Abstract
This study examined whether cognitive functioning was related to treatment outcomes in persons with severe mental illness who received a cognitive behavioral therapy (CBT) program for co-occurring posttraumatic stress disorder (PTSD). The study sample was drawn from a larger controlled trial of 108 persons with severe mental illness and PTSD comparing the effects of CBT with treatment as usual on PTSD and related outcomes, with assessments conducted at baseline, post-treatment, and 3- and 6-month follow-ups. Among the 54 persons in CBT, 49 were administered a neuropsychological battery at baseline and 40 were exposed to the CBT program. Statistical analyses of these 40 participants were conducted to evaluate whether cognitive functioning was related to participation in the CBT program, completion of homework assignments, and improvements in PTSD, and other outcomes. Cognitive functioning was not related to participation in CBT or completion of homework. Lower cognitive functioning predicted less learning of information about PTSD at post-treatment and follow-up, but not less clinical benefit from CBT in PTSD diagnosis or symptoms, other symptoms, or health. The results suggest that cognitive impairment does not attenuate response to the CBT for PTSD program in persons with severe mental illness. Clinical Trials.gov Identifier: NCT00053690
1. Introduction
Psychologically traumatic events such as physical and sexual abuse/assault, witnessing violence, and the sudden and unexpected death of a loved one are common in persons with psychotic and other severe mental illnesses, both before and following onset of the disorder (Khalifeh et al., 2015; Roy et al., 2014). Trauma exposure in this population is associated with worse psychiatric and other symptoms, higher levels of substance abuse, worse psychosocial functioning, and greater use of acute treatment services (Bebbington et al., 2004; Goodman et al., 2001; Ng et al., 2016). As would be expected from the high rates of trauma in persons with severe mental illness, high rates of posttraumatic stress disorder (PTSD) have also been documented (Grubaugh et al., 2011; Mueser et al., 2004). PTSD has been hypothesized to mediate the association between trauma exposure and worse outcomes in people with severe mental illness (Cusack et al., 2013; Mueser et al., 2002; Subica et al., 2011). To address this problem, recent efforts have focused on developing or adapting treatments for PTSD designed to accommodate the special challenges of this population, such as lack of social support, psychotic symptoms, cognitive impairment, severe depression, and suicidal ideation (Mueser et al., 2004; Rosenberg et al., 2001).
In the general population, there is strong evidence for the effectiveness of three psychotherapeutic approaches to the treatment of PTSD, including prolonged exposure, cognitive restructuring (also referred to as cognitive processing therapy, cognitive therapy, and cognitive behavioral therapy), and eye movement desensitization and reprocessing (EMDR) therapy (Ehring et al., 2014; Watts et al., 2013). Several randomized controlled trials have established the feasibility and evaluated the effectiveness of adaptations of these interventions for PTSD in persons with severe mental illness. One randomized controlled trial from the Netherlands showed that 8 weekly sessions of prolonged exposure or EMDR were more effective than usual services at reducing PTSD symptoms and diagnoses in 155 persons with a psychotic disorder, with effects maintained at 6 months follow-up (Van den Berg et al., 2015).
Three randomized controlled trials have evaluated the CBT program for PTSD in persons with severe mental illness, a 12–16 session individual therapy approach that includes psychoeducation about PTSD, breathing retraining, and cognitive restructuring to address trauma-related beliefs (Mueser et al., 2009). The first randomized controlled trial was conducted in a rural area in northeastern U.S. with 108 persons with serious mental illness and severe PTSD, and found that the CBT program more effective than usual services at improving PTSD and depression, with effects maintained three and six months later (Mueser et al., 2008). The second randomized controlled trial was conducted in an urban area in eastern U.S. with 201 persons with serious mental illness and severe PTSD, and compared the CBT program with a brief (three session) program that included just the psychoeducational and breathing retraining components of the full program (Mueser et al., 2015). The CBT program was found to be more effective at improving PTSD outcomes and overall functioning than the brief program, with effects maintained six and 12 months later. A third randomized controlled trial from the United Kingdom comparing the CBT program with usual services in 61 individuals with schizophrenia and PTSD reported significant but comparable reductions in PTSD and other symptoms for both groups at the six month post-treatment assessment and 12-month follow-up (Steel et al., 2017). However, participants in this study had significant less severe PTSD symptoms than those in the two U.S. studies of the CBT program.
The evidence supporting the effectiveness of the CBT program for PTSD in persons with severe mental illness raises the question of whether it is more effective for some clients than others. Cognitive functioning is of particular interest as a potential moderator of treatment effectiveness. Compared to health controls, significantly greater grey matter loss in the anterior insula/dorsal anterior cingulate-based network thought to reflect impaired executive functions has been reported across a diverse range of diagnostic groups (schizophrenia, bipolar disorder, depression, addiction, obsessive-compulsive disorder, and anxiety) and has been hypothesized to reflect a shared neurobiologic substrate to mental illness (Goodkind et al., 2015; McTeague et al., 2017). Cognitive impairment is a common, stable feature of schizophrenia (Harvey, 2013; Heaton et al., 2001) that shows only modest associations with symptoms (Hughes et al., 2003; Dominguez et al., 2009; Rund et al., 2004; Ventura et al., 2010). Two meta-analyses of the research literature on cognitive functioning in schizophrenia conducted 1990–2006 (Dickenson et al., 2007) and 2006–2013 (Schafer et al., 2013) reported remarkably similar findings, with large mean effect sizes across all cognitive tests of g = −0.98 and −1.03, respectively, and the worst performance on digit symbol coding, g = −1.57 and −1.55, respectively. Although severity of cognitive impairment is greater in schizophrenia than bipolar disorder (Bortolato et al., 2015; Depp et al., 2012), reduced cognitive functioning is often present in bipolar disorder (Dickerson et al., 2004), and meta-analyses have found lower cognitive performance in persons with bipolar disorder I compared to healthy controls (Bostock et al., 2017; Torres et al., 2007). Reduced cognitive functioning has also been proposed to reflect a stable marker of major depression (Bortolato et al., 2014; Murrough et al., 2011). A meta-analysis by Ahern and Samkovska (2017) reported that persons with a first episode of major depression demonstrated significant cognitive impairments compared to healthy controls, with remission associated with small improvements in processing speed and shifting but persistent impairment in inhibition and verbal fluency. Meta-analyses of more heterogeneous samples of persons with major depression on the other hand show moderate deficits across the range of cognitive domains (Porter et al., 2015).
