Highlights
-
•
An abdominal wall abscess without a known cause requires thorough investigation.
-
•
We describe a case of right abdominal wall abscess and spontaneous drainage.
-
•
Appendicitis necessitatis needs to be considered a cause of abdominal wall abscess.
Keywords: Appendicitis, Abdominal abscess, Appendicitis necessitatis, Case report
Abstract
Introduction
Appendicitis is a common cause of acute abdomen; however, the classic clinical signs are not often present, and it has unusual presentations. Thus, its diagnosis can be challenging. PRESENTATION OF CASE: We describe the case of an elderly man who presented with right abdominal wall abscess with spontaneous drainage in the emergency department. Since we suspected a subjacent abdominal pathology, we performed surgery, and intraoperatively, we observed that the Appendix tip had invaded the abdominal wall.
Discussion
This patient had a challenging diagnostic process and surgical visualization of the appendicular tip invading the abdominal wall was an important characteristic in proving the cause of the abdominal wall abscess.
Conclusion
The onset of an abdominal wall abscess without a known cause needs to be thoroughly investigated, with consideration of a subjacent abdominal cause and appendicitis necessitatis.
1. Introduction
Appendicitis is a prevalent cause of abdominal pain, and the lifetime risk of appendicitis is 7%; worldwide, it more frequently requires a non-trauma emergency procedure. [1], [2], [3] It is a typical disease of young men, with a high incidence in those aged 10–19 years and a low frequency (5–10%) in elderly individuals aged more than 50–60 years. [3], [4]
Diagnosing acute appendicitis can be challenging, as the typical clinical history and signs are not always present in 30–40% of cases. [5] Additionally, making a diagnosis can be more challenging in some groups of patients, including elderly individuals, which contributes to a delayed diagnosis and complicated onset. [3], [5]
Many clinical evaluations, such as the Alvarado score, [5] and further imaging examinations, such as ultrasonography, computed tomography (CT), and magnetic resonance imaging, are used to increase the diagnostic accuracy; however, in some patients, the diagnosis can only be made postoperatively.
We describe the case of an elderly man with an abdominal wall abscess resulting from subjacent abdominal disease and acute appendicitis complicated by an appendicular fistula managed at a community hospital. This case report has been written in line with the SCARE criteria. [6]
2. Presentation of case
An 84-year-old man presented with hypertension, no surgical history, no allergies, and no remarkable family history. He was previously independent in performing activities of daily living. Two months earlier, he started to complain of pain in the thighs, difficulty walking on the right inferior limb, and limitations in activities of daily living. One week earlier, he experienced the onset of painful swelling in the skin of the lower right lateral region of the abdomen.
He was admitted to a general hospital with a wall abscess in the lower right quadrant, and his groin and thigh had spontaneous drainage with foul smelling discharge. An initial abdominal computed tomography (CT) scan showed fluid collection extending from his retroperitoneal space to the subcutaneous layer of the right abdominal wall, without gas or collection in the abdominal cavity. About 1 L of purulent secretion was drained from the abscess.
He has transferred by ambulance to our hospital’s emergency department at night on day 1 with a draining abscess in the right lower abdominal wall; his vital signs were within normal limits, he was afebrile, he had no abdominal pain or tenderness, and he had regular bowel movements. The laboratory evaluation showed an increased total leukocyte count, with a white blood cell count of 17 200/cm3 (reference range, 4500-11 000/cm3), polymorphonuclear cell count of 88% (reference range, 40–80%), hemoglobin level of 6.6 g/dL (reference range, 14–18 g/dL), mean corpuscular volume of 86.4 fL (normocytic), mean corpuscular hemoglobin concentration of 32.4 g/dL (normochromic), creatinine serum level of 0.89 mg/dL with an estimated glomerular filtration rate of 80 mL/min/1.73 m2, serum potassium level of 4.92 mEq/L (reference range, 3.6-5.5 mEq/L), serum sodium level of 126 mEq/L (reference range, 135–145 mEq/L), and serum chloride level of 95 mEq/L (reference range, 94–112 mEq/L). The first management option was to stabilize the patient with intravenous antibiotics starting with ciprofloxacin and metronidazole, electrolyte correction, transfusion of three concentration of erythrocytes and wound care, and to assess him for subjacent abdominal disease with CT Scan.
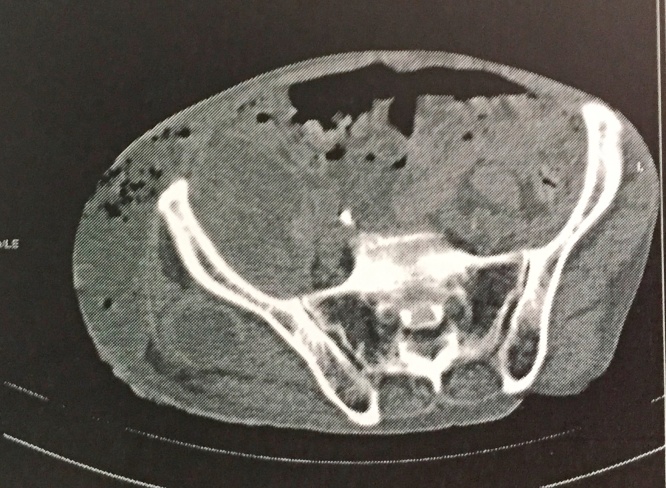
On the second day of hospitalization, after initial stabilization he presented with a fever, low blood pressure, abdominal discomfort, and necrotic wound of the right abdominal wall, groin, and thigh (Fig. 1). An abdominal ultrasonogram showed a mild amount of fluids with echoes in suspension in the abdominal cavity, and the CT scan showed gas and fluid collection extending from his retroperitoneal space to the subcutaneous layer of his right groin and abdominal wall (Fig. 2), without identification of the Appendix or free gas in the perihepatic and perisplenic spaces. Findings of both examinations were suggestive of perforation of the hollow viscera in the abdominal cavity.
Fig. 1.
Photograph showing the large wound with sloughing of the skin in the lateral abdominal and thigh regions.
Fig. 2.
CT-Scan showing gas and fluid collection extending from his retroperitoneal space to the subcutaneous layer of his right groin and abdominal wall, without identification of the appendix.
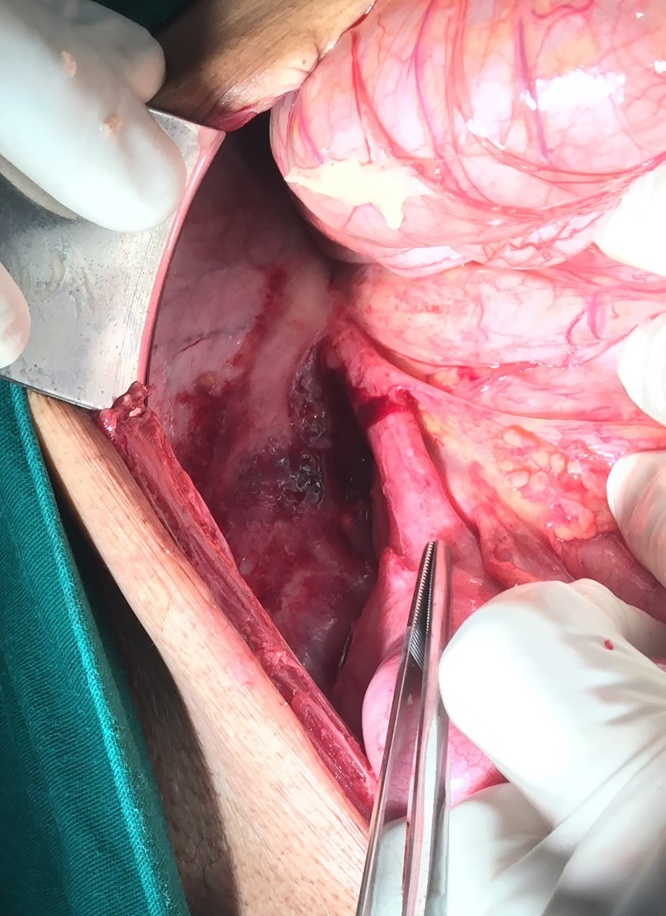
The emergency department was not equipped with a laparoscopic surgery device, and in this case, median infraumbilical laparotomy was mandatory. Intraoperatively, we found the retrocecal Appendix and its tip invaded the posterior lateral abdominal wall in the area of the necrotic wound; the stumps of the Appendix were preserved (Fig. 3), and about 200 mL of abdominal serous fluid was collected with debris. Appendectomy was performed with ligation, transfixation, and inversion of the appendicular stumps, and the tip was excised up to the retroperitoneum and lateral abdominal wall. The peritoneum was closed primarily, and peritoneal toilet was performed. The necrotic wound of the abdominal wall was extensively debrided, and the specimen was sent to the laboratory for a bacterial culture.
