Abstract
Background and Purpose
Although current guidelines advocate pretreatment with intravenous thrombolysis (IVT) in all eligible acute ischemic stroke (AIS) patients with large vessel occlusion (LVO) prior to mechanical thrombectomy (MT), there are observational data questioning the efficacy of this approach. One of the main arguments in favour of IVT pretreatment is the potential for tPA-induced successful reperfusion (SR) before the onset of endovascular procedure.
Methods
We performed a systematic review and meta-analysis of randomized-controlled clinical trials (RCTs) and observational cohorts providing rates of SR with IVT in patients with LVO before the initiation of MT. We also performed subgroup analyses according to study type (RCTs vs. observational) and according to the inclusion per-protocol of patients with tandem (intracranial/extracranial) occlusions.
Results
We identified 13 eligible studies (7 RCTs & 6 observational cohorts), including 1561 AIS patients (median NIHSS score: 17) with LVO. SR following IVT and before MT was documented in 11% [95% confidence interval (95%CI): 7%–16%], with no difference among cohorts derived from RCTs and observational studies. There was significant heterogeneity across included studies both in the overall analysis and among subgroups (I2>84%, p for Cochran Q<0.001). Higher tPA-induced SR rates were documented in studies reporting the exclusion of tandem occlusions (17%, 95%CI:11%–23%) compared to the rest (7%, 95%CI: 4%–11%;p for subgroup differences: 0.003).
Conclusions
Pretreatment with systemic thrombolysis in LVO patients eligible for MT results in SR in one out of ten cases, negating the need for additional endovascular reperfusion. Tandem occlusions appear to be the least responsive to IVT pretreatment.
Keywords: intravenous thrombolysis, acute ischemic stroke, large vessel occlusion, mechanical thrombectomy, recanalization, reperfusion
Introduction
Although randomized data and current guidelines advocate pretreatment with intravenous thrombolysis (IVT) in all eligible acute ischemic stroke (AIS) patients with large vessel occlusion (LVO) prior to mechanical thrombectomy (MT),1 there are observational data questioning the efficacy of systemic thrombolysis in patients with LVO.2 One of the main arguments in favour of IVT pretreatment is the potential for tissue-plasminogen-activator (tPA) induced successful reperfusion (SR) before the onset of endovascular procedure averting the need for MT.2
In view of the former considerations we performed a systematic review and meta-analysis of all available cohorts published to date providing rates of SR with IVT in patients with LVO before the initiation of MT.
Methods
Authors declare that all supporting data are available within the article and its online supplementary files. This meta-analysis is presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews and meta-analyses and was written according to the Meta-analysis of Observational Studies in Epidemiology proposal.3 The present manuscript also adheres to the AHA Journals’ implementation of the Transparency and Openness Promotion (TOP) guidelines.4 Eligible cohorts were identified by searching MEDLINE and SCOPUS databases for published randomized-controlled clinical trials (RCTs) and observational cohort studies on the use of bridging therapy (IVT followed by MT) for AIS patients with LVO. Additional details (including the complete search algorithm) for the database search are available in the Online Supplement.
SR at the beginning of MT was defined as modified Thrombolysis in Cerebral Infarction grades of IIb/III on the angiography before MT procedure (second angiographic run) or significant clinical improvement (considered suggestive of successful reperfusion) amending the need for subsequent MT procedure following tPA-bolus.5 We calculated the point prevalence in all included cohorts by dividing the number of events (SR with IVT pretreatment) by the total number of patients scheduled to receive bridging therapy. Publication bias was evaluated graphically using a funnel plot, and with the Egger’s statistical test for funnel plot asymmetry. After the overall analysis, we performed a post-hoc sensitivity analysis after excluding studies not clearly describing the timing of initial vascular imaging in relation to IVT onset. We also conducted additional subgroup analyses according to study type (RCT vs. observational study) and the inclusion per-protocol of patients with tandem (intracranial/extracranial) occlusions. Finally, we performed meta-regression analyses according to the OTBT (onset-to-bolus time), BTGPT (bolus-to–groin-puncture time) and baseline demographic characteristics (admission NIHSS score, age and male sex) reported in included studies. Further details on the statistical analysis are available in the Online Supplement.
Results
The flow chart on study selection procedure and the list of excluded studies are available in the Online Supplement (Supplemental Figure I & Supplemental Table). Patient characteristics from eligible cohorts (7 RCTs and 6 observational studies) comprising a total of 1561 patients (median admission-NIHSS: 17), are briefly summarized in the Table (See supplemental material).
Table.
