Abstract
Background
The Organ Procurement and Transplantation Network requires that United States transplant centers maintain follow-up with living donors for 2 years postdonation, but lack of donor follow-up is pervasive. Donor characteristics, including younger age, minority race, and lower education, have been associated with incomplete follow-up, but it is unknown whether altruistic donors, having no prior connection to their recipient, differ from traditional donors in their likelihood of follow-up.
Methods
Utilizing Scientific Registry of Transplant Recipients data, we examined all adult living kidney donors from 2005–2015 (n=63 592) classified as altruistic or traditional, and compared likelihood of 6-month medical follow-up using modified Poisson regression.
Results
Altruistic donors did not differ from traditional donors in likelihood of follow-up (aRR: 1.02, 95% CI: 0.99–1.06). Among previously identified at-risk subgroups, however, altruistic donors were more likely to have follow-up than their traditional counterparts, including those who were younger (aRR: 1.04, 95% CI: 1.00–1.09), had less than college education (aRR: 1.05, 95% CI: 1.00–1.11), and were unmarried (aRR: 1.08, 95% CI: 1.04–1.12). Having medical follow-up at 6 months was significantly associated with having follow-up at 1 (aRR: 1.84, 95% CI: 1.75–1.93) and 2 years (aRR: 1.63, 95% CI: 1.56–1.70) postdonation.
Conclusions
These data provide additional granularity on living donor phenotypes associated with short-term (6 month) postdonation follow-up, which is important given its association with future likelihood of follow-up. These findings offer the opportunity to tailor and direct educational efforts to increase living donor follow-up, particularly among groups at higher risk of loss to follow-up.
Introduction
The Organ Procurement and Transplantation Network (OPTN) began requiring postdonation follow-up on all living donors in the United States in 2005, and since 2013 the OPTN has defined specific thresholds for completeness of data submission. For individuals who donated after December 31, 2014, transplant programs are required to document complete clinical information on 80% and laboratory data on 70% of donors, at each follow-up milestone, with the stated goals of monitoring the safety and well-being of living donors while allowing for ongoing quality improvement assessments.1
Despite these requirements, lack of donor follow-up persists among US transplant centers. In 2015, Schold and colleagues found that only 67% of donors had complete clinical data at 6 months, which decreased to 60% at 1 year and 50% at 2 years. Completeness for laboratory data at 6 months, 1 year, and 2 years was 51%, 40%, and 30%, respectively.2 Their analysis identified younger age, African American race, lack of insurance, and lower educational attainment as factors that were associated with higher odds of missing laboratory data. In contrast, they found that a higher proportion of nonbiological or unrelated donors had complete laboratory follow-up than those biologically-related, and on adjusted analyses, nonbiological donors had lower odds of missing follow-up when compared to donors who were the biological parent of the recipient (adjusted odds ratio (aOR): 0.88, 95% confidence interval (CI): 0.78–0.99, p=0.03). Recent data by Henderson et al, of living donor follow-up after implementation of the UNOS mandate also demonstrated that only 68% of transplant centers met criteria for complete living donor follow-up at 6-months postdonation, decreasing to 54% at 2-years.3 Neither study, however, examined likelihood of postdonation follow-up among the subset of nonbiological donors known as nondirected or altruistic living kidney donors.
There has been an increase in living unrelated donation in the United States, with the number of nonbiological donors doubling since 2000, predominantly through improvements in immunosuppressive therapy and the use of kidney paired exchanges and incompatible transplant programs.4 The group of living donors that often serves as the starting point for kidney chains, the altruistic or nondirected donor, has seen the largest rate of growth.5 Altruistic donors are characterized by donation to a stranger or someone with whom the donor has no previous relationship and for which they receive no direct benefit.6 The transplant community has traditionally been skeptical of these donors’ motivation to donate and their psychological well-being, but this nontraditional living donor source has become more accepted, increasing 8-fold from 20 transplants in 2000 to 163 transplants in 2015 and accounting for just over 3% of all living donors in 2014.5 In fact, in response to this growing segment of living donors, a national consensus conference was held to discuss practice guidelines for approval and care of these donors.7
When compared to traditional living donors, altruistic donors are older, more often Caucasian, and have higher levels of education, characteristics all associated with higher likelihood of postdonation follow-up.2,5,8 However, altruistic donors lack a predonation connection to the recipient and are less likely to report having had personal experiences with transplantation or medicine prior to contacting the transplant center than their traditional counterparts.9 They are also are less likely to report having received support for their decision to donate when compared to traditional donors, with some even reporting resistance from spouses or other family members.8,10 As a result, centers that more commonly approve this type of donor may be particularly vulnerable to gaps in follow-up and regulatory sanctions, but to date, the association between nondirected donation and medical follow-up has not been examined. Interestingly, surveys have shown that the proportion of individuals that say they would consider donating a kidney to a stranger in need ranges from 10% to 50%, demonstrating that altruistic donation is an acceptable practice among the public.11–15 As altruistic donation continues to grow in acceptance by the transplant community, persons considering nondirected donation have the potential to increase the number of living donor inquiries and transplants.16 However, the effect of the altruistic donor type on postdonation follow up is unknown. Herein, we report results from the first national study to assess the impact of nondirected (altruistic) donation on likelihood of postdonation medical follow-up at 6 months.
Materials and Methods
Data source
This study used data from the Scientific Registry of Transplant Recipients (SRTR), which includes data on all donor, waitlisted candidates, and transplant recipients in the US, submitted by members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration of the US Department of Health and Human Services provides the oversight to the activities of the OPTN and SRTR contractors.
Study population
We identified all adult kidney-only living donors between January 2005 and July 2015 (n=63 592), and classified them as altruistic based on the SRTR code for nondirected donor type (n=1242) or traditional donor (n=62 350).
Outcome
Medical follow-up was defined as having a recorded measurement of serum creatinine at 6 months postdonation. We also examined whether the likelihood of having medical follow-up at 1 and 2 years was associated with having recorded medical follow-up at 6 months. These data are presented as supplementary tables (Tables S1 and S2).
Data analyses
We described donor characteristics by living donor type (altruistic vs. traditional) using measures of central tendency and spread for continuous variables and frequencies for categorical variables. Donor characteristics were compared using t tests and Wilcoxon rank sum tests or chi-square tests as appropriate. We examined the frequency of altruistic donation by transplant center and found substantial center-level variation in the utilization of these donors. As such, we performed adjusted analyses using modified Poisson regression with robust standard errors to account for clustering at the center level. Multivariable models adjusted for donor age, race (African American, Caucasian, Other, gender, education level, marital status, obesity (BMI≥ 30 kg/m2), history of hypertension, health insurance status at the time of donation, history of cigarette smoking, year of donation, and whether the donor resided in the same state as the transplant center. Factors significant on unadjusted analyses were considered for model building, with the most parsimonious model chosen by minimizing the quasi-likelihood under the independence model criterion (QIC). We examined the presence of effect modification of altruistic status by other covariates using stratified analyses for covariates significant on adjusted analyses. Donors who were missing information (ranging from 2% missing smoking status to 18% missing health insurance) were excluded from the final model.
Sensitivity analyses
To confirm that the 18 321 patients who were missing at least 1 data element did not affect the conclusions, we conducted several sensitivity analyses. We first coded missing covariates as “Missing” to allow for inclusion in the adjusted analyses. We then set those who were missing an observation for a variable to a “no” response for that variable, and finally we performed multiple imputation. Given the significant differences between altruistic and traditional donors, we also performed exact 1:5 matching without replacement. Inferences of the model including only complete cases were consistent, and for simplicity the complete case analysis has been reported.
Results
Donor Characteristics
Overall, 70.4% of all donors had medical follow-up at 6 months (77.4% among altruistic vs. 70.3% among traditional, p < 0.001). When compared to traditional donors, altruistic donors were older (43.9 years vs. 41.4 years), more often male (45.4% vs. 39.0%), and were less often African American (2.4% vs. 12.0%). At the time of donation, altruistic donors were more likely to have had a college or higher education (53.1% vs. 34.7%) or to have had health insurance (83.7% vs. 68.9%), whereas they were less likely to have been smokers (19.8% vs. 24.6%) or obese (14.1% vs. 22.3%). Altruistic donors also had a shorter median surgical length of stay (2.0 days vs. 3.0 days) when compared to their traditional donor counterparts and were less likely than traditional donors to reside in the same state as the center performing the transplant (65.8% vs. 68.7%, p=0.03) (Table 1).
Table 1.
Characteristics of altruistic vs. all other living donors (N=63 592).
| Characteristics | Altruistic | Traditional | p value |
|---|---|---|---|
| N=1242 | N=62 350 | ||
| Age at donation (years), Mean (SD) | 43.9 (12.3) | 41.4 (11.5) | < 0.001 |
| Age ≥ 50 years, % | 37.4 | 26.4 | < 0.001 |
| Male, % | 45.4 | 39.0 | < 0.001 |
| Race | |||
| African American, % | 2.4 | 12.0 | < 0.001 |
| Caucasian | 95.3 | 83.2 | |
| Other | 2.3 | 4.9 | |
| Preoperative systolic BP, mean (SD) | 121.0 (12.7) | 120.9 (13.2) | 0.65 |
| Preoperative diastolic BP, mean (SD) | 74.3 (8.6) | 73.6 (9.4) | 0.003 |
| History of hypertension, % | 2.5 | 2.6 | 0.10 |
| College or higher education, % | 53.1 | 34.7 | < 0.001 |
| Health insurance, % | 83.7 | 68.9 | < 0.001 |
| History of cigarette use, % | 19.8 | 24.6 | < 0.001 |
| Married/life partner, % | 59.0 | 61.5 | 0.06 |
| Obese (BMI ≥ 30 kg/m2), % | 14.1 | 22.3 | < 0.001 |
| Surgical length of stay (days), median (IQR) | 2.0 (2–3) | 3.0 (2–3) | < 0.001 |
| In-state donor, % | 65.8 | 68.7 | 0.03 |
Center variation
There was notable center level variation in the practice of altruistic donation, with 92 (34.8%) centers in the US having never performed an altruistic donor. Most US transplant centers have accepted at least 1 altruistic donor eg, 105 (39.7%) centers having done 1 to 5 in the past decade and 14 (5.3%)performed more than 20 (Figure 1).
Figure 1.
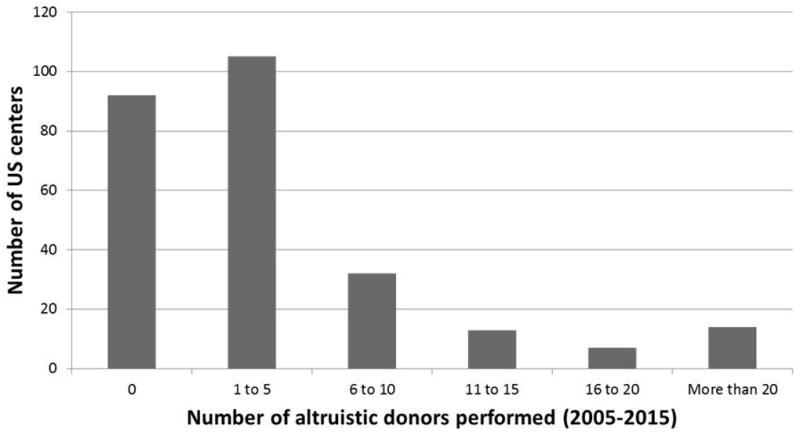
Altruistic donation by transplant center (2005–2015).
Likelihood of follow-up
On unadjusted analyses, altruistic donors were 6% more likely than their traditional counterparts to have 6-month medical follow-up (RR: 1.06, 95%CI: 1.02–1.10, p=0.002). Overall, there was also a higher likelihood of follow-up among donors who were age 50 or older (RR: 1.06, 95% CI: 1.05–1.08, p < 0.001), college educated (RR: 1.06, 95% CI: 1.04–1.08, p < 0.001), married or had a life partner (RR: 1.05, 95% CI: 1.04–1.06, p < 0.001), had a history of hypertension at the time of donation (RR: 1.08, 95% CI: 1.05–1.12, p < 0.001), were insured at donation (RR: 1.08, 95% CI: 1.01–1.12, p < 0.001), and resided in the same state as the transplant center (RR: 1.09, 95% CI: 1.06–1.12, p < 0.001). However, male donors were significantly less likely to have medical follow-up (RR: 0.95, 95% CI: 0.94–0.96, p < 0.001), as were African American donors (RR: 0.96, 95% CI: 0.94–0.98, p < 0.001) and donors who were obese at the time of donation (RR: 0.98, 95% CI: 0.97–0.99, p < 0.001) (Table 2). Similar results were seen for likelihood of medical follow-up at 1 and 2 years, most notably that having a recorded medical follow-up at 6 months was associated with an 84% and 63% higher likelihood of follow-up at 1 and 2 years respectively (Tables S1 and S2).
