Abstract
Objective
Officers' volunteering for Crisis Intervention Team (CIT) training—rather than being assigned—is assumed to be an important, beneficial self-selection bias. This bias remains poorly characterized, though CIT officers are more likely to be female and to have had exposure to the mental health field. We determined whether or not self-selection is beneficial with regard to knowledge, attitudes, and skills, as well as level of force used (i.e., no or low force versus any form of physical force) and disposition of subjects, in actual encounters.
Methods
We compared CIT-trained officers who had volunteered with those who had been assigned using data from two prior, linked studies that compared CIT-trained and non-CIT officers on knowledge, attitudes, and skills (251 CIT-trained officers; 68% had volunteered), as well as behaviors (517 actual encounters provided by 91 CIT-trained officers; 70% had volunteered).
Results
Of 28 scores on knowledge, attitudes, and skills compared, six were statistically significantly different (p<.01) and another eight were marginally significant (.01<p<.05). Furthermore, although CIT officers who had volunteered were more likely to report use of some form of physical force as we had defined it (which included the use of handcuffs), when they did so, they were more likely to refer to treatment services and less likely to make an arrest. These effects were apparent even when taking into account effects of gender, having had exposure to the mental health field, empathy, and other covariates.
Conclusions
We found evidence for benefits of self-selection/volunteering that should be further characterized as it appears to be associated with better outcomes with regard to key attitudes, skills, and behaviors.
Keywords: Crisis Intervention Team, law enforcement, mental illness, police
The Crisis Intervention Team (CIT) model of police response to mental health crises developed out of a collaboration among multiple stakeholders in Memphis, Tennessee, after an officer shot and killed a man with a mental illness in 1987 (Cochran & Deane, 2000). The model includes and is most known for 40 hours of specialized training for patrol officers in recognizing and responding to mental health crises (Dupont, Cochran, & Pillsbury, 2007). Officers completing CIT training take on a specialist role when responding to mental health crisis situations. However, CIT is more than training, as it requires and cultivates collaboration among community stakeholders to improve system-wide coordination (Cochran, 2004). Core elements include establishing a centralized site to which officers can transport persons in crisis for emergency evaluation, while improving policies for both law enforcement and mental health agencies to allow more seamless transfers to appropriate care (Dupont et al., 2007). The goals of CIT are to improve safety in encounters between police and persons in crisis and to divert individuals with mental illnesses from arrest to psychiatric treatment whenever possible.
As diverse law enforcement agencies implement CIT, practices vary. One area of variation is the extent to which officers enrolled in CIT training are “self-selected” and voluntary, as opposed to being assigned to the training. The widely accepted core elements of CIT indicate that officers should voluntarily apply for the program (Dupont et al., 2007, p. 12): “Officers within a patrol division should voluntarily apply for CIT positions. Each candidate then goes through a selection process, which is assessed according to the officer's application, recommendations, personal disciplinary police file, and an interview. Once selected, each of the CIT Officers maintains their role as a patrol officer and gains new duties and skills through the CIT training, serving as the designated responder and lead officer in mental health crisis events.” As an empirical question, however, the potential value of volunteering remains largely untested. Some evidence suggests that self-selected CIT officers are more likely to have been exposed to mental health professionals, though they do not significantly differ in empathy or psychological mindedness before their training (Compton, Broussard, Hankerson-Dyson, Krishan, Stewart-Hutto, 2011). However, little research is available on whether or not self-selected/volunteering officers differ from assigned officers in meaningful ways after completing CIT training.
We used extensive data from two previous studies (Compton et al., 2014a; Compton et al., 2014b) to thoroughly compare self-selected/volunteered versus assigned CIT officers. In light of limited available evidence, we hypothesized that baseline differences would exist—in gender, years of service as an officer, educational level, and exposure to the mental health field, the latter meaning having personally (or in a family member or friend) received mental health treatment or volunteered or worked in the mental health field—indicating a potentially beneficial “self-selection bias” into CIT training. But given no prior research comparing volunteered versus assigned CIT officers on outcomes, we tested the null hypothesis that, after going through the same training, and when controlling for the expected pre-trainng differences noted above, eight post-training outcomes would not differ. Those outcomes included (1) knowledge about mental illnesses, (2) attitudes toward mental illnesses and their treatments, (3) self-efficacy for working with individuals with mental illnesses, (4) stigma, (5) de-escalation skills, (6) referral decisions, (7) level of force used, meaning which of several techniques or equipment was used (no or low force versus physical force, which included using handcuffs or other devices, or any physical engagement), and (8) disposition (resolution at the scene with no further action, referral to services or transport to a treatment facility, or arrest). That is, in comparing the two groups, we assumed equivalence in training outcomes—that assigned officers would be equally equipped to serve as CIT officers compared to those who had self-selected/volunteered. The findings could have substantial policy implications given the extent of implementation of CIT across the U.S.
Methods
We previously examined differences in six constructs (knowledge about mental illnesses, attitudes toward mental illnesses and their treatments, self-efficacy for interacting with persons with serious mental illnesses, stigma, de-escalation skills, and referral decisions) between 251 CIT-trained and 335 non-CIT officers (Study 1; Compton et al., 2014a), and differences in level of force and disposition in 1,063 actual encounters involving 180 officers recruited from Study 1, 91 with and 89 without CIT training (Study 2; Compton et al., 2014b). We now consider only CIT-trained officers from these studies, comparing those who reported having volunteered for CIT training with those who reported having been assigned to it, according to their response to an item on how they entered CIT training from Study 1. Both prior studies were approved by the Emory University Institutional Review Board, and participants provided written informed consent.
Study 1 Participants and Methods
Of the 251 CIT-trained officers in Study 1, 171 (68%) volunteered and 80 (32%) were assigned to CIT training. As described previously (Compton et al., 2014a), officers were recruited from six law enforcement agencies in Georgia, each having implemented CIT training with local instructors and a standardized 40-hour curriculum from a statewide CIT initiative (Oliva & Compton, 2008). After hearing about the study through roll-call presentations, e-mail notices, flyers posted in department precincts, or word of mouth, officers interested in participating called to register for one of 34 proctored survey administrations (April–October 2010). Officers took part during off-duty hours and were remunerated for travel/parking and approximately three hours of survey participation.
The mean±SD age and years of service of the 251 CIT officers was 37.3±8.9 and 10.1±7.4, respectively; 67 were women (26.7%). Of 245 who specified their education, 31 (12.4%) were high school graduates, 103 (41.0%) had completed some college, and 111 (44.2%) had an associate's or higher degree. Ninety (35.9%) self-identified as African American, 151 (60.2%) as Caucasian/non-Hispanic, and 10 (4.0%) as other. The median time since CIT training was 22 months, varying from <1 month to >7 years.
As detailed previously (Compton et al., 2014a), about one-third of the survey dealt with demographics, exposure to the mental health field, empathy, knowledge, and attitudes. The remainder focused on attitudinal and behavioral responses to two vignettes, one written and one video, developed specifically for this study—depicting a man exhibiting signs of agitation and psychosis digging through a trashcan, with an officer arriving on the scene (“the psychosis vignette”), and a woman showing intoxication and suicidality who had locked herself in her home bathroom, with an officer arriving on the scene (“the suicidality vignette”).
We derived the following scores from Study 1: two key potential covariates (exposure to the mental health field and empathy), demographic covariates (age, years as an officer, gender, race, time since CIT training, and educational attainment), and 28 measures constituting the six constructs of interest. Exposure to the mental health field was based on four items that asked whether the participant (referred to herein as “self”), a family member, or a friend had received or was now receiving mental health treatment, or whether the participant or family members or friends had volunteered or worked in the mental health field (“other”) (Compton et al., 2014a). Specifically, we created an exposure index, coded 0–5, to summarize these four items: 0 if they responded negatively to all four items; 1 for an affirmative response only to “other”; 2 if they responded yes only to “friend,” and maybe “other” as well; 3 if they responded yes to “family” but not “friend,” and maybe “other” as well; 4 if they responded yes to both “family” and “friend,” and maybe “other’ as well; and 5 if they responded affirmatively to “self.” The construct of empathy toward individuals with mental illnesses (Compton et al., 2011) was assessed with an adapted version of a 9-item measure (Levy, Freitas, & Salovey, 2002). In response to “indicate how much you feel each emotion toward people with mental illnesses,” each item (e.g., compassion, disgust, respect) is rated 0=not at all, to 10=extremely; Cronbach's α=.78.
To measure knowledge about mental illnesses, officers completed the 33-item Knowledge of Mental Illnesses Test (Compton, Hankerson-Dyson, & Broussard, 2011), scored as the percentage correct. Attitudes about mental illnesses and their treatments, the second construct, was assessed with 17 scores, the first of which was an attitudes score derived from three measures (Broussard et al., 2011; Cohen & Struening, 1962; Struening & Cohen, 1963; Talyor & Dear, 1981; Taylor, Dear, & Hall, 1979), as described previously (Compton et al., 2014a). An additional 12 scores were derived from the Attribution Questionnaire (Corrigan, River, & Lundin, 1999; Corrigan et al., 2003), and the final four from the Revised Causal Dimensions Scale (McAuley, Duncan, & Russell, 1992; Russell, 1982; Russell, McAuley, & Tarico, 1987) corresponding to each vignette. Self-efficacy for deescalating crisis situations and referring to treatment (Broussard et al., 2011) was assessed with two scores, one for each vignette (Compton et al., 2014a). Stigma toward people with mental illnesses was assessed with four scores, two for each vignette, using two instruments—an adapted version of the Social Distance Scale and a semantic differential measure (Compton et al., 2014a). Finally, de-escalation skills and referral decisions were each assessed with two scores, one for each vignette, using two instruments designed specifically for Study 1 and tested previously in an independent sample of nearly 200 officers (Broussard et al., 2011). We used all of these same variables to be consistent with the previously published study (Compton et al., 2014a), which had compared CIT-trained and non-CIT officers in terms of knowledge about mental illnesses, attitudes toward mental illnesses and their treatments, self-efficacy for interacting with persons with serious mental illnesses, stigma, de-escalation skills, and referral decisions.
Study 2 Participants and Methods
Of the 91 CIT-trained officers participating in Study 2, 64 (70%) reported having volunteered for, and 27 (30%) reported having been assigned to, CIT training. They contributed 368 and 149 encounter reports, respectively. The modal number of reports per officer was four, and the number submitted did not vary significantly between volunteered and assigned groups. Their mean±SD age and years of service were 37.2±8.2 and 10.2±7.5, respectively; 28 (31%) were women. Of the 88 who specified their education, nine (10.2%) were high school graduates, 44 (50.0%) had completed some college, and 47 (53.4%) had an associate's or higher degree. Thirty-seven (40.7%) identified as African American, 53 (58.2%) as Caucasian/non-Hispanic, and one (1.1%) as Hispanic. The median number of months since training was 23. They did not differ significantly with respect to age, gender, education, race, or time since training from the 160 CIT-trained officers in Study 1 who did not participate in Study 2.
As detailed previously (Compton et al., 2014b), the encounter form was a doubled-sided page consisting mostly of check-boxes, which could be completed in 1–2 minutes (Compton et al., 2014b; Krishan et al., 2014). For level of force, officers checked which of several techniques or equipment was used (no level of force was checked for 14 encounters, so n=503). We defined two levels: no or low force (406, 81%) and physical force (97, 19%). Physical force was coded if the officer checked that handcuffs were used or “I pushed, hit, grabbed, or otherwise physically engaged the subject” or used physical maneuvers (for example, soft or hard empty hands) or devices to handle the situation. For disposition, encounters were coded as resolution at the scene with no further action (245, 47%), referral to services or transport to a treatment facility (205, 40%), or arrest (67, 13%). We used these same variables to be consistent with the previously published Study 2 (Compton et al., 2014b), which had compared CIT-trained and non-CIT officers on levels of force and dispositions including resolution, referral, and arrest.
Statistical Analysis
As in Study 1 (Compton et al., 2014a), for analyses involving the six key constructs of interest, because of the extent of the data from multiple measures and the number of analyses, we used p<.01 as significant; effects significant at the .05 but not the .01 level are referred to as marginal. We present effect sizes (Cohen's d) (Cohen, 1988) in addition to statistical significance (Wilkinson, 1999), where .2 is a small (weak), .5 is a medium (moderate), and .8 is a large (strong) effect.
For analyses using Study 2 (Compton et al., 2014b) data, descriptive statistics are reported primarily in percentages. Odds ratios (ORs) were used to characterize effects of CIT officers' volunteered versus assigned status. Because encounters were nested within officers, ORs were estimated with MPlus 6.1, which accommodates multilevel models, including those with binary outcomes. With MPlus, ORs are usually >1 when the volunteered percentage is higher than the assigned percentage, and <1 when it is not. ORs with 95% confidence intervals (CIs) excluding 1 are deemed significant. However, when cell numbers are small (low power), we consider OR values ≤.33 or ≥3.00 as strong effects; >.33 but ≤.50, or ≥2.00 but <3.00 as moderate effects; and >.50 but ≤.80, or ≥1.25 but <2.00 as weak effects (Compton et al., 2014b; Bakeman & Quera, 2011).
Results
Group Differences in Background Characteristics, Exposure, and Empathy
CIT officers who had volunteered for their training did not differ in age, years as an officer, gender, race, or time since training, from those who had been assigned, and this was true for both Study 1 and Study 2 participants. Study 1 officers who had volunteered had a higher educational attainment; e.g., 82 (49%) had a degree, compared to 29 (37%) in assigned officers; χ2=9.25, df=2, p=.010. This significant educational difference was not apparent in the smaller group of Study 2 participants (χ2=5.41, df=2, p=.067). The mean exposure index score (regarding exposure to the mental health field) was higher among officers who reported having volunteered than among those who reported having been assigned (2.6 versus 2.0 on a 0–5 scale; t=2.40, df=249, d=.33, p=.017). The groups did not differ significantly on empathy (t=1.18, df=249, d=.16, p=.24).
Group Differences in the Six Key Constructs from Study 1
For consistency with the earlier report (Compton et al., 2014a), group differences were examined with analyses of covariance including age, gender, years as an officer, years of education, the exposure index, and empathy as covariates. Controlling for these covariates did not substantially change the between-group differences observed with t tests. Officers who had volunteered for their training differed in several ways from those who had been assigned (Table 1). As would be expected with a smaller sample size (251, as opposed to 586 in Study 1), fewer differences were significant in the current study as compared to the CIT-trained versus non-CIT differences in Study 1 (six rather than 18 were statistically significant, and eight rather than four were marginally significant). However, the magnitudes of effects—which are a more appropriate metric when comparing samples of different sizes—were about the same: 17 of 28 were at least weak for volunteered–assigned comparisons, and 19 of 28 were at least weak for CIT-trained–non-CIT comparisons. Additionally, those effects that were at least weak were all in the same direction: positive items were more positive, and negative items were less negative, for the volunteered versus assigned group.
Table 1. Measures of six key constructs among police officers who had volunteered or had been assigned to Crisis Intervention Team (CIT) training.
| Variablea | Possible score range | Volunteered for training | Assigned to training | t | df | p | d b | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| N of respondents | Score | N of respondents | Score | ||||||||
|
|
|
||||||||||
| M | SD | M | SD | ||||||||
| Knowledge about mental illnesses | 0–100 | 171 | 60 | 16 | 80 | 58 | 14 | –.61 | 249 | .54 | .08 |
| Attitudes toward mental illnesses and their treatments | |||||||||||
| Opinions About Mental Illnesses Scale | 1–6 | 169 | 4.29 | .43 | 80 | 4.14 | .48 | –2.48 | 247 | .014 | .34 |
| Attribution Questionnaire (vignette) | |||||||||||
| Personal responsibility (P) | 1–9 | 171 | 2.56 | 1.34 | 78 | 2.51 | 1.24 | –.29 | 247 | .78 | .04 |
| Personal responsibility (S) | 1–9 | 171 | 4.62 | 1.75 | 80 | 5.44 | 1.82 | 3.40 | 249 | .001 | –.46 |
| Pity (P) | 1–9 | 171 | 6.39 | 1.75 | 78 | 6.24 | 1.68 | –.65 | 247 | .51 | .09 |
| Pity (S) | 1–9 | 170 | 5.95 | 1.68 | 80 | 5.83 | 1.85 | –.47 | 248 | .64 | .06 |
| Anger (P) | 1–9 | 171 | 3.13 | 1.72 | 78 | 3.64 | 1.71 | 2.17 | 247 | .031 | –.30 |
| Anger (S) | 1–9 | 171 | 2.92 | 1.58 | 80 | 3.58 | 1.75 | 2.93 | 249 | .004 | –.40 |
| Fear (P) | 1–9 | 171 | 4.58 | 1.72 | 78 | 5.00 | 1.74 | 1.76 | 247 | .080 | –.24 |
| Fear (S) | 1–9 | 171 | 4.17 | 1.59 | 80 | 4.43 | 1.71 | 1.20 | 249 | .23 | –.16 |
| Help (P) | 1–9 | 171 | 3.66 | 1.46 | 79 | 3.09 | 1.15 | –3.04 | 248 | .003 | .41 |
| Help (S) | 1–9 | 171 | 5.15 | 1.82 | 80 | 4.63 | 1.72 | –2.14 | 249 | .033 | .29 |
| Coercion-segregation (P) | 1–9 | 170 | 4.64 | 1.75 | 79 | 5.03 | 1.76 | 1.65 | 247 | .10 | –.23 |
| Coercion-segregation (S) | 1–9 | 171 | 3.02 | 1.58 | 80 | 3.15 | 1.52 | .61 | 249 | .54 | –.08 |
| Revised Causal Dimensions Scale | |||||||||||
| External control (P) | 1–9 | 171 | 4.64 | 1.70 | 79 | 4.46 | 1.65 | –.78 | 248 | .43 | .11 |
| External control (S) | 1–9 | 171 | 4.80 | 1.58 | 80 | 4.58 | 1.75 | –.98 | 249 | .33 | .13 |
| Personal control (P) | 1–9 | 171 | 3.55 | 1.59 | 79 | 3.39 | 1.65 | –.70 | 248 | .48 | .10 |
| Personal control (S) | 1–9 | 171 | 5.82 | 1.81 | 80 | 6.35 | 1.64 | 2.23 | 249 | .027 | –.30 |
| Self-efficacy | |||||||||||
| Self-efficacy (P) | 1–4 | 171 | 3.40 | .43 | 79 | 3.22 | .44 | –3.07 | 248 | .002 | .42 |
| Self-efficacy (S) | 1–4 | 171 | 3.52 | .41 | 80 | 3.32 | .41 | –3.74 | 249 | <.001 | .51 |
| Stigma | |||||||||||
| Social distance (P) | 1–4 | 171 | 4.77 | .80 | 79 | 4.92 | .91 | 1.28 | 248 | .20 | –.17 |
| Social distance (S) | 1–4 | 166 | 4.62 | .91 | 78 | 4.71 | .94 | .68 | 242 | .50 | –.09 |
| Stigmatizing attitudes (P) | 0–9 | 171 | 2.37 | .69 | 79 | 2.57 | .62 | 2.19 | 248 | .030 | –.30 |
| Stigmatizing attitudes (S) | 0–9 | 171 | 2.01 | .68 | 80 | 2.24 | .67 | 2.51 | 249 | .013 | –.34 |
| Deescalation skills | |||||||||||
| Deescalation skills (P) | 1–4 | 171 | 3.23 | .36 | 78 | 3.15 | .35 | –1.65 | 247 | .10 | .23 |
| Deescalation skills (S) | 1–4 | 171 | 3.21 | .32 | 80 | 3.12 | .30 | –2.14 | 249 | .033 | .29 |
| Referral decisions | |||||||||||
| Referral decisions (P) | 1–4 | 171 | 3.50 | .36 | 78 | 3.36 | .38 | –2.82 | 247 | .005 | .39 |
| Referral decisions (S) | 1–4 | 171 | 3.53 | .35 | 80 | 3.40 | .36 | –2.55 | 249 | .011 | .35 |
P, psychosis vignette; S, suicidality vignette.
Cohen's d is the standardized difference between the means.
The groups scored essentially the same on knowledge about mental illnesses, in marked contrast to the earlier study in which, as expected, the CIT-trained group scored significantly higher on knowledge about mental illnesses than the non-CIT group. Results for the 17 items constituting attitudes, our second construct, (the first of which is a mean of six scales) are shown in Table 1. Differences were at least weak for eight items (compared with 10 for the CIT-trained–non-CIT comparisons). In particular, those who volunteered scored lower on anger and higher on help than those assigned. Regarding the remaining four constructs, differences were at least weak for the two self-efficacy items (p=.002 and <.001), two of the four stigma items (p=.030 and .013), the two de-escalation skills items (p=.10 and .033), and the two referral decisions items (p=.005 and .011). The same was true for the CIT-trained–non-CIT comparisons in Study 1 (except that p<.001 for all).
Effect of Volunteering on Disposition and Level of Force
Figure 1 shows the percentage of encounters coded for each disposition and for physical force, by volunteered or assigned status. For all dispositions (resolution on the scene, referral or transport to mental health services, and arrest), percentages were similar for self-selected/volunteered and assigned groups (e.g., 47% and 48% of encounters were resolved on the scene among self-selected/volunteered and assigned officers, respectively) and odds ratios comparing the two groups were not statistically significant (e.g., OR=0.80, p=.50 for resolution on the scene, when comparing self-selected/volunteered and assigned officers). Volunteering CIT officers, however, were more likely to use physical force, as we had defined it, than assigned officers (77 of 279 encounters (22%), versus 20 of 127 (14%); OR=2.24, p=.03, a moderate effect).
Figure 1.
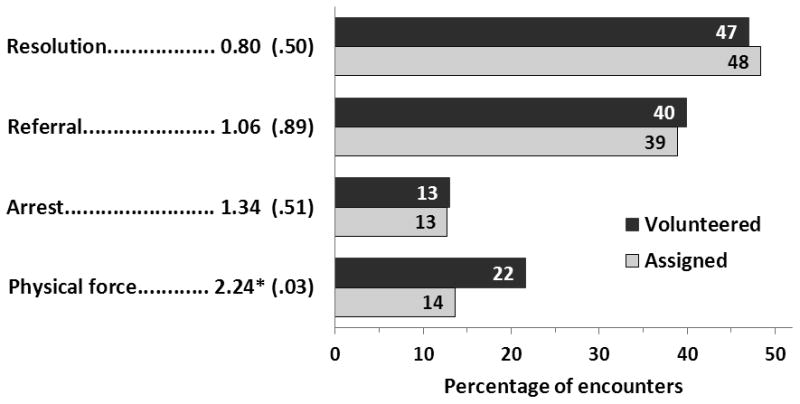
Percentage of encounters for each disposition.
* p < .05
Bars represent the percentage of encounters resulting in each disposition and in physical force, separately for police officers who had self-selected/volunteered for or had been assigned to Crisis Intervention Team (CIT) training. Numbers before the bars are odds ratios, computed by MPlus, comparing volunteered versus assigned percentages (with p-values in parentheses); odds ratios > 1 indicate a higher percentage for volunteered than assigned. Officers who had volunteered coded 368 encounters by disposition and 356 by level of force. Officers who had been assigned coded 149 encounters by disposition and 147 by level of force.
Figure 2 shows the percentage of encounters coded by the two groups for no/low force versus physical force, separately for encounters that resulted in resolution, referral or transport, or arrest. As expected, resolution at the scene was more likely when officers used no or low force (55% among self-selected/volunteered officers and 54% among assigned officers, compared to 14% and 10%, respectively, when physical force was required), and arrest was more likely when they used physical force; however, volunteer status also mattered. When physical force was required, officers who had volunteered for CIT training were more likely than assigned officers to refer or transport to mental health services (39 of 77 encounters (51%), compared to 6 of 20 (30%); OR=3.13, a strong effect, albeit p=.23) and less likely to arrest (27 of 77 (35%), compared to 12 of 20 (60%); OR=.35, a moderate effect, albeit p=.13).
Figure 2.
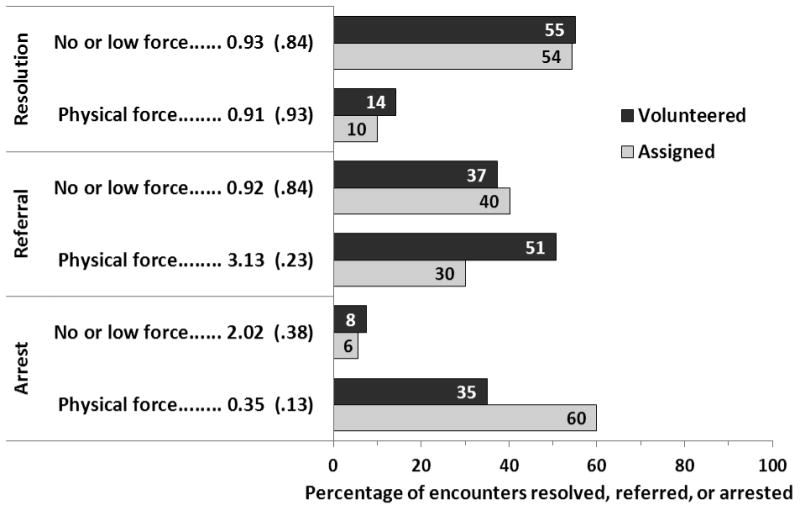
Percentage of encounters resulting in each disposition by level of force used.
Bars represent the percentage of encounters resulting in each disposition by level of force used, separately for officers who had self-selected/volunteered for or been assigned to Crisis Intervention Team (CIT) training. Numbers before the bars are odds ratios, computed by MPlus, comparing volunteered versus assigned percentages (with p-values in parentheses); odds ratios > 1 indicate a higher percentage for volunteered than assigned.
Discussion
Several findings emerged from this first comparison of CIT officers who had volunteered and those who were assigned for training. First, as we had hypothesized, we did observe evidence of baseline differences that confirm the presence of a “self-selection bias” into CIT training. Specifically, CIT officers who had volunteered had a higher level of education and were more likely to have had exposure to the mental health field than those who had been assigned. Second, contrary to the null hypothesis of no meaningful post-training differences between the two groups, we found that, even when controlling for baseline covariates, CIT officers who had volunteered had consistently better scores on a range of measures of attitudes toward mental illnesses and their treatments, self-efficacy for interacting with persons with serious mental illnesses, stigma, de-escalation skills, and referral decisions. Furthermore, the magnitudes of effects mimicked those previously reported (Compton et al., 2014a) in CIT-trained versus non-CIT comparisons. One aspect of training appeared equally effective: the volunteered and assigned groups scored essentially the same on knowledge about mental illnesses.
Third, also partly contrary to our hypothesis of no meaningful post-training differences, we found that although overall dispositions of encounters did not differ between those who had volunteered and those who had been assigned, when physical force was required, officers who had volunteered were more likely to transport or refer to mental health services and less likely to execute an arrest. It should be noted, however, that if they had to handcuff subjects in order to transport them to a treatment facility (as many jurisdictions require), this might explain the apparent increased “use of force.” As such, the somewhat counterintuitive finding pertaining to use of physical force could be an artifact of how we defined physical force.
These findings might have programmatic and policy implications for further dissemination of CIT, especially because many law enforcement agencies are deliberating about training select officers versus training a fixed percentage of or all officers, and no research has yet been available to guide such decisions. In Memphis, where CIT originated, the program is all-volunteer. However, not all jurisdictions have chosen to adhere with the all-volunteer model. Until now, there was no evidence that assigning officers to complete the training could influence outcomes; however, given the results of the current study, this practice may need to be reconsidered. In particular, jurisdictions planning to implement a CIT program may want to consider using an all-volunteer model. Short of this, they may want to establish criteria for assigning officers for training. Officers with little interest in working with those with mental illnesses or substance use disorders likely should not be considered for specialized CIT training. After-training measures may also be considered, such as providing post-training supervision on cases where a decision was made to arrest. While our results require replication, and there needs to be a greater understanding of how officers are assigned to participate in CIT training, assigning officers to training may need to be reconsidered if the goals of CIT are to be realized.
Several methodological limitations should be noted. First, there may have been an unwanted selection bias in officers' participation in the study. Second, while differences in attitudes or responses to vignettes are encouraging, the real question is whether volunteering or assigned officers behave differently in the field. Third, officers who were CIT-trained may have been more likely to complete encounter forms when the outcome was perceived as having had a desirable outcome. (Of note, however, CIT status—and volunteered versus assigned status among CIT officers—was intentionally not included on the encounter forms in Study 2; it was obtained as part of Study 1 data.) Similarly, because officers may have been selective in terms of which encounters were documented, rates of arrest and referral must be considered in the context of a sample and cannot be assumed to equate to arrest and referral rates for all encounters. Fourth, one cannot assume that the mere act of volunteering will produce better outcomes; research is now needed to better understand the factors affecting an officer's decision to volunteer. Fifth, although one of the core elements of CIT indicates that officers within a patrol division should voluntarily apply for CIT positions (which we attempted to study herein), it also states that each candidate would then go through a selection process based on the officer's application, recommendations, personal disciplinary file, and an interview. It is not known how often these aspects of selection are carried out by jurisdictions implementing CIT, nor is research available on these subsequent steps after the initial volunteering. Sixth, because we only had one self-report indicator variable (volunteered versus assigned), it is not known how some officers came to be assigned within the six departments; a stronger methodology would be to compare departments that mandate all officers to attend CIT training with those that follow the core element with high fidelity.
Conclusion
Debate exists within the expanding CIT community as to whether officers should only self-select (assuming that a beneficial self-selection bias exists) or if it is acceptable for them to be assigned to CIT training. The exact nature of the presumed self-selection bias has yet to be elucidated, though it is known that volunteering CIT officers are more likely to have been exposed to the mental health profession (e.g., through personal or family history) than non-CIT officers and assigned CIT officers. Our analysis suggests that volunteering CIT officers have—at a median of nearly two years after their training—better opinions and attitudes about mental illnesses (e.g., lesser personal responsibility attitudes and anger toward someone with suicidality, greater helping attitudes toward someone with psychosis). They also show greater self-efficacy, better de-escalation skills, and better referral decisions. Furthermore, when physical force was documented, volunteering CIT officers were more likely to refer to treatment services and less likely to make an arrest. These findings support the CIT core element that officers should volunteer/self-select into CIT training as they appear to have better post-training diversion outcomes than their assigned counterparts.
A number of law enforcement agencies across the country, often following tragic incidents and community pressure, have made the decision to assign all personnel to CIT training. Our findings suggest that this may dilute the value of implementing a CIT program and not produce the outcomes desired. Alternatively, agencies may want to consider assigning all personal to basic mental health response training, but reserving specialist CIT training for vetted volunteers.
Acknowledgments
Research reported in this publication was supported by National Institute of Mental Health grant R01 MH082813 (“Modeling Officer-Level Effects of Crisis Intervention Team (CIT) Training”) to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Institute of Mental Health.
