Abstract
Despite increasing awareness of stigma from mental health service providers as a barrier to recovery, little research has directly examined how it might influence the service users’ self-perceptions and treatment experience. The present study examined the association of service users’ perceived provider stigma with their experience of internalized stigma and disempowerment, two psychosocial constructs known to hinder recovery. Mental health service users (N = 350) completed questionnaires assessing perceived stigma from mental health service providers, including perceptions of negative affective reactions towards individual users and desired social distance towards people with mental illnesses across various life domains, internalized stigma, and disempowerment (i.e., diminished self-efficacy and mastery) in mental health treatment settings. Structural equation modeling showed that both perceived negative affective reactions and perceived social distance were positively associated with disempowerment. Furthermore, these associations were significantly mediated by internalized stigma. These findings illuminate how perceived stigma from providers can “get under the skin” of mental health service users and contribute to their overall sense of disempowerment in mental health settings. They also highlight the need for future stigma reduction interventions to specifically target the attitudes and beliefs held by mental health professionals.
Keywords: Perceived stigma, internalized stigma, mental health professionals, mental health service users, empowerment
1. Introduction
Among people with serious mental illnesses, stigma associated with psychiatric diagnoses represents a major barrier to recovery. Across numerous studies, perceived stigma (i.e., the perception that most members of the general public devalue those with mental illnesses) has been shown to undermine self-esteem (Link et al., 2001), increase social withdrawal and isolation (Perlick et al., 2001), and deter individuals from seeking mental health treatment (Corrigan et al., 2014). Among some individuals, perceived stigma can also induce internalized stigma (i.e., endorsement of negative mental-illness-related stereotypes as self-relevant), which is associated with a wide range of adverse outcomes known to hinder recovery, including hopelessness, diminished self-efficacy, and limited consumer participation in mental health treatment (Hamann et al., 2017; Livingston and Boyd, 2010; Quinn et al., 2015). Little research, however, has examined how perceived stigma from mental health professionals might influence the self-perceptions and recovery of individuals who utilize mental health services. This limitation is noteworthy given that perceptions of negative attitudes from professionals can reinforce societal stigma and interfere with the development of successful therapeutic relationships, thereby undermining the quality and effectiveness of mental health treatment. In the present research, we examined how mental health service users’ perceived stigma from providers might relate to their levels of internalized stigma and their sense of disempowerment, which is defined as a lack of self-worth, power, and ability to harness anger into action against social injustice.
Qualitative research on the experience of mental health service users clearly indicates that stigmatizing attitudes and behaviors from professionals represent an important concern for those who utilize mental health services. As outlined in an ethnographic content analysis of personal account literature authored by mental health service users and their families, stigma in the mental healthcare context is often characterized by blame and shame, disinterest and annoyance, dehumanization, poor prognosis, and coercion (Charles, 2013). These themes have been consistently reflected in individual interview and focus group studies with mental health service users. In one study, for example, service users interviewed recounted poignant instances in which they experienced stigma from mental health service providers, including being stereotyped as incompetent and lacking recovery potential as well as being treated in a patronizing, disrespectful manner (Wahl, 1999). Other studies further highlighted similar experiences of devaluation and discrimination from mental health professionals, as manifested in a lack of interest in service users’ individual needs and treatment preferences (Pinfold et al., 2005; Schulze and Angermeyer, 2003).
A separate body of literature on the attitudes of mental health professionals towards people with mental illnesses converges with the perceptions of service users. Although some studies suggest that professionals tend to hold more positive attitudes than members of the general public (Kingdon et al., 2004; Stuber et al., 2014), others indicate that they are not immune to stigmatizing beliefs commonly associated with mental illnesses. For example, one of the most prevalent emotions reported by service providers about those living with mental illnesses is fear (Overton and Medina, 2008), and other negative affective reactions, such as dislike, anger, and neglect, are also common (Penn and Martin, 1998). Furthermore, in comparison with members of the general public, professionals reported similar levels of desired social distance and implicit negative attitudes towards those living with mental illnesses, highlighting their reluctance to interact closely with people with mental illnesses (Kopera et al., 2015; Lauber et al., 2004; Nordt et al., 2006).