Fig. 3.
Photograph showing the tip of the Appendix entering the retroperitoneal space in the region of the necrotic wound in the abdominal wall.
At the end of the surgery, he continued to be hypotensive and required vasoactive drugs, so he was transferred to the intensive care unit, The antibiotics were changed to piperacillin/tazobactam, metronidazole, and vancomycin; the choice of antibiotics was maintained because all the bacterial cultures showed negative findings. On the next day, he developed progressive organ failures and died on the eleventh postoperative day.
3. Discussion
Conventional treatment of appendicitis is surgical excision of the inflamed Appendix as soon as the diagnosis is suspected to prevent perforation. Treatment may vary when the patient presents with complications, and the option is no operative treatment with antibiotics and drainage or an operation. In patients with fistulae on the skin, the tract usually closes spontaneously, and if it remains open, resection of the tract and excision of the appendices are necessary. [7], [9], [10]
In the case of our patient, the medical history was compatible in that he started to complain of right groin pain, which was possibly undiagnosed retrocecal appendicitis, and its natural course includes a loss of appetite and slow progression. After resolution of the acute process, the Appendix tips cause perforation and produce a fistula tract in the abdominal wall with discharge of intestinal content into an abdominal wall abscess, and the fistula tract spontaneously closes. [7], [8], [11]
When he arrived to emergency department, the initial treatment option was not surgical debridement; instead, it was stabilization with blood transfusion during the first night of admission because of acute anemia and possible blood loss after erosion of the abdominal wall, electrolyte reposition, and further investigation for a subjacent abdominal disease. When the CT scan showed free gas and fluid in the abdominal cavity with signs suggestive of a perforated hollow viscera, laparotomy was indicated with extensive debridement of the necrotic wound. Intraoperatively, there was no fistulae tract, and the base of the Appendix was preserved; thus, the surgical team chose to perform appendectomy and excise the appendicular tip invading the abdominal wall. In similar cases when there is an infiltrate, treatment can be challenging, and when a diagnosis is confirmed, the initial management should be a delayed surgical approach after resolution of the initial infection.
This patient had a challenging diagnostic process. Furthermore, analysis of the abdominal CT was difficult because we did not have a trained radiologist in the hospital’s emergency room, so the surgical team always interprets the CT scans; thus, the diagnosis can be delayed. Surgical visualization of the appendicular tip invading the abdominal wall was an important characteristic in proving the cause of the abdominal wall abscess.
4. Conclusion
All patients with unexplained groin and thigh symptoms require a thorough evaluation to exclude intraabdominal disease despite minimal abdominal signs. [7] In the present patient, the complication was the formation of an abscess of the appendices with drainage to the abdominal wall. This condition was named appendicitis necessitatis by Gockel et al. [8]
The onset of an abdominal wall abscess without a known cause requires thorough investigation to exclude abdominal diseases, and appendicitis should be considered.