Reduced cognitive functioning is also predictive of a greater likelihood of developing PTSD or more severe PTSD symptoms following exposure to a traumatic event (Breslau et al., 2006; McNally and Shin, 1995; Yurgil et al., 2014), and is a common clinical feature associated with the disorder (Golier and Yehuda, 2002; Woon et al., 2010). People with severe mental illness who have lower levels of cognitive functioning benefit less from psychosocial interventions (Kurtz, 2011) such as social skills training (Kern et al., 1992; Mueser et al., 1991) and supported employment (McGurk et al., 2003). However, research has not examined whether cognitive functioning is predictive of attenuated benefit from cognitive behavioral interventions for PTSD, including the CBT program. The present study addresses this question.
2. Methods
This study reports on previously unreported data from a randomized controlled trial of the CBT program (Mueser et al., 2008). While main study results have been reported previously (Mueser et al., 2008), data on cognitive functioning as related to treatment participation and outcomes have not yet been reported. All of the study procedures were approved by the Rutgers and Dartmouth IRBs. The study took place at four publicly funded community mental health centers in the northeastern U.S. (New Hampshire and Vermont) and compared the effectiveness of the CBT program to treatment as usual for improving PTSD and other psychiatric symptoms in 108 persons with serious mental illness, with assessments conducted at post-treatment and 3-and 6-month follow-ups.
Intent-to-treat statistical analyses indicated that participants in the CBT program improved significantly more in PTSD symptoms and diagnosis, knowledge of PTSD, trauma-related cognitions, depression, and anxiety at post-treatment than those in treatment as usual, with treatment gains maintained at the follow-up assessments. Furthermore, reductions in PTSD symptoms in participants who received the CBT program were mediated by decreases in trauma-related cognitions. Finally, participants with higher rates of homework completion improved more in PTSD and other symptoms than those with lower rates of homework completion. The study methods and results have been previously reported (Mueser et al., 2008).
At the baseline assessment participants who were randomized to the CBT program (but not those in treatment as usual) were also administered a neuropsychological battery to assess cognitive functioning. The present report examined the relationship between cognitive functioning at baseline and response to the CBT program at post-treatment and follow-up. These cognitive data have not been previously reported.
2.1 Participants
Inclusion criteria for study participants were: 1) minimum 18 years old; 2) meets States of New Hampshire or Vermont definition of severe mental illness as defined by DSM-IV (American Psychiatric Association, 1994) and persistent impairment in work, school, or ability to care for oneself; 3) DSM-IV diagnosis of schizophrenia, schizoaffective disorder, major depression, or bipolar disorder, based on the Structured Clinical Interview for DSM-IV (First et al., 1996); 4) current DSM-IV diagnosis of PTSD, based on the Clinician Administered PTSD Scale (CAPS), schizophrenia version (Blake et al., 1995; Gearon, et al., 2004); and 5) interested in receiving treatment for PTSD and legally able to and willing to provide informed consent to participate in the study. Exclusion criteria were: 1) hospitalization or suicide attempt in the past three months, and 2) substance dependence within the past three months. Individuals with a DSM-IV diagnosis of borderline personality disorder, based on the SCID-II (First et al., 1994), were included if they met the other criteria to participate in the study.
A total of 54 participants were randomized to the CBT program, of whom 49 (91%) completed the neurocognitive evaluation. The demographic and clinical characteristics of the participants who received the neurocognitive assessment at baseline are summarized in Table 1. The average age of the participants was in the mid 40s, with approximately three-quarters being women, 82% had a major mood disorder and 18% had a schizophrenia-spectrum disorder, and 67% had borderline personality disorder.
Table 1.
Demographic and Clinical Characteristics of Study Participants
| Categorical variables | N | % |
|---|---|---|
| Gender | ||
| Male | 13 | 26.5% |
| Female | 36 | 73.5% |
| Race | ||
| White | 43 | 87.8.% |
| Other | 6 | 12.2% |
| Marital Status | ||
| Never Married | 15 | 30.6% |
| Ever Married | 34 | 69.4% |
| Highest Level of Education | ||
| Some elementary school | 1 | 2.0% |
| Completed 8th grade | 4 | 8.2% |
| Some high school | 7 | 14.3% |
| Completed high school or GED | 19 | 38.8% |
| Some college or technical school | 10 | 20.4% |
| Completed associates degree | 2 | 4.1% |
| Completed bachelors degree | 6 | 12.2% |
| Current Employment Status | ||
| Not employed | 46 | 93.9% |
| Employed | 3 | 6.1% |
| Psychiatric Diagnosis | ||
| Major depression | 26 | 53.1% |
| Bipolar disorder | 14 | 28.6% |
| Schizophrenia | 5 | 10.2% |
| Schizoaffective disorder | 4 | 8.1% |
| Borderline Personality Disorder | ||
| Absent | 36 | 73.5% |
| Present | 13 | 26.5% |
| Lifetime Substance Use Disorder | ||
| Absent | 34 | 70.8% |
| Present | 14 | 29.2% |
| Continuous Variables | Mean | SD |
| Age | 44.04 | 10.07 |
| Lifetime psychiatric hospitalizations | 12.48 | 22.51 |
| Months since last hospitalization | 38.10 | 56.30 |
| Age at first hospitalization | 28.56 | 12.46 |
2.2. Assessment instruments
Clinical interviews and self-report measures of PTSD and other psychiatric diagnoses and symptoms, knowledge of PTSD, and trauma-related cognitions were administered at baseline, post-treatment, and 3 and 6 months post-treatment, except where noted. The neurocognitive battery was administered at baseline only
2.2.1. Screening
Potential study participants were identified by administering self-report screening instruments, including a 16-item abbreviated version of the Traumatic Life Events Questionnaire (Kubany et al., 2000), followed by the PTSD Checklist (PCL) based on the most upsetting traumatic event, with a total score of > 45 on the PCL used to indicate probable PTSD (Blanchard et al., 1996).
2.2.2. Interview-based assessments
PTSD severity and diagnosis were assessed with the CAPS-Schizophrenia version (Blake et al., 1995; Gearon et al., 2004). Psychiatric symptoms were assessed with the Brief Psychiatric Rating Scale-Expanded Version (BPRS; Lukoff et al., 1986).
2.2.3. Self-report measures
Knowledge of PTSD was assessed with the PTSD Knowledge Test (Pratt et al., 2005), which contains 15 multiple choice questions about PTSD that are covered in the psychoeducational sessions of the CBT program. The Posttraumatic Cognitions Inventory (PTCI; Foa et al., 1999) was used to assess trauma-related cognitions. The PTCI contains 36 items pertaining to common negative beliefs about oneself, other people, and the world that are often related to traumatic experiences. Each item is a statement, which the respondent indicates his or her degree of belief in (e.g., “I am a weak person,”).