Table 2.
Unadjusted likelihood of 6-month medical follow-up.
| Relative risk (95% CI) | p value | |
|---|---|---|
| Altruistic | 1.06 (1.02–1.10) | 0.002 |
| Age ≥ 50 years | 1.06 (1.05–1.08) | < 0.001 |
| Race/ethnicity | ||
| Caucasian | Ref | |
| African American | 0.96 (0.94–0.98) | < 0.001 |
| Other | 0.98 (0.95–1.00) | 0.05 |
| Male | 0.95 (0.94–0.96) | < 0.001 |
| College education | 1.06 (1.04–1.08) | < 0.001 |
| Married/life partner | 1.05 (1.04–1.06) | < 0.001 |
| Obese at donation (BMI ≥ 30 kg/m2) | 0.98 (0.97–0.99) | < 0.001 |
| History of hypertension | 1.08 (1.05–1.12) | < 0.001 |
| Insured at donation | 1.08 (1.01–1.12) | < 0.001 |
| History of cigarette use | 0.97 (0.95–0.98) | < 0.001 |
| Surgical LOS | 1.00 (0.99–1.00) | 0.63 |
| Year of donation (per year increase) | 1.03 (1.02–1.05) | < 0.001 |
| In-state donor | 1.09 (1.06–1.12) | < 0.001 |
On adjusted analyses, the association between altruism and medical follow-up was attenuated when year of donation was included in the model, such that there was no longer a significant association (aRR: 1.02, 95% CI: 0.99–1.06, p=0.19) (Table 3). Although altruism was no longer significant after controlling for year of donation, several factors known to be associated with altruistic donation remained significantly associated with likelihood of follow-up, including donor age ≥ 50 years, other race, higher education, obesity, and marital status, prompting us to examine the potential for effect modification. We stratified the adjusted models and found that among donors who were 50 and older, there was no difference in the likelihood of follow-up based on altruistic status (aRR: 0.99, 95% CI: 0.95–1.04, p=0.82); however, among younger donors, altruistic donors were 4% more likely to have medical follow-up when compared to traditional donors (aRR: 1.04, 95% CI: 1.00–1.09, p=0.03). A similar association was seen among less educated donors, with altruistic donors having a 5% increased likelihood of follow-up (aRR: 1.05, 95% CI: 1.00–1.11, p=0.05) and altruistic donors who were single/never married having an 8% increased likelihood of follow-up (aRR: 1.08, 95% CI: 1.04–1.12, p < 0.001), compared to single/never married traditional donors. Additionally, when era of donation was defined as pre-UNOS mandate (prior to February 2013) vs. post, a significant interaction was observed between altruism and era (p=0.047). On stratified analyses, we found that altruistic donors had a significantly increased likelihood of 6-month medical follow-up (aRR: 1.06, 95% CI: 1.01–1.11, p=0.01), while the same association was not observed for altruistic donors in the more recent era (Table 4).
Table 3.
Adjusted likelihood of 6-month medical follow-up.
| Relative risk (95% CI) | p value | |
|---|---|---|
| Altruistic | 1.02 (0.99–1.06) | 0.19 |
| Age ≥ 50 years | 1.05 (1.04–1.07) | < 0.001 |
| Race/ethnicity | ||
| Caucasian | Ref | |
| African American | 0.98 (0.96–1.00) | 0.06 |
| Other | 0.97 (0.95–0.99) | 0.02 |
| Male | 0.96 (0.95–0.97) | < 0.001 |
| College education | 1.04 (1.02–1.05) | < 0.001 |
| Married/life partner | 1.03 (1.02–1.04) | < 0.001 |
| Obese at donation (BMI ≥ 30 kg/m2) | 0.98 (0.97–0.99) | 0.003 |
| History of hypertension | 1.04 (1.01–1.06) | 0.007 |
| Insured at donation | 1.04 (1.00–1.08) | 0.08 |
| History of cigarette use | 0.98 (0.96–0.99) | 0.004 |
| Year of donation (per year increase) | 1.03 (1.02–1.04) | < 0.001 |
| In-state donor | 1.08 (1.06–1.10) | < 0.001 |
Table 4.
