Abstract
Introduction
Acute decompensated heart failure (ADHF) is the leading causeof hospitalization in older adults. Rehabilitation Therapy in Older Acute Heart Failure Patients (REHAB-HF) trial is a multi-site clinical trial to determine if physical rehabilitation intervention in older patients with ADHF improves physical function and reduces rehospitalizations. The REHAB-HF intervention aims to improve functional performance utilizing reproducible and progressive exercises that are individually tailored to the patient’s physiological and physical capabilities. Fidelity of the intervention is essential to the trial’s integrity and success. Maintaining fidelity is challenged by the complex, multi-domain design of the intervention implemented across multiple sites and delivered to an older, heterogeneous participant pool with severe underlying disease and multi-morbidity.
Methods/Design
Given the dynamic nature of the REHAB-HF intervention, rigorous fidelity strategies were formulated. In this paper we summarize the specific strategies that REHAB-HF is using to meet the National Institutes of Health (NIH) Behavior Change Consortium Treatment Fidelity Workgroup recommendations in 5 key areas: 1) ensuring the intervention dose is consistent across participants, 2) standardizing interventionist training, 3) monitoring intervention delivery, 4) evaluating participants’ understanding of information provided, and 5) ensuring that participants use the skills taught in the intervention.
Discussion
Effective intervention fidelity strategies are essential to the reliability and validity of physical function intervention trials. The REHAB-HF trial has developed comprehensive, specific strategies to ensure intervention fidelity despite a challenging study population and a complex intervention to meet NIH recommendations. This experience provides a strong working model for future physical function intervention trials.
Keywords: Acute Decompensated Heart Failure, Aging, Frailty, Rehabilitation, Fidelity, Exercise
1. Introduction
1Acute decompensated heart failure (ADHF) is the leading cause of hospitalization in older persons [1] and is associated with high rehospitalization rates [2] and mortality [3], costing over $16 billion per year in the United States alone [4]. Mounting evidence, including data from our group, suggest that severe impairments across multiple domains of physical function – strength, balance, mobility, and endurance – strongly contribute to adverse outcomes for older ADHF patients [5, 6]. However, current ADHF management paradigms do not account for or address the marked physical dysfunction. In addition, exercise training trials in HF that have reported results to date (n>17) have either underrepresented or systematically excluded ADHF [7–13]. The multi-site Rehabilitation Therapy in Older Acute Heart Failure Patients (REHAB-HF) trial will test whether a multi-domain structured and progressive physical exercise intervention that addresses deficits in strength, balance, mobility, and endurance will improve physical function and reduce adverse outcomes among older persons experiencing hospitalization for ADHF[14].
Intervention fidelity is crucial to the successful design and implementation of intervention effectiveness studies like REHAB-HF. Standardized and consistent implementation of the intervention by both investigators and participants is imperative not only for replication of the study but also for interpretation of the effects of the intervention, identification of essential features of the intervention, and reduction of random and unintended variability [15–18]. The Treatment Fidelity Workgroup of the National Institutes of Health (NIH) Behavior Change Consortium (BCC) published the results of a multicenter collaborative project designed to identify and evaluate strategies for ensuring that complex interventions are delivered as designed when used in multiple sites and with heterogeneous populations [15]. The Workgroup recommended five areas that should be addressed in the design and implementation of a study to optimize intervention fidelity: 1) ensuring the intervention dose is consistent across participants; 2) standardizing interventionist training, 3) monitoring intervention delivery, 4) evaluating participants’ understanding of information provided, and 5) ensuring that participants use the skills taught in the intervention [15, 19].
The REHAB-HF intervention presents several challenges to maintaining fidelity as it is conducted across several sites and includes exercises across multiple domains of physical function individually tailored for a highly heterogeneous older participant pool with complex disease. This paper summarizes the specific intervention fidelity strategies used in the REHAB-HF trial, illustrates how these are consistent with NIH Workgroup recommendations, and provides a working model for the improvement of scientific findings from physical intervention studies.
2. Methods
2.1 REHAB-HF trial overview
REHAB-HF is the first major clinical trial of a physical rehabilitation intervention for older patients with ADHF, a population characterized by severe physical impairments, heterogeneity in mobility status, multiple co-morbid conditions, and high rates of frailty [6, 14]. The overall trial design details and outcomes of our pilot study have been published previously [14, 20]. In brief, the trial is designed to determine if addressing deficits in balance, mobility, strength and endurance improves physical function and reduces rehospitalizations. REHAB-HF is a multi-site, randomized, controlled, single-blinded trial in 360 older patients (≥ 60 years) with ADHF to test the primary specific hypothesis that the 12-week REHAB-HF intervention will improve physical function as measured by the Short Physical Performance Battery (SPPB). The SPPB is a composite measure of balance, leg strength, and gait speed that is a strong predictor of hospitalization, disability, and death. The secondary aim is to collect clinical outcomes data during follow-up to test the hypothesis that the REHAB-HF intervention group will have a reduced 6-month all-cause rehospitalization rate. The investigators are a multidisciplinary team from three well-established HF clinical research sites: Wake Forest Baptist Health, Thomas Jefferson University, and Duke University. The REHAB-HF trial is being conducted in accordance with the Declaration of Helsinki and has been approved by Institutional Review Boards of all participating institutions. All study participants provide informed written consent. The REHAB-HF trial is registered with Clinicaltrials.gov (NCT02196038).
2.2 REHAB-HF intervention overview
The REHAB-HF multi-domain rehabilitation intervention is a novel application of proven rehabilitation therapies selected and integrated specifically for older patients hospitalized for ADHF. The intervention targets deficits in physical function worsened by acute illness and hospital-associated immobility with an initial emphasis on regaining strength, balance, and functional mobility to then allow for safe participation in rehabilitation more specifically targeting deficiencies related to central and peripheral pathophysiologic effects of HF (i.e., walking-based endurance training and strength training). The goal of the intervention is to increase functional performance across the four physical function domains of strength, balance, mobility, and endurance using reproducible, targeted exercises with specific milestones for progression. The intervention begins during the acute hospitalization and continues for 12 weeks after discharge in the outpatient setting. This transitional intervention is designed to provide the appropriate rehabilitation from the time of acute decompensation, through recovery, and finally to return to chronic, stable disease state.