Depression and anxiety severity were evaluated with the Beck Depression Inventory-II (BDI; Beck et al., 1996) and the Beck Anxiety Inventory (BAI; Beck and Steer, 1993), respectively. Self-reported mental health and physical functioning were assessed with the Short Form-12 (Ware et al., 1994).
2.2.4. Neurocognitive battery
Because of the length and overall demands of the assessment on subjects with multiple stresses and handicaps, we sought to keep the battery as short as possible while yielding valid and reliable indices of cognitive capacities in key spheres related to treatment participation. The battery was designed to assess cognition across a broad range of domains, including attention, information processing speed, verbal learning and memory, and executive functions based on widely used, standardized neuropsychological measures. Working memory was assessed with the Digit Span Forward and Backward (total correct, per condition: Total Digits) from the Wechsler Adult Intelligence Scale-Revised (WAIS-R; Wechsler, 1998). Information processing speed was evaluated with the Digit Symbol Substitution Test (DSST) from the WAIS-R (Total Correct). The California Verbal Learning Test (CVLT; Delis et al., 2000) was used to assess verbal learning and memory (Total Correct Trials 1–5 and Total Correct Delayed Recall). The Wisconsin Card Sorting Test (WCST; Berg, 1948) was employed to assess executive functions (Number of Categories Obtained, Percent of Perseverative Errors). An overall composite measure of cognitive functioning was computed by standardizing each of the cognitive measures (i.e., computing z-scores) and summing the scores.
2.3. Treatments
All study participants continued to receive their usual psychiatric services following randomization to the CBT program. These services included continued pharmacological treatment, case management, supportive counseling, and access to psychiatric rehabilitation programs such as vocational rehabilitation. No efforts were made to modify any of the services provided to study participants.
2.3.1. Cognitive behavioral therapy (CBT) program
The CBT program is a 12–16 session intervention for PTSD, with individual sessions following a structured format and including handouts, worksheets, and homework assignments (Mueser et al., 2009). The first three sessions include instruction in breathing retraining, a self-management strategy for reducing anxiety (Foa and Rothbaum, 1998) and education about trauma and PTSD. The remaining 9–13 sessions focus on teaching cognitive restructuring as a skill for coping with negative emotions. Participants initially learn how to use cognitive restructuring to address and modify inaccurate thoughts and beliefs related to any negative feeling they are experiencing. As the participant becomes more adept at cognitive restructuring, the focus shifts towards using the skill to examine and change inaccurate trauma-related thoughts and beliefs that underlie PTSD symptoms. Participation in the CBT program was defined a priori as completion of at least six sessions (Rosenberg et al., 2004).
All sessions were conducted at participants’ local community mental health center, with regular contact and coordination between the therapist and the treatment teams providing comprehensive mental health treatment. The therapy was provided by six Ph.D. level clinicians and one Masters level clinician. Weekly supervision was provided.
2.4. Statistical analysis
First, we examined performance on the neurocognitive battery and computed coefficient alpha to evaluate the extent to which performance on the different cognitive tests was inter-correlated. Second, we evaluated exposure to the CBT program for the study participants who had completed the neurocognitive battery. Third, we conducted t-tests or χ2 analyses to compare participants who were “exposed” to the CBT program (completed > 6 sessions) to those who were not exposed to the program on demographics, baseline clinical functioning, and performance on the neurocognitive battery. Fourth, we evaluated whether cognitive functioning was related to follow-through on homework assignments by computing Pearson correlations between the baseline cognitive composite scores and the percentage of homework assignments completed for participants who were exposed to the CBT program.
Fifth, to evaluate whether cognitive functioning at baseline predicted response to the CBT program, we conducted covariance pattern models within general mixed-effects linear regression models framework for the continuous outcome variables (Hedeker and Gibbons, 2006). For these models, the post-treatment and 3- and 6 month follow-up scores of each outcome were the repeated dependent variables, and the predictor variables were the baseline level of each outcome variable, cognitive functioning (composite score), education level, primary psychiatric diagnosis, time, and the cognition by time interaction. For the binary outcome variable of PTSD diagnosis we conducted a similar mixed-effects logistic regression analysis, excluding baseline PTSD diagnosis as a predictor because all participants had PTSD at baseline. The main effect for cognition in these analyses is a test of whether participants with lower levels of cognitive functioning improved less after completing the CBT program and at the follow-up assessments than participants with more intact cognitive functioning. The effect for the cognition by time interaction is a test of whether cognitive impairment at baseline predicted less improvement at some subsequent assessments than others (e.g., post-treatment vs. 3- or 6-month follow-up). Preliminary analyses indicated that the cognition by time interaction was not significant for any outcome variables, and therefore this term was dropped from the analyses.
Last, to explore whether cognitive performance on the individual cognitive tests predicted improvement in PTSD, we conducted similar mixed-effects linear (or logistic) regression models to those described above on two PTSD outcomes: PTSD symptom severity and PTSD diagnosis. We elected to conduct these analyses on only the two primary outcome variables to minimize the increased risk of committing Type I errors (i.e., rejecting the null hypothesis of no difference between groups when the null hypothesis is correct) when performing multiple statistical tests. We fit separate regression models predicting PTSD severity or diagnosis at post-treatment and the follow-ups from each of the following cognitive test scores: Digits Total on Digit Span, Total Correct on the DSST, CVLT Total Correct Trials 1–5, CVLT Total Correct Delayed Recall, WCST Total Categories Obtained, and WCST Percent Perseverative Errors. For each regression model, in addition to including the cognitive test score as a predictor, education level, diagnosis, and time were also included as predictors, as well as the cognition by time interaction. For the linear regression models predicting PTSD symptom severity, PTSD severity at baseline was also included as a predictor. As in the preliminary analyses of the cognitive composite scores described above, the cognition by time interaction was not significant for any of the individual cognitive tests for any of the outcome measures, and was dropped from the final analyses. For these analyses, a significant effect for a cognitive test score indicates that cognitive performance at baseline on that test was a significant predictor of PTSD at post-treatment and follow-up after controlling baseline PTSD, education level, and diagnosis.
3. Results
Participants’ performance on the individual tests in neurocognitive battery is summarized in Table 2. We used a psychometric conversion table to determine T scores from WAIS scaled scores (Brock, 2017). We employed conventional clinical descriptors of cognitive test performance (Mejía-Arango et al., 2015) to indicate the level of cognitive functioning in the Table (e.g., low average = 1–1.5 SDs below average; mildly impaired = 1.5–2 SDs below average; moderately impaired = 2–3 SDs below average). We used clinical descriptors associated WAIS performance (e.g., average is 25% below the mean to 75% above mean) to determine level of impairment.
Table 2.
Baseline Cognitive Performance of Study Participants (N = 49)
| Cognitive Test | Mean | SD | T-scorea | Level of Impairment |
|---|---|---|---|---|
| Digit Span | ||||
| Digits Forward | 8.90 | 2.10 | ||
| Digits Backward | 5.84 | 2.36 | ||
| Digits Total | 14.74 | 4.46 | 43 | Low Average |
| Digit Symbol | ||||
| Total Correct | 54.53 | 17.39 | 40 | Low Average |
| California Verbal Learning Test | ||||
| Total Correct, Trials 1–5 | 41.61 | 11.85 | 36 | Mildly Impaired |
| Total Correct, Delayed Recall | 8.10 | 3.38 | 31 | Mildly Impaired |
| Wisconsin Card Sorting Test | ||||
| Total Categories Obtained | 2.20 | 2.27 | 34 | Mildly Impaired |
| Percent Perseverative Errors | 33.68 | 21.20 | 22 | Moderately Impaired |
Based on population norms, average t=50, SD=10
The overall level of cognitive functioning was in the mildly impaired range, and ranged from low average for Digit Span and the DSST to moderately impaired for Percent Perseverative Errors on the WCST. The coefficient α on the summary scores for the cognitive tests in the battery was 0.86, indicating high internal consistency among the different measures. Examination of the correlations between the individual cognitive tests and the total score indicated that the lowest was r = 0.48 (for DSST) and the highest was r = 0.77 (for CVLT Total Correct, Trials 1–5).
Among the 49 participants who were randomized to the CBT program and who completed the neurocognitive battery at baseline, 40 (81.6%) were exposed to the program (i.e., completed > 6 sessions). The χ2 analyses and t-tests comparing the 9 participants who were not exposed to the program with the 40 participants who were exposed on the demographic and baseline clinical and cognitive variables indicated one significant difference. Participants with a lifetime substance use disorder were less likely to be exposed to the program (9/14 or 64.3%) than those without such a disorder (3/34 or 91.2%), χ2 = 5.16, df = 1, N = 48, p = 0.016.
Among the 40 participants who were exposed to CBT program, the average rate of homework completion was 50% (range: 0%–92%.) The Pearson correlation between the baseline cognitive composite score and the percentage of homework assignments completed for participants who were exposed to the CBT program was 0.12 (NS). Thus, participants with higher levels of cognitive functioning did not tend to complete more homework assignments to practice the breathing retraining and cognitive restructuring skills than participants with less intact cognitive functioning.
The results of the general mixed-effects linear regression and logistic analyses that evaluated whether cognitive functioning predicted improvements in PTSD and related outcomes are summarized in Table 3. Cognitive functioning was a significant predictor of only one outcome variable: improvement on the PTSD Knowledge Test: participants with lower levels of cognitive functioning at baseline learned less information about PTSD at the post-treatment and follow-up assessments compared to participants with more intact cognitive functioning.
Table 3.
Results of Mixed-Effects Linear Regression Analyses Examining Cognitive Functioning at Baseline as a Predictor of Outcomes at Post-treatment and 3- and 6-month Follow-up Assessments Among Participants Exposed to the Cognitive Restructuring Program (N = 40)a
| Mixed-Effects Linear Regression Analysesa | |||||
|---|---|---|---|---|---|
| Cognitive Composite Score Effect | |||||
| Outcome Variables | Regression Coefficient |
Standard Error |
DF | T | P |
| CAPS-Severity | −0.06 | 0.74 | 30 | −0.08 | 0.93 |
| CAPS-Re-experiencing | 0.02 | 0.24 | 30 | 0.07 | 0.94 |
| CAPS-Avoidance | −0.01 | 0.30 | 30 | −0.03 | 0.97 |
| CAPS-Hyperarousal | −0.05 | 0.24 | 30 | −0.20 | 0.84 |
| Beck Depression Inventory-II | −0.51 | 0.34 | 30 | −0.15 | 0.88 |
| Beck Anxiety Inventory | −0.32 | 0.25 | 30 | −1.27 | 0.21 |
| Post Traumatic Cognitions Inventory | 0.04 | 0.02 | 30 | 1.58 | 0.12 |
| Brief Psychiatric Rating Scale (BPRS) Total | −0.04 | 0.22 | 28 | −0.16 | 0.87 |
| BPRS Affect | 0.00 | 0.03 | 30 | 0.15 | 0.87 |
| BPRS Anergia | −0.01 | 0.01 | 28 | −1.25 | 0.22 |
| BPRS Thought Disorder | 0.00 | 0.02 | 30 | −0.05 | 0.96 |
| BPRS Activation | 0.01 | 0.01 | 28 | 0.91 | 0.37 |
| BPRS Disorganization | 0.00 | 0.00 | 27 | −1.25 | 0.22 |
| SF-12 Physical Component | −0.27 | 0.21 | 27 | −1.25 | 0.22 |
| SF-12 Mental Component | −0.19 | 0.27 | 27 | −0.72 | 0.47 |
| PTSD Knowledge Test | 0.10 | 0.05 | 29 | 2.12 | 0.02 |
| Mixed-Effects Logistic Regression Analysisb | |||||
|
Cognitive Composite Score Effect |
|||||
| Outcome Variable |
Regression Coefficient |
Standard Error |
DF | t | p |
| PTSD Diagnosis | 0.05 | 0.34 | 30 | 0.15 | 0.88 |
All analyses included baseline level of outcome variable, cognitive composite score, education, diagnosis, and time as predictors.
This analysis included cognitive composite score, education, diagnosis, and time as predictors.