Conflicts of interest
The authors declare there is no conflict of interest.
Funding
There are no sponsors involved in the study.
Ethical approval
The study received ethical approval from Centro de Pesquisa em Medicina Tropical − Cepem − Rondônia (N 1.832.099), and written informed consent was obtained from the patient’s guardian.
Consent
An informed written consent was obtained from the guardian of the patient. And All details of the patient an in the images attached with the case report has been deleted and patient remains anonymous
Author contributions
Ibrahim Massuqueto Andrade Gomes de Souza operated on the patient; took the photographs; and contributed to the study concept and design, data collection, and editing the manuscript. Diego Antonio De Almeida Nunes operated on the patient; and contributed to the study concept and design, data collection, editing the manuscript, and literature review. Carolina Morandim Granito Massuqueto contributed to editing the manuscript and the literature review. Marcos Alberto de Mendonça Veiga contributed to editing the manuscript. Horacio Tamada contributed to editing the manuscript. All authors have made a significant contribution and approved the final version of the manuscript for publication.
Guarantor
Ibrahim Massuqueto Andrade Gomes de Souza
Division of General Surgery, Hospital de Base, Porto Velho City, Brazil
Avenida Jorge Teixeira 3766, Zip Code: 76821092, Industrial, Porto Velho, RO, Brazil.
Tel.: +55 69 32165446;
fax: +55 69 3216544
Ibrahim_massuqueto@hotmail.com
Acknowledgements
None.
References
- 1.Ibrahim N.A., Oludara M.A., Ajani A., Mustafa I., Balogun R., Idowu O. Non-trauma surgical emergencies in adults: spectrum, challenges and outcome of care. Ann. Med. Surg. 2014;4:325–330. doi: 10.1016/j.amsu.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Addiss D.G., Shaffer N., Fowler B.S., Tauxe R.V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 3.Zbierska K., Kenig J., Lasek A., Rubinkiewicz M., Wałȩga P. Differences in the clinical course of acute appendicitis in the elderly in comparison to younger population. Pol. Prz. Chir. Polish J. Surg. 2016;88:142–146. doi: 10.1515/pjs-2016-0042. [DOI] [PubMed] [Google Scholar]
- 4.Sulu B., Günerhan Y., Palanci Y., Işler B., Çaǧlayan K. Epidemiological and demographic features of appendicitis and influences of several environmental factors. Ulus. Travma ve Acil.Cerrahi Derg. 2010;16:38–42. [PubMed] [Google Scholar]
- 5.Alvarado A. How to improve the clinical diagnosis of acute appendicitis in resource limited settings. World J. Emerg. Surg. 2016;11:16. doi: 10.1186/s13017-016-0071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S. Orgill DP; SCARE group: the SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Singal R., Gupta S., Mittal A., Gupta S., Singh M., Dalal A.K. Appendico-cutaneous fistula presenting as a large wound: a rare phenomenon-brief review. Acta Med. Indones. 2012;44:53–56. [PubMed] [Google Scholar]
- 8.Gockel I., Jäger F., Shah S., Steinmetz C., Junginger T. Appendicitis necessitatis. Der Chir. 2007;78:840–842. doi: 10.1007/s00104-006-1300-6. [DOI] [PubMed] [Google Scholar]
- 9.Tannoury J., Abboud B. Vol. 19. 2013. pp. 3942–3950. (Treatment Options of Inflammatory Appendiceal Masses in Adults). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malhotra P., Sharma D., Kanwar A., Gupta S. Vol. 4. 2015. pp. 1829–1833. (Case Report Appendico-cutaneous Fistula: an Unusual Presentation Appendico-cutaneous Fistula: an Unusual Presentation). [Google Scholar]
- 11.Humes D.J., Simpson J. Acute Appendicitis. 2006;333:530–534. doi: 10.1136/bmj.38940.664363.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]