Abstract
Objective
To describe fetal and neonatal mortality due to congenital anomalies in Colombia.
Methods
We analyzed all fetal and neonatal deaths due to a congenital anomaly registered with the Colombian vital statistics system during 1999–2008.
Results
The registry included 213,293 fetal deaths and 7,216,727 live births. Of the live births, 77,738 (1.08%) resulted in neonatal deaths. Congenital anomalies were responsible for 7321 fetal deaths (3.4% of all fetal deaths) and 15,040 neonatal deaths (19.3% of all neonatal deaths). The fetal mortality rate due to congenital anomalies was 9.9 per 10,000 live births and fetal deaths; the neonatal mortality rate due to congenital anomalies was 20.8 per 10,000 live births. Mortality rates due to congenital anomalies remained relatively stable during the study period. The most frequent fatal congenital anomalies were congenital heart defects (32.0%), central nervous system anomalies (15.8%), and chromosomal anomalies (8.0%). Risk factors for fetal and neonatal death included: male or undetermined sex, living in villages or rural areas, mother's age >35 years, low and very low birthweight, and <28 weeks gestation at birth.
Conclusions
Congenital anomalies are an important cause of fetal and neonatal deaths in Colombia, but many of the anomalies may be preventable or treatable.
Keywords: Fetal mortality, infant mortality, neonatal mortality, congenital anomalies, vital statistics, Colombia
Introduction
Congenital anomalies, also called birth defects or congenital disorders, are conditions leading to high infant mortality and disability [1]. It is estimated that worldwide each year 330,000 newborns die during the first 28 days of life due to congenital anomalies [1]. Whereas neonatal mortality is decreasing as labor care and the prevention of infectious diseases has improved, the proportion of deaths due to premature birth or birth defects has been increasing [2]. As a result, congenital anomalies must be addressed in order to finish the work of the World Health Organization's 4th Millennium Development Goal related to reducing child mortality and the related Sustainable Development Goals [3].
The Pan American Health Organization (PAHO) has reported that in Colombia approximately 20% of all deaths in children younger than five years of age are related to congenital anomalies [4]. Furthermore, among children under one year of age, congenital anomalies are the second leading cause of death in Colombia [4]. This and other reports (e.g. [5,6]), however, have important limitations, which may include little information on time trends, geographic distributions, or major risk determinants of congenital anomaly-related mortality. Furthermore, data are typically only available on under-five or infant mortality, rather than neonatal, or perinatal mortality (i.e. including fetal deaths) [4].
To address these research gaps in Colombia, we carried out a study of death certificates to describe trends and characteristics of fetal and neonatal mortality due to congenital anomalies during 1999–2008 according to type of congenital anomaly, as well as geographical, socioeconomic, and obstetric determinants.
Methods
Data source
We reviewed all fetal and neonatal deaths registered at the Colombian vital statistics system of the National Administrative Department of Statistics (known as DANE) during the period 1999–2008. Fetal death was defined as death prior to birth of a fetus weighing at least 500 grams (g). Neonatal death was defined as death of a liveborn baby occurring within 28 days after birth. Deaths due to congenital anomalies were classified according to the tenth revision of the International Classification of Diseases (ICD-10), chapter XVII Q000-Q999 for congenital malformations, deformations, and chromosomal abnormalities. During these years some changes were made in how the DANE vital statistics system collected and categorized certain variables; therefore, we standardized categories for maternal age, gestational age, and birthweight in order to ensure comparability over time. DANE is responsible for cleaning the database to avoid duplicate information.
Statistical analysis
The analysis was done using Microsoft Excel 2007 (Microsoft Corporation, Redmond, WA), SPSS 18® (SPSS, Chicago, IL) and Epi-Info© version 3.5.3 (CDC, Atlanta, GA). Descriptive statistics (numbers, percentages, and rates) are presented. We defined the fetal mortality rate as number of fetal deaths per 10,000 live births and fetal deaths, and we defined the neonatal mortality rate as the number of neonatal deaths per 10,000 live births. We calculated these rates for both overall fetal and neonatal mortality, and also for fetal and neonatal mortality due to congenital anomalies. We calculated these mortality rates by year and computed the proportions of fetal and neonatal deaths due to congenital anomalies.