Models examining effect modification.
| aRR for altruistic vs. traditional |
95% CI | p value | |
|---|---|---|---|
| Age ≥ 50 years | 0.99 | 0.95–1.04 | 0.82 |
| Age < 50 years | 1.04 | 1.00–1.09 | 0.03 |
| ≥ College Education | 1.00 | 0.96–1.04 | 0.87 |
| < College Education | 1.05 | 1.00–1.11 | 0.05 |
| Married/life partner | 0.99 | 0.94–1.04 | 0.74 |
| Single/never married | 1.08 | 1.04–1.12 | < 0.001 |
| Era 1: Pre-UNOS mandate (2005- Feb. 2013) | 1.06 | 1.01–1.11 | 0.01 |
| Era 2: Post-UNOS mandate (Feb. 2013-June 2015) | 1.00 | 0.95–1.05 | 0.86 |
Discussion
Our national study comparing altruistic to traditional donors found significant center-level variation in the number of altruistic donors accepted at US transplant centers. Compared to traditional donors altruistic donors were not less likely to comply with transplant center follow-up, and in fact, subgroups of altruistic donors were more likely to have medical follow-up postdonation than their traditional counterparts. We detected effect modification by donor age, education level, marital status, and era, with younger, less-educated, unmarried, and earlier traditional donors significantly less likely to have medical follow-up compared to their altruistic counterparts.
With the implementation of the new OPTN living donor specific follow-up requirements, transplant centers can be penalized for failing to meet donor follow-up benchmarks. The UNOS requirements for donor follow-up will not only hold centers accountable for their data collection practices but will also provide more complete data with which to monitor donors. Motivating the regulatory requirements is the need to maintain the safety of prior living donors, both to continue to promote living donation and to establish effective methods for assessing long-term risk. Our findings demonstrated that altruistic donors were at no greater risk of loss-to-follow up at 6 months when compared to traditional donors, an important finding given the increase in this type of donor, as well as providing additional evidence that the UNOS mandate has made progress in achieving its goal of improving follow-up among all living donors. Additionally, our study confirmed previous findings that identified several subgroups of traditional living donors that are less likely to complete follow-up.2,3 Characterizing the living donor phenotype associated with likelihood of postdonation medical follow-up affords opportunities for the development of targeted educational efforts aimed at improving living donor follow-up and may enhance and promote postdonation long-term health. Frequency of follow-up should not differ by donor type, rather these at-risk subgroups should be counseled on the importance of long-term follow-up in the predonation phase.
It is unknown why among subgroups of living donors at high-risk for loss to follow-up (eg, young, less than college education, and single), altruistic donors are more likely to complete follow-up than their traditional high-risk counterparts, particularly given they are less likely than traditional donors to report prior experience with transplantation or the medical field as a motive for donation.9 Qualitative research by Tong et al, obtained from interviews with 18 prior nondirected donors demonstrated that most felt they had been well-prepared for the process of donation, and some reported a sense of connectedness with the medical community resulting from their decision. Additionally, these donors indicated a sense of urgency and commitment surrounding their decision to donate.17 These experiences may contribute to a greater willingness to remain in contact with the transplant center and remain engaged in one’s own health postdonation.
Our data demonstrate that concerns over failure to complete postdonation follow-up should not be a deterrent for approving these altruistic donors even among the subset of donors known to have the highest risk for loss to follow-up, including young, single donors with less than college education, as within this high-risk subset altruistic donors were found to more likely follow-up postdonation than their traditional counterparts. These findings are not surprising, given that altruistic donors report similar health-related quality of life, psychological symptoms, and satisfaction with donation compared to their traditional counterparts or to the general population.18–20 In fact, educational efforts aimed at improving postdonation follow-up may prove most efficacious by targeting young, single, less well-educated traditional living donors rather than altruistic donors.