Despite the well-documented presence of mental health provider stigma and an increasing recognition of its importance as a barrier to recovery (Corrigan et al., 2014; Schulze, 2007), no quantitative studies, to our knowledge, has directly examined how it might influence the other aspects of the service users’ treatment experience. In the present research, we addressed this question by examining the association of service users’ perceived stigma from mental health professionals with their experience of internalized stigma and disempowerment, two psychosocial constructs that have been identified as key factors hindering recovery. Because both negative emotional reactions (e.g., anger, pity, anxiety) and social distance (ie., willingness to interact with a target person across different life domains) have been identified as important components of mental illness stigma (Link et al., 2004), we focused on two components of perceived provider stigma: (1) perceptions of negative affective reactions towards individual service users; and (2) perceptions of desired social distance towards individuals with mental illnesses across various life domains. In light of the known adverse impact of perceived stigma on self-efficacy and mastery (Link et al., 2001; Perlick et al., 2001), we hypothesized that service users’ perceptions of both negative affective reactions and desired social distance from providers would be positively associated with their sense of disempowerment in mental health settings. Furthermore, considering that chronic exposure to negative mental-illness-related stereotypes can often result in the internalization of such stereotypes (Corrigan et al., 2006; Quinn et al., 2015) and that internalized stigma has been linked to more passive, less participatory behaviors in the context of interactions with mental health professionals (Hamann et al., 2017), we hypothesized that internalized stigma would significantly mediate these associations.
2. Methods
2.1. Participants and Procedures
Data for this study were taken from a larger project examining the experiences of service users in mental health settings. Participants, all of whom were users of outpatient mental health services, were recruited from 18 Lead Mental Health Authorities (LMHA) affiliated with the Connecticut Department of Mental Health and Addiction Services. These LMHAs cover all of the state of Connecticut and include ten state-operated behavioral health centers (which serve clients without insurance, many of whom receive social security disability) as well as eight private non-profit community behavioral health centers (which serve clients with private insurance and state insurance). Approximately 52% of LMHA clients qualify for a serious mental illness (SMI) diagnosis (i.e., Schizophrenia and related psychotic disorders, Bipolar Disorder, or Major Depressive Disorder); 67.5% have a substance use disorder, and 27.5% qualify for a dual diagnosis (i.e., both SMI and substance use disorder diagnoses; Connecticut Department of Mental Health and Addiction Services, 2016). Between March and May in 2009, research staff visited each LMHA to survey clients who were interested in participating in a study on “what it is like to receive services at this LMHA.” Each participant completed the questionnaire individually via paper and pencil; bilingual research assistants read questions to those who have difficulty reading English. All study measures were approved by the Yale University Human Investigation Committee and the Connecticut Department of Mental Health and Addiction Services Institutional Review Board.
A total of 394 mental health service users took part in the study. Of these, 44 were omitted from analysis due to missing data on one or more variables of interest, resulting in an analytic sample of 350 participants. The demographic characteristics of the sample are summarized in Table 1. As can be seen, the mean age of the sample was 41.97 years (sd = 12.09). More than half of the participants were male; a majority were unemployed and identified as White. The analytic sample did not significantly differ from the excluded participants with respect to age, gender, and race/ethnicity, p > 0.10.
Table 1.