Baseline characteristics of study populations across included studies
| Study name | Study type | N | Age (years) | Men (%) | NIHSS-score on admission | OTBT (min) | BTGPT (min) |
|---|---|---|---|---|---|---|---|
| ESCAPE | RCT | 120* | N/A | N/A | N/A | N/A | N/A |
| EXTEND-IA | RCT | 35 | 68.6±12.3** | 49% | 17 | 127 | 74 |
| MR CLEAN | RCT | 203* | N/A | N/A | N/A | N/A | N/A |
| REVASCAT | RCT | 70* | N/A | N/A | N/A | N/A | N/A |
| SWIFT PRIME | RCT | 98 | 65.0±12.5** | 55% | 17 (13–20)*** | N/A | 57 |
| THRACE | RCT | 204 | 66 (54–74)*** | 57% | 18 | 153 | 100 |
| THERAPY | RCT | 55 | 67±11** | 62% | 17 | 108 | 119 |
| Fjetland et al | OS | 57 | 71.8 | 59.6% | 18 | 105 | 75 |
| Gerschenfeld et al | OS | 159 | 72 | 54.1% | 16 | 144 | 76 |
| Kim et al | OS | 118 | 71.5±14.5** | 47.0% | 14.4 | N/A | 75 |
| Mueller et al | OS | 319 | 68.4±14.5** | 58.0% | 15 | 166±64** | N/A |
| Sallustio et al | OS | 18 | 64.5±12.1** | 62.0% | 19±5** | N/A | N/A |
| Weber et al | OS | 105 | 70.2±12.6** | 49.5% | 15.5 (12–20)*** | 115 (84–181)*** | 118 |
excluded patients receiving direct mechanical thrombectomy
mean± standard deviation
median (interquartile range)
RCT: randomized-controlled clinical trial
OS: observational study
N/A: not available
NIHSS: National-Institutes-of-Health Stroke Scale
OTBT: onset-to-bolus time
BTGPT: bolus-to-groin-puncture time
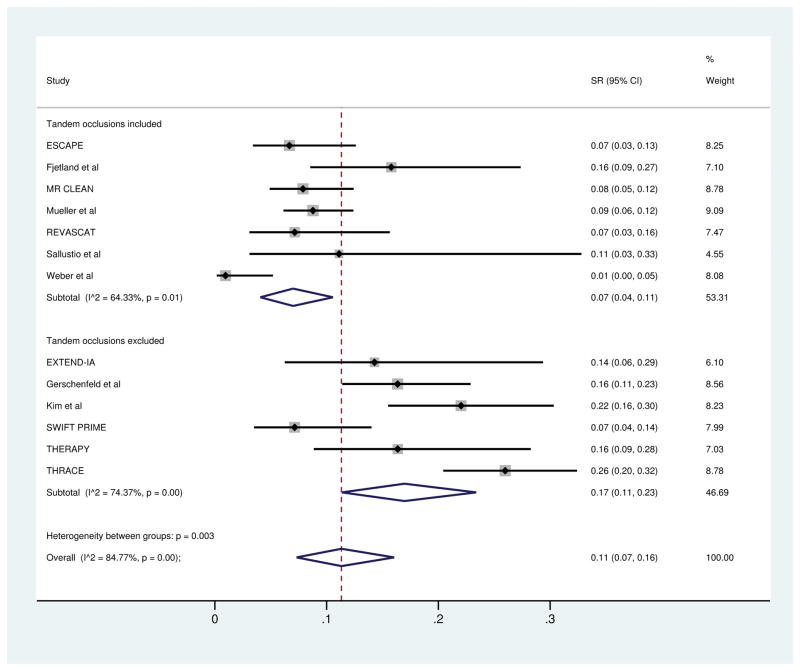
The pooled prevalence of SR was 11% [95% confidence interval (95%CI): 7%–16%)] in the overall analysis of all included studies (See supplemental material) and 12% (95%CI:8–17%) in the post-hoc sensitivity analysis of eligible studies (n=11) clearly reporting timing of initial vascular imaging in relation to IVT administration (Supplemental Figure II). In subgroup analysis according to study type, no difference was found among cohorts derived from RCTs 11% (95%CI:6%–18%) and observational studies 11% (95%CI:5%–19%). Significant heterogeneity was identified in both the overall analysis, sensitivity analysis and among subgroups (I2>80%, p for Cochran Q: <0.001; Supplemental Figures II&III). The presence of considerable heterogeneity among studies was also evident in the asymmetrical appearance of funnel plot (Supplemental Figure IV; p for Egger’s test: 0.041). Studies reporting the exclusion of LVO patients with tandem occlusions had higher rates of SR (17%, 95%CI: 11%–23%) compared to the rest (7%, 95%CI:4%–11%; p=0.003; Figure). Moreover, the detected heterogeneity was the lowest (I2:64%) across studies including patients with tandem occlusions. Finally, meta-regression analyses uncovered no moderating effect on the rates of SR according to reported OTBT (Supplemental Figure V), BTGPT (Supplemental Figure VI), admission NIHSS score (Supplemental Figure VII), mean/median age (Supplemental Figure VIII) and male sex (Supplemental Figure IX) in included studies.
Figure.
Successful reperfusion rates following intravenous thrombolysis in patients with Large Vessel Occlusion stratified by the inclusion of patients with tandem occlusions.
Discussion
Our meta-analysis showed that one in ten LVO patients pretreated with IVT achieves SR prior to MT onset averting additional endovascular procedures. We also documented that part of the heterogeneity across included studies could be explained by the presence of tandem occlusions, which were the least responsive to IVT pretreatment. Finally, the effect of IVT on SR was not modified by OTBT, BTGPT, baseline stroke severity, age or sex.
The reported percentage of SR in our meta-analysis 11% (95%CI:7%–16%) is significantly lower from the pooled percentage of complