Abstract
Objective
Racial variation in total knee replacement (TKR) utilization in the U.S. has been reported in administrative database studies. We investigated racial variation in TKR procedures in a diverse cohort with severe knee pain followed in an ongoing clinical trial.
Methods
The Vitamin D and Omega-3 Trial (VITAL) is a nationwide, randomized controlled trial of 25,874 adults, 20% of whom are Black. We identified a subgroup highly likely to have knee osteoarthritis (OA) based on severity of knee pain, physician-diagnosed knee OA, and inability to walk 2–3 blocks without pain. Participants completed a modified Western Ontario and McMaster’s Universities Osteoarthritis Index (WOMAC) at baseline and self-reported incident TKR annually in follow-up. Using Cox regression, we analyzed the association of Black vs. White race with TKR, adjusting for demographic and socioeconomic characteristics, comorbidities, WOMAC pain and function.
Results
Among 1070 participants who met inclusion criteria, Black participants reported worse baseline WOMAC pain (45 vs. 32, p<0.001) and worse function (45 vs. 32, p<0.001). During a median of 3.6 (IQR 3.2, 3.8) years of follow-up, TKRs were reported by 180 participants. Black participants were less likely to undergo TKR (11% vs. 19%). After adjustment, the hazard ratio for TKR for Black vs. White participants was 0.51 (0.32, 0.81). Lower use of TKR among Black participants was observed across all levels of income and education.
Conclusion
Despite worse baseline knee pain and function, Black participants had much lower adjusted risk of having TKR than White participants, demonstrating persistent racial disparity in TKR utilization.
Keywords: orthopedic, outcomes, race, disparity, trial
Introduction
Symptomatic knee osteoarthritis (OA) affects an estimated 7% of the U.S. adult population[1]. Total knee replacement (TKR), a treatment for end-stage OA, is one of the most common surgical procedures, with over 600,000 performed each year in the U.S.[2].
Prior studies have shown that Black and Hispanic individuals have lower rates of TKR than Whites[3–8]. The majority of these studies used Medicare claims data, with rates of TKR calculated using the general population as the denominator, rather than the population "at risk" – individuals with symptomatic knee OA[3, 5–9]. One study of a predominantly male cohort of “at risk” individuals with a diagnosis of OA within the Veteran’s Administration database reported that Black OA patients were significantly less likely than Whites to undergo TKR with an odds ratio (OR) of 0.72 (95% confidence interval (CI) 0.65–0.80)[4].
The aim of the current study was to investigate the Black-White racial disparity in TKR surgery rates and the effects of socioeconomic factors within a unique and diverse cohort of men and women with self-reported physician-diagnosed knee OA who are currently participating in a national randomized controlled trial. The trial allows for the use of an “at risk” population and access to a broad array of demographic, socioeconomic and health variables
Methods
Study Population
The VITamin D and OmegA-3 TriaL (VITAL) is an ongoing randomized double-blind, placebo-controlled trial of vitamin D and omega-3 fatty acid supplementation[10]. A total of 25,874 U.S. adults were enrolled from 2011 to 2014 from the community through brochures, targeted mailings, media reports, and advertisement. Men aged ≥50 and women aged ≥55 were eligible for enrollment. Black participants were oversampled (n=5,107, 20%)[10].
At baseline, we identified a "Knee Pain Subcohort" with frequent and chronic knee pain, highly likely to have knee OA based on an affirmative response to all of the following: a) self-reported knee pain symptoms in walking 2–3 blocks; b) knee pain > 1 day/week c) knee pain for ≥ 1 year; and d) a physician's diagnosis of knee OA. These questions were chosen based on previous validation studies of questions regarding knee pain symptoms and self-report of knee OA, which showed high sensitivity (90.1 %) and specificity (82.9%)[11]. Patients with previous bilateral TKR were excluded. For participants with prior unilateral TKR (n=155 among Whites and 57 among Blacks), the native contralateral knee was eligible for inclusion. (Individuals who reported race other than Black or White were excluded from these analyses because they had too few TKRs to permit meaningful analysis.) The VITAL trial is registered at clinicaltrials.gov (NCT01169259 for parent trial, and NCT01351805 for knee pain trial). The Partners’ Human Research Committee approved this study.
Data Elements at Baseline
Race was the exposure of interest and classified as Black or White based on participant self- report.
Participants’ demographic and socioeconomic characteristics, including age, sex, geographic location of residence, education level and income, were collected on baseline survey. The baseline surveys included the Western Ontario and McMaster’s Universities Osteoarthritis Index (WOMAC) Pain and Function[12]. WOMAC subscale scores were individually summed and scaled (0–100, 100 worst). A WOMAC end-user license was obtained for this study.
Data on the following medications were collected: 1) acetaminophen, 2) non-steroidal anti-inflammatory drugs (NSAID): naproxen, cox-2 inhibitors, indomethacin, etodolac, ibuprofen, nabumetone, diclofenac, salsalate, and piroxicam, 3) stronger pain medications: morphine, propoxyphene, oxycodone, hydrocodone, tramadol, amitriptyline, butalbital, and gabapentin. Potential co-morbid variables included body mass index (BMI in kg/m2, calculated from self-reported weight and height), and self-reported depression, smoking, hypertension, diabetes, and physical activity (MET-hours per week).
Total Knee Replacement Outcome
Self-reported incident TKR occurring during the study period was the outcome of interest. Self-reported incident TKR with laterality and operative date were collected on annual questionnaires to the Knee Pain Subcohort during the three-year follow-up period. Data on whether it was an initial or a secondary (not revision, but naïve contralateral knee) TKR were recorded. The first TKR reported during follow up was used for modeling analysis. Both initial and secondary TKRs were included in calculation of incidence rates for those patients with bilateral TKR during follow up period.
Validation Studies
Physician and hospital medical records from 200 men and 200 women in the Knee Pain Subcohort (26%, randomly selected) were requested for validation of cause of knee pain. Two physicians (LM and KC) manually reviewed the records for evidence of physician diagnosis of OA in progress notes, or radiographic evidence of OA (x-ray or magnetic resonance imaging with osteophytes, joint space narrowing, or OA listed in the impression). Records were recorded as either confirmed OA or not confirmed.
A second validation study was performed to ascertain the validity of participant self-report of TKR. Hospital medical records were requested from 156 participants (87%) who reported incident TKR occurring during the study period. These medical records were manually reviewed by two physicians (LM and KC) for confirmation of TKR, and date of procedure. Records were recorded as confirmed TKR, not confirmed TKR or insufficient medical records.
Statistical Analysis
Baseline characteristics were compared using means and percentages. Statistical significance was assessed with t-test for continuous variables and Chi-square or Fisher exact tests for binary variables. We investigated potential baseline variable differences between individuals who completed follow-up knee pain questionnaires and non-responders using chi-squared tests and t-tests.
We used log-rank test to assess for difference in cumulative incidence of TKR between Black and White participants. Cox proportional hazards regression models were used to calculate hazard ratios (HR) and 95% confidence intervals (CI) for TKR over time associated with Black vs. White race (reference). TKR-free survival was calculated from baseline to first TKR, death, drop-out or end of follow-up. We ran four models adjusting for potential covariates. The first model was adjusted for age and sex. The second was adjusted for age, sex, TKR at baseline, and WOMAC pain and function. The third additionally adjusted for education, income, and geographic region and the fourth model included all measured covariables: age, sex, baseline TKR, WOMAC pain and function, education, income, geographic region, medication use, BMI, self-reported depression, smoking, hypertension, diabetes, and physical activity. The proportional hazards assumption was tested using an interaction term for time and Black vs. White race.
Based on prior evidence, we were particularly interested in the influence of income, education and geographic region on the relationship between race (Black vs. White) and TKR utilization[3, 8, 13, 14]. In a secondary analysis, we used interaction terms to investigate the effect of income, education and geographic region on the race-TKR relationship. A p value of <0.05 was considered statistically significant. All analyses were performed using SAS 9.4 statistical software (SAS Institute Inc., Cary, NC).
Results
Baseline Characteristics
During the VITAL trial run-in period (baseline), 1430 (6%) trial participants were eligible for the knee pain cohort and were mailed supplementary baseline knee pain questionnaires. Of this group, 1106 (77%) participants who had returned the baseline knee pain questionnaire and completed all annual follow-up questionnaires to date; among them, 1070 self-identified as either Black (285 participants) or White (785 participants) were included. The median time of follow-up was 3.6 (IQR 3.2, 3.8) years.