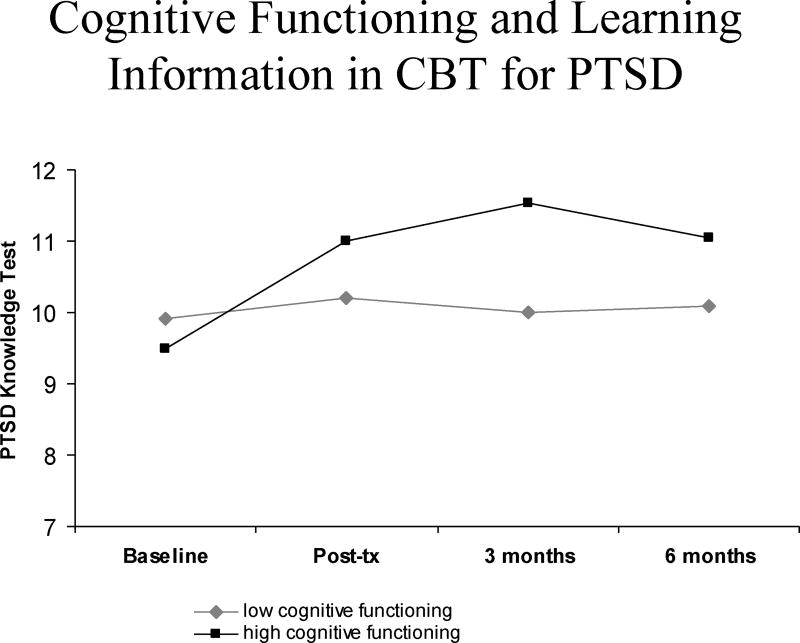
In order to illustrate the association between baseline cognitive functioning and learning of information about PTSD, the participants were divided into low or high cognitive functioning groups based on a median split of the cognitive composite measure, and their scores on the PTSD Knowledge Test were plotted over the four assessment points (see Figure 1). Although the high and low cognitive functioning groups appeared to have similar levels of knowledge at the last (6-month) assessment, the mixed effects linear regression analyses indicated that the baseline cognition by time interaction was not statistically significant. This means that after controlling for baseline knowledge, higher levels of cognitive functioning at baseline predicted greater knowledge scores across all three post-CBT assessments points (post-treatment, 3- and 6-month follow-ups), with no significant differences in prediction between those assessments. The baseline composite cognitive score did not predict improvement on any of the other outcome variables, including PTSD diagnosis and symptoms, anxiety or depression, other psychiatric symptoms, health, or trauma-related thoughts (ps > 0.05).
Figure 1.
Changes in Knowledge About PTSD Following CBT Program for Participants with High vs. Low Baseline Cognitive Functioning
None the 12 mixed-effects linear (or logistic) regression analyses examining whether individual cognitive test scores predicted PTSD symptom severity or PTSD diagnosis after treatment were statistically significant (ps > 0.05).
4. Discussion
The randomized controlled trial that this analysis is based on showed that the 12–16 session CBT program was a more effective treatment for PTSD in persons with severe mental illness than usual care (Mueser et al., 2008). Specifically, participants assigned to the CBT program improved more than those assigned to treatment as usual in PTSD diagnosis and symptoms, other symptoms, and self-reported health, as well as trauma-related cognitions and knowledge about PTSD, with treatment gains maintained at 3- and 6-month follow-ups. The present analysis found that among the participants in the CBT program who completed at least six sessions (i.e., were “exposed” to the program), performance on a neuropsychological battery administered at baseline was not related to clinical change in PTSD outcomes, interview-based or self-reported other symptoms or health, or trauma-related cognitions. When individual cognitive test scores were examined as predictors of improvement in PTSD symptom severity or diagnosis, none were statistically significant.
While participants with lower levels of cognitive functioning appeared to benefit clinically from the CBT program just as much as those with higher levels, cognitive functioning was significantly related to changes in a non-clinical outcome variable: knowledge about PTSD. Participants with lower levels of cognitive functioning learned less information about PTSD during CBT than those with better cognitive functioning. Interestingly, Jahn et al. (2011) also found that lower neurocognitive functioning predicted less learning of illness knowledge during psychoeducation for schizophrenia.
The guidelines for implementing the CBT program may provide a clue for why cognitive functioning predicted learning about PTSD but not clinical change in PTSD and related outcomes (Mueser et al., 2009). The CBT program is based on cognitive theories that posit PTSD emerges following exposure to a traumatic events that results in excessively negative appraisals of the event or the person’s reaction to it, and a disturbance in autobiographical memory about the trauma leading to re-experiencing symptoms (Ehlers and Clark, 2000; Ehlers et al., 2005; Horowitz, 1986). The CBT guidelines indicate that the primary role of education about trauma and PTSD is to harness the client’s motivation for treatment. Cognitive restructuring, on the other hand, is aimed at teaching a self-management skill for dealing with negative feelings that involves identifying, challenging, and correcting inaccurate thoughts or beliefs underlying those feelings, beginning with any negative feelings but eventually targeting trauma-related cognitions underlying PTSD. Because of the central role of cognitive restructuring in targeting PTSD, the treatment manual recommends spending no more than three sessions on psychoeducation, regardless of the amount of information learned, in order to have enough time to teach cognitive restructuring over the remaining 10–13 sessions. The fixed, limited amount of time spent on education about PTSD may have posed a greater challenge to learning this information for individuals with lower levels of cognitive functioning. The longer amount of time in the program for teaching cognitive restructuring, and opportunities to practice this skill afforded by homework, may have been sufficient for clients with lower cognitive abilities to learn and apply this skill to thoughts and beliefs related to their traumatic experiences, resulting in no association between baseline cognitive functioning and clinical benefit from the CBT program.
The implications of the observed association between cognitive functioning and reduced learning of information about PTSD are unclear. Although one goal of psychoeducation is to motivate clients to actively participate in the CBT program, clients with lower levels of cognitive functioning were not less likely to be successfully engaged and exposed to the program. It is possible that psychoeducation about the nature of PTSD also serves to normalize PTSD symptoms by explaining that they are common reactions to a traumatic event, which could reduce negative appraisals of those symptoms and distress associated with them, as well as facilitate cognitive restructuring related to PTSD symptoms. More research is needed to understand the contribution of psychoeducation about PTSD to clinical improvements in the disorder following CBT, and more broadly about the role of psychoeducation in the treatment of persons with severe mental illness (Lincoln et al., 2007).
Some research has suggested that impaired cognitive functioning can attenuate the benefits of illness self-management and social skills training programs due to its effects on reducing attendance at treatment sessions (Färdig et al., 2016; Kern et al., 1992). In the present study, cognitive functioning at baseline was not related to either attendance at treatment sessions (i.e., exposure to the program) or to the completion of homework assignments, which may in part account for the comparable clinical outcomes of participants with a range of different levels of cognitive functioning.
Although cognitive functioning was not related to clinical improvements in PTSD and other symptoms in this study, the overall diagnostic composition of the sample was primarily mood disorders (81.7%), with only 18.3% schizophrenia or schizoaffective disorder. Cognitive impairment tends to be particularly pronounced in people with schizophrenia (Harvey, 2013), but are a common feature of mood disorders as well (Dickerson et al., 2004; McIntyre and Lee, 2016; Ragguett et al., 2016). Somewhat consistent with this, the cognitive functioning of the overall sample was in the low average range for processing speed and short-term memory, and was in the mild to moderate range of impairment for learning and memory and executive functions. Most of the research suggesting that cognitive functioning is a predictor of response to psychosocial treatment in persons with severe mental illness has been conducted with samples of clients who have schizophrenia or with mixed diagnostic samples including a higher proportion of persons with schizophrenia (Kurtz, 2011; McGurk and Mueser, 2004). Research is needed to evaluate whether cognitive functioning is predictive of response to the CBT program in clients with more compromised cognitive functioning.
