Key Teaching Points.
-
•
Epicardial unipolar electrogram recording with the filter setting in the same manner as surface electrocardiograms (ECGs) could reveal the local J-ST elevation on the right ventricle in Brugada syndrome.
-
•
The type of J-ST elevation in unipolar electrodes could be related to the local activation delay in bipolar electrodes.
-
•
However, after pilsicainide administration, the association between the type of J-ST elevation and local conduction delay was attenuated.
Introduction
The mechanisms of J-ST elevation in the right precordial leads in patients with Brugada syndrome (BrS) remain controversial (ie, repolarization vs depolarization hypotheses).1 Recently, epicardial substrate ablation for late fractionated potentials and a low-voltage area (LVA) in the right ventricular outflow tract (RVOT) has been performed for ventricular fibrillation (VF) that is not controllable with medications.2 Epicardial ablation is reported to be effective for the suppression of VF recurrence, and it eliminates J-ST elevation in most cases.2 Unipolar electrodes used in the 3-dimensional mapping system are, however, generally recorded with different filters than those of surface electrocardiograms (ECGs). As such, we could not precisely compare the morphology of the J-ST segment in unipolar electrodes with those in surface ECGs. The relationship between J-ST elevation in surface ECGs and bipolar fractionated and low-amplitude electrograms in the RVOT epicardium remains unclear.
We present a unique case of epicardial substrate mapping using unipolar electrodes with filter setting that is the same as surface ECGs (0.05–100 Hz).3, 4 We investigated the correlation between unipolar J-ST elevation and bipolar abnormal potentials in a patient with BrS who had episodes of VF recurrence.
Case report
A 43-year-old man with BrS who had undergone implantation of an implantable cardioverter-defibrillator for secondary prevention was admitted to our institution for electrical storm of VF refractory to quinidine, bepridil, and cilostazol. Even after a continuous infusion of isoproterenol, VF was induced by frequent premature ventricular contraction.
Both the endocardial approach with femoral venous access and the epicardial approach with mini-thoracotomy were performed for arrhythmogenic substrate modification using the 3-dimensional mapping system (CARTO 3, Biosense Webster, Diamond Bar, CA). Endocardial and epicardial substrate maps were obtained using an irrigated-tip ablation catheter (ThermoCool SmartTouch, Biosense Webster). We recorded local unipolar electrograms with a 0.05- to 100-Hz bandwidth and local bipolar electrograms with a 30- to 250-Hz bandwidth, as described previously.3, 4 The voltage map (Bi-amp) was constructed by bipolar amplitudes, and the map of late activation time (LAT) demonstrated the time from the beginning of QRS in lead V2 to the offset of the latest local bipolar component. Local unipolar ST level at the timing of J point in lead V5 (J-ST) and local unipolar ST level at the timing of 40 ms after J point in lead V5 (J40-ST) were also evaluated. In bipolar voltage maps, the LVA was defined as the voltage area recorded ≤ 1.5 mV. The ST level with 0.05–100 Hz filtering was carefully measured in a proximal electrode to exclude the influence of baseline drift. The unipolar electrograms were divided into 4 groups according to form: (1) no–ST elevation group, defined as <0.2 mV at J-ST without ST elevation in the following phase (shown as a green tag); (2) saddleback-type group, defined as ≥0.2 mV at J-ST with concave upward ST elevation (shown as a yellow tag); (3) coved-type group, defined as ≥0.2 mV at J-ST with negative T wave (shown as a pink tag); and (4) convex-type group, defined as ≥0.2 mV convex-type ST elevation without negative T wave (this was only recorded after the pilsicainide challenge test; shown as a red tag) (Figures 1A and 2A).
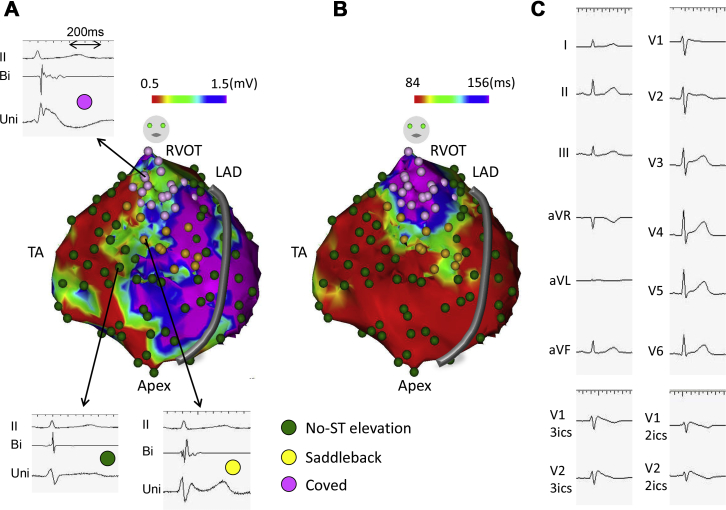
Figure 1.