Statistically significant baseline differences were identified between follow-up questionnaire responders and non-responders (those who did not respond to at least 1 follow up questionnaire). In comparing responders to all questionnaires (n=1106) to non-responders (n=324), males had an 81% response rate versus a 75% response rate for females. The Northeast and West had a higher response rate (82% and 80%) than the Midwest or South (76% and 74%). Participants with prior TKR had a higher response rate (84%) than those without prior TKR (76%). Non-responders had statistically significantly worse WOMAC pain (45 vs. 36) and function (45 vs. 36) scores than responders.
Characteristics from the severe knee pain cohort were similar to those reported from the entire VITAL cohort[10]. (Table 1) Black participants were significantly younger (63 vs. 68 years old) and more likely to be female (78% vs. 61%) and to reside in the Southern U.S. (51% vs. 32%) compared to White participants. Fewer Black participants reported education beyond high school (68% vs. 88%) or had income greater than $50,000/year (28% vs. 55%). Black participants were also more likely to be obese (BMI > 30 kg/m2, 68% vs. 50%), have diabetes (29% vs. 18%), or hypertension (83% vs. 65%). At baseline, Black participants reported higher WOMAC pain (45 vs. 32) and worse WOMAC function (45 vs. 32) scores than White participants. Black patients were also more likely to use stronger pain medications (43% vs. 24%). Black patients reported less physical activity (≥2hrs/week 70% vs. 76%). No significant differences were found between the two races for the prevalence of depression, smoking, or use of acetaminophen or NSAIDS. (Table 2)
Table 1.
Baseline Characteristics between entire VITAL cohort and Knee Pain Subcohort
| VITAL (n=25,874) |
'Knee Pain' Subcohort (n=1070) |
|
|---|---|---|
| Age, mean years, SD | 67.14 (7.1) | 66.9 (6.7) |
| Female, % | 13,081 (50.6) | 699 (65.3) |
| Race | ||
| -White, % | 18,047 (71.3) | 785 (73.4) |
| -Black, % | 5,107 (20.2) | 285 (26.6) |
| Geographic Location | ||
| -Northeast, % | 7,162 (27.7) | 230 (21.5) |
| -Midwest, % | 5,541 (21.4) | 264 (24.7) |
| -West, % | 5,928 (22.9) | 179 (16.7) |
| - South, % | 7,242 (28.0) | 397 (37.1) |
| > High School Education, % | 22,517 (87.2) | 878 (82.4) |
| Income >=$50,000/ year, % | 14,752 (63.4) | 507 (47.4) |
| Physical activity, ≥ 2 met hours/week, % | 21,895 (85.5) | 789 (74.7) |
| Smoking, % | 12,301 (48.3) | 495 (47.1) |
| Depression, % | 4,876 (20.7) | 289 (27.0) |
| Diabetes mellitus, % | 3,402 (13.2) | 221 (21.0) |
| Hypertension, % | 13,721 (53.6) | 741 (69.7) |
| Body Mass Index, ≥30 kg/m2 % | 7,205 (28.8) | 564 (54.8) |
SD; standard deviation
Table 2.
Baseline Characteristics of the Black and White Participants in the Knee Pain Trial
| Black (n=285) |
White (n=785) |
p value |
Black (n=285) |
White (n=785) |
p value |
|||
|---|---|---|---|---|---|---|---|---|
| Age, mean (SD) | 63.0(6.3) | 68.3(6.3) | <0.001 | Depression, (%) | 29.1 | 26.2 | 0.35 | |
| Female, (%) | 77.5 | 60.9 | <0.001 | Diabetes, (%) | 29.3 | 17.9 | <.001 | |
| Geographic Location, (%) | <0.001 | Hypertension, (%) | 83.0 | 64.9 | <.001 | |||
| Northeast | 20 | 22 | Smoking, (%) | 48.0 | 46.7 | 0.70 | ||
| Midwest | 22.1 | 25.6 | Acetaminophen, (%) | 51.4 | 50.4 | 0.78 | ||
| West | 7.4 | 20.1 | NSAID, (%) | 73.7 | 77.3 | 0.25 | ||
| South | 50.5 | 32.2 | Stronger pain medication, (%) | 43.3 | 24.0 | <0.001 | ||
| Education, (%) | <0.001 | Body Mass Index, (%) | <0.001 | |||||
| ≤High school | 32.0 | 12.3 | < 30 (kg/m2) | 31.6 | 50.1 | |||
| >High school | 68.0 | 87.7 | ≥30 (kg/m2) | 68.4 | 49.9 | |||
| Income, (%) | <0.001 | WOMAC pain, mean (SD) | 44.8(20.5) | 32.4(16.0) | <0.001 | |||
| <50,000 | 64.2 | 34.8 | 44.9(20.9) | 32.2(17.8) | <0.001 | |||
| ≥50,000 | 27.7 | 54.5 | WOMAC function, mean (SD) | |||||
| Baseline TKR | 57 (20.0) | 155 (19.8) | 0.93 | Physical Activity, ≥ 2 met hours/week, (%) | 69.8 | 76.4 | 0.03 | |
SD; standard deviation, NSAID; non steroidal anti-inflammatory drugs, WOMAC; Western Ontario and McMaster’s 0–100 (100 worse), Stronger pain medication; morphine, propoxyphene, codeine, oxycodone, hydrocodone, tramadol, butalbital/acetaminophen/caffeine, amitryptiline, gabapentin.
Knee Pain Cause Validation
Of the 400 randomly selected participants for validation of baseline OA, 226 (57%) participants provided medical records for review. Thirty-two (8%) participants did not consent to record review and in 103 (26%) either the participant or physician was unable to be reached. Twenty-four (6%) participants denied ever being evaluated or treated for knee OA. The remaining 15 (4%) could not provide records for miscellaneous reasons including destruction of older records. Of the 226 records received and reviewed, 207 (92% of reviewed; 52% of the random subsample) were confirmed to have OA based on physician's diagnosis and/or radiographic imaging.
Total Knee Replacement Validation
Of the 156 participants (87% of those self-reporting TKR) who were contacted to request medical record review for validation of TKR, 20 (13%) participants did not consent to medical records release, and two (0.01%) subsequently denied TKR. Of the 134 who provided consent and medical records, 134 participants (100%) were confirmed to have TKR or 86% of the entire requested cohort.
Total Knee Replacement Rates
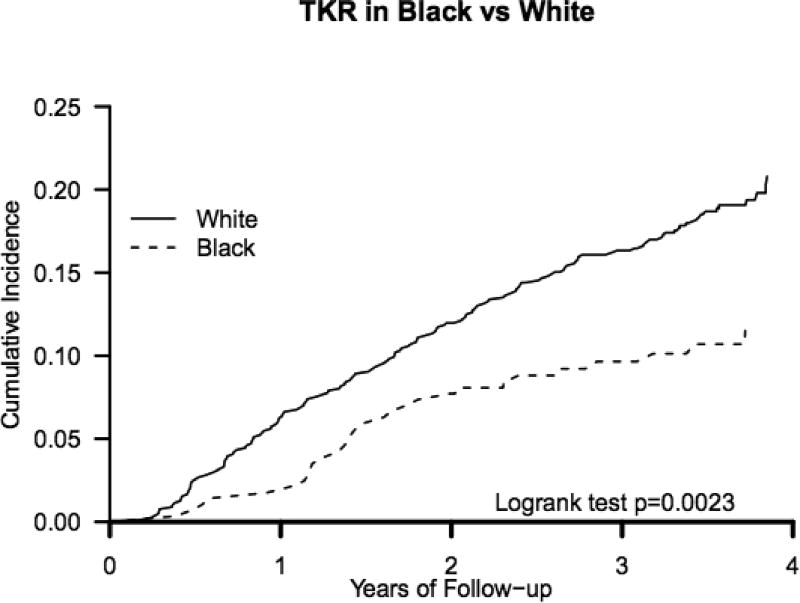
TKRs were self-reported in 180 individuals during the follow-up period. Thirty participants were Black participants and 150 were White. Proportionally fewer Blacks than Whites had a TKR (11% vs. 19%, p< 0.001). The cumulative incidence of TKR was statistically lower in Black participants than White participants (p=0.002). (Figure 1) Twenty-three initial TKRs were reported in Black participants and 114 in White participants. Secondary (contralateral naïve knee) TKR was reported by 9 Black participants and 56 White participants. The incidence rate (IR) per 100 patient-years for initial TKR was 2.5 (95% CI 1.5, 3.4) in Black participants and 4.3 (95% CI 3.5, 5.0) in White participants. The IR per 100 patient-years for secondary TKR (TKR on contralateral knee) was 0.9 (095% CI 0.3, 1.5) in Black participants and 2.0 (95% CI 1.5, 2.5) in White participants. The overall TKR IR per 100 patient-years was 3.2 (95% CI 2.1, 4.4) in Black participants and 5.8 (95% CI 4.9, 6.7) in White participants.
Figure 1.
Kaplan- Meier and Log-rank test for cumulative incidence of TKR in Black vs. White participants
Multivariable Modeling
In age- and sex-adjusted models, the HR for having a TKR for Black participants in comparison to White participants was 0.60 (95% CI 0.40, 0.90). In expanded models, further adjusting for TKR prior to baseline, WOMAC pain and function scores, the HR of TKR for Black participants decreased to 0.49 (95% CI 0.32, 0.75). The addition of income, education and geographic location to the model yielded a HR of TKR in Black compared to White participants of 0.53 (95% CI 0.34, 0.83). In our final model, including all baseline covariates, the HR of TKR for Black patients compared to White patients was 0.51 (95% CI 0.32, 0.81). (Table 3). The proportional hazards assumption was valid (p=0.62).
Table 3.
Adjusted Risk of Undergoing Total Knee Replacement among Black versus White Participants, Cox Regression Analyses
| Black Participants | White Participants | |
|---|---|---|
| TKR, n (%) | 30 (10.5) | 150 (19.1) |
| Model 1 Hazard ratio (95% CI) | 0.60 (0.40, 0.90) | Ref. |
| Model 2 Hazard ratio (95% CI) | 0.49 (0.32, 0.75) | Ref. |
| Model 3 Hazard ratio (95% CI) | 0.53 (0.34, 0.83) | Ref. |
| Model 4 Hazard ratio (95% CI) | 0.51 (0.32, 0.81) | Ref. |
CI; confidence interval
Model 1: age, sex
Model 2: age, sex, baseline TKR, WOMAC pain and function (25 participants missing)
Model 3: age, sex, baseline TKR, WOMAC pain and function, education, income, geographic region (30 participants missing)
Model 4: age, sex, baseline TKR, WOMAC pain and function, education, income, geographic region, body mass index, depression, diabetes, hypertension, smoking, Tylenol, non steroidal anti-inflammatory, stronger pain medication, physical activity (missing for 112 participants)
In tests of interactions utilizing cross-classified variables in the full multivariable analyses, we found no statistically significant multiplicative interactions between race and income (Black and income <$50,000 per year= reference, p= 0.12), education (Black and < or = high school education= reference group, p=0.57), or U.S. region (Black and South= reference, p=0.59).
Discussion
In a subcohort of individuals with severe and frequent knee pain and likely knee OA, we found that Black participants had approximately 50% lower hazards of having a TKR compared to White participants. This was true despite Black participants reporting more knee pain and worse function at baseline. In fact, the HR of TKR among Blacks compared to Whites further diminished after adjusting for differences in baseline WOMAC pain and function. We did not find that socioeconomic variables including geographic location, education level and income, modified the TKR- race relationship. Prior studies using U.S. Medicare data (1991–2008 and 2000–2006) demonstrate TKR utilization was approximately 40% lower in Black patients. The current study demonstrates a persistence of this disparity of a similar magnitude[5, 13].
The current data indicating lower incidence rates and adjusted odds of undergoing TKR among Black patients are in agreement with prior literature based on a “general population” denominator[3, 5–8]. This issue of a “denominator bias” has been raised in the literature, as using the “general population” instead of a population “at risk” for the procedure of interest may underestimate procedure rates[9]. Jones et al used ICD-9 codes to identify “at risk” patients with OA, however, only 2% of the Black and 3% of the White patients were female, and patients’ with OA at any site were included instead of limiting analysis to those with likely knee OA as was done in our study[4]. While age, sex and comorbidities were included as covariates, the contribution of socioeconomic factors was not addressed. Our study augments this prior research by using a nationwide sample with likely OA including women, as the “at risk denominator” and further investigated the potential role of socioeconomic factors. Based on our validation subcohort, we were able to validate the vast majority of likely OA as confirmed OA (92%).
In the current analysis, the wide racial disparity in TKR rates was not significantly modified by socioeconomic factors, though the interaction term for income and race approached statistical significance. The high percentage of trial participants’ with high school education may have limited our ability to discern effect modification. A 2003 study of Medicare enrollees found that the disparity was only slightly diminished when Black males with incomes above the median income for Black patients were compared to Black males with income below the median[3]. A subsequent study in the Medicare population found a statically significant but weak association of income and TKR (OR 0.98, CI 0.96–1.00)[8]. Thus, while socioeconomic factors should not be overlooked in the discussion of racial disparity in TKR, these factors do not completely explain the observed disparities, based on this and other studies.
Several explanations for this racial disparity have been investigated including both intrinsic and extrinsic factors. Racial differences in disease prevalence have been considered, however, the prevalence of radiographic knee OA was 16% higher among Black than White patients in the NHANES III cohort[15]. This finding was also described in the Johnston County cohort[15] and in our current study, WOMAC knee pain and function scores were worse among Blacks than Whites. Regional variation in TKR surgery has been found to influence TKR variability. One prior study calculated that 35% of the difference in arthroplasty rates among Black vs. White women was attributable to Black women being more likely to live in regions with low arthroplasty rates[3]. Existing demographic data suggest the prevalence of TKR is higher in some of the U.S. Midwest and Western regions, where fewer of our Black participants reside, and lower in certain southern regions, where the majority of our Black participants lived[16, 17]. However, adjustment for socio-demographic features including geographic region did not mitigate the disparity in this cohort, nor did we find a significant interaction between geographic region and race in the risk of TKR, suggesting that in this large nationwide cohort geographic region was not a significant determinant of TKR rate between the races. In our study Black participants were significantly younger, and were more likely to report income <$50,000. It may be that Black participants were more affected by the time needed away from work to undergo surgery and recovery. The lack of current employment data in this dataset is a limitation.
Physician bias and patient willingness to undergo TKR have been considered as contributors to TKR disparity. A 2009 study of veterans showed that Black patients were as clinically eligible and appropriate for consideration of joint replacement as White patients based on age, prior treatment, pain severity, functional limitations and surgical risk[18]. A recent publication exploring potential physician bias, found that that U.S. orthopedic surgeons were equally as likely to recommend TKR to Black and White patients in standardized scenarios (age 68 with similar presentation, exam, socio-economic status and one comorbidity). These data raised the question of patient preferences concerning surgery[19]. Several recent studies have focused on the preference or willingness of Black patients to undergo joint replacements, finding that Black patients are less willing to consider or undergo joint replacement in comparison to their White counterparts[20–23].
This study does have limitations. Patient willingness and preference to undergo TKR may contribute to the different rates of TKR among the races[22]. However, our surveys did not assess these patient factors. We were also unable to assess whether there were racial differences in referral to orthopedic surgeons or whether patients had been offered TKR. Black patients were more likely to have co-morbid health issues such as hypertension and diabetes. However, we were unable to assess all potential contraindications to surgery or appropriate surgical candidacy that could in part explain the disparity. We did not have data on knee osteoarthritis radiographic severity between the races, although we were able to assess extent of symptoms with WOMAC scores. We are unable to further examine provider and system-level etiologies for the disparity in our current dataset. By nature of enrolling in a clinical trial, members of this cohort may be more engaged in healthcare. However, the study sample is representative and generalizable to older adults in the U.S. population. We relied on patient reported data, but of the charts received in the validation subset we were able to validate 100% of the TKRs and 92% of the OA cases.
Evidence of disparity in risks of TKR surgeries exists between Black and White participants using an “at risk” denominator in this ongoing diverse, nationwide trial. While racial disparity in TKR has been recognized in the U.S. for several years, our data demonstrate that we have not succeeded in reducing the gap. We did not observe significant modification from socioeconomic or demographic factors, suggesting that this issue is likely multifactorial based on patient, provider and system-wide features in our healthcare system. Further research to understand the drivers, and to identify new broad strategies encompassing patient, provider and health care access are needed to address this ongoing divide.
Significance and Innovations.
We found a striking racial disparity in total knee replacement utilization between Black and White participants in a subcohort of participants with severe knee pain from an ongoing nationwide clinical trial.
We employed an “at risk” denominator population, consisting of individuals with severe knee pain and likely knee osteoarthritis, rather than otherwise healthy individuals.
This disparity was not affected by socioeconomic factors such as education level, income and region.
Acknowledgments
This project was funded by NIH R01 CA138962 and R01 AR057327. Dr. Costenbader receives support from NIH K24 AR066109 and Dr. MacFarlane from NIH T32 055885.
Footnotes
None of the authors have conflicts of interest to declare
References
- 1.Deshpande BR, Katz JN, Solomon DH, et al. The number of persons with symptomatic knee osteoarthritis in the United States: Impact of race/ethnicity, age, sex, and obesity. Arthritis Care Res (Hoboken) 2016 doi: 10.1002/acr.22897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Services USDoHH. Healthcare Cost and Utlization Project (HCUP) Vol. 2016. Rockville, MD: 2016. [Google Scholar]
- 3.Skinner J, Weinstein JN, Sporer SM, et al. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 4.Jones A, Kwoh CK, Kelley ME, et al. Racial disparity in knee arthroplasty utilization in the veterans health administration. Arthritis Rheum. 2005;53:979–981. doi: 10.1002/art.21596. [DOI] [PubMed] [Google Scholar]
- 5.Singh JA, Lu X, Rosenthal GE, et al. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73:2107–2115. doi: 10.1136/annrheumdis-2013-203494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jha AK, Fisher ES, Li Z, et al. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 7.Wilson MG, May DS, Kelly JJ. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethn Dis. 1994;4:57–67. [PubMed] [Google Scholar]
- 8.Skinner J, Zhou W, Weinstein J. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159–2166. doi: 10.2106/JBJS.E.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katz JN, Losina E. Measures matter: racial disparities in the provision of total knee replacement. Arthritis Rheum. 2005;53:805–807. doi: 10.1002/art.21600. [DOI] [PubMed] [Google Scholar]
- 10.Bassuk SS, Manson JE, Lee IM, et al. Baseline characteristics of participants in the VITamin D and OmegA-3 TriaL (VITAL) Contemp Clin Trials. 2016;47:235–243. doi: 10.1016/j.cct.2015.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morvan J, Roux CH, Fautrel B, et al. A case-control study to assess sensitivity and specificity of a questionnaire for the detection of hip and knee osteoarthritis. Arthritis Rheum. 2009;61:92–99. doi: 10.1002/art.24079. [DOI] [PubMed] [Google Scholar]
- 12.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 13.Racial disparities in total knee replacement among Medicare enrollees--United States, 2000–2006. MMWR Morb Mortal Wkly Rep. 2009;58:133–138. [PubMed] [Google Scholar]
- 14.Dunlop DD, Manheim LM, Song J, et al. Age and racial/ethnic disparities in arthritis-related hip and knee surgeries. Med Care. 2008;46:200–208. doi: 10.1097/MLR.0b013e31815cecd8. [DOI] [PubMed] [Google Scholar]
- 15.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.A Dartmouth Atlas Surgery Report: Trends and Regional Variation in Hip, Knee, and Shoulder Replacement. [cited 2017 June 13];2010 Available from http://www.dartmouthatlas.org/ [PubMed]
- 18.Ang DC, Tahir N, Hanif H, et al. African Americans and Whites are equally appropriate to be considered for total joint arthroplasty. J Rheumatol. 2009;36:1971–1976. doi: 10.3899/jrheum.081214. [DOI] [PubMed] [Google Scholar]
- 19.Dy CJ, Lyman S, Boutin-Foster C, et al. Do patient race and sex change surgeon recommendations for TKA? Clin Orthop Relat Res. 2015;473:410–417. doi: 10.1007/s11999-014-4003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim SA, Siminoff LA, Burant CJ, et al. Differences in expectations of outcome mediate African American/white patient differences in "willingness" to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 21.Vina ER, Cloonan YK, Ibrahim SA, et al. Race, sex, and total knee replacement consideration: role of social support. Arthritis Care Res (Hoboken) 2013;65:1103–1111. doi: 10.1002/acr.21925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen KD, Golightly YM, Callahan LF, et al. Race and sex differences in willingness to undergo total joint replacement: the Johnston County Osteoarthritis Project. Arthritis Care Res (Hoboken) 2014;66:1193–1202. doi: 10.1002/acr.22295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hausmann LR, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25:982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]