This study is not without limitations. SRTR data do not capture psychological factors including social support, motive for donation, or history of mental health; these factors may be associated with a donor’s likelihood to complete follow-up as posited by Schold and colleagues, who found that widowed donors were significantly more likely to have missing follow-up data.2 Additionally, the short time frame associated with living donor follow-up in SRTR prevents examination of long-term outcomes, an area that is lacking among altruistic donors whose recorded follow-up time to date is relatively limited.10,18,19 Further studies using qualitative and administrative claims linkage are needed to assess long-term physical and psychological outcomes of these donors, such as psychological well-being and development of end-stage renal disease, and to determine whether early experiences or loss to follow-up may be associated with these longer term outcomes. To maximize the number of donors eligible for inclusion, our analyses were limited to 6-month follow-up, which makes it difficult to compare our results to studies with longer follow-up windows. However, these data represent the totality of altruistic donors in the US since 2005. As such, these data contribute novel and important information about donors who are lost to follow-up in early stages postdonation, and given our findings that likelihood of persistent follow-up at 1 and 2 years was associated with having follow-up at 6 months, suggest that early postdonation follow-up may be most predictive of longer-term follow-up.
In summary, we found that among the subgroup of living donors at highest-risk for failure to follow-up postdonation, including young, single, and less well-educated donors, altruistic donors performed better than their traditional counterparts. These data provide additional granularity on living donor phenotypes associated with postdonation follow-up, and offer the opportunity to more accurately tailor and direct educational efforts aimed to increase living donor follow-up. We believe that future studies aimed at understanding altruistic donors’ motivation for follow-up may help to identify strategies for improving the health maintenance of all living donors and increase compliance with current OPTN reporting requirements.
Supplementary Material
Acknowledgments
This research was supported in part by the National Institutes of Health grant number K23-DK103918 (PI: Locke). The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the SRTR. The interpretation and reporting of these data are the responsibility of the authors and in no way, should be seen as an official policy of or interpretation by the SRTR or US Government.
Abbreviations
- aOR
adjusted odds ratio
- aRR
adjusted relative risk
- CI
confidence interval
- OPTN
Organ Procurement and Transplantation Network
- OR
odds ratio
- RR
relative risk
- SRTR
Scientific Registry of Transplant Recipients
Footnotes
Authorship
Mrs. Reed contributed to the design of the study, performed the data analyses, and wrote the manuscript. Ms. Shelton assisted with data analysis, interpretation, and manuscript revision. Dr. MacLennan consulted on the analyses, assisted with interpretation, and participated in manuscript revision. Dr. Sawinski consulted on the design of the study, assisted with interpretation, and participated in manuscript revision. Dr. Locke oversaw the design of the study, coordinated analyses, and revised the manuscript.
Disclosure
The authors declare no conflicts of interest.
This study was presented at the Living Donor Abdominal Organ Transplant Conference; September 9, 2016; Trieste, Italy.
References
- 1.Organ Procurement and Transplantation Network. [Accessed November 1, 2016];Organ Procurement and Transplantation Network Policies - policy 14: living donation. https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf#nameddest=Policy_14. Updated June 29, 2017.
- 2.Schold JD, Buccini LD, Rodrigue JR, et al. Critical factors associated with missing follow-up data for living kidney donors in the United States. Am J Transplant. 2015;15(9):2394–2403. doi: 10.1111/ajt.13282. [DOI] [PubMed] [Google Scholar]
- 3.Henderson ML, Thomas AG, Shaffer A, et al. The national landscape of living kidney donor follow-up in the United States. Am J Transplant. doi: 10.1111/ajt.14356. [published May 16, 2017] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandelbrot DA, Pavlakis M. Living donor practices in the United States. Adv Chronic Kidney Dis. 2012;19(4):212–219. doi: 10.1053/j.ackd.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faber DA, Joshi S, Ciancio G. Demographic characteristics of non-directed altruistic kidney donors in the United States. J Kidney. 2016;2(121) [Google Scholar]
- 6.Organ Procurement and Transplantation Network. [Accessed November 1, 2016];Living non-directed organ donation. https://optn.transplant.hrsa.gov/resources/ethics/living-non-directed-organ-donation/. Updated December 2015.
- 7.Adams PL, Cohen DJ, Danovitch GM, et al. The nondirected live-kidney donor: ethical considerations and practice guidelines: a national conference report. Transplantation. 2002;74(4):582–589. doi: 10.1097/00007890-200208270-00030. [DOI] [PubMed] [Google Scholar]
- 8.Maple H, Chilcot J, Burnapp L, et al. Motivations, outcomes, characteristics of unspecified (nondirected altruistic) kidney donors in the United Kingdom. Transplantation. 2014;98(11):1182–1189. doi: 10.1097/TP.0000000000000340. [DOI] [PubMed] [Google Scholar]
- 9.Henderson AJ, Landolt MA, McDonald MF, et al. The living anonymous kidney donor: lunatic or saint? Am J Transplant. 2003;3(2):203–213. doi: 10.1034/j.1600-6143.2003.00019.x. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs CL, Roman D, Garvey C, Kahn J, Matas AJ. Twenty-two nondirected kidney donors: an update on a single center’s experience. Am J Transplant. 2004;4(7):1110–1116. doi: 10.1111/j.1600-6143.2004.00478.x. [DOI] [PubMed] [Google Scholar]
- 11.Spital A. Public attitudes toward kidney donation by friends, altruistic strangers in the United States. Transplantation. 2001;71(8):1061–1064. doi: 10.1097/00007890-200104270-00009. [DOI] [PubMed] [Google Scholar]
- 12.Toronyi E, Alfoldy F, Jaray J, et al. Attitudes of donors towards organ transplantation in living related kidney transplantations. Transpl Int. 1998;11(Suppl 1):S481–483. doi: 10.1007/s001470050524. [DOI] [PubMed] [Google Scholar]
- 13.Landolt MA, Henderson AJ, Barrable WM, et al. Living anonymous kidney donation: what does the public think? Transplantation. 2001;71(11):1690–1696. doi: 10.1097/00007890-200106150-00034. [DOI] [PubMed] [Google Scholar]
- 14.Sadler HH, Davison L, Carroll C, Kountz SL. The living, genetically unrelated, kidney donor. Semin Psychiatry. 1971;3(1):86–101. [PubMed] [Google Scholar]
- 15.Fellner CH, Schwartz SH. Altruism in disrepute. Medical versus public attitudes toward the living organ donor. N Engl J Med. 1971;284(11):582–585. doi: 10.1056/NEJM197103182841105. [DOI] [PubMed] [Google Scholar]
- 16.Landolt MA, Henderson AJ, Gourlay W, et al. They talk the talk: surveying attitudes judging behavior about living anonymous kidney donation. Transplantation. 2003;76(10):1437–1444. doi: 10.1097/01.TP.0000085289.19858.90. [DOI] [PubMed] [Google Scholar]
- 17.Tong A, Craig JC, Wong G, et al. “It was just an unconditional gift.” Self reflections of non-directed living kidney donors. Clin Transplant. 2012;26(4):589–599. doi: 10.1111/j.1399-0012.2011.01578.x. [DOI] [PubMed] [Google Scholar]
- 18.Massey EK, Kranenburg LW, Zuidema WC, et al. Encouraging psychological outcomes after altruistic donation to a stranger. Am J Transplant. 2010;10(6):1445–1452. doi: 10.1111/j.1600-6143.2010.03115.x. [DOI] [PubMed] [Google Scholar]
- 19.Rodrigue JR, Schutzer ME, Paek M, Morrissey P. Altruistic kidney donation to a stranger: psychosocial, functional outcomes at two US transplant centers. Transplantation. 2011;91(7):772–778. doi: 10.1097/TP.0b013e31820dd2bd. [DOI] [PubMed] [Google Scholar]
- 20.Timmerman L, Zuidema WC, Erdman RA, et al. Psychologic functioning of unspecified anonymous living kidney donors before, after donation. Transplantation. 2013;95(11):1369–1374. doi: 10.1097/TP.0b013e31828eaf81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