The relationship of unipolar ST elevation type with the bipolar voltage map (A) and the local activation time (LAT) map (B) and surface electrocardiogram (ECG) (C) before the administration of pilsicainide. A: The unipolar electrogram reveals saddleback-type ST elevation in the middle level of the right ventricular outflow tract (RVOT) and coved-type ST elevation in the high level of the RVOT. There is no obvious relationship between ST elevation type and bipolar voltage. Representative bipolar and unipolar electrograms are shown in each of the ST elevation types. B: ST elevation type clearly relates to prolonged LAT in the RVOT. C: Surface ECG on the standard position and V1 and V2 on the third and second intercostal spaces (3ics and 2ics, respectively) before pilsicainide administration. No–ST elevation type is shown as a green tag, saddleback-type is shown as a yellow tag, and coved-type is shown as a pink tag in panels A and B. LAD = left anterior descending artery; TA = tricuspid annulus.
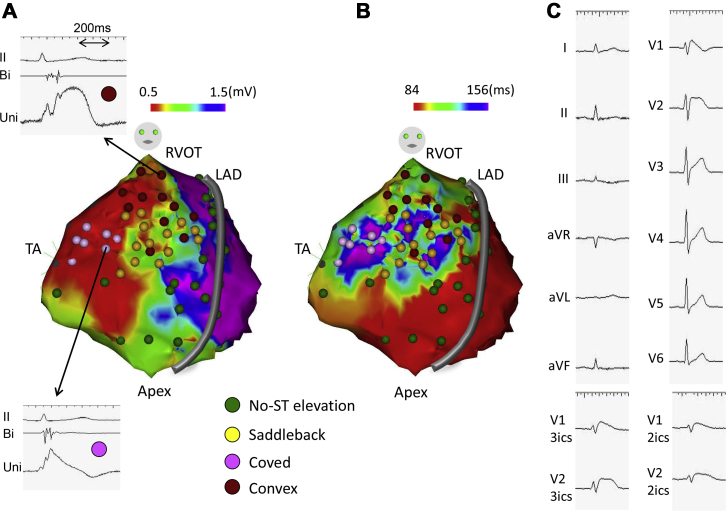
Figure 2.
The relationship of unipolar ST elevation type with the bipolar voltage map (A) and the local activation time (LAT) map (B) and surface electrocardiogram (ECG) (C) after the administration of pilsicainide. A: The unipolar electrogram shows both saddleback-type and convex-type ST elevation in the middle level of the right ventricular outflow tract (RVOT), coved-type ST elevation in the tricuspid annulus, and convex-type ST elevation in the high level of the RVOT. Representative bipolar and unipolar electrograms are shown for each of the ST elevation types. B: The prolonged LAT zone in the low-voltage area of ≤0.5 mV (shown in A) shows coved- or convex-type ST elevation. C: Surface ECG after pilsicainide administration. Convex-type is shown as a red tag. Other colored dots are the same as those described in Figure 1.
The endocardial voltage map revealed normal voltage and no fragmented or split potentials, including the RVOT. In the epicardial bipolar voltage map, LVA was identified from the tricuspid annulus (TA) region to the RVOT and the inferior wall (Figure 1A). Most of the coved-type and saddleback-type unipolar electrograms were presented in the moderately impaired voltage area. No relationships were found between bipolar amplitudes and J-ST or J40-ST levels (data not shown). With regard to the epicardial LAT map, the final excitation area was the RVOT (Figure 1B). Saddleback-type tags were found in the moderately delayed excitation area, shown as the yellow and green zone, and coved-type tags in the most delayed excitation area, shown as the blue and purple zone. Surface ECG exhibited coved-type ST elevation in leads V1 and V2 on the upper intercostal spaces (Figure 1C). Both J-ST and J40-ST levels were positively correlated with LAT (Figure 3A, B).
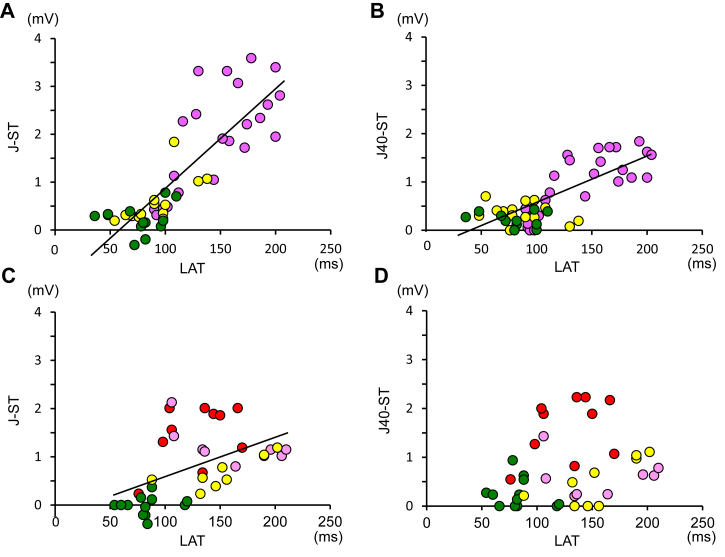
Figure 3.
The relationship between local activation time (LAT) and local unipolar ST elevation at the timing of J point (J-ST) and 40 ms after J-point (J40-ST) in lead V5. A: Before the administration of pilsicainide. LAT is positively correlated with J-ST, the regression line y = 0.02x − 1.26, r = 0.84, P < .01, and n = 50. B: Before the administration of pilsicainide. J40-ST is also positively correlated with LAT, the regression line y = 0.01x − 0.48, r = 0.77, P < .01, and n = 50. C: After the administration of pilsicainide. LAT is positively correlated with J-ST, the regression line y = 0.01x − 0.25, r = 0.50, P < .01, and n = 40. D: After the administration of pilsicainide. J40-ST has no relationship with LAT, n = 40. Colored dots are the same as those described in Figures 1 and 2.
After the administration of pilsicainide (50 mg), surface ECG exhibited coved-type ST elevation even on the standard intercostal space (Figure 2C). The LVA expanded and coved-type ST elevation observed with a unipolar electrode changed to convex-type ST elevation in the RVOT (Figure 2A). It is of note that the highly reduced voltage area (red zone) near the TA exhibited coved-type ST elevation in which ST elevation was not observed before pilsicainide administration. In the LAT map, epicardial myocardial excitation showed mosaic pattern in the right ventricular free wall; the delayed excitation area, including the TA region and the RVOT, exhibited ST elevation (Figure 2B). J-ST but not J40-ST level was positively correlated with LAT after pilsicainide administration (Figure 3C, D).
Owing to the ablation of the epicardial substrate that was determined to be a fractionated potential with a prolonged LAT area, the J-ST level decreased and coved-type ST elevation disappeared in the right precordial leads at all intercostal spaces. After the procedure, the patient experienced no episodes of implantable cardioverter-defibrillator–appropriate therapy or detections of VF.
Discussion
These images illustrate the relationship between LAT and J-ST elevation as recorded in unipolar electrodes filtering in the same manner as surface ECGs in the RVOT epicardium. BrS is characterized as ST elevation in the right precordial leads.5 It is known that fragmented potentials can be recorded in the RVOT epicardium, and the RVOT has been suggested as the origin of arrhythmic activity in BrS.6, 7 Recent studies reported that slow conduction has been identified in the area without overt voltage abnormalities in the RVOT.8, 9 Zhang and colleagues9 reported that ST elevation at the J-point is correlated with the dispersion between the latest activation time on the epicardium and endocardium in the RVOT, but not the LVA. Similarly, the J-ST level in the present case was associated with LAT, but not with bipolar amplitudes. Especially in the inferior wall, J-ST did not elevate completely despite a broad range of LVA because of the shorter LAT than those in the RVOT (Figure 1A, B). Moreover, the unipolar electrogram in the TA region after the administration of pilsicainide exhibited coved-type ST elevation despite the normal ST level before administration; the LAT in the TA after pilsicainide administration was longer than that before administration (Figures 1B and 2B). These results also suggest that the type of ST elevation is dependent on the LAT, which correlates with conduction delay.
J-ST levels in the right precordial leads on surface ECG decreased after the procedure. These results verified the conduction disorder hypothesis of ST elevation in the J point in Brugada-type ECG.10 Recent claims that the localized abnormal potentials in the RVOT represent a pure depolarization abnormality cannot, however, be completely verified.9, 11 As in the present case, convex-type ST elevation was observed in the RVOT after the pilsicainide challenge test despite the shorter LAT than those before the pilsicainide challenge test in the RVOT (Figures 1B and 2B). However, this might be associated with pilsicainide-induced localized conduction block or reduced amplitude of delayed potentials, leading to short LAT. Proponents of a new conduction disorder hypothesis, current-to-load mismatch, might, however, posit that short LAT makes prominent ST elevation.10 According to this theory, the deterioration of conduction abnormalities leads to conduction block of the conduction isthmus, resulting in short LAT and convex-type ST elevation. Moreover, pilsicainide-induced inhomogeneous conduction owing to local conduction block may have failed to show correlation between LAT and J40-ST after pilsicainide administration.
Regardless of evaluation on the same area for the accurate comparison of electrograms between before and after pilsicainide test, the measurement points after pilsicainide infusion could not completely match those same points measured before pilsicainide infusion, leading to the limitations of the present case.
In conclusion, this case demonstrates that local conduction delay in the RVOT epicardium is associated with J-ST elevation in BrS.
Acknowledgments
We thank Dr Naomasa Makita, Nagasaki University; Dr Masahiko Takagi, Kansai Medical University Medical Center; Dr Kohei Yamashiro, Takatsuki General Hospital; Dr Yuichiro Sakamoto, Toyohashi Heart Center; Dr Haruo Honjo, Nagoya University; Dr Masatoshi Yamazaki, The University of Tokyo; and Dr Hiroshi Nakagawa, The University of Oklahoma, for their generous support to our study.
Footnotes
Dr Kusano has received lecture fees from Medtronic Japan.
References
- 1.Wilde A.A., Postema P.G., Di Diego J.M., Viskin S., Morita H., Fish J.M., Antzelevitch C. The pathophysiological mechanism underlying Brugada syndrome: depolarization versus repolarization. J Mol Cell Cardiol. 2010;4:543–553. doi: 10.1016/j.yjmcc.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nademanee K., Veerakul G., Chandanamattha P., Chaothawee L., Ariyachaipanich A., Jirasirirojanakorn K., Likittanasombat K., Bhuripanyo K., Ngarmukos T. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011;123:1270–1279. doi: 10.1161/CIRCULATIONAHA.110.972612. [DOI] [PubMed] [Google Scholar]
- 3.Nakagawa K., Nagase S., Morita H., Ito H. Left ventricular epicardial electrogram recordings in idiopathic ventricular fibrillation with inferior and lateral early repolarization. Heart Rhythm. 2014;11:314–317. doi: 10.1016/j.hrthm.2013.10.057. [DOI] [PubMed] [Google Scholar]
- 4.Nagase S., Tanaka M., Morita H., Nakagawa K., Wada T., Murakami M., Nishii N., Nakamura K., Ito H., Ohe T., Kusano K.F. Local left ventricular epicardial J waves and late potentials in Brugada syndrome patients with inferolateral early repolarization pattern. Front Physiol. 2017;8:14. doi: 10.3389/fphys.2017.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brugada P., Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–1396. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 6.Nagase S., Kusano K.F., Morita H., Fujimoto Y., Kakishita M., Nakamura K., Emori T., Matsubara H., Ohe T. Epicardial electrogram of the right ventricular outflow tract in patients with the Brugada syndrome: using the epicardial lead. J Am Coll Cardiol. 2002;12:1992–1995. doi: 10.1016/s0735-1097(02)01888-0. [DOI] [PubMed] [Google Scholar]
- 7.Yokokawa M., Takaki H., Noda T., Satomi K., Suyama K., Kurita T., Kamakura S., Shimizu W. Spatial distribution of repolarization and depolarization abnormalities evaluated by body surface potential mapping in patients with Brugada syndrome. Pacing Clin Electrophysiol. 2006;29:1112–1121. doi: 10.1111/j.1540-8159.2006.00505.x. [DOI] [PubMed] [Google Scholar]
- 8.Brugada J., Pappone C., Berruezo A., Vicedomini G., Manguso F., Ciconte G., Giannelli L., Santinelli V. Brugada syndrome phenotype elimination by epicardial substrate ablation. Circ Arrhythm Electrophysiol. 2015;8:1373–1381. doi: 10.1161/CIRCEP.115.003220. [DOI] [PubMed] [Google Scholar]
- 9.Zhang P., Tung R., Zhang Z. Characterization of the epicardial substrate for catheter ablation of Brugada syndrome. Heart Rhythm. 2016;13:2151–2158. doi: 10.1016/j.hrthm.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 10.Hoogendijk M.G., Potse M., Vinet A. ST segment elevation by current-to-load mismatch: an experimental and computational study. Heart Rhythm. 2011;8:111–118. doi: 10.1016/j.hrthm.2010.09.066. [DOI] [PubMed] [Google Scholar]
- 11.Yan G.X., Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation. 1999;100:1660–1666. doi: 10.1161/01.cir.100.15.1660. [DOI] [PubMed] [Google Scholar]