Several limitations of this study should be considered. First, the neurocognitive assessment was limited, and a more comprehensive battery would have permitted a finer grain analysis of the relationships between different domains of cognitive functioning and benefit from the CBT program. Second, the neurocognitive battery was administered only to the study participants who had been randomized to the CBT program and not those in the treatment as usual group, precluding the ability to evaluate whether cognitive functioning was a differential predictor of response to treatment vs. usual care. Third, the sample size was relatively small, and thus this study had limited statistical power to detect associations between cognitive functioning and treatment outcomes.
These limitations notwithstanding, this study was the first to evaluate whether cognitive functioning is related to response to an intervention targeting PTSD in people with severe mental illness. The fact that level of cognitive functioning was not predictive of clinical benefit from the CBT program is encouraging, and suggests that the methods in the program for teaching cognitive restructuring are robust, and may be useful when working with a range of persons with different diagnoses and levels of cognitive functioning. More research is needed to evaluate the effects of the CBT for PTSD program on other clinical populations, and to further explore whether cognitive functioning is related to treatment outcomes.
Highlights.
Cognitive behavioral therapy (CBT) is effective at treating posttraumatic stress disorder (PTSD) in people with severe mental illness.
It is unknown whether cognitive impairment limits response to CBT for PTSD in persons with severe mental illness.
A neuropsychological battery was administered at baseline to participants in trial who received a CBT program to evaluate whether it predicted participation in the program or treatment outcomes.
Reduced cognitive functioning predicted learning less information about PTSD at post-treatment and 3- and 6-month follow-ups, but was not related to participation in CBT or PTSD or other clinical outcomes.
Cognitive impairment does not appear to limit clinical benefit from CBT for PTSD in people with severe mental illness
Acknowledgments
This research was supported by the National Institute of Mental Health grant #R01MH064662.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahern E, Samkovska M. Cognitive functioning in the first-episode of major depressive disorder: A systematic review and meta-analysis. Neuropsychol. 2017;31:52–72. doi: 10.1037/neu0000319. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Fourth. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bebbington PE, Bhugra D, Brugha T, Singleton N, Farrell M, Jenkins R, et al. Psychosis, victimisation and childhood disadvantage: Evidence from the second British National Survey of Psychiatric Morbidity. Br. J. Psychiat. 2004;185:220–26. doi: 10.1192/bjp.185.3.220. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. The Beck Anxiety Inventory Manual. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Berg EA. A simple objective test for measuring flexibility in thinking. J. General Psychol. 1948;39:15–22. doi: 10.1080/00221309.1948.9918159. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM. Clinician Administered PTSD Scale for DSM-IV. National Center for Posttraumatic Stress Disorder; Boston, MA: 1995. [DOI] [PubMed] [Google Scholar]
- Blanchard EP, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist. Behav. Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bortolato B, Carvalho AF, McIntyre RS. Cognitive dysfunction in major depressive disorder: A state-of-the-art clinical review. CNS Neurol. Dis.-Drug Targ. 2014;13:1804–18. doi: 10.2174/1871527313666141130203823. [DOI] [PubMed] [Google Scholar]
- Bortolato B, Miskowaik KW, Köhler CA, Vieta E, Carvalho AF. Cognitive dysfunction in bipolar disorder and schizophrenia: A systematic review of meta-analyses. Neuropsychiat Dis. Treat. 2015;11:3111–25. doi: 10.2147/NDT.S76700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostock ECS, Kirkby KC, Garry MI, Taylor BVM. Systematic review of cognitive function in euthymic bipolar disorder and pre-surgical temporal lobe epilepsy. Front. Psychiat. 2017;8(133) doi: 10.3389/fpsyt.2017.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: A follow-up study at age 17 years. Arch. Gen. Psychiat. 2006;63:1238–45. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- Brock SE. Descriptive Statistics and Psychological Testing. Webpage. California State University; Sacramento, CA: 2017. [accessed on April 6, 2017]. URL: http://www.csus.edu/indiv/b/brocks/courses/eds%20250/eds%20250/handouts/11/descrptive%20statistics%20and%20the%20normal%20curve.pdf. [Google Scholar]
- Cusack KJ, Herring AH, Steadman HJ. PTSD as a mediator between lifetime sexual abuse and substance use among jail diversion participants. Psychiat. Serv. 2013;64:776–81. doi: 10.1176/appi.ps.000052012. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test-Second Edition. Psychological Corporation; San Antonio, TX: 2000. [Google Scholar]
- Depp CA, Mausbach BT, Harmell AL, Savla GN, Bowie CR, Harvey PD, et al. Meta-analysis of the association between cognitive abilities and everyday functioning in bipolar disorder. Bipolar Dis. 2012;14:217–26. doi: 10.1111/j.1399-5618.2012.01011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson FB, Boronow JJ, Stallings C, Origoni AE, Cole SK, Yolken RH. Cognitive functioning in schizophrenia and bipolar disorder: comparison of performance on the Repeatable Battery for the Assessment of Neuropsychological Status. Psychiat. Res. 2004;129:45–53. doi: 10.1016/j.psychres.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch. Gen. Psychiat. 2007;64:532–42. doi: 10.1001/archpsyc.64.5.532. [DOI] [PubMed] [Google Scholar]
- Dominguez MD, Viechtbauer W, Simons CJP, van Os J, Krabbendam L. Are psychotic psychopathology and neurocognition orthogonal? A systematic review of their associations. Psychol. Bul. 2009;135:157–71. doi: 10.1037/a0014415. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav. Res. Ther. 2000;38:319–45. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: Development and evaluation. Behav. Res. Ther. 2005;43:413–31. doi: 10.1016/j.brat.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Ehring T, Welboren R, Morina N, Wicherts JM, Freitag J, Emmelkamp PMG. Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clin. Psychol. Rev. 2014;34:645–57. doi: 10.1016/j.cpr.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Färdig R, Fredriksson S, Lewander T, Melin L, Mueser KT. Neurocognitive functioning and outcome of the Illness Management and Recovery Program for clients with schizophrenia and schizoaffective disorder. Nord. J. Psychiat. 2016;70:430–35. doi: 10.3109/08039488.2016.1146797. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-I Disorders - Patient Edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Axis-II Personality Disorders (SCID-II) (Version 2.0) New York State Psychiatric Institute, Biometrics Research Department; New York: 1994. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychol. Assess. 1999;11:303–14. [Google Scholar]
- Foa EB, Rothbaum BO. Treating the Trauma of Rape: Cognitive-Behavioral Therapy for PTSD. Guilford Press; New York: 1998. [Google Scholar]
- Gearon JS, Bellack AS, Tenhula WN. Preliminary reliability and validity of the Clinician-Administered PTSD Scale for schizophrenia. J. Consult. Clin. Psychol. 2004;72:121–25. doi: 10.1037/0022-006X.72.1.121. [DOI] [PubMed] [Google Scholar]
- Golier JA, Yehuda R. Neuropsychological processes in post-traumatic stress disorder. Psychiat. Clin. N. Am. 2002;25:295–315. doi: 10.1016/s0193-953x(01)00004-1. [DOI] [PubMed] [Google Scholar]
- Goodkind M, Eikhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiat. 2015;72:305–14. doi: 10.1001/jamapsychiatry.2014.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman LA, Salyers MP, Mueser KT, Rosenberg SD, Swartz M, Essock SM, et al. Recent victimization in women and men with severe mental illness: Prevalence and correlates. J. Traum. Str. 2001;14:615–32. doi: 10.1023/A:1013026318450. [DOI] [PubMed] [Google Scholar]
- Grubaugh AL, Zinzow HM, Paul L, Egede LE, Frueh BC. Trauma exposure and posttraumatic stress disorder in adults with severe mental illness: A critical review. Clin. Psychol. Rev. 2011;31:883–99. doi: 10.1016/j.cpr.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PD, editor. Cognitive Impairment in Schizophrenia. Cambridge University Press; Cambridge, England: 2013. [Google Scholar]
- Heaton RK, Gladsjo JA, Palmer BW, Kuck J, Marcotte TD, Jeste DV. Stability and course of neuropsychological deficits in schizophrenia. Arch. Gen. Psychiat. 2001;58:24–32. doi: 10.1001/archpsyc.58.1.24. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. Wiley; New York: 2006. [Google Scholar]
- Horowitz MJ. Stress Response Syndromes. 2. Jason Aronson; New York: 1986. [Google Scholar]
- Hughes C, Kumari V, Soni W, Das M, Binneman B, Drozd S, et al. Longitudinal study of symptoms and cognitive function in chronic schizophrenia. Schiz. Res. 2003;59:137–46. doi: 10.1016/s0920-9964(01)00393-0. [DOI] [PubMed] [Google Scholar]
- Jahn T, Pitschel-Walz G, Gsottschneider A, Froböse T, Kraemer S, Bäuml J. Neurocognitive prediction of illness knowledge after psychoeducation in schizophrenia: Results from the Munich COGPIP study. Psychol. Med. 2011;41:533–44. doi: 10.1017/S0033291710001029. [DOI] [PubMed] [Google Scholar]
- Kern RS, Green MF, Satz P. Neuropsychological predictors of skills training for chronic psychiatric patients. Psychiat. Res. 1992;43:223–30. doi: 10.1016/0165-1781(92)90055-8. [DOI] [PubMed] [Google Scholar]
- Khalifeh H, Johnson S, Howard LM, Borschmann R, Osborn D, Dean K, et al. Violent and non-violent crime against adults with severe mental illness. Br. J. Psychiat. 2015;206:275–82. doi: 10.1192/bjp.bp.114.147843. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychol. Assess. 2000;12:210–24. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kurtz MM. Neurocognition as a predictor of response to evidence-based psychosocial interventions in schizophrenia: What is the state of the evidence? Clin. Psychol. Rev. 2011;31:663–72. doi: 10.1016/j.cpr.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln TM, Wilhelma K, Nestoriuca Y. Effectiveness of psychoeducation for relapse, symptoms, knowledge, adherence and functioning in psychotic disorders: A meta-analysis. Schizophr. Res. 2007;96:232–45. doi: 10.1016/j.schres.2007.07.022. [DOI] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein KH, Ventura J. Manual for the Expanded Brief Psychiatric Rating Scale (BPRS) Schizophr. Bul. 1986;12:594–602. [Google Scholar]
- McGurk SR, Mueser KT. Cognitive functioning, symptoms, and work in supported employment: A review and heuristic model. Schizophr. Res. 2004;70:147–74. doi: 10.1016/j.schres.2004.01.009. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Harvey PD, Marder J, LaPuglia R. Cognitive and symptom predictors of work outcomes for clients with schizophrenia in supported employment. Psychiat. Serv. 2003;54:1129–35. doi: 10.1176/appi.ps.54.8.1129. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Lee Y. Cognition in major depressive disorder: A Systemically Important Functional Index’ (SIFI) Cur. Opin. Psychiat. 2016;29:48–55. doi: 10.1097/YCO.0000000000000221. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Shin LM. Association of intelligence with severity of posttraumatic stress disorder symptoms in Vietnam combat veterans. Am. J. Psychiat. 1995;152:936–38. doi: 10.1176/ajp.152.6.936. [DOI] [PubMed] [Google Scholar]
- McTeague LM, Huemer J, Carreon DM, Jiang Y, Eikhoff SB, Etkin A. Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. Am. J. Psychiat. 2017;174:676–85. doi: 10.1176/appi.ajp.2017.16040400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejía-Arango S, Wong R, Michaels-Obregón A. Normative and standardized data for cognitive measures in the Mexican Health and Aging Study. Salud Publica de Mexico. 2015;57:S90–6. doi: 10.21149/spm.v57s1.7594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Bellack AS, Douglas MS, Wade JH. Prediction of social skill acquisition in schizophrenic and major affective disorder patients from memory and symptomatology. Psychiat. Res. 1991;37:281–96. doi: 10.1016/0165-1781(91)90064-v. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Gottlieb JD, Xie H, Lu W, Yanos PT, Rosenberg SR, et al. Evaluation of cognitive restructuring for PTSD in people with severe mental illness. Br. J. Psychiat. 2015;206:501–8. doi: 10.1192/bjp.bp.114.147926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Goodman LA, Trumbetta SL. Trauma, PTSD, and the course of schizophrenia: An interactive model. Schizophr. Res. 2002;53:123–43. doi: 10.1016/s0920-9964(01)00173-6. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Jankowski MK, Hamblen JL, Descamps M. A cognitive-behavioral treatment program for posttraumatic stress disorder in severe mental illness. Am. J. Psychiat. Rehab. 2004;7:107–46. [Google Scholar]
- Mueser KT, Rosenberg SD, Rosenberg HJ. Treatment of Posttraumatic Stress Disorder in Special Populations: A Cognitive Restructuring Program. American Psychological Association; Washington, DC: 2009. [Google Scholar]
- Mueser KT, Rosenberg SR, Xie H, Jankowski MK, Bolton EE, Lu W, et al. A randomized controlled trial of cognitive-behavioral treatment of posttraumatic stress disorder in severe mental illness. J. Consult. Clin. Psychol. 2008;76:259–71. doi: 10.1037/0022-006X.76.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Salyers MP, Rosenberg SD, Goodman LA, Essock SM, Osher FC, et al. Interpersonal trauma and posttraumatic stress disorder in patients with severe mental illness: Demographic, clinical, and health correlates. Schizophr. Bul. 2004;30:45–57. doi: 10.1093/oxfordjournals.schbul.a007067. [DOI] [PubMed] [Google Scholar]
- Murrough JW, Iacoviello B, Neumeister A, Charney DS, Iosifescu DV. Cognitive dysfunction in depression: Neurocircuitry and new therapeutic strategies. Neurobiol. Learn. Mem. 2011;96:553–63. doi: 10.1016/j.nlm.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Ng LC, Patruzzi LJ, Green MC, Mueser KT, Borba CPC, Henderson DC. Posttraumatic stress disorder symptoms and social and occupational functioning of people with schizophrenia. J. Nerv. Ment. Dis. 2016;204:590–8. doi: 10.1097/NMD.0000000000000523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter RJ, Robinson LJ, Malhi GS, Gallagher P. The neurocognitive profile of mood disorders - a review of the evidence and methodological issues. Bipolar Dis. 2015;17:21–40. doi: 10.1111/bdi.12342. [DOI] [PubMed] [Google Scholar]
- Pratt SI, Rosenberg SD, Mueser KT, Brancato J, Salyers MP, Jankowski MK, et al. Evaluation of a PTSD psychoeducational program for psychiatric inpatients. J. Ment. Heal. 2005;14:121–27. [Google Scholar]
- Ragguett RM, Cha DS, Kakar R, Rosenblat JD, Lee Y, McIntyre RS. Assessing and measuring cognitive function in major depressive disorder. Evidence Based Mental Health. 2016;19:10609. doi: 10.1136/eb-2016-102456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SD, Mueser KT, Friedman MJ, Gorman PG, Drake RE, Vidaver RM, et al. Developing effective treatments for posttraumatic disorders among people with severe mental illness. Psychiat. Serv. 2001;52:1453–61. doi: 10.1176/appi.ps.52.11.1453. [DOI] [PubMed] [Google Scholar]
- Rosenberg SD, Mueser KT, Jankowski MK, Salyers MP, Acker K. Cognitive-behavioral treatment of posttraumatic stress disorder in severe mental illness: Results of a pilot study. Am. J. Psychiat. Rehab. 2004;7:171–86. [Google Scholar]
- Roy L, Crocker AG, Nicholls TL, Latimer EA, Reyes Ayllon AR. Criminal behavior and victimization among homeless individuals with severe mental illness: A systematic review. Psychiat. Serv. 2014;65:739–50. doi: 10.1176/appi.ps.201200515. [DOI] [PubMed] [Google Scholar]
- Rund BR, Melle I, Friis S, Larsen TK, Midboe LJ, Opjordsmoen S, et al. Neurocognitive dysfunction in first-episode psychosis: correlates with symptoms, premorbid adjustment, and duration of untreated psychosis. Am. J. Psychiat. 2004;161:466–72. doi: 10.1176/appi.ajp.161.3.466. [DOI] [PubMed] [Google Scholar]
- Schaefer J, Giangrande E, Weinbrerger DR, Dickinson D. The global cognitive impairment in schizophrenia: Consistent over decades and around the world. Schiz. Res. 2013;150:42–50. doi: 10.1016/j.schres.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel C, Hardy A, Smith B, Wykes T, Rose S, Enright S, et al. Cognitive behaviour therapy for posttraumatic stress in schizophrenia. A randomised controlled trial. Psychol. Med. 2017;47:43–51. doi: 10.1017/S0033291716002117. [DOI] [PubMed] [Google Scholar]
- Subica AM, Claypoole KH, Wylie AM. PTSD’S mediation of the relationships between trauma, depression, substance abuse, mental health, and physical health in individuals with severe mental illness: Evaluating a comprehensive model. Schizophr. Res. 2011;104–09:136. doi: 10.1016/j.schres.2011.10.018. [DOI] [PubMed] [Google Scholar]
- Torres IJ, Boudreau VG, Yatham LN. Neuropsychological functioning in euthymic bipolar disorder: A meta-analysis. Acta Psychiat. Scand. 2007;434:17–26. doi: 10.1111/j.1600-0447.2007.01055.x. [DOI] [PubMed] [Google Scholar]
- Van den Berg DPG, de Bont PAJM, van der Vleugel BM, de Roos A, de Jongh A, van Minnen A, et al. Prolonged exposure versus eye movement desensitization and reprocessing versus waiting list for posttraumatic stress disorder in patients with a psychotic disorder. JAMA Psychiat. 2015;72:259–67. doi: 10.1001/jamapsychiatry.2014.2637. [DOI] [PubMed] [Google Scholar]
- Ventura J, Thames AD, Wood RC, Guzik LH, Hellemann GS. Disorganization and reality distortion in schizophrenia: A meta-analysis of the relationship between positive symptoms and neurocognitive deficits. Schiz. Res. 2010;121:1–14. doi: 10.1016/j.schres.2010.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Health Assessment Lab; Boston: 1994. [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J. Clin. Psychiat. 2013;74:e541–50. doi: 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale-Revised (WAIS III Manual) Psychological Corporation; New York: 1998. [Google Scholar]
- Woon FL, Sood S, Hedges DW. Hippocampal volume deficits associated with exposure to psychological trauma and posttraumatic stress disorder in adults: A meta-analysis. Progr. Neuro-Psychopharmacol. Biol. Psychiat. 2010;34:1181–8. doi: 10.1016/j.pnpbp.2010.06.016. [DOI] [PubMed] [Google Scholar]
- Yurgil KA, Barkauskas DA, Vasterling JV, Nievergelt CM, Larson GE, Schork N, et al. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty marines. JAMA Psychiat. 2014;71:149–57. doi: 10.1001/jamapsychiatry.2013.3080. [DOI] [PubMed] [Google Scholar]