In addition, using information available on the death certificate, we calculated descriptive statistics according to the following characteristics: type of congenital anomaly, type of residence (urban, villages, or rural), maternal age, infant sex, birth weight, gestational week, maternal education level, number of living children, health insurance, and civil marriage status. However, we were unable to calculate mortality rates for the last four variables because the live births database did not record information on them. For selected mortality rates, we compared variable characteristics using the Mantel–Haenszel chi square test.
Ethical considerations
This study followed the good clinical practice guidelines and the guidelines of the Helsinki Declaration. The publically available vital statistics database did not contain any identifiers, there was no contact with any of the affected families, and no samples were taken. Thus, according to national regulations (resolution 008430 of 1993), our study was considered to be without risks for the participants and exempt from human subjects review.
Results
During 1999–2008 a total of 213,293 fetal deaths and 7,216,727 live births were registered (Table 1). Of the live births, 77,738 (1.08%) resulted in neonatal deaths. Congenital anomalies were responsible for 7321 fetal deaths (3.4% of all fetal deaths) and 15,040 neonatal deaths (19.3% of all neonatal deaths) (Table 1). The fetal mortality rate due to congenital anomalies was 9.9 per 10,000 live births and fetal deaths, while the neonatal mortality rate due to congenital anomalies was 20.8 per 10,000 live births (Table 1).
Table 1.
Fetal and neonatal deaths due to congenital anomalies in Colombia, 1999–2008.
| Year | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of live births | 746,194 | 752,834 | 724,319 | 700,455 | 710,702 | 723,099 | 719,968 | 714,450 | 709,253 | 715,453 | 7,216,727 |
| Number of fetal deaths | 16,583 | 14,218 | 18,380 | 14,727 | 17,874 | 18,709 | 25,354 | 26,482 | 29,384 | 31,582 | 213,293 |
| Fetal mortality rate (per 10,000 live births and fetal deaths) | 217.4 | 185.4 | 247.5 | 205.9 | 245.3 | 252.2 | 340.2 | 357.4 | 397.8 | 422.8 | 287.1 |
| Number of fetal deaths due to congenital anomalies | 666 | 741 | 697 | 687 | 709 | 500 | 813 | 792 | 1160 | 556 | 7,321 |
| Fetal mortality rate due to congenital anomalies (per 10,000 live births and fetal deaths) | 8.7 | 9.7 | 9.4 | 9.6 | 9.7 | 6.7 | 10.9 | 10.7 | 15.7 | 7.4 | 9.9 |
| Proportion of fetal deaths due to congenital anomalies (%) | 4.0% | 5.2% | 3.8% | 4.7% | 4.0% | 2.7% | 3.2% | 3.0% | 3.9% | 1.8% | 3.4% |
| Number of neonatal deaths | 9336 | 9730 | 8812 | 7838 | 7552 | 7288 | 7129 | 6693 | 6782 | 6578 | 77,738 |
| Neonatal mortality rate (per 10,000 live births) | 125.1 | 129.2 | 121.7 | 111.9 | 106.3 | 100.8 | 99.0 | 93.7 | 95.6 | 91.9 | 107.7 |
| Number of neonatal deaths due to congenital anomalies | 1357 | 1592 | 1539 | 1481 | 1521 | 1555 | 1450 | 1506 | 1540 | 1499 | 15,040 |
| Neonatal mortality rate due to congenital anomalies (per 10,000 live births) | 18.2 | 21.1 | 21.2 | 21.1 | 21.4 | 21.5 | 20.1 | 21.1 | 21.7 | 21.0 | 20.8 |
| Proportion of neonatal deaths due to congenital anomalies (%) | 14.5% | 16.4% | 17.5% | 18.9% | 20.1% | 21.3% | 20.3% | 22.5% | 22.7% | 22.8% | 19.3% |
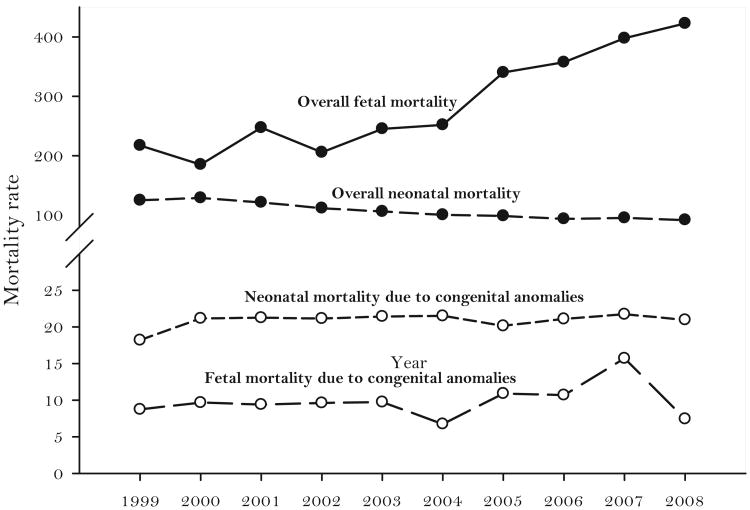
Over time, the fetal mortality rate due to congenital anomalies did not exhibit a clear trend (Figure 1), although rates were lower than the mean in 2004 and 2008 and higher than the mean in 2007. This lack of clear trend was in contrast to overall fetal mortality rates, which increased substantially from 217.4 per 10,000 live births and fetal deaths in 1999–422.8 per 10,000 live births and fetal deaths in 2008. The combination of stable fetal deaths due to congenital anomalies and rising numbers of overall fetal deaths resulted in a decrease in the percentage of fetal deaths due to congenital anomalies from 4.0% in 1999 to 1.8% in 2008.