Demographic Characteristics of the Sample
| Mean age (SD) | 41.97 (12.09) |
| Gender (% male) | 55.1% |
| Race/ethnicity | |
| Black/African American | 21.7% |
| Hispanic | 10.9% |
| White | 72.0% |
| Other race/ethnicity | 6.3% |
| Educational Attainment | |
| Less than high school | 23.1% |
| Completed high school | 53.7% |
| Some college | 14.9% |
| Completed college | 7.7% |
| Marital Status | |
| Never married | 64.9% |
| Married | 6.6% |
| Divorced | 21.1% |
| Separated | 6.0% |
| Widowed | 1.4% |
| Employment Status | |
| Not employed | 79.7% |
| Employed | 20.3% |
2.2. Measures
2.2.1. Perceived negative affective reactions
The Affective Reactions Scale (Penn et al., 1994), which was developed to assess individuals’ affective responses to people with mental illnesses, was adapted to capture service users’ perceptions of negative affective reactions from their mental health providers. Participants rated how they thought the staff at this mental health center (clinicians, case managers, psychiatrists, etc.) feel about them across 10 pairs of bipolar adjectives (e.g., “apprehensive-comfortable”, “empathetic-angry”) using a seven-point scale. Items were scored such that a higher total score on the scale indicated more negative affective reactions (in the current sample, α = 0.77).
2.2.2. Perceived social distance
The Social Distance Scale (Link et al., 1987), which captures desired social distance endorsed by members of the general public towards those with mental illness, was adapted to assess service users’ perceptions of desired social distance endorsed by service providers. Participants answered seven questions about the extent they thought the staff at their mental health center would feel comfortable about interacting with someone with mental illness across different life domains. Sample items include “How would the staff at this mental health center feel about working on the same job as someone with mental illness?” and “How would the staff at this mental health center feel about being neighbors with someone with mental illness?” Each item was rated on a seven-point scale ranging from 1 (not at all comfortable) to 7 (very comfortable). All items were reversed scored such that a higher total score on the measure indicated greater perceived social distance (in the current sample, α = 0.88).
2.2.3. Internalized stigma
Internalized stigma was assessed using the Self Stigma of Mental Illness Scale (SSMI) (Corrigan et al., 2006). This measure consists of four 10-item subscales capturing distinct though highly correlated processes, including stereotype awareness, stereotype agreement, stereotype self-concurrence, and self-esteem decrement. Because the awareness of negative mental-illness-related stereotypes does not necessarily lead to the internalization of such stereotypes, we only included the Stereotype Agreement (e.g., “Most persons with mental illness cannot get or keep a regular job.”), Stereotype Self-Concurrence (e.g., “Because I have a mental illness, I cannot get or keep a regular job.”, and Self-Esteem Decrement (e.g., “I respect myself less because I cannot get or keep a regular job.”) subscales in the current analyses. Participants indicated their agreement with each statement using a nine-point scale, ranging from 1 (strongly disagree) to 9 (strongly agree). In the current sample, the Cronbach α for the Stereotype Agreement, Stereotype Self-Concurrence, and Self-Esteem Decrement subscales were 0.90, 0.86, and 0.91, respectively.
2.2.4. Disempowerment
Disempowerment in mental health settings was assessed using an adapted version of Empowerment Scale (Rogers et al., 1997). Across 21 items, participants rated their experiences at the mental health center with regard to their sense of self-efficacy, personal control, and ability to harness righteous anger into action using a four-point scale, ranging from 1 (strongly agree) to 4 (strongly disagree). Sample items include “At this mental health center, I feel powerless most of the time” and “At this mental health center, I generally accomplish what I set out to do.” Items were scored such that a higher total score on the scale indicated greater disempowerment. The Cronbach α in the current sample was 0.78.
2.3. Data Analysis
Preliminary analyses indicated that, among all of the demographic variables (i.e., age, gender, race/ethnicity, education, employment status), only age was significantly associated with disempowerment in mental health settings, r = 0.14, p = 0.007. Thus, we included age as a covariate in all subsequent analyses. To test our hypothesized associations among perceived stigma (i.e., perceptions of negative affective reactions and desired social distance from service providers), internalized stigma, and disempowerment among mental health service users, we utilized structural equation modeling (SEM) via Mplus 7.4, in which we specified internalized stigma as a latent variable consisting of scores on the SSMI’s Stereotype Agreement, Stereotype Self-Concurrence, and Self-Esteem Decrement subscales; all other variables were treated as manifest. We utilized the Mplus default of maximum likelihood estimation and requested that standard errors be calculated using 10,000 bootstrap draws. Estimates of indirect effects were requested and their significance also estimated utilizing the bootstrapping procedures. Given the cross-sectional design of the current study, we also tested an alternative model in which perceived negative affective reactions and internalized stigma were posited to mediate the association between internalized stigma and disempowerment. Across all models, we used standard indicators of model fit, which included a root mean square error of approximation (RMSEA) at or below 0.06, a comparative fit index (CFI) at or above 0.95, and a standardized root mean square residual (SRMR) at or below 0.08. We utilized the likelihood-based information criteria—Akaike’s information criteria (AIC), Bayesian information criteria (BIC), and adjusted Bayesian information criteria (ABIC)—to compare the fit of the hypothesized and alternative models, with lower information criteria suggesting better fit.
3. Results
The means and standard deviations of all variables of interest, along with bivariate correlations among all variables, are summarized in Table 2. As can be seen, participants reported relatively low levels of perceived provider stigma (including both perceived negative affective reactions and desired social distance), internalized stigma, and disempowerment. Specifically, the mean score for perceived negative affective reactions (M = 3.43) was closer to the positive adjectives (e.g., comfortable, empathetic) than to their corresponding negative adjectives (e.g., apprehensive, angry) on a seven-point bipolar scale. Similarly, the mean scores for perceived desired social distance (M = 3.23), the four SSMI subscales (Ms = 2.36–2.87), and disempowerment (M = 2.08) all fell below the midpoint on their respective scales. Perceived negative affective reactions were positively correlated with stereotype agreement, stereotype self-concurrence, self-esteem decrement, and disempowerment. Perceived social distance was also positively correlated with stereotype agreement, stereotype self-concurrence, and disempowerment, though not with self-esteem decrement. Stereotype agreement, stereotype self-concurrence, and self-esteem decrement were all strongly correlated with one another.
Table 2.
Correlations among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Negative affective reactions | -- | 0.15** | 0.14* | .23** | 0.25** | 0.34** | .003 |
| 2. Desired social distance | -- | -- | 0.25** | 0.13* | 0.06 | 0.18** | −0.02 |
| 3. SSMI_agreement | -- | -- | -- | 0.51** | 0.38** | 0.24** | 0.03 |
| 4. SSMI_concurrence | -- | -- | -- | -- | 0.66** | 0.36** | −0.03 |
| 5. SSMI_decrement | -- | -- | -- | -- | -- | 0.34** | .02 |
| 6. Disempowerment | -- | -- | -- | -- | -- | -- | 0.14** |
| 7. Age | -- | -- | -- | -- | -- | -- | -- |
| M | 3.43 | 3.23 | 2.87 | 2.45 | 2.36 | 2.08 | 41.97 |
| SD | 1.02 | 1.41 | 1.73 | 1.54 | 1.71 | 0.36 | 12.09 |
p < 0.05
p < 0.01
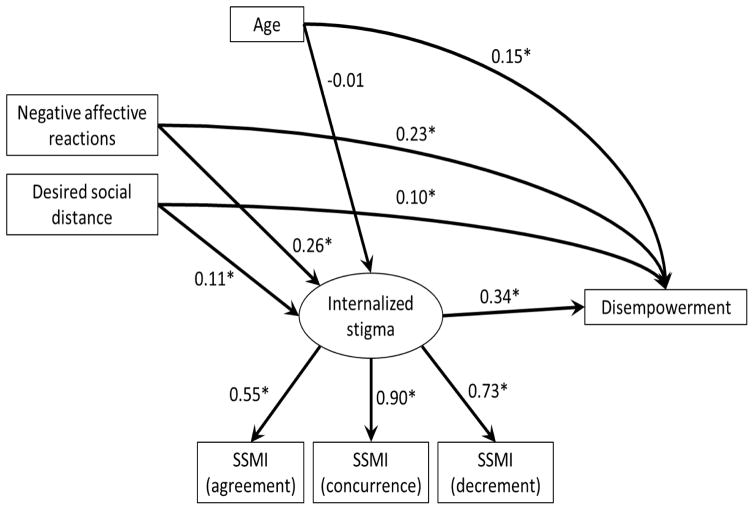
We proposed that perceived negative affective reactions and desired social distance from service providers would be associated with elevated levels of internalized stigma, which would in turn relate to disempowerment in mental health settings. We examined these hypothesized pathways using the model depicted in Figure 1. The model demonstrated adequate fit, RMSEA = 0.07, CFI = 0.97, SRMR = 0.03, χ2(8) = 22.46, p = 0.004. As expected, perceived negative affective reactions were positively associated with both internalized stigma (β = 0.26, p < 0.001) and disempowerment (β = 0.23, p < 0.001). Also as expected, internalized stigma was positively associated with disempowerment (β = 0.34, p < 0.001). In line with our mediation hypothesis, there was a significant indirect effect of perceived negative affective reactions on disempowerment through internalized stigma (β = 0.09, p < 0.001). Similarly, perceived social distance was positively associated with both internalized stigma (β = 0.12, p = 0.027) and disempowerment (β = 0.10, p = 0.029); the indirect effect of perceived social distance on disempowerment through internalized stigma was marginally significant (β = 0.04, p = 0.057). Overall, the model explained 26% of the variance in disempowerment among our sample of mental health service users.
Figure 1.
Hypothesized Pathways Among Perceived Mental Health Provider Stigma, Internalized Stigma, and Disempowerment
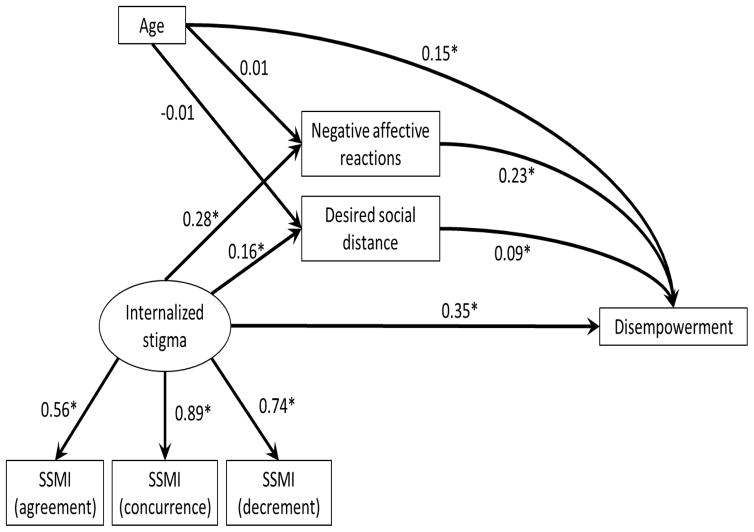
Due to the cross-sectional design of the current study, it is not possible to ascertain the directionality of relationships among our variables of interest. In particular, one might reasonably suggest that service users who internalize negative mental illness-related stereotypes might be more inclined to anticipate and perceive stigma from their mental health service providers. To examine this possibility, we tested an alternative model (Figure 2), which contains the same set of variables but reverse causal pathways between perceived stigma (including both perceived negative affective reactions and desired social distance) and internalized stigma. In contrast to the hypothesized model, although the indirect effect of internalized stigma on disempowerment through perceived negative affective reactions was significant (β = 0.06, p < 0.001), the indirect effect through perceived social distance was not (β = 0.02, p = 0.099). Furthermore, the likelihood-based information criteria were lower in the hypothesized model than in the alternative model (AIC = 3917.45 vs. 6166.58, BIC = 3986.89 vs. 6255.32, ABIC = 3929.79 vs. 6182.35), suggesting that the hypothesized model had superior fit to the data.
Figure 2.
Alternative Pathways Among Perceived Mental Health Provider Stigma, Internalized Stigma, and Disempowerment
4. Discussion
The present research examined how perceived stigma from mental health service providers, which is characterized by perceptions of negative affective reactions towards individual service users as well as perceptions of desired social distance towards those with mental illnesses more generally, related to the self-perceptions and treatment experience of mental health service users. Consistent with our hypotheses, we found that both perceived negative affective reactions and perceived social distance were positively associated with disempowerment in mental health settings. Furthermore, these associations were significantly mediated by internalized stigma: Perceptions of negative mental-illness-related beliefs held by service providers were associated with the internalization of such beliefs by service users, which was in turn linked to diminished self-efficacy and mastery in mental health treatment settings.
These findings represent the first quantitative evidence, to our knowledge, that illustrates the adverse impact of perceived provider stigma on mental health service users. Previous studies have clearly shown that, despite their professional training and extensive contact with people with mental illnesses, mental health service providers are nonetheless susceptible to the pervasive stigmatizing beliefs endorsed by the general public (Kopera et al., 2015; Lauber et al., 2004; Nordt et al., 2006; Overton and Medina, 2008; Penn and Martin, 1998). Qualitative research on the experiences of mental health service users further revealed that perceptions of provider stigma represent an important concern for those who utilize mental health services (Charles, 2013; Pinfold et al., 2005; Schulze and Angermeyer, 2003; Wahl, 1999). The current study contributes to this existing knowledge base by illuminating the role of internalized stigma as a potential mechanism underlying the association between perceived provider stigma and disempowerment. Extending prior research demonstrating the insidious impact of perceived societal stigma on both internalized stigma and self-esteem (Corrigan et al., 2006; Link et al., 2001; Quinn et al., 2015) as well as the role of internalized stigma in hindering active consumer participation in mental health treatment (Hamman et al., 2017), our results highlight how perceived stigma from mental health providers can “get under the skin” of service users and contribute to their overall sense of disempowerment in mental health settings.
The present investigation has several limitations. First, the cross-sectional nature of our data precludes drawing predictive, causal conclusions. In particular, whereas our conceptualization of perceived provider stigma as a predictor of internalized stigma and disempowerment is well-grounded in the theoretical literature (Corrigan et al., 2006; Link et al., 2001; Quinn et al., 2015), it is also possible that mental health service users who internalize negative mental-illness-related stereotypes would be more inclined to perceive stigma from their service providers and, as a result of these perceptions, experience greater disempowerment in mental health settings. Although we were able to demonstrate statistically that our hypothesized model was superior to this possible alternative, additional research is needed to clarify the relationships among perceived provider stigma, internalized stigma, and disempowerment. For example, prospective designs that include measures of these constructs at repeated assessment points over time could help elucidate the long-term and causal effects of perceived provider stigma on internalized stigma and disempowerment among mental health service users. Future studies utilizing matched designs in which levels of provider stigma is assessed from the perspectives of both mental health service users and their providers could also help clarify the causal impact of provider stigma on service users’ self-perceptions and recovery.
Second, the current dataset lacks a measure of psychiatric symptom severity, which has been associated with both internalized stigma (Livingston and Boyd, 2010) as well as hopelessness and low self-esteem (Yanos et al., 2008). As such, we cannot rule out the possibility that our results were driven by participants’ underlying psychiatric symptoms, such that those who experienced more severe symptoms were more likely to perceive and internalize stigma as well as experience disempowerment as a result of their symptoms. Given that both perceived stigma from the general public and internalized stigma have been shown to predict low self-esteem and mastery above and beyond psychiatric symptoms (Link et al., 2001; Livingston and Boyd, 2010), we believe that our hypothesized associations among perceived provider stigma, internalized stigma, and disempowerment would remain significant even after accounting for psychiatric symptom severity. Nevertheless, future research should carefully test our proposed model while including symptom severity as a covariate. Future research could also productively examine the impact of perceived provider stigma on other recovery-related outcomes, such as treatment adherence and quality of life.
Third, we acknowledge that, as in many studies that utilize venue-based recruitment, we did not track the total number of individuals we approached during the recruitment process nor the number of individuals who declined to participate in our study, thus preventing us from determining the response/refusal rate of our survey. We also cannot determine whether the mental health service users who chose to participate in our study significantly differed from those who declined to participate with respect to demographics, clinical characteristics, and/or treatment experiences. We further note that participants in our sample, on average, reported relatively low levels of perceived provider stigma, internalized stigma, and disempowerment. By demonstrating the significance of our hypothesized model with this sample, we showed that even “small doses” of stigma can significantly influence service users’ sense of self-efficacy and mastery in mental health settings. Nevertheless, future research should carefully examine the generalizability of our results using more heterogeneous, representative samples of mental health service users who have a wider range of experiences with stigma and disempowerment.
Lastly, future research is needed to identify potential intervention strategies for reducing stigma among mental health service providers. Beyond exposure to mental-illness-related stereotypes that are prevalent in the contemporary society, clinician burnout among mental health professionals has been linked to negative affective reactions towards, and internalized stigma among, their clients (Holmqvist & Jeanneau, 2006; Verhaeghe & Bracke, 2012). Intervention efforts that seek to reduce stigma among mental health professionals should therefore also incorporate activities that have been shown to effectively reduce clinician burnout, such as exercises in mindfulness and setting boundaries/priorities (Sayers et al., 2011).
It is unfortunate that people with mental illnesses often encounter stigma from professionals whose duty is to care for their mental health and to facilitate their recovery. The present research serves as an initial starting point in understanding how perceptions of stigma from service providers can influence the self-perceptions and recovery of those who utilize mental health services. It is our hope that these results will prompt continued reflection of mental health professionals on their own attitudes towards those with mental illnesses and highlight the need for future stigma reduction interventions that specifically target the attitudes and beliefs held by mental health professionals.
Highlights.
Mental health service users often encounter stigma from their providers.
Perceived provider stigma was linked to disempowerment in mental health settings.
Internalized stigma partially mediated this association.
Perceived provider stigma is powerful in shaping service users’ experiences.
Acknowledgments
Preparation of this manuscript was supported by grants K01MH079128 and R01MH109413 from National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Charles JLK. Mental health provider-based stigma: Understanding the experience of clients and families. Soc Work Ment Health. 2013;11(4):360–375. [Google Scholar]
- Connecticut Department of Mental Health and Addiction Services. Annual Statistical Report SFY 2016. 2016 Retrieved October 1, 2017 from http://www.ct.gov/dmhas/lib/dmhas/eqmi/annualreportsfy2016.pdf.
- Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37–70. doi: 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25(8):875–884. [Google Scholar]
- Hamann J, Buhner M, Rusch N. Self-Stigma and consumer participation in shared decision making in mental health services. Psychiatr Serv. 2017;68(8):783–788. doi: 10.1176/appi.ps.201600282. [DOI] [PubMed] [Google Scholar]
- Holmqvist R, Jeanneau M. Burnout and psychiatric staff’s feelings towards patients. Psychiatry Res. 2006;145(2–3):207–213. doi: 10.1016/j.psychres.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Kingdon D, Sharma T, Hart D. What attitudes do psychiatrists hold towards people with mental illness? Psychiatr Bull. 2004;28(11):401–406. [Google Scholar]
- Kopera M, Suszek H, Bonar E, Myszka M, Gmaj B, Ilgen M, et al. Evaluating explicit and implicit stigma of mental illness in mental health professionals and medical students. Community Ment Health J. 2015;51(5):628–634. doi: 10.1007/s10597-014-9796-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauber C, Anthony M, Ajdacic-Gross V, Rossler W. What about psychiatrists’ attitude to mentally ill people? Eur Psychiatry. 2004;19(7):423–427. doi: 10.1016/j.eurpsy.2004.06.019. [DOI] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: Understanding why labels matter. Am J Sociol. 1987;92(6):1461–1500. [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. 2001;52(12):1621–1626. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull. 2004;30(3):511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Nordt C, Rossler W, Lauber C. Attitudes of mental health professionals toward people with schizophrenia and major depression. Schizophr Bull. 2006;32(4):709–714. doi: 10.1093/schbul/sbj065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overton SL, Medina SL. The stigma of mental illness. J Couns Devel. 2008;86(2):143–151. [Google Scholar]
- Penn DL, Guynan K, Daily T, Spaulding WD, Garbin CP, Sullivan M. Dispelling the stigma of schizophrenia: what sort of information is best? Schizophr Bull. 1994;20(3):567–578. doi: 10.1093/schbul/20.3.567. [DOI] [PubMed] [Google Scholar]
- Penn DL, Martin J. The stigma of severe mental illness: some potential solutions for a recalcitrant problem. Psychiatr Q. 1998;69(3):235–247. doi: 10.1023/a:1022153327316. [DOI] [PubMed] [Google Scholar]
- Perlick DA, Rosenheck RA, Clarkin JF, Sirey JA, Salahi J, Struening EL, et al. Stigma as a barrier to recovery: Adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatr Serv. 2001;52(12):1627–1632. doi: 10.1176/appi.ps.52.12.1627. [DOI] [PubMed] [Google Scholar]
- Pinfold V, Byrne P, Toulmin H. Challenging stigma and discrimination in communities: a focus group study identifying UK mental health service users’ main campaign priorities. Int J Soc Psychiatry. 2005;51(2):128–138. doi: 10.1177/0020764005056760. [DOI] [PubMed] [Google Scholar]
- Quinn DM, Williams MK, Weisz BM. From discrimination to internalized mental illness stigma: The mediating roles of anticipated discrimination and anticipated stigma. Psychiatr Rehabil J. 2015;38(2):103–108. doi: 10.1037/prj0000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv. 1997;48(8):1042–1047. doi: 10.1176/ps.48.8.1042. [DOI] [PubMed] [Google Scholar]
- Schulze B. Stigma and mental health professionals: a review of the evidence on an intricate relationship. Int Rev Psychiatry. 2007;19(2):137–155. doi: 10.1080/09540260701278929. [DOI] [PubMed] [Google Scholar]
- Schulze B, Angermeyer MC. Subjective experiences of stigma. A focus group study of schizophrenic patients, their relatives and mental health professionals. Soc Sci Med. 2003;56(2):299–312. doi: 10.1016/s0277-9536(02)00028-x. [DOI] [PubMed] [Google Scholar]
- Stuber JP, Rocha A, Christian A, Link BG. Conceptions of mental illness: Attitudes of mental health professionals and the general public. Psychiatr Serv. 2014;65(4):490–497. doi: 10.1176/appi.ps.201300136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhaeghe M, Bracke P. Associative stigma among mental health professionals: implications for professional and service user well-being. J Health Soc Behav. 2012;53(1):17–32. doi: 10.1177/0022146512439453. [DOI] [PubMed] [Google Scholar]
- Wahl OF. Mental health consumers’ experience of stigma. Schizophr Bull. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- Yanos PT, Roe D, Markus K, Lysaker PH. Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatr Serv. 2008;59(12):1437–1442. doi: 10.1176/appi.ps.59.12.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]