2.3 REHAB-HF intervention fidelity strategies
Intervention fidelity is the ongoing assessment and monitoring of the reliability and validity of the study. Conclusive statements regarding the effects of intervention cannot be made without detailed attention to intervention fidelity, which increases the confidence that changes in the dependent variable (outcomeof interest) are due to manipulations of the independent variable (believed to have an effect on the dependent variable)[16]. Applying this concept to our trial, implementation of fidelity strategies increases the confidence that changes in outcomes such as the SPPB and rehospitalization result from the REHAB-HF intervention. Given the dynamic nature of the REHAB-HF intervention, rigorous fidelity assessment and implementation strategies were formulated consistent with NIH Treatment Fidelity Workgroup recommendations (Table 1).
Table 1.
Summary of NIH Workgroup Recommendations and REHAB-HF Strategies and Assurance Metrics
| Goal | NIH Workgroup Description | REHAB-HF Strategies | Assurance Metrics |
|---|---|---|---|
| Ensure intervention dose consistent across participants | Ensure that dose is adequately described and is the same for each participant within each condition | Intervention Manual of Procedures Exercise Guide by Level Intervention Fidelity Committee and Site Leads |
Intervention fidelity review (bi-weekly) |
| Standardize interventionist training | Ensure that training is conducted similarly across interventionists and maximize acquisition and maintenance of skills | Interventionist selection criteria Training Manual of Procedures Site-specific training, communication, meetings Study-wide webinars |
Completion of site and study-wide training modules (initially, annually) |
| Monitor intervention delivery | Ensure that intervention is being delivered as intended | Intervention Manual of Procedures Intervention Fidelity Committee and Site Leads Structured field notes and electronic data capture Participant Progress Report |
Intervention fidelity review (bi-weekly) |
| Evaluate participant understanding of the information provided | Ensure participant comprehends information to attend to and perform study-related skills | Participant commitment agreement Comprehension facilitation Attendance facilitation Participant Progress Report |
Completion of agreement (enrollment) Return demonstration of exercises (each session) Intervention fidelity review (bi-weekly) |
| Ensure participant use of skills taught in intervention | Ensure the participant actually uses the skills provided in the intervention in appropriate life settings | Home environment evaluation Home exercise program Maintenance exercise |
Completion of home evaluation (enrollment) Home exercise performance query (each session) |
2.3.1 Recommendation 1 – Ensuring the intervention dose is consistent across participants
To help maximize intervention fidelity, the intervention dose must be the same for each subject within a particular condition and contamination across conditions must be minimized. Intervention dose is constituted by 1) attendance at the intervention sessions and 2) compliance with prescribed exercise parameters for that session; both must be stringently monitored and reported to be able to appropriately interpret the effects of the intervention.
Strategy 1. Intervention Manual of Procedures (MOP)
An essential tool for ensuring that the intervention dose is consistent across participants is the REHAB-HF Intervention MOP (see Supplementary File 1. REHAB-HF Intervention MOP). The Intervention MOP articulates the: 1) theoretical underpinnings of the study; 2) overview of the intervention; 3) specific rehabilitation exercises for each of the four physical function domains; and 4) selection of initial exercises and progression based on standardized assessments. Descriptions of exercise prescription and dosing parameters follow.
Exercise Prescription
Intervention sessions are administered once a day in the hospital and 3 days per week in the outpatient setting. Each session includes 3 stages: 1) warm-up (seated core exercises, light walking, if able, and stretching exercises), 2) rehabilitation/training, and 3) cool-down (stretching). The rehabilitation/training portion includes standard exercises in each of the four physical function domains: strength, balance, mobility, and endurance. To accommodate the heterogeneous capabilities and rehabilitation needs of our participants, the exercises are individualized to each participant based on their functional performance level (1–4, from lowest to highest) using objective criteria as outlined in Table 2 [14].
Table 2.
REHAB-HF Stratification Grid: Performance Levels for Rehabilitation Exercise Prescription
| Level 1 (low function) |
Level 2 (low-moderate function) |
Level 3 (moderate function) |
Level 4 (high function) |
|
|---|---|---|---|---|
| Balance Standing | Unable with feet together for 10 s | Feet together for 10 s | Unsupported and reach forward 10 inches | On 1 leg for 10 s |
| Strength: Lower Extremity Rise from chair without hand support | Unable | A least once | 5 times in > 15 s but < 60 s | 5 times in ≤ 15 s |
| Endurance: Continuous Walking (at usual pace; can use assistive device) | < 2 min | ≥ 2 but < 10 min | ≥ 10 but < 20 min | ≥ 20 min |
| Mobility: Gait Speed (usual pace over 4 meters) | ≤ 0.4 m/s | > 0.4 m/s but ≤ 0.6 m/s | > 0.6 m/s but ≤ 0.8 m/s | > 0.8 m/s |
Reprinted from Rehabilitation Therapy in Older Acute Heart Failure Patients (REHAB-HF) trial: Design and rationale, Am Heart J, Volume 185, Reeves GR et al., Table 3, p.133 © 2017 with permission from Elsevier.
Exercises are then selected to specifically target the participant’s functional level in that domain (see Supplementary File 1. REHAB-HF Intervention MOP, Supplementary File 2. REHAB-HF Exercise Guide by Level, and Supplementary File 3. REHAB-HF Functional Strengthening Quick Reference Guide).
Exercise Duration
During the hospitalization, each session lasts approximately 30 minutes, including warm-up (5 minutes), cool-down (5 minutes), and rest periods as needed. The outpatient sessions lasts for approximately 60 minutes (range 45–75), including 5–10 minutes each for warm-up and cool-down. The relative time spent on each domain during the session is tailored to the participant’s physical function deficits. For instance, a participant with poor balance and functional mobility spends a greater proportion of time performing balance and mobility exercises in the early stages of the intervention. As balance and mobility improve, these comprise a smaller portion of the session and time spent on endurance is increased. Alternatively, a participant with only modest impairments in balance and mobility at baseline spends most of the session performing endurance and strengthening, even in early stages of the intervention (Fig 1) [14].
Fig 1. Levels of performance and time spent in rehabilitation domains.