References
- Bakeman R, Quera V. Sequential Analysis and Observational Methods for the Behavioral Sciences. Cambridge, United Kingdom: Cambridge University Press; 2011. [Google Scholar]
- Broussard B, Krishan S, Hankerson-Dyson D, Husbands L, Stewart-Hutto T, Compton MT. Development and initial reliability and validity of four self-report measures used in research on interactions between police officers and individuals with mental illnesses. Psychiatry Research. 2011;189:458–462. doi: 10.1016/j.psychres.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran S. In my opinion: Fighting stigma in law enforcement: The message has to come from the heart. ADS Center memorandum. 2004 Winter;2004 Retrieved February 22, 2007, from http://www.adscenter.org/memoranda/indexwinter2004.htm. [Google Scholar]
- Cochran S, Deane MW, Borum R. Improving police response to mentally ill people. Psychiatric Services. 2000;51:1315–1316. doi: 10.1176/appi.ps.51.10.1315. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. Journal of Abnormal and Social Psychology. 1962;64:349–360. doi: 10.1037/h0045526. [DOI] [PubMed] [Google Scholar]
- Compton MT, Bakeman R, Broussard B, Hankerson-Dyson D, Husbands L, Krishan S, Stewart-Hutto T, D'Orio BM, Oliva JR, Thompson NJ, Watson AC. The police-based Crisis Intervention Team (CIT) model: I. Effects on officers' knowledge, attitudes, and skills. Psychiatric Services. 2014a;65:517–522. doi: 10.1176/appi.ps.201300107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Bakeman R, Broussard B, Hankerson-Dyson D, Husbands L, Krishan S, Stewart-Hutto T, D'Orio BM, Oliva JR, Thompson NJ, Watson AC. The police-based Crisis Intervention Team (CIT) model: II. Effects on level of force and resolution, referral, and arrest. Psychiatric Services. 2014b;65:523–529. doi: 10.1176/appi.ps.201300108. [DOI] [PubMed] [Google Scholar]
- Compton MT, Broussard B, Hankerson-Dyson D, Krishan S, Stewart-Hutto T. Do empathy and psychological mindedness affect police officers' decision to enter Crisis Intervention Team training? Psychiatric Services. 2011;62:632–638. doi: 10.1176/appi.ps.62.6.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Hankerson-Dyson D, Broussard B. Development, item analysis, and initial reliability and validity of a multiple-choice knowledge of mental illnesses test for lay samples. Psychiatry Research. 2001;189:141–148. doi: 10.1016/j.psychres.2011.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior. 2003;44:162–179. [PubMed] [Google Scholar]
- Corrigan PW, River LP, Lundin RK, Wasowski KU, Campion J, Mathisen J, Goldstein H, Gagnon C, Bergman M, Kubiak MA. Predictors of participation in campaigns against mental illness stigma. Journal of Nervous and Mental Disease. 1999;187:378–380. doi: 10.1097/00005053-199906000-00008. [DOI] [PubMed] [Google Scholar]
- Dupont R, Cochran S, Pillsbury S. Crisis Intervention Team Core Elements. Memphis, Tenn: University of Memphis School of Urban Affairs and Public Policy, Department of Criminology and Criminal Justice, CIT Center, 2007; 2007. [Accessed February 8, 2017]. Available at: http://cit.memphis.edu/pdf/CoreElements.pdf. [Google Scholar]
- Krishan S, Bakeman R, Broussard B, Cristofaro SL, Hankerson-Dyson D, Husbands L, Watson AC, Compton MT. The influence of neighborhood characteristics on police officers' encounters with persons suspected to have a serious mental illness. International Journal of Law and Psychiatry. 2014;37:359–369. doi: 10.1016/j.ijlp.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy SR, Freitas AL, Salovey P. Construing action abstractly and blurring social distinctions: Implications for perceiving homogeneity among, but also empathizing with and helping, others. Journal of Personality and Social Psychology. 2002;83:1224–1238. doi: 10.1037//0022-3514.83.5.1224. [DOI] [PubMed] [Google Scholar]
- McAuley E, Duncan TE, Russell DW. Measuring causal attributions: the Revised Causal Dimension Scale (CDSII) Personality and Social Psychology Bulletin. 1992;18:566–573. [Google Scholar]
- Oliva JR, Compton MT. A statewide Crisis Intervention Team (CIT) initiative: evolution of the Georgia CIT program. Journal of the American Academy of Psychiatry and the Law. 2008;36:38–46. [PubMed] [Google Scholar]
- Russell D. The Causal Dimension Scale: A measure of how individuals perceive causes. Journal of Personality and Social Psychology. 1982;42:1137–1145. [Google Scholar]
- Russell DW, McAuley E, Tarico V. Measuring causal attributions for success and failure: a comparison of methodologies for assessing causal dimensions. Journal of Personality and Social Psychology. 1987;52:1248–1257. [Google Scholar]
- Struening EL, Cohen J. Factorial invariance and other psychometric characteristics of five opinions about mental illness factors. Educational and Psychological Measurement. 1963;23:289–298. [Google Scholar]
- Taylor SM, Dear MJ. Scaling community attitudes toward the mentally ill. Schizophrenia Bulletin. 1981;7:225–240. doi: 10.1093/schbul/7.2.225. [DOI] [PubMed] [Google Scholar]
- Taylor SM, Dear MJ, Hall GB. Attitudes toward the mentally ill and reactions to mental health facilities. Social Science and Medicine. 1979;13D:281–290. doi: 10.1016/0160-8002(79)90051-0. [DOI] [PubMed] [Google Scholar]
- Wilkinson L. Statistical methods in psychology journals: Guidelines and explanations. American Psychologist. 1999;54:594–604. [Google Scholar]