Figure 1.
Fetal and neonatal mortality trends by year of death, Colombia, 1999–2008.
Similarly, the neonatal mortality rate due to congenital anomalies did not exhibit a clear trend and in fact appeared nearly constant during 1999–2008, with the exception of 1999, where the rate was about 10% lower than the mean (Figure 1). This lack of trend was also in contrast to the overall neonatal mortality rates, which decreased from 125.1 per 10,000 live births in 1999 to 91.9 per 10,000 live births in 2008 (Table 1). The combination of stable neonatal deaths due to congenital anomalies and decreasing numbers of fetal deaths resulted in an increase in the percentage of neonatal deaths due to congenital anomalies from 14.5% in 1999 to 22.8% in 2008.
The distribution of mortality due to congenital anomalies within each year was rather homogeneous, although a higher rate was usually observed during the months of September and October (data not shown).
Among combined fetal and neonatal deaths due to congenital anomalies, the most frequent category (Table 2) was congenital heart defects (32.0%), followed by central nervous system anomalies (15.8%) and chromosomal anomalies (8.0%). However, for neonatal deaths only, a much larger proportion was due to congenital heart defects (45.0%) than to central nervous system anomalies (14.1%) or chromosomal anomalies (2.2%). In contrast, for fetal deaths only, a larger proportion was due to central nervous system anomalies (18.9%) and chromosomal anomalies (20.0%) than to congenital heart defects (6.1%). The collection of “other” congenital anomalies also contributed to a substantial proportion of fetal deaths (46.6%) and neonatal deaths (16.7%) due to congenital anomalies.
Table 2.
Distribution of fetal and neonatal mortality by type of congenital anomaly, Colombia, 1999–2008.
| Congenital anomaly | Fetal deaths | % of all fetal deaths | Fetal mortality rate | Neonatal deaths | % of all neonatal deaths | Neonatal mortality rate | Total deaths | % of all fetal and neonatal deaths |
|---|---|---|---|---|---|---|---|---|
| Congenital heart defects | 448 | 6.1 | 0.6 | 6773 | 45.0 | 9.4 | 7221 | 32.0 |
| Central nervous system | 1388 | 18.9 | 1.9 | 2128 | 14.1 | 2.9 | 3516 | 15.8 |
| Chromosomal | 1470 | 20.0 | 2.0 | 329 | 2.2 | 0.5 | 1799 | 8.0 |
| Musculoskeletal system | 173 | 2.4 | 0.2 | 1073 | 7.1 | 1.5 | 1246 | 5.6 |
| Digestive system | 67 | 0.9 | 0.1 | 1001 | 6.7 | 1.4 | 1068 | 4.8 |
| Respiratory system | 196 | 2.7 | 0.3 | 697 | 4.6 | 1.0 | 893 | 4.0 |
| Urinary system | 151 | 2.1 | 0.2 | 498 | 3.3 | 0.7 | 649 | 3.0 |
| Orofacial clefts | 9 | 0.1 | 0.01 | 24 | 0.2 | 0.03 | 33 | 0.15 |
| Visual, auditory, face or neck | 3 | 0.04 | 0.004 | 2 | 0.01 | 0.003 | 5 | 0.02 |
| Genital organs | 1 | 0.01 | 0.001 | 1 | 0.01 | 0.001 | 2 | 0.008 |
| Other congenital anomalies | 3415 | 46.6 | 4.6 | 2514 | 16.7 | 3.5 | 5929 | 26.5 |
| Total | 7321 | 100 | 9.9 | 15,040 | 100 | 20.8 | 22,361 | 100 |
The most frequent congenital heart defect reported among fetal and neonatal deaths was unspecified congenital heart disease (65%) followed by hypoplastic left heart syndrome (3.2%), ventricular septal defect (2.8%), and aortic coarctation (2.4%) (Table 2). Neural tube defects (anencephaly, spina bifida and encephalo-cele) accounted for 50% of the central nervous system anomalies among fetal and neonatal deaths (including 39% due to anencephaly alone), followed by hydrocephalus (24%) and brain hypoplasia (6%). The majority of the chromosomal abnormalities among fetal and neonatal deaths were “unspecified” chromosomal abnormalities (77%), followed by Edwards syndrome (9%), Patau syndrome (6%), and Down syndrome (6%).
For variables whose rates could be computed, the characteristics with higher fetal and neonatal mortality rates due to congenital anomalies included: male or undetermined sex (versus female sex, p<.01), living in villages or rural areas (versus urban area, p<.001), mother's age >35 years (versus ≤35 years, p<.001), low and very low birth-weight (versus normal birth-weight, p<.001), and ≤28 weeks gestation at birth (versus >28 weeks, p<.001) (Table 3). Fetal and neonatal mortality rates due to congenital anomalies were also elevated when there was missing information on these characteristics (Table 3).
Table 3.
Fetal and neonatal deaths due to congenital anomalies by maternal sociodemographic and obstetric characteristics, Colombia, 1999–2008.
| Characteristics | Category | Live births (n = 7,216,727) | Fetal deaths (n = 213,293) | Fetal deaths due to congenital anomalies n = 7321) | % of fetal deaths due to congenital anomalies | Fetal mortality rate due to congenital anomalies (per 10,000 live births and fetal deaths) | Neonatal deaths due to congenital anomalies n = 15,040) | % of neonatal deaths due to congenital anomalies | Neonatal mortality rate due to congenital anomalies (per 10,000 live births) |
|---|---|---|---|---|---|---|---|---|---|
| Variables with denominators to compute rates by characteristic | |||||||||
| Sex | Female | 3,508,344 | 37,624 | 2290 | 31.3 | 6.5 | 6595 | 43.8 | 18.8 |
| Male | 3,708,383 | 50,672 | 2623 | 35.8 | 7.0 | 8426 | 56.0 | 22.7 | |
| Undetermined | 0 | 124,997 | 2408 | 32.9 | 192.6 | 19 | 0.1 | Undefined | |
| Residence | Urban | 6,809,539 | 197,076 | 5095 | 69.6 | 7.3 | 11,506 | 76.5 | 16.9 |
| Villages | 166,190 | 3169 | 586 | 8.0 | 34.6 | 902 | 6.0 | 54.3 | |
| Rural | 206,682 | 8943 | 1201 | 16.4 | 55.7 | 1865 | 12.4 | 90.2 | |
| Missing information | 34,316 | 4105 | 439 | 6.0 | 114.3 | 767 | 5.1 | 223.5 | |
| Mother's age | Less than 19 years | 1,620,437 | 40,956 | 1398 | 19.1 | 8.4 | 2798 | 18.6 | 17.3 |
| 20–34 years | 4,787,540 | 122,632 | 3968 | 54.2 | 8.1 | 8287 | 55.1 | 17.3 | |
| More than 35 years | 746,361 | 32,578 | 1223 | 16.7 | 15.7 | 1955 | 13.0 | 26.2 | |
| Missing information | 62,389 | 17,127 | 732 | 10.0 | 92.1 | 2000 | 13.3 | 320.6 | |
| Birth weight | <1000g | 21,137 | 45,369 | 1369 | 18.7 | 205.8 | 948 | 6.3 | 448.5 |
| 1000–1499 g | 46,463 | 8538 | 835 | 11.4 | 151.8 | 1384 | 9.2 | 297.9 | |
| 1500–2499 g | 502,061 | 16,994 | 1530 | 20.9 | 29.5 | 4677 | 31.1 | 93.2 | |
| 2500–3999 g | 6,104,671 | 19,192 | 988 | 13.5 | 1.6 | 6572 | 43.7 | 10.8 | |
| ≥4000 g | 329,750 | 1348 | 95 | 1.3 | 2.9 | 376 | 2.5 | 11.4 | |
| Missing information | 212,645 | 121,852 | 2504 | 34.2 | 74.9 | 1083 | 7.2 | 50.9 | |
| Gestational week | Less than 22 | 486 | 100,585 | 1728 | 23.6 | 171.0 | 75 | 0.5 | 1543.2 |
| Between 22 and 27 | 22,359 | 21,706 | 1112 | 15.2 | 252.4 | 857 | 5.6 | 383.3 | |
| More than 28 | 6,921,303 | 65,790 | 3639 | 49.7 | 5.2 | 12,920 | 85.9 | 18.7 | |
| Missing information | 272,579 | 11,142 | 842 | 11.5 | 29.7 | 1188 | 7.9 | 43.6 | |
| Variables without denominators to compute rates by characteristic | |||||||||
| Mother's educational level | Without | NA | NA | 220 | 3.0 | NA | 391 | 2.6 | NA |
| Primary | NA | NA | 2167 | 29.6 | NA | 3670 | 24.4 | NA | |
| Secondary | NA | NA | 3111 | 42.5 | NA | 5309 | 35.3 | NA | |
| Superior | NA | NA | 820 | 11.2 | NA | 1639 | 10.9 | NA | |
| Missing information | NA | NA | 1003 | 13.7 | NA | 4031 | 26.8 | NA | |
| Number of children alive | 1 | NA | NA | 1823 | 24.9 | NA | 5204 | 34.7 | NA |
| 2–4 | NA | NA | 2181 | 29.7 | NA | 7219 | 48.0 | NA | |
| More than 5 | NA | NA | 2255 | 30.8 | NA | 1324 | 8.8 | NA | |
| Missing information | NA | NA | 1062 | 14.5 | NA | 1293 | 8.6 | NA | |
| Health insurance | Private | NA | NA | 2123 | 29.0 | NA | 4828 | 32.1 | NA |
| Public | NA | NA | 2540 | 34.7 | NA | 5008 | 33.3 | NA | |
| None | NA | NA | 1567 | 21.4 | NA | 3008 | 20.0 | NA | |
| Other | NA | NA | 447 | 6.1 | NA | 1113 | 7.4 | NA | |
| Missing information | NA | NA | 644 | 8.8 | NA | 1083 | 7.2 | NA | |
| Civil status | Single | NA | NA | 1464 | 20.0 | NA | 2015 | 13.4 | NA |
| Previously in a relationship/separated | NA | NA | 81 | 1.1 | NA | 165 | 1.1 | NA | |
| In a relationship | NA | NA | 5190 | 70.9 | NA | 10,017 | 66.5 | NA | |
| Missing information | NA | NA | 586 | 8.0 | NA | 2843 | 18.9 | NA | |
Discussion
We found that congenital anomalies are important contributors to fetal and neonatal mortality in Colombia. Over a 10-year period, congenital anomalies caused more than 22,000 fetal and neonatal deaths, including over 3% of fetal deaths and nearly 20% of neonatal deaths. It is difficult to compare these proportions with other countries in the region because limited data have been published on fetal and neonatal mortality due to congenital anomalies. We were only able to identify one comparable study in the region, where it was reported that in Costa Rica congenital anomalies contributed to 4% of fetal deaths [7].
Although we did not observe clear time trends in neonatal mortality due to congenital anomalies, given the inherent limitations of death certificate data it is still possible that some modest underlying trends were present. As overall neonatal mortality decreased, neonatal mortality due to congenital anomalies remained relatively stable, meaning that congenital anomalies are contributing to higher proportions of neonatal mortality each year. Similar trends have been observed worldwide [2]. Thus, to reduce overall neonatal mortality, new approaches may be needed in Colombia for decreasing the occurrence of congenital anomalies and the occurrence of death among neonates with congenital anomalies.
Fetal mortality rates due to congenital anomalies were more volatile over time. For three years (2004, 2007, and 2008), rates were substantially different (−31.6%, 60.2%, and −24.4%, respectively) from the 10-year average (9.9%). All-cause fetal mortality was also more volatile over time, but experienced an overall increase that did not clearly correspond to increases and decreases in fetal mortality due to congenital anomalies. The volatility is likely due in part to smaller denominators for fetal deaths compared to neonatal deaths, leading to uncertainty about whether there were any long-term trends in fetal mortality due to congenital anomalies. It is possible that fetal mortality is rising because of better ascertainment, rather than because of increased incidence, but whatever the explanation, the data do not suggest that congenital anomalies are contributing substantially to that rise.
Although many types of congenital anomalies resulted in fetal and neonatal deaths, a large proportion of deaths were attributable to congenital anomalies that are potentially treatable or preventable. A recent study conducted in Colombia revealed that adequate treatment could improve outcomes in more than 80% of newborns with non-lethal anomalies [6]. In our study, nearly half (45.0%) of neonatal deaths were caused by congenital heart defects, many of which might be treatable [8].
The next biggest specific contributor to fetal and neonatal deaths was central nervous system anomalies, of which half were neural tube defects. Many neural tube defects can be prevented if women consume adequate folic acid prior to and during the peri-conceptional period, either through vitamin supplements or fortified food [9,10]. In fact, neural tube defects occurrence can be reduced to less than seven cases per 10,000 live births if women have adequate blood folate levels [11]. Several studies have shown that the occurrence of neural tube defects has decreased by 20–70% following implementation of folic acid food fortification policies [12–15]. Colombia passed folic acid food fortification legislation in 1996 [16], but our data were collected after fortification was implemented, so we cannot determine whether deaths due to neural tube defects decreased after implementation. Therefore, it would be important to collect other data to assess whether rates of neural tube defects have reached optimal levels achievable through food fortification [17] across all population groups [18].
Another important finding was that mortality rates due to congenital anomalies increased substantially as one moves away from urban areas. In particular, rates were more than three times higher in villages and six times higher in rural areas compared to urban areas. In Chile, infant mortality due to congenital anomalies was also elevated in rural areas [19]. Similar urban/rural disparities were found in Down syndrome birth rates in Australia, where the authors suggested that differences could be caused by inequities in access to prenatal screening and care [20]. Contributors to higher mortality rates in rural Colombia may include lack of access to care and treatment to prevent death, and higher underlying rates of congenital anomalies due to risk factors such as insufficient folic acid intake because fortified staple foods may not be available or affordable.
Consistent with previous studies [19,21], maternal age was another important predictor of mortality due to congenital anomalies. Rates were approximately 70% higher when mothers were ≥35 years of age compared to younger mothers. This may be because older mothers are more likely to have babies with congenital anomalies such as Down syndrome. Other studies [7,22,23] have found higher rates of some congenital anomalies among women aged 35–40 [23], but mortality was not assessed. Older maternal age has also been associated with fetal mortality in general [24], which is what we found in our data, but it is nclear how much that association can explain higher rates of fetal mortality due to congenital anomalies among older women. Male sex was also associated with slightly higher mortality due to congenital anomalies, which is consistent with previous findings of male excess for a number of congenital anomalies [25].
Unsurprisingly, mortality rates due to congenital anomalies were higher with very low birthweights and very early gestational ages. These birth outcomes are likely to be the result rather than the cause of congenital anomalies.
Of note, mortality rates due to congenital anomalies were much higher when accompanying information was missing, such as residence, mother's age, or birth-weight, suggesting that death certificates may be less rigorously filled out when a congenital anomaly is present, or that the mother or other family members may be less likely to provide this information when a congenital anomaly is present.
The problem of assigning cause of death has been a common difficulty in studies investigating congenital anomalies, especially among the fetal deaths where a high percentage of deaths are defined as “unspecified reasons” [26]. Our study also found a high number of cases without a specifically defined cause of death (data not shown). Therefore, there is a need to implement strategies within the healthcare system to improve the registration of causes of death, thus leading to a better understanding of the burden caused by various congenital anomalies [27]. In addition, better death registration in Colombia would improve the evaluation of preventive interventions, such as folic acid food fortification, that target congenital anomalies [15].
This study had several strengths. The study included 10 years of national data, allowing for a country-wide assessment of trends over an extended time period. Furthermore, we reported not only neonatal mortality rates, but also fetal death rates. Very few studies have looked at the burden of congenital anomalies from the perspective of perinatal mortality. This study also provided evidence of the need for better reporting of causes of death and identified subpopulations with higher rates of perinatal mortality due to congenital anomalies.
This study had several limitations. Examining death certificates only captures a small portion of the burden caused by congenital anomalies. Many children with congenital anomalies survive but face serious challenges of disability, intensive medical care, and stigma [28]. Also, as previously mentioned, there was a large proportion of reported deaths without a specified cause. In addition, vital records surveillance underestimates the occurrence of birth defects overall in comparison with active surveillance [29]. Thus, the prevalence of perinatal mortality due to congenital anomalies is likely to be underestimated. Another limitation from our study was that all variables had missing values, making it more difficult to assess risk factors for mortality due to congenital anomalies. Furthermore, in some cases there was a discrepancy between direct cause of death and underlying cause of death, indicating shortcomings in the official mortality register and highlighting the urgent need to train medical doctors on the identification of congenital anomalies and the correct reporting of cause of death to the vital statistics officials [30].
Furthermore, the database did not contain information on congenital anomalies that resulted in elective termination of pregnancy, which is another reason that the true impact of congenital anomalies in this population was underestimated.
In conclusion, we did not observe any clear increasing or decreasing trends in fetal or neonatal mortality rates due to congenital anomalies between 1999 and 2008; the rates remained relatively stable over this time period. These surveillance data are useful for identifying regional, demographic, and socioeconomic risk factors affecting fetal and neonatal mortality in Colombia. These data also point to an opportunity for intervention, since they show that many deaths due to congenital anomalies may be preventable or treatable. These interventions can be targeted to address those subpopulations that have the biggest risk factors for mortality due to congenital anomalies. Finally, there is an urgent need to implement population-based surveillance to monitor all occurrence of congenital anomalies rather than only fatal congenital anomalies, and to improve early identification and referral to services for newborns that survive.
Footnotes
Disclosure statement: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.World Health Organization. Congenital anomalies. 2015 [Internet]. Available from: http://www.who.int/mediacentre/factsheets/fs370/en/
- 2.Rosano A, Botto LD, Botting B, et al. Infant mortality and congenital anomalies from 1950 to 1994: an international perspective. J Epidemiol Commun Health. 2000;54:660–666. doi: 10.1136/jech.54.9.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Millennium Development Goals 4 and 5 [Internet] [last accessed 5 Nov 2011]; Available from: http://www.who.int/pmnch/about/about_mdgs/en/
- 4.Organización Panamericana de la Salud. Datos de Mortalidad para Salud en las Américas 2012. 2012 [Internet]. Available from: http://www.paho.org/hq/index.php?-option=com_content&view=article&id=5605&catid=2391%3Adatabases&Itemid=2392&lang=es.
- 5.Baltaxe E, Zarante I. Prevalence of congenital heart disease in 44,985 newborns in Colombia. Archiv Cardiol Mex. 2006;76:263–268. [PubMed] [Google Scholar]
- 6.Zarante I, Franco L, López C. Frequencies of congenital malformations: assessment and prognosis of 52,744 births in three cities of Colombia. Biomedica. 2010;30:65–71. [PubMed] [Google Scholar]
- 7.Barboza-Arguello MDLP, Umana-Solis LM. Analisis de diez anos de registro de malformaciones congenitas en Costa Rica (Ten year analysis of the national registry of congenital anomalies in Costa Rica) Acta Med Costarricense. 2008;50:221–229. [Google Scholar]
- 8.Zeng Z, Zhang H, Liu F, et al. Current diagnosis and treatments for critical congenital heart defects (Review) Exp Ther Med. 2016;11:1550–1554. doi: 10.3892/etm.2016.3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry RJ, Li Z, Erickson JD, et al. Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative Project for Neural Tube Defect Prevention. N Engl J Med. 1999;341:1485–1490. doi: 10.1056/NEJM199911113412001. [DOI] [PubMed] [Google Scholar]
- 10.Blencowe H, Cousens S, Modell B, et al. Folic acid to reduce neonatal mortality from neural tube disorders. Int J Epidemiol. 2010;39:i110–i121. doi: 10.1093/ije/dyq028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crider KS, Devine O, Hao L, et al. Population red blood cell folate concentrations for prevention of neural tube defects: Bayesian model. BMJ (Online) 2014;349:g4554. doi: 10.1136/bmj.g4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castillo-Lancellotti C, Tur JA, Uauy R. Impact of folic acid fortification of flour on neural tube defects: a systematic review. Public Health Nutr. 2013;16:901–911. doi: 10.1017/S1368980012003576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenthal J, Casas J, Taren D, et al. Neural tube defects in Latin America and the impact of fortification: a literature review. Public Health Nutr. 2014;17:537–550. doi: 10.1017/S1368980013000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos LMP, Lecca RCR, Cortez-Escalante JJ, et al. Prevention of neural tube defects by the fortification of flour with folic acid: a population-based retrospective study in Brazil. Bull World Health Organ. 2016;94:22–29. doi: 10.2471/BLT.14.151365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams J, Mai CT, Mulinare J, et al. Updated estimates of neural tube defects prevented by mandatory folic acid fortification — United States, 1995–2011. Morbid Mortal Week Rep. 2015;64:1–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Government of Colombia. DECRETO NÚMERO 1944 DE 1996 (Octubre 28) por el cual se reglamenta la for-tificación de la harina de trigo y se establecen las condiciones de comercializacion, rotulado, vigilancia y control. 1996 [Internet]. Available from: https://www.invima.gov.co/images/stories/aliementos/decreto_1944_1996.pdf.
- 17.Cordero AM, Crider KS, Rogers LM, et al. Optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects: World health organization guidelines. Morbid Mortal Week Rep. 2015;64:421–423. [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenthal J, Lopez-Pazos E, Dowling NF, et al. Folate and Vitamin B12 deficiency among non-pregnant women of childbearing-age in Guatemala 2009–2010: prevalence and identification of vulnerable populations. Matern Child Health J. 2015;19:2272–2285. doi: 10.1007/s10995-015-1746-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taucher E, Icaza G. Infant mortality differentials from congenital malformations with paired data. Rev Med Chile. 2001;129:405–412. [PubMed] [Google Scholar]
- 20.Coory MD, Roselli T, Carroll HJ. Antenatal care implications of population-based trends in Down syndrome birth rates by rurality and antenatal care provider, Queensland, 1990–2004. Med J Aust. 2007;186:230–234. doi: 10.5694/j.1326-5377.2007.tb00878.x. [DOI] [PubMed] [Google Scholar]
- 21.Kiely JL, Paneth N, Susser M. An assessment of the effects of maternal age and parity in different components of perinatal mortality. Am J Epidemiol. 1986;123:444–454. doi: 10.1093/oxfordjournals.aje.a114259. [DOI] [PubMed] [Google Scholar]
- 22.Chen XK, Wen SW, Fleming N, et al. Teenage pregnancy and congenital anomalies: which system is vulnerable? Hum Reprod. 2007;22:1730–1735. doi: 10.1093/humrep/dem043. [DOI] [PubMed] [Google Scholar]
- 23.Reefhuis J, Honein MA. Maternal age and non-chromosomal birth defects, Atlanta – 1968–2000: teenager or thirty-something, who is at risk? Birth Defect Res A. 2004;70:572–579. doi: 10.1002/bdra.20065. [DOI] [PubMed] [Google Scholar]
- 24.Gordon A, Raynes-Greenow C, McGeechan K, et al. Risk factors for antepartum stillbirth and the influence of maternal age in New South Wales Australia: a population based study. BMC Pregnancy Childbirth. 2013;13:12. doi: 10.1186/1471-2393-13-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lisi A, Botto LD, Rittler M, et al. Sex and congenital malformations: an international perspective. Am J Med Genet. 2005;134A:49–57. doi: 10.1002/ajmg.a.30514. [DOI] [PubMed] [Google Scholar]
- 26.Cockerill R, Whitworth MK, Heazell AEP. Do medical certificates of stillbirth provide accurate and useful information regarding the cause of death? Paediatr Perinat Epidemiol. 2012;26:117–123. doi: 10.1111/j.1365-3016.2011.01247.x. [DOI] [PubMed] [Google Scholar]
- 27.Walker S, Rampatige R, Wainiqolo I, et al. An accessible method for teaching doctors about death certification. Health Inform Manage J. 2012;41:4–10. doi: 10.1177/183335831204100101. [DOI] [PubMed] [Google Scholar]
- 28.Christianson A, Howson CP, Modell B. Global report on birth defects: the hidden toll of dying and disabled children. White Plains (NY): March of Dimes Foundation; 2006. [Google Scholar]
- 29.Banerjee E, Zabel E, Alexander B. Comparison of defects identified through Minnesota's Birth Defects Information System And Vital Records, 2006–2008. J Reg Manage. 2012;39:8–12. [PubMed] [Google Scholar]
- 30.Gupta N, Bharti B, Singhi S, et al. Errors in filling WHO death certificate in children: lessons from 1251 death certificates. J Trop Pediatr. 2014;60:74–78. doi: 10.1093/tropej/fmt059. [DOI] [PubMed] [Google Scholar]