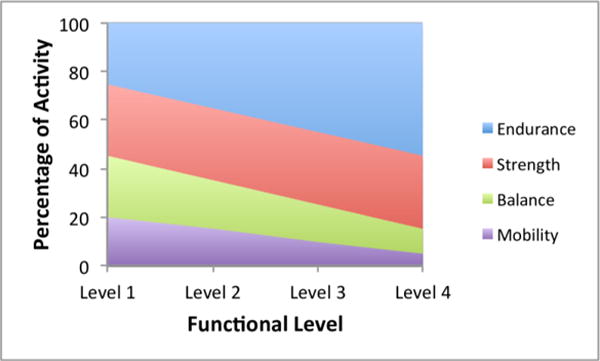
*Reprinted from Rehabilitation Therapy in Older Acute Heart Failure Patients (REHAB-HF) trial: Design and rationale, Am Heart J, Volume 185, Reeves GR et al., Figure 1, p.135 © 2017 with permission from Elsevier.
Time allocation during rehabilitation exercise sessions may be distributed at different levels of functional performance, lowest (Level 1) to highest (Level 4). The exact proportions for any single participant are adjusted based on individual needs and performance in each domain on the REHAB-HF stratification grid. The general trend of increasing the relative portion of endurance training as functional mobility and balance improves is followed for all participants.
Exercise Intensity
For endurance and strengthening rehabilitation, exercise intensity is based on patient-reported rate of perceived exertion (RPE) using the 6–20 point Borg scale [21–24]. While hospitalized, target intensity is low (RPE ≤ 12, light). In the outpatient settings, target intensity is initially low (RPE 11–12) and gradually increases over the first 2 weeks of the intervention. For strengthening rehabilitation, the target RPE progresses to 15–16 (hard), as this level of intensity is likely necessary to obtain significant functional improvements in strength [25, 26]. For endurance, the target RPE progresses to 13 (somewhat hard) with a range of 11–15. After 4 weeks of participation, intensity within the RPE range is adjusted to ensure a heart rate response of at least 20 beats per minute above resting heart rate, as exercise without the guidance of RPE and HR together may likely be below 60% of oxygen uptake reserve. [27]. Using both RPE and heart rate ensures an adequate training effect and minimizes non-responders while maintaining safety [28–30].
Progression
A key aspect of the REHAB-HF intervention is structured, gradual progression using specific small increments in level of difficulty for each domain. Participants are continually challenged to safely and effectively improve physical function by advancing through this progression based on their individual functional performance level. Performance level (Table 2)[14] is reassessed daily in the hospital and at least biweekly in the outpatient setting by a trained physical therapist or exercise physiologist. As function improves, the duration of endurance-based exercise is increased while maintaining the targeted intensity level (Fig 1)[14].
Specific Exercises
Strengthening rehabilitation includes both functional strengthening exercises on the lower extremities (i.e., closed chain sit-to-stand, step-ups, calf/toe raises) and general resistance exercises for major muscle groups of upper and lower extremities (i.e., open chain knee extension, bicep curls). Functional strength exercises are the priority as exemplified in Fig 2 and as noted in Supplementary Files 1 through 3. Open chain exercises can serve as adjunct training for high functioning participants and for those with a temporary restricted weight-bearing status (e.g., musculoskeletal-related pain, foot wound). Balance rehabilitation incorporates static exercises, including progressively narrowing base of support with eyes open or closed, and dynamic exercises, including reaching forward and backward starting within base of support and progressing to outside base of support. Mobility rehabilitation includes dynamic start and stop while walking, changing direction while walking, and episodes of decelerated and accelerated gait. Endurance rehabilitation includes walking as the preferred mode; however, other exercises utilizing equipment (i.e., exercise bicycle) may be incorporated to supplement walking. An example of gradual progression in sit-to-stand functional strengthening exercise is shown in Fig 2.
Fig 2. Functional strengthening progression example.
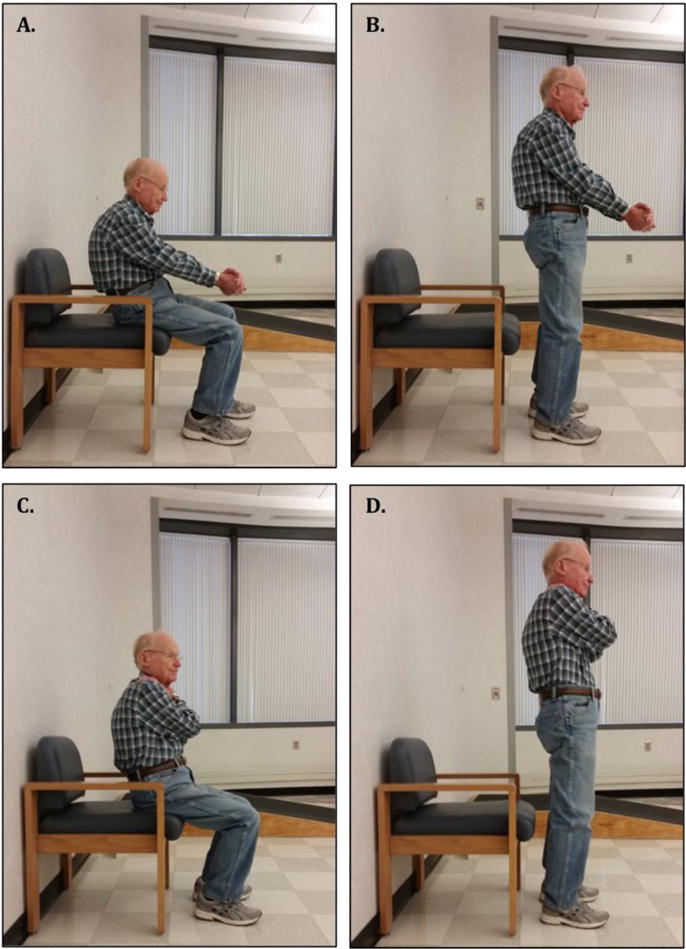
Example of progression in sit-to-stand functional strengthening. Sit-to-stand from chair requires that the participant stand up from a seated position with weight evenly distributed on both lower extremities. At each session, the participant begins at the level completed during the previous session. The participant completes 1 set of 5 repetitions before attempting to complete a 2nd set of repetitions at the next, higher level. For example, at the previous session, a participant was able to perform 5 repetitions at Level 2b, whereby they moved their body to the edge of the chair, leaned forward, put arms out in front, and stood up (Panels A–B). In the current session, the participant performs that same maneuver for the 1st set and then attempts the 2nd set at the next higher difficulty level, Level 2c, whereby their armed are folded across the chest (instead of out in front as in 2b)(Panels C–D). Refer to Supplementary File 3. REHAB-HF Functional Strengthening Quick Reference Guide for difficulty levels.
Strategy 2. Attention Control Group
Participants in attention control receive bi-weekly contact from the study coordinator. The purpose of the average 5- to 10-minute telephone call is to maintain contact, collect information regarding changes in health status, clinical events, and physical activity/exercise, and ensure retention.
2.3.2 Recommendation 2 – Standardizing interventionist training
To ensure that the intervention protocol is administered in the same manner, we developed standardized training procedures. Training is done initially and throughout the study to ensure that providers are satisfactorily trained to deliver the intervention to study participants, to allow for turnover in interventionists, and to limit deviation from the standardized procedures over time [15, 16].
Strategy 1. Selection of interventionists and critical number per site
The Training MOP specifies the criteria for the selection of interventionists and critical number of interventionists per site. Each site has an Intervention Leader who is responsible for overseeing the intervention and interventionists at that site. All interventionists are physical therapists or exercise physiologists experienced in working with frail, elderly patients with chronic disease. At least two interventionists at each site are trained for inpatient and for outpatient intervention delivery to minimize potential gaps in care (i.e., holidays, sick days) and to minimize individual interventionist effects across study participants.
Strategy 2. Training MOP
An essential tool for standardizing training of interventionists is the REHAB-HF Training MOP. The Training MOP details the specific modules required for interventionist training. These include: 1) Slide presentation detailing background, hypothesis, and aims of REHAB-HF, concepts of intervention fidelity and intervention drift, introduction to the REHAB-HF intervention and the Intervention MOP, and case studies illustrating implementation of the intervention; 2) Text files that explain how to complete the structured field notes required to document the intervention sessions or missed visits; 3) Demonstration videos of low, moderate and high functioning patient volunteers participating in exercises for each physical function domain; and 4) Opportunities for role-play simulations to practice administering the exercises.
Strategy 3. On-site training
Prior to study launch, all intervention personnel participated in on-site training sessions conducted by the overall Trial Intervention Leader and the Site Intervention Leader lasting approximately a half-day. After study launch, the Site Intervention Leader is responsible for training interventionists new to the study after study launch.
Strategy 4. Maintenance of provider skills
Interactive study-wide webinars are conducted at least annually to provide refresher training, address concerns, review challenging cases and implement any updates to study protocols that may occur. Site Intervention Leaders perform in-person checks with participants and interventionists during intervention sessions at least monthly, and facilitate discussion with the intervention team via meetings, email, and/or conference calls as needed to discuss intervention protocol and participant cases; specifics are described in the following section.
2.3.3 Recommendation 3 – Monitoring intervention delivery
Monitoring of intervention delivery involves assessment of intervention competency (did interventionists maintain the skill set learned in training), intervention differentiation (did the interventionists only deliver the target treatment and not other treatments), and intervention adherence (were intervention components delivered as intended) [15, 16].
Strategy 1. Intervention MOP
As discussed above in 2.3.1. Recommendation 1, the Intervention MOP provides concrete instructions for administering the intervention.
Strategy 2. Intervention Fidelity Committee (IFC)
The IFC is composed of the Trial Intervention Leaders, including the Principle Investigator and the Chair of the IFC, and Site Intervention Leaders. The IFC holds bi-weekly teleconference calls to evaluate and discuss the delivery and progression of the intervention for each intervention participant at each site. The Site Intervention Leader is then responsible for reviewing with the treating interventionist at their respective site the Participant Progress Report (PPR, discussed below in Strategy 5) and any IFC recommendations. The IFC provides an overall report to the Trial Steering Committee on scheduled monthly Steering Committee teleconference calls. Leadership structure of the IFC is depicted in Fig 3.
Fig 3. Intervention Leadership Structure.
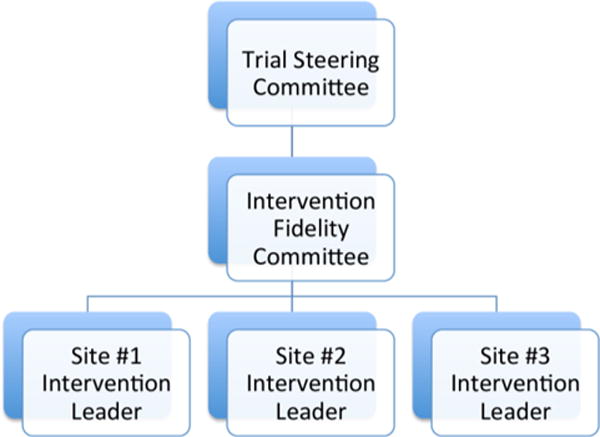
The IFC is composed of the Trial Intervention Leaders and Site Intervention Leaders. The IFC holds a biweekly teleconference call to discuss the progress of each intervention participant at each site. The Site Intervention Leader is then responsible for reviewing the Participant Progress Report and the IFC recommendations with the treating interventionist at their respective site. The IFC provides an overall report to the Trial Steering Committee on scheduled monthly Steering Committee teleconference calls.
Strategy 3. On-site and on-line training
As discussed above in Recommendation 2, study-wide webinars and site-specific visits and communication are conducted to help maintain interventionist skills and adherence to the protocol.
Strategy 4. Structured field notes and electronic database
Exercises performed in each domain (strength, balance, mobility, and endurance) are logged on a structured field note, or what we call the Intervention Log, for each intervention session (see Supplementary File 4. REHAB-HF Intervention Log Example). Specifically, the number of rehabilitation sessions attended, the specific exercises performed in each domain, the RPE achieved and pre- and post-exercise blood pressure, heart rate, and oxygen saturation are recorded. The information on the paper Intervention Log is then entered into a study-wide electronic database, Research Electronic Data Capture (REDCap)[31]. REDCap is a secure web application in a Health Insurance Portability and Accountability Act (HIPAA)-compliant environment that supports online data capture for research studies and operations.
Strategy 5. Participant progress reports (PPR)
Data entered into the database is compiled to generate the PPR. The PPR from each participant actively engaged in the study physical rehabilitation intervention are discussed during bi-weekly teleconferences of the IFC. The Site Intervention Leader then individually reviews the IFC recommendations and implementation of the study intervention for each participant with the treating interventionist. Thus, any challenges or inconsistencies with implementation of the study protocol are promptly addressed. Also, extensions to the intervention period because of intercurrent illness or rehospitalization, as provided for in the protocol, are examined and approved by IFC consensus. See Figs 4 and 5 for PPR examples reflecting consistent progression versus stagnant progression, respectively, in functional performance across sessions.
Fig 4. Patient Progress Report Example #1.
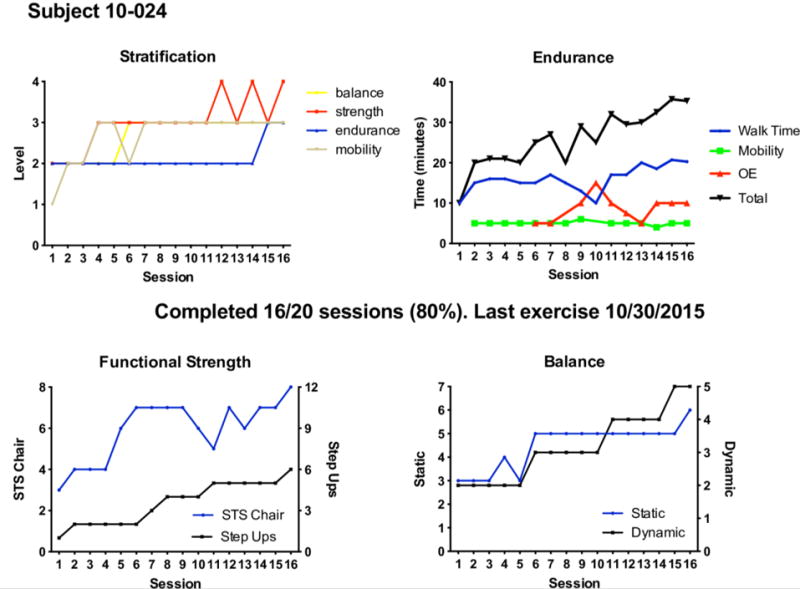
The PPR reflects the attendance and progress of a patient actively engaged in the REHAB-HF intervention. The stratification grid graph (upper left) details progress in functional performance levels (1, lowest to 4, highest, See Table 2) over time. The endurance graph (upper right) provides progress on time spent in walking, other endurance (OE) activity (i.e., stationary bicycle), and mobility activities. The total time (black line) is the summation of all endurance activity time. The functional strength graph (lower left) displays progress in sit-to-stand (STS; x-axis 1 corresponds to exercise Level 1, 8 corresponds to Level 4b in the Intervention MOP) and step-up (x-axis 1 corresponds to exercise Level 1a, 12 corresponds to exercise Level 4c in the Intervention MOP). The balance graph (lower right) shows progress in static balance (x-axis 1 corresponds to exercise Level 1a, 7 corresponds to maintenance in the Intervention MOP) and dynamic balance (x-axis 1 corresponds to exercise Level 1a, 5 corresponds to exercise Level 4 in the Intervention MOP). In this example, the participant attended 16 of a possible 20 sessions (80% attendance) and the last date the participant attended a session is displayed. Overall, the participant is progressing in all domains as noted by the increased time and exercise levels achieved over the sessions. Note that as functional strength and balance improved, so did the capacity for endurance/sustained walking. For descriptions of exercise Levels, see Supplementary File 1. REHAB-HF Study Intervention MOP or Supplementary File 2. REHAB-HF Exercise Guide.
Fig 5. Patient Progress Report Example #2.
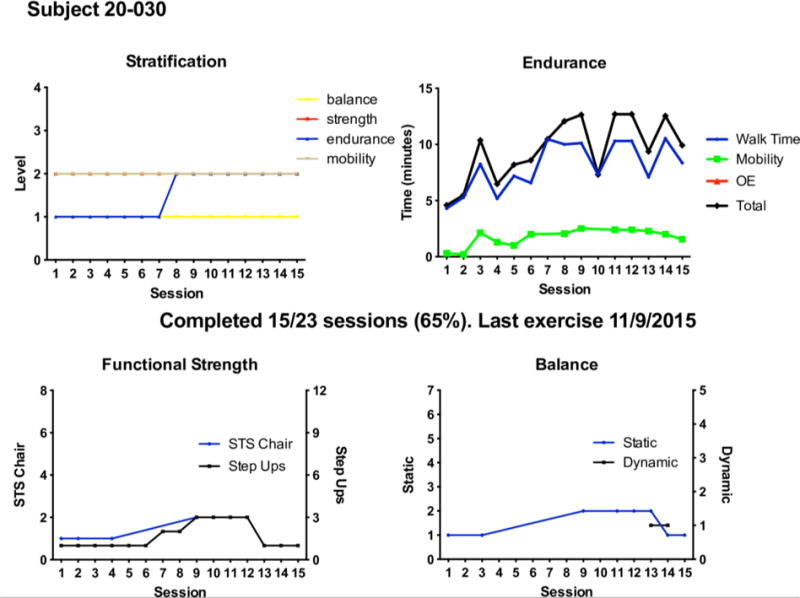
The PPR reflects the attendance and progress of a patient engaged in the REHAB-HF intervention. The stratification grid graph (upper left) details progress in functional performance levels (1, lowest to 4, highest, see Table 2) over time. The endurance graph (upper right) provides progress on time spent in walking, other endurance (OE) activities (i.e., stationary bicycle), and mobility activities. The total time (black line) is the summation of all endurance activity time. The functional strength graph (lower left) displays progress in sit-to-stand (STS; x-axis 1 corresponds to exercise Level 1, 8 corresponds to Level 4b in the Intervention MOP) and step-ups (x-axis 1 corresponds to exercise Level 1a, 12 corresponds to exercise Level 4c in the Intervention MOP). The balance graph (lower right) shows progress in static balance (x-axis 1 corresponds to exercise Level 1a, 7 corresponds to maintenance in the Intervention MOP) and dynamic balance (x-axis 1 corresponds to exercise Level 1a in, 5 corresponds to exercise Level 4 in the Intervention MOP). In this example, the participant attended 15 of a possible 23 sessions (65% attendance) and the last date the participant attended a session is displayed. Overall, the participant demonstrated relatively stagnant progress in all domains as noted by the similar time and exercise levels achieved over the sessions. Upon IFC review, the Site Intervention Lead discussed recommendations for enhancing progress with the interventionist. In this participant, who seemed to be limited by fatigue from endurance (walking) training, IFC recommendations included: the use of assistive device such as a rollator to reduce fatigue during walking; incorporating other endurance activities to supplement limitations in walking; and changing the order of the activities to allow for adequate strength and balance training before endurance training. For descriptions of exercise Levels, see Supplementary File 1. REHAB-HF Study Intervention MOP or Supplementary File 2. REHAB-HF Exercise Guide.
2.3.4 Recommendation 4 – Evaluating participants’ understanding of the information provided
The previous aspects of fidelity focused primarily on the interventionists and how the intervention is delivered and monitored. This particular aspect focuses on the participant’s receipt of the study information, which is demonstrated by his/her ability to attend to and perform the physical rehabilitation exercises [15, 16, 19].
Strategy 1. Participant commitment agreement
At the time of enrollment, a Participant Commitment Agreement (see Supplementary File 5. REHAB-HF Commitment Agreement) is shared with and signed by each participant confirming their understanding of the study requirements and willingness to accept their assigned group.
Strategy 2. Comprehension/performance facilitation
The interventionists are clinicians who have worked extensively with a diverse population of older, frail adults with complex disease. They are skilled in verifying whether the participant comprehends information to appropriately perform the study-related activities and are skilled in the use of evidence-based techniques (i.e., motivational interviewing, shared-decision making, learning style instruction, teach-back methods) that promote comprehension and performance [32–36]. For instance, the interventionists employ return demonstration, a variation of the teach-back technique whereby the participant performs the skill that the interventionist taught, enabling the interventionist to evaluate how well the participant follows the correct steps and performs the exercise.
Strategy 3. Attendance facilitation
The participant receives a clear schedule of all visits, reminders, and same day phone calls for any missed visits to ascertain and discuss the reason for the missed visit. Attendance and reasons for missed visits (see Supplementary File 6. REHAB-HF Missed Visit Form Example) is captured in the REDCap database. Given that transportation was identified as critical to adherence in our pilot study[20], transportation to the intervention sessions is provided for participants who lack access to transportation, do not drive, or are reluctant to drive. Family and/or caregivers identified as supportive by the participant are engaged early in study at recruitment/enrollment and at the home visit. Supportive individuals, especially those for participants with mild cognitive impairment, are encouraged to remind participants of the intervention session schedule and home exercises through a shared calendar. They are also invited to attend and observe the intervention sessions to promote understanding of the intervention and reinforce the importance of consistent attendance.
Strategy 4. PPR
In addition to providing verbal discussion of progress, interventionists share the graphical PPR with the participant on a biweekly basis. Using a shared-decision making model, the interventionist and participant together discuss and devise the plan for moving forward through the intervention [37–40].
2.3.5 Recommendation 5 – Ensuring participants use of skills taught in the intervention
Making use of skills taught in the intervention, also known as enactment, involves assessment, monitoring, and improving the ability of participants to perform intervention-related skills outside the clinic and in relevant life settings [15, 16, 19].
Strategy 1. Home evaluation and exercise
Within a week after hospital discharge, the Site Intervention Lead evaluates the participant’s home environment and proximate environment (presence and condition of sidewalks and streets, presence of nearby parks and community exercise facilities) (See Supplementary File 6. REHAB-HF Home Visit Example) for safe participation in exercises outside the clinic, which we refer to in this study as home exercise. The goals of the environmental evaluation are to establish patient identified goals, prescribe a customized home exercise program based on patient goals and identified functional deficits, identify areas safe for walking and functional strengthening exercises, engage the participant’s caregiver/family to support home exercise, and identify community-based resources in the proximate environment to promote participant’s self-management of and adherence to home exercise and goals. On non-program days (2 days per week) participants are instructed to perform functional strengthening exercises and low intensity walking at their usual pace, gradually increasing toward a goal of 30 minutes of activity. Participants are encouraged to wear a pedometer provided by the program to both motivate and track adherence to the home exercise program. Participant performance of the home exercise program and step counts on the pedometer are documented at every session on the Outpatient Exercise Log.
Strategy 2. Maintenance exercise
Following completion of the outpatient intervention, participants are encouraged to continue with exercise training as part of a self-management maintenance phase. Preparations for this self-management phase begin immediately after randomization and continue throughout the supervised outpatient portion. Preparations for this phase include those already discussed in home exercise and, near the last intervention session, distribution of an individualized exercise prescription developed by the interventionists and approved by the study physician. Participants receive phone calls in this maintenance phase to assess and encourage adherence and revise the prescription as needed.
3. Discussion
Increased use and reporting of intervention fidelity strategies are essential in testing and advancing the reliability and validity of physical intervention research. Given the multiple potential challenges posed in the REHAB-HF trial related to intervention application across a frail and heterogeneous population with severe disease, REHAB-HF is responding to these challenges by comprehensively applying intervention fidelity strategies consistent with NIH recommendations. These strategies allow for improved consistency of intervention application across participants and sites and provide a strong working model for enhancing the causal inferences of future physical intervention studies (Fig 6).
Fig 6. Model of Intervention Fidelity for Physical Intervention Studies.

Intervention fidelity enhances confidence in scientific findings, increases power to detect effects, and facilitates hypothesis testing. The REHAB-HF trial comprehensively applies fidelity strategies consistent with the five NIH-recommended fidelity components and provides a working model for the improvement of scientific findings for physical intervention studies. MOP, Manual of Procedures; PPR, Participant Progress Report.
Despite their significance, intervention fidelity strategies are inconsistently used and reported in clinical trials [16]. This is particularly problematic in physical intervention trials, as results are of little value without precise, comprehensive information about the physical training itself [41–44]. Session attendance, typically as a percentage of total sessions prescribed, is often reported, but data pertaining to the extent to which the participants complied with the prescribed training parameters (i.e., frequency, intensity, duration, type) is inconsistently reported. Attendance and compliance with the prescribed exercise parameters together constitute the “dose” of the intervention to influence the physiological response to exercise training and must be stringently monitored and reported to be able to appropriately interpret the effects of the intervention [43, 44]. To heighten the ability to draw solid conclusions from the trial, the investigators of REHAB-HF rigorously address “dose” through multiple fidelity strategies, including articulation of the exercise protocol in a manual of procedures and exercise guide by functional level, standardized interventionist training, and standardized monitoring and reporting of intervention delivery.
As stated by the NIH Fidelity Workgroup [15], their recommendations are not intended to be a series of rigid steps, but rather a set of guidelines to assist investigators in increasing the likelihood of fairly testing an intervention; flexible adaptation is required within the fidelity components to account for differences in providers and in participants. For instance, training needs to be standardized but also flexibly adapted to cater to different provider learning styles. The REHAB-HF interventionist training uses various learning mediums– text documents, outlines, videos, and role-play simulations. As another example, intervention delivery must take into account different patient types. A primary feature of the REHAB-HF intervention is that the exercises are standardized across the various performance levels yet are individually tailored and gradually progressed in step-wise fashion according to the participant’s functional status and capacity. This is crucial given our highly heterogeneous participant pool who are at high-risk for functional decline and who have to this point been purposely excluded from exercise trials. Additionally, intervention enactment must be tailored to the participant’s environmental and social contexts. REHAB-HF involves a thorough home and proximate environment assessment, a rarity in physical intervention trials, to promote and enhance the performance of intervention-related skills outside the clinic and in the participant’s relevant life settings.
Conversion of structured field notes into graphical PPRs allows for the streamlined visual assessment of functional progression in each physical domain across time. These reports are shared with the interventionists and participants and serve as a platform for fostering shared-decision making among the Fidelity Committee, the interventionist, and the participant. Importantly, the simplistic visual presentation accommodates variations in levels of health literacy among our participant pool. Given its potential value as a pragmatic tool for assessing functional progression in routine rehabilitation care, we are working on developing clinician and patient-friendly applications that can be interwoven in the patient care pathway.
The creation and implementation of our intervention fidelity plan has required extra personnel time and costs. However, we hypothesize that the benefits will outweigh the scientific costs that could result from insufficient attention to fidelity. We believe there is an ethical responsibility to conduct trials such as REHAB-HF in a manner that ensures fair testing of the intervention and that the level of vigilance is essential for the overall scientific and clinical integrity of the trial. We also maintain that the consistent attention to fidelity can be a source of professional growth and development for the interventionists.
In summary, the REHAB-HF trial uses innovative methods to support intervention fidelity, which are consistent with NIH Workgroup recommendations. Intervention fidelity necessitates the considerate application of strategies that balance rigorous study design with clinical practice realities. Doing so serves to protect the reliability and validity of the trial, enhancing the causal inferences of the intervention, and facilitates future application of the intervention in routine clinical practice. We have presented REHAB-HF as a strong working model for application of fidelity strategies in physical intervention research.
Supplementary Material
Acknowledgments
Funding
This paper was supported by National Institute on Aging (www.nia.nih.gov/) R01AG045551 (All Authors), R01AG018915 (DWK), P30AG021332 (DWK), P30AG028716 (AMP) and National Heart, Lung and Blood Institute (www.nhlbi.nih.gov) U10HL110312 (RJM). The funding agencies played no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations
ADHF, Acute Decompensated Heart Failure; BCC, Behavior Change Consortium; HF, Heart Failure; IFC, Intervention Fidelity Committee; NIH, National Institutes of Health; PPR, Participant Progress Report; SPPB, Short Physical Performance Battery; REHAB-HF, Rehabilitation Therapy in Older Acute Heart Failure Patients; RPE, Rate of Perceived Exertion
Competing interests
The authors have none to declare.
References
- 1.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, Hospitalizations, and Expenditures for the Medicare Population Aged 65 Years or Older, 1999–2013. JAMA. 2015;314(4):355–65. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bueno H, Ross JS, Wang Y, Chen J, Vidan MT, Normand SL, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303(21):2141–7. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng RK, Cox M, Neely ML, Heidenreich PA, Bhatt DL, Eapen ZJ, et al. Outcomes in patients with heart failure with preserved, borderline, and reduced ejection fraction in the Medicare population. Am Heart J. 2014;168(5):721–30. doi: 10.1016/j.ahj.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murad K, Kitzman DW. Frailty and multiple comorbidities in the elderly patient with heart failure: implications for management. Heart Fail Rev. 2012;17(4–5):581–8. doi: 10.1007/s10741-011-9258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reeves GR, Whellan DJ, Patel MJ, O’Connor CM, Duncan P, Eggebeen JD, et al. Comparison of Frequency of Frailty and Severely Impaired Physical Function in Patients >/=60 Years Hospitalized With Acute Decompensated Heart Failure Versus Chronic Stable Heart Failure With Reduced and Preserved Left Ventricular Ejection Fraction. Am J Cardiol. 2016;117(12):1953–8. doi: 10.1016/j.amjcard.2016.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kitzman DW, Rich MW. Age disparities in heart failure research. JAMA. 2010;304(17):1950–1. doi: 10.1001/jama.2010.1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitzman DW. Outcomes in patients with heart failure with preserved ejection fraction: it is more than the heart. J Am Coll Cardiol. 2012;59(11):1006–7. doi: 10.1016/j.jacc.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Scrutinio D, Passantino A, Ricci VA, Catanzaro R. Association between conformity with performance measures and 1-year postdischarge survival in patients with acute decompensated heart failure. Am J Med Qual. 2013;28(2):160–8. doi: 10.1177/1062860612451049. [DOI] [PubMed] [Google Scholar]
- 10.McKelvie RS, Teo KK, Roberts R, McCartney N, Humen D, Montague T, et al. Effects of exercise training in patients with heart failure: the Exercise Rehabilitation Trial (EXERT) Am Heart J. 2002;144(1):23–30. doi: 10.1067/mhj.2002.123310. [DOI] [PubMed] [Google Scholar]
- 11.Davies EJ, Moxham T, Rees K, Singh S, Coats AJ, Ebrahim S, et al. Exercise trainingfor systolic heart failure: Cochrane systematic review and meta-analysis. Eur J Heart Fail. 2010;12(7):706–15. doi: 10.1093/eurjhf/hfq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piepoli MF, Davos C, Francis DP, Coats AJ, ExTra MC. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH) BMJ. 2004;328(7433):189. doi: 10.1136/bmj.37938.645220.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whellan DJ, O’Connor CM, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Heart failure and a controlled trial investigating outcomes of exercise training (HF-ACTION): design and rationale. Am Heart J. 2007;153(2):201–11. doi: 10.1016/j.ahj.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Reeves GR, W D, Duncan P, O’Conner CM, Pastva AM, Eggebeen JD, Hewston LA, Morgan TM, Reed SD, Mentz RJ, Rosenberg PB, Kitzman D. Rehabilitation Therapy in Older Acute Heart Failure Patients (REHAB-HF) trial: Design and rationale. Am Heart J. 2017;185(0):130–9. doi: 10.1016/j.ahj.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–51. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 16.Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Czajkowski S, Breger R, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol. 2005;73(5):852–60. doi: 10.1037/0022-006X.73.5.852. [DOI] [PubMed] [Google Scholar]
- 17.Resnick B, Bellg AJ, Borrelli B, Defrancesco C, Breger R, Hecht J, et al. Examples of implementation and evaluation of treatment fidelity in the BCC studies: where we are and where we need to go. Ann Behav Med. 2005;29(Suppl):46–54. doi: 10.1207/s15324796abm2902s_8. [DOI] [PubMed] [Google Scholar]
- 18.Robb SL, Burns DS, Docherty SL, Haase JE. Ensuring treatment fidelity in a multi-site behavioral intervention study: implementing NIH Behavior Change Consortium recommendations in the SMART trial. Psychooncology. 2011;20(11):1193–201. doi: 10.1002/pon.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horner SD. Best practices for improving intervention fidelity that every nurse should know. J Spec Pediatr Nurs. 2012;17(2):171–4. doi: 10.1111/j.1744-6155.2012.00327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reeves GR, W D, O’Conner CM, Duncan P, Eggebeen JD, Morgan TM, Hewston LA, Pastva AM, Patel MJ, Kitzman D. A novel rehabilitation intervention for older patients with acute decompensated heart failure: The REHAB-HF Pilot Study. JACC Heart Fail. 2017 May;5(5):359–366. doi: 10.1016/j.jchf.2016.12.019. Epub 8 March 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2(2):92–8. [PubMed] [Google Scholar]
- 22.Borg G. Borg’s Perceived Exertion and Pain Scales. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 23.Perceived Exertion (Borg Rating of Perceived Exertion Scale) Centers for Disease Control and Prevention; website; [updated updated August 11, 2015; cited 2017 October 4]. https://www.cdc.gov/physicalactivity/basics/measuring/exertion.htm. [Google Scholar]
- 24.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. [PubMed] [Google Scholar]
- 25.Investigators LS. Pahor M, Blair SN, Espeland M, Fielding R, Gill TM, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157–65. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 26.Rejeski WJ, Marsh AP, Chmelo E, Prescott AJ, Dobrosielski M, Walkup MP, et al. The Lifestyle Interventions and Independence for Elders Pilot (LIFE-P): 2-year follow-up. J Gerontol A Biol Sci Med Sci. 2009;64(4):462–7. doi: 10.1093/gerona/gln041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joo KC, Brubaker PH, MacDougall A, Saikin AM, Ross JH, Whaley MH. Exercise prescription using resting heart rate plus 20 or perceived exertion in cardiac rehabilitation. J Cardiopulm Rehabil. 2004;24(3):178–84. 85–6. doi: 10.1097/00008483-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 28.O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–50. doi: 10.1001/jama.2009.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brubaker PH, Moore JB, Stewart KP, Wesley DJ, Kitzman DW. Endurance exercise training in older patients with heart failure: results from a randomized, controlled, single-blind trial. J Am Geriatr Soc. 2009;57(11):1982–9. doi: 10.1111/j.1532-5415.2009.02499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Savage PD, Antkowiak M, Ades PA. Failure to improve cardiopulmonary fitness in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2009;29(5):284–91. 92–3. doi: 10.1097/HCR.0b013e3181b4c8bd. [DOI] [PubMed] [Google Scholar]
- 31.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stonerock GL, Blumenthal JA. Role of Counseling to Promote Adherence in Healthy Lifestyle Medicine: Strategies to Improve Exercise Adherence and Enhance Physical Activity. Prog Cardiovasc Dis. 2016 doi: 10.1016/j.pcad.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: A systematic review. Patient Educ Couns. 2017;100(1):65–75. doi: 10.1016/j.pec.2016.07.030. [DOI] [PubMed] [Google Scholar]
- 34.Stromberg A. The crucial role of patient education in heart failure. Eur J Heart Fail. 2005;7(3):363–9. doi: 10.1016/j.ejheart.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Paul S. Hospital discharge education for patients with heart failure: what really works and what is the evidence? Crit Care Nurse. 2008;28(2):66–82. [PubMed] [Google Scholar]
- 36.Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database System Rev Implement Rep. 2016;14(1):210–47. doi: 10.11124/jbisrir-2016-2296. [DOI] [PubMed] [Google Scholar]
- 37.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651–61. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 38.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44(5):681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 39.Dierckx K, Deveugele M, Roosen P, Devisch I. Implementation of shared decision making in physical therapy: observed level of involvement and patient preference. Phys Ther. 2013;93(10):1321–30. doi: 10.2522/ptj.20120286. [DOI] [PubMed] [Google Scholar]
- 40.Lal S, Korner-Bitensky N. Motivational interviewing: a novel intervention for translating rehabilitation research into practice. Disabil Rehabil. 2013;35(11):919–23. doi: 10.3109/09638288.2012.711897. [DOI] [PubMed] [Google Scholar]
- 41.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 42.Mujika I. The alphabet of sport science research starts with Q. Int J Sports Physiol Perform. 2013;8(5):465–6. doi: 10.1123/ijspp.8.5.465. [DOI] [PubMed] [Google Scholar]
- 43.Taylor KL, Weston M, Batterham AM. Evaluating intervention fidelity: an example from a high-intensity interval training study. PLoS One. 2015;10(4):e0125166. doi: 10.1371/journal.pone.0125166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Conraads VM, Deaton C, Piotrowicz E, Santaularia N, Tierney S, Piepoli MF, et al. Adherence of heart failure patients to exercise: barriers and possible solutions: a position statement of the Study Group on Exercise Training in Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2012;14(5):451–8. doi: 10.1093/eurjhf/hfs048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


