heightened the pain sensitivity.1,2 In clinical, occluding or sealing the exposed dentinal tubules were commonly conducted to prevent the increased postoperative sensitivity.3,4
Recently, a novel resin coating technique was introduced in indirect restorations, which involved hybrid layer and tight-sealing film.5 They were generated at the dentin surface under the help of dentin adhesive system. This tubule plugging technique could reduce pulpal stimulation and pain sensitivity to a minimum. However, the layers generated a thick coating on the prepared tooth that would make the crown preparations deformed, and the widely application of the resin coating technique was limited. Thus, a thinner film was needed.6
Hybrid Coat could occlude the tubules or reduce the diameter of dentinal tubules and consequently decrease the probability of adhesion after tooth preparation. Hybrid Coat is an all-in-one adhesive system, which provides a thin and convenient crown preparation coating at the dentin surface.7 However, there remains a possible change in the shear bond strength when the common cements were used.8 Zinc phosphate cement (ZPC), zinc polycarboxylate cement (ZPCC), glass ionomer cement (GIC), resin-modified glass ionomer cement (RMGIC), and resin cement (RC) were the commonly used cements. The fixation of retentions was closely related with the mechanical properties of cement and the surface characteristics of the dentin. Therefore, selected appropriate materials for cementation were very critical for a tight dentin bonding and a successful indirect restoration. Previous studies have reported that the all-inone adhesive system could improve the micro-tensile bond strengths of resin cement to dentin for a composite crown restoration,9 but there was little information about the effect of Hybrid Coat on the adhesive properties of the cements for indirect use.
Currently, Hybrid Coat was more commonly used to decrease dentin hypersensitivity after tooth preparation. In order to get the optimal performance, the combined use with other cements was necessary. While, the knowledge about sealability and optimal combination with cementation agents were lacking. The purpose of the present study was to compare the shear bond strengths of five different commercial cements, including ZPC, ZPCC, GIC, RMGIC, and RC to dentin with or without Hybrid Coat. We hypothesized that Hybrid Coat would occlude dentinal tubules or reduce the diameter of dentinal tubules to decrease the probability of adhesion after tooth preparation, and the combined use of dentin desensitizer and cements would alter the shear bond strength.
MATERIALS AND METHODS
A total of 46 intact human premolars were extracted freshly. Soft tissue was removed, and the teeth were immediately stored in 1% chloramine solution at 4℃ for one month before use. Calculus, residual roots, and periodontal tissues were removed prior to the experiment. The study was approved by the Ethics Committee of the Second Xiangya Hospital of Central South University, China.
The buccal enamel was removed from 6 premolars using a diamond bur (ISO No. TR-11EF) and the dentin surface was exposed. The teeth were examined with a stereomicroscope at × 16 magnifications to ensure the enamel was removed completely. The specimens were then randomly divided into two groups, control group (the dentin surface was untreated) and treatment group (the dentin surface was treated by Hybrid Coat) with 3 in each group. All the specimens were immersed in water at 37℃ for 24 hours and then cleaved longitudinally into equal halves. Each fractured sample was coated with a thin surface gold layer and observed by SEM.
Forty teeth were cleaved longitudinally and produced 80 semi-sections. They were polished with wet 180-grit SiC paper to produce a flat, smooth test surface. They were divided into control group and study group to have 40 in each group. The dentin surfaces were untreated in control group and treated with Hybrid Coat in study group. 80 nickel-chromium alloy restorations (3 cm3) were prepared. Each tooth specimen was bonded to the alloy restoration with different cements. According to the different types of cements used, each group was then randomly subdivided into 5 sub-groups (n = 8 in each sub-group). The characteristics of the five commercial cements used in this study were summarized in Table 1. The bonded specimens were then stored in water at 37℃ for 24 hours, and the shear bond strength was measured using a universal testing machine (858 Mini BionixII, MTS Systems Corp., Eden Prairie, MN, USA) at a speed of 0.5 mm/min. The shear strength values were calculated as the following formula: R = F / A, where R represented to the shear strength in MPa, F was the load required to break the bond of dentin-restorations, and A correspond to the bonding area.9
Table 1. The characteristics of the five commercial cements used in this study.
| Materials | Type | Main compositiona | Adhesive system | Manufacturer |
|---|---|---|---|---|
| Harvard Cement | Zinc-phosphate cement | P: zinc oxide L: phosphoric acid |
No adhesive system | Harvard Dental International, Germany |
| Durelon | Zinc-polycarboxylate cement | P: zinc oxide, zinc fluoride, dried polyacrylic acid L: diluted polyacrylic acid |
No adhesive system | 3M ESPE, Seefeld, Germany |
| Ketac Cem Easymix | Conventional glass ionomer cement | P: Glass powder, polycarboxylic acid, pigments L: Water, tartaric acid, conservation agents |
No adhesive system | 3M ESPE, Seefeld, Germany |
| RelyX Luting | Resin-modified glass ionomer cement | P: radiopaque fluorine-alumina-silica-glass, L: water-based, modified polyalcenic acid, HEMA |
No adhesive system | 3M ESPE, Seefeld, Germany |
| RelyX Unicem | Self-adhesive universal resin cement | Phosphoric acid methacrylates, dimethacrylates, inorganic fillers, fumed silica, initiators | No adhesive system | 3M ESPE, Seefeld, Germany |
P, Power; L, liquid
aAccording to the information provided by the manufacturers
Four failure types were determined based on the previous description10: (1) cement mainly on dentin (more than 75%); (2) cement on both casting and dentin (between 25% and 75%); (3) cement mainly on casting (more than 75%); (4) fracture of tooth without casting separation. Failure types were observed under a stereomicroscope at × 16 magnification.
The data were analyzed using SPSS version 15.0. Results were expressed as mean ± SD and analyzed by one-way ANOVA and LSD multiple comparison tests. P < .05 was considered to be statistically significant.
RESULTS
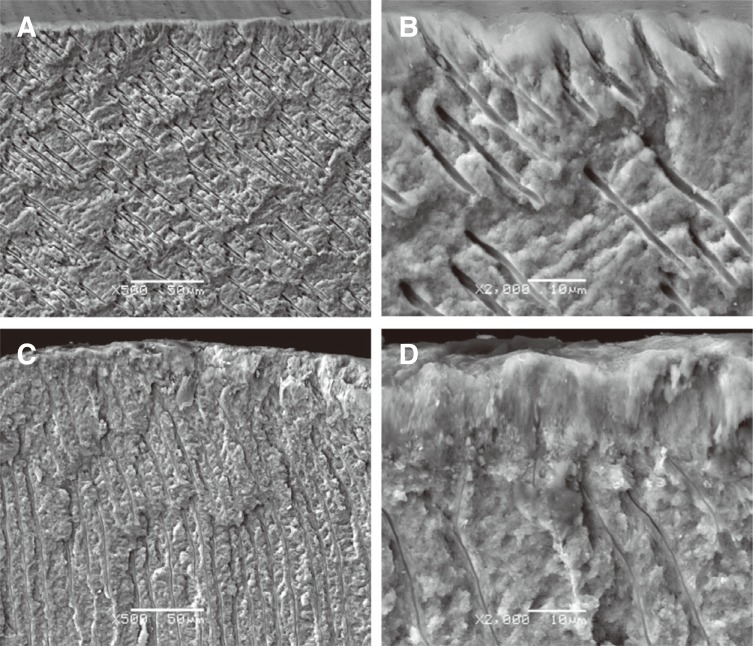
Photomicrographs for the premolars untreated or treated with Hybrid Coat were shown in Figure 1. The dentin in control group (Fig. 1A) revealed that the dentinal tubules were well arranged, and the lumens were partially open. At high magnification (Fig. 1B), well-demarcated structures were observed in the tubules, with a 2 – 3 µm partially open lumen, as well as some impurities. For the premolars treated with Hybrid Coat desensitizing agent (Fig. 1C and Fig. 1D), a thin coating layer was observed, but the majority of dentinal tubules were covered, and their lumens were plugged.
Fig. 1. SEM images of untreated dentin in group 1 (control group) at a magnification of ×500 (A) and ×2000 (B), no smear layer or smear plugs were observed, lateral canals were seen in the tubule walls. SEM images of dentin treated with Hybrid Coat Desensitizer (group 2) at a magnification of ×500 (C) and ×2000 (D), a thin layer of Hybrid Coat over the dentin that occluded the lumens of dentinal tubules.
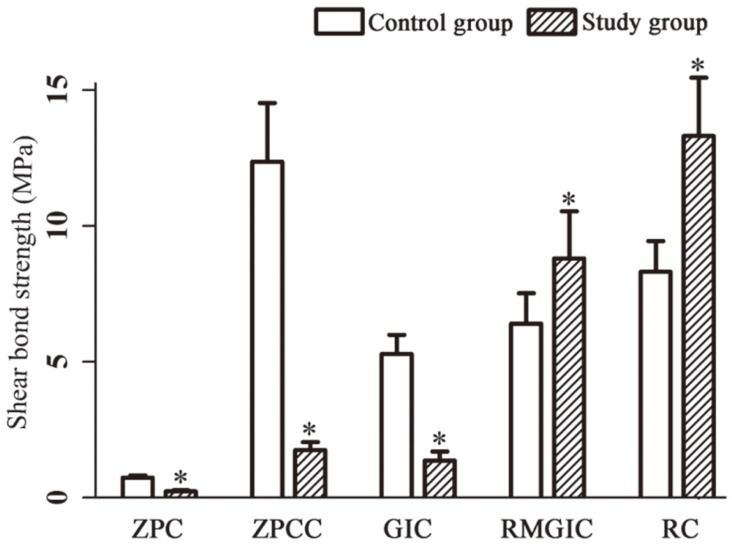
Figure 2 showed the shear bond strength values of each sub-group. For the control group, the lowest shear bond strength was found in ZPC sub-group with a value of 0.746 ± 0.078 MPa. There were significant differences within the last four sub-groups, which ranged from 5.284 ± 0.715 MPa (GIC) to 12.363 ± 2.160 MPa (ZPCC). After treated with Hybrid Coat, the shear bond strength in RMGIC and RC sub-groups were significantly higher than that in the control group (P = .005, P = .000). However, the performance in the ZPC, ZPCC, and GIC sub-groups were significantly reduced, when compared with control group.
Fig. 2. Values of shear bond strength (in MPa) for each group. Data were represented as mean ± SD. Compared with control group, *P < .05.
Statistical analyses showed there were significant statistical differences in shear strengths between the control group and the study group (P < .05). The RC-Hybrid Coat subgroup displayed the highest bond shear strength (13.309 ± 2.152 MPa), and the ZPC-Hybrid Coat sub-group had the lowest value (0.228 ± 0.039 MPa). The order of shear bond strength for the five commercial cements were RC-Hybrid Coat > RMGIC-Hybrid Coat > ZPCC-Hybrid Coat > GIC-Hybrid Coat > ZPC-Hybrid Coat.
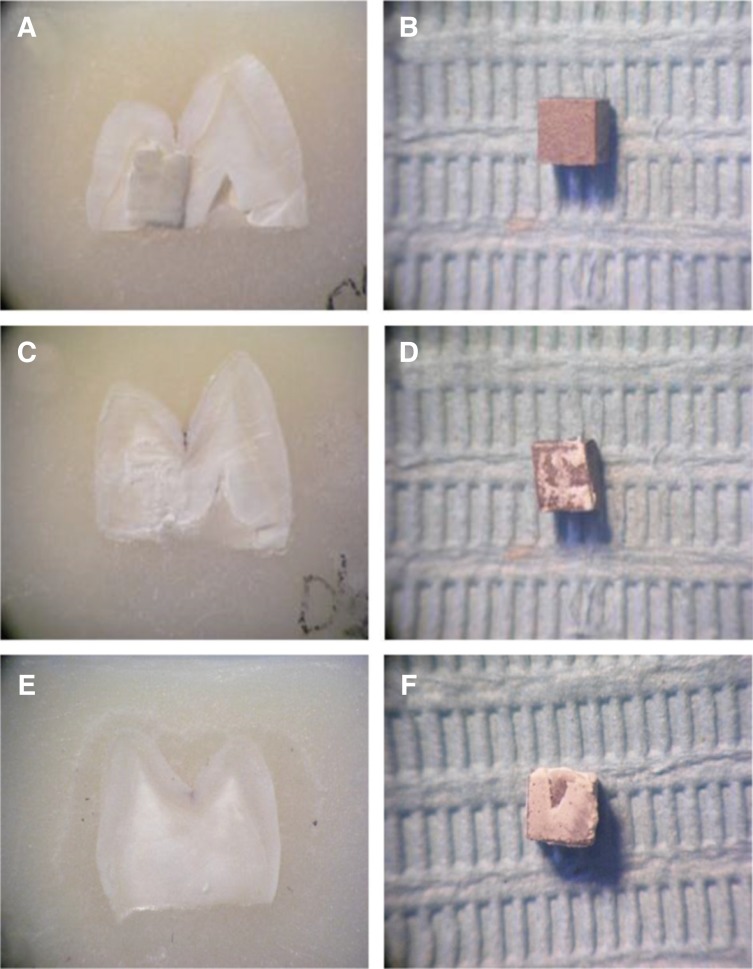
The results of fracture analysis were presented in Table 2 and illustrated in Fig. 3. The most occurred failure types in this study was types 1 – 3, and the failure type 4 (fracture of the tooth without casting separation) was not observed, irrespective of tensile strength applied.
Table 2. Frequency of failure types for each group after debonding.
| Failure mode | Decementing of the crown | Failure in the tooth | Failure mode | Decementing of the crown | Failure in the tooth | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1 (freq.) | 2 (freq.) | 3 (freq.) | 4 (freq.) | 1 (freq.) | 2 (freq.) | 3(freq.) | 4 (freq.) | ||
| ZPC | 5 | 3 | 0 | 0 | ZPC-Hybrid Coat | 0 | 2 | 6 | 0 |
| ZPCC | 4 | 3 | 1 | 0 | ZPCC-Hybrid Coat | 0 | 3 | 5 | 0 |
| GIC | 2 | 5 | 1 | 0 | GIC-Hybrid Coat | 0 | 3 | 5 | 0 |
| RMGIC | 0 | 3 | 5 | 0 | RMGIC-Hybrid Coat | 3 | 3 | 2 | 0 |
| RC | 2 | 5 | 1 | 0 | RC-Hybrid Coat | 7 | 1 | 0 | 0 |
Fig. 3. The illustration of different failure types. Failure type 1, cement mainly on dentin (A and B); failure type 2, cement on both casting and dentin (C and D); failure type 3, cement mainly on casting (E and F).
In the control group, failure type 1 accounted for the highest proportion in ZPC (62.5%) and ZPCC sub-groups (50.0%). The addition of Hybrid Coat to these cements reduced the occurrence of failure type 1 and caused a greater number of failure type 3. There were significant differences in the distribution of failure types between the control group and the study group when bonded with ZPC and ZPCC, respectively. For the GIC sub-group, failure type 2 was the most frequent, and type 3 was in the majority when Hybrid Coat was added. However, statistical results revealed no significant difference between the GIC and GIC-Hybrid Coat sub-groups. For RMGIC sub-group, failure type 3 was prevalent, while in RMGIC-Hybrid Coat sub-group, both failure type 1 and type 2 accounted for 37.5%, and the rest 25.0% was observed in failure type 3. There was no statistically significant difference between the two sub-groups. For RC sub-group, failure type 2 was dominated, while failure type 1 was the most common for RC-Hybrid Coat subgroup. There were significant differences in the distribution of failure types between RC and RC-Hybrid Coat subgroup. Failure type 4 did not occur in this study.
DISCUSSION
The present study confirmed our hypothesis that the combination use of dentin desensitizer and crown cementation agent would alter the shear bond strength. Hybrid Coat sealed the dentinal tubules effectively. In order to fix the restorations, teeth had to be prepared to offer enough space for restorations. During this process, the mineralized tissue was shattered, and thus considerable debris was produced. Much debris accumulated on the dentin surface and formed the smear layer.11 Removing the smear layer could open the dentinal tubules and initiate a hypersensitive lesion.12 In clinical situations, the thickness and roughness of the smear layer were varied with the dental rotary instruments used13,14 and the way in which the smear layer was produced.15
In the current study, in order to simulate the clinical tooth preparation, a yellow polishing bur was used to grind and polish the dentin surface. Dentin untreated with Hybrid Coat showed substantial deposits in the tubule lumens. 4-Methacryloxyethyl trimellitic anhydride (4-META) was the core component of Hybrid Coat, and it could promote the penetration of monomers into demineralized tooth structure.16 A thinner coating film is required for the application of resin coating technique on crown preparation. Nikaido et al.17 found that a single coat of Hybrid Coat was 5 – 6 µm thick approximately, and the hybrid layer was less than 1.0 µm thick, which was appropriate for crown preparation. Takahashi et al.18 revealed that dual-application of all-in-one adhesive systems, such as Hybrid-Coat, created a thin coating on dentin and significantly improved the bond strengths of resin cements. Consistent with previous studies, the present study found that Hybrid Coat formed a thin hybrid layer under the stereomicroscope observation, and it was capable of plugging the exposed dentinal tubule effectively.
The use of Hybrid Coat could isolate the external environment from internal environment, and therefore, the exposed dentin was protected, the postoperative pain was alleviated, and the secondary caries could be prevented. Cements were commonly used dental adhesive materials, and they were often used for bonding restorations and tooth structure. The different five frequently-used cements were chosen in this study. There were significant differences among them in the shear bond strength. The strength value listed in turn: ZPCC > RC > RMGIC > GIC > ZPC. When the cements were combined with Hybrid Coat, the strength order was changed as RC > RMGIC > ZPCC > GIC > ZPC, the change might come from their different bonding mechanism. Our findings were in agreement with the other studies. RMGIC was proved to exhibit greater shear-peel band strengths than the ZPC.19 In addition, a previous study conducted by Piwowarczyk A demonstrated that only the self-adhesive universal resin cement (RelyX Unicem) and RC showed strong bond strengths to specific prosthodontic materials, but ZPC, GIC, RMGIC exhibited the lowest values.20 Peutzfeldt et al.21 compared the 6 types of luting agents when used to bond different indirect, laboratory restorative materials to human dentin, implying that ZPC and GIC produced the lowest bond strengths, whereas the self-etch RC and self-adhesive RC had the highest bond strengths.
It was reported that the degree of polymerization and mechanical properties of bonding resin influence the bond strength to dentin.22 The use of Hybrid Coat reduced the adhesion of ZPCC, ZPC, and GIC to teeth in this study. The possible explanation was that, ZPCC and GIC cements bond to teeth mainly via the mechanical retention and chemical retention. The reaction between polyacrylic acid and calcium ions of hydroxyapatite made the bonding tighter, especially for ZPCC. The addition of Hybrid Coat sealed the dentin tubules and thereby generated an altered dentin interface, which would prevent their interaction. It was further confirmed by the high proportion of failure type 3 when debonding. For ZPC, the main bonding force was the mechanical retention, and the application of Hybrid Coat made the decline of mechanical retention, so the shear bond strength in ZPC-Hybrid Coat sub-group was remarkably lower than that in ZPC sub-group. However, Hybrid Coat significantly enhanced the shear bond strength when bonded with RMGIC and RC. The increased adhesive performance might come from the interaction between Hybrid Coat and the cements. The main component of RelyX luting, hydroxyethyl methacrylate (HEMA), had two function groups: the hydrophilic group and the hydrophobic group. The hydrophilic group could react with dentin collagen,23 and the hydrophobic group could react with resin component of Hybrid Coat, which improved the wettability of dentin and deepened the penetrability of resin monomer. Furthermore, 4-META could increase the integrity of composite materials, which was attributed to the extensive crosslinking.24 The positive effect of 4-META on bond strength for adhesive resins to dentin has also been observed and then were substantiated by the high proportion of failure type 1 when debonding, which indicated the difficulty in the break between the cement and dentin.
There are some limitations. This research focused on the Hybrid Coat material and shear bond strength of 5 kinds of cements. The material should also be evaluated in many aspects, such as sealing performance, micro leakage, etc. In addition, the bonding mechanism of the Hybrid Coat and 5 kinds of cements was not lucubrated in this paper. Therefore, we should pay more attention on the bonding mechanisms, and sealing performance and micro leakage need further study.
CONCLUSION
The study revealed that Hybrid Coat formed a hybrid layer at the surface of the dentin, and it could plug the exposed dentinal tubule effectively. Additionally, the Hybrid Coat significantly improved the shear bond strengths of RC and RMGIC cements, while reducing the performance of ZPC, ZPCC, and GIC cements. In conclusion, Hybrid Coat is an effective sealant of dentinal tubules and it can be combined with resin cements or resin-modified ionomer cements to attach the prostheses.
Footnotes
This study was supported by National Natural Scientific Foundation of China (81370975); National Natural Scientific Foundation of China (81070278); The Science & Technology Department of Hunan Province (2015JC3012); The Science & Technology Department of Hunan Province (100JJ1007).
References
- 1.Mantzourani M, Sharma D. Dentine sensitivity: past, present and future. J Dent. 2013;41:S3–17. doi: 10.1016/S0300-5712(13)70002-2. [DOI] [PubMed] [Google Scholar]
- 2.Farias D, Walter R, Swift EJ., Jr Critic appraisal. Postoperative sensitivity with indirect restorations. J Esthet Restor Dent. 2014;26:208–213. doi: 10.1111/jerd.12103. [DOI] [PubMed] [Google Scholar]
- 3.Thanatvarakorn O, Nakashima S, Sadr A, Prasansuttiporn T, Thitthaweerat S, Tagami J. Effect of a calcium-phosphate based desensitizer on dentin surface characteristics. Dent Mater J. 2013;32:615–621. doi: 10.4012/dmj.2013-073. [DOI] [PubMed] [Google Scholar]
- 4.Han L, Okiji T. Dentin tubule occluding ability of dentin desensitizers. Am J Dent. 2015;28:90–94. [PubMed] [Google Scholar]
- 5.Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17:144–154. doi: 10.1111/j.1708-8240.2005.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 6.Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94:511–519. doi: 10.1016/j.prosdent.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Carvalho AO, Oliveira MT, Nikaido T, Tagami J, Giannini M. Effect of adhesive system and application strategy on reduction of dentin permeability. Braz Oral Res. 2012;26:397–403. doi: 10.1590/s1806-83242012005000020. [DOI] [PubMed] [Google Scholar]
- 8.Yim NH, Rueggeberg FA, Caughman WF, Gardner FM, Pashley DH. Effect of dentin desensitizers and cementing agents on retention of full crowns using standardized crown preparations. J Prosthet Dent. 2000;83:459–465. doi: 10.1016/s0022-3913(00)70042-4. [DOI] [PubMed] [Google Scholar]
- 9.Reis A, Loguercio AD, Manso AP, Grande RH, Schiltz-Taing M, Suh B, Chen L, Carvalho RM. Microtensile bond strengths for six 2-step and two 1-step self-etch adhesive systems to enamel and dentin. Am J Dent. 2013;26:44–50. [PubMed] [Google Scholar]
- 10.Wolfart S, Linnemann J, Kern M. Crown retention with use of different sealing systems on prepared dentine. J Oral Rehabil. 2003;30:1053–1061. doi: 10.1046/j.1365-2842.2003.01180.x. [DOI] [PubMed] [Google Scholar]
- 11.Violich DR, Chandler NP. The smear layer in endodontics - a review. Int Endod J. 2010;43:2–15. doi: 10.1111/j.1365-2591.2009.01627.x. [DOI] [PubMed] [Google Scholar]
- 12.Cummins D. Dentin hypersensitivity: from diagnosis to a breakthrough therapy for everyday sensitivity relief. J Clin Dent. 2009;20:1–9. [PubMed] [Google Scholar]
- 13.Tani C, Finger WJ. Effect of smear layer thickness on bond strength mediated by three all-in-one self-etching priming adhesives. J Adhes Dent. 2002;4:283–289. [PubMed] [Google Scholar]
- 14.Faus-Matoses I, Solá-Ruiz F. Dental preparation with sonic vs high-speed finishing: analysis of microleakage in bonded veneer restorations. J Adhes Dent. 2014;16:29–34. doi: 10.3290/j.jad.a30754. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira SS, Pugach MK, Hilton JF, Watanabe LG, Marshall SJ, Marshall GW., Jr The influence of the dentin smear layer on adhesion: a self-etching primer vs. a total-etch system. Dent Mater. 2003;19:758–767. doi: 10.1016/s0109-5641(03)00023-x. [DOI] [PubMed] [Google Scholar]
- 16.Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16:265–273. doi: 10.1002/jbm.820160307. [DOI] [PubMed] [Google Scholar]
- 17.Nikaido T, Nakaoki Y, Ogata M, Foxton R, Tagami J. The resin-coating technique. Effect of a single-step bonding system on dentin bond strengths. J Adhes Dent. 2003;5:293–300. [PubMed] [Google Scholar]
- 18.Takahashi R, Nikaido T, Ariyoshi M, Kitayama S, Sadr A, Foxton RM, Tagami J. Thin resin coating by dual-application of all-in-one adhesives improves dentin bond strength of resin cements for indirect restorations. Dent Mater J. 2010;29:615–622. doi: 10.4012/dmj.2009-110. [DOI] [PubMed] [Google Scholar]
- 19.Aggarwal M, Foley TF, Rix D. A comparison of shear-peel band strengths of 5 orthodontic cements. Angle Orthod. 2000;70:308–316. doi: 10.1043/0003-3219(2000)070<0308:ACOSPB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Piwowarczyk A, Lauer HC, Sorensen JA. In vitro shear bond strength of cementing agents to fixed prosthodontic restorative materials. J Prosthet Dent. 2004;92:265–273. doi: 10.1016/j.prosdent.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 21.Peutzfeldt A, Sahafi A, Flury S. Bonding of restorative materials to dentin with various luting agents. Oper Dent. 2011;36:266–273. doi: 10.2341/10-236-L. [DOI] [PubMed] [Google Scholar]
- 22.Swift EJ, Jr, Wilder AD, Jr, May KN, Jr, Waddell SL. Shear bond strengths of one-bottle dentin adhesives using multiple applications. Oper Dent. 1997;22:194–199. [PubMed] [Google Scholar]
- 23.Yilmaz Y, Dalmis A, Gurbuz T, Simsek S. Retentive force and microleakage of stainless steel crowns cemented with three different luting agents. Dent Mater J. 2004;23:577–584. doi: 10.4012/dmj.23.577. [DOI] [PubMed] [Google Scholar]
- 24.Atsuta M, Abell AK, Turner DT, Nakabayashi N, Takeyama M. A new coupling agent for composite materials: 4-methacryloxyethyl trimellitic anhydride. J Biomed Mater Res. 1982;16:619–628. doi: 10.1002/jbm.820160509. [DOI] [PubMed] [Google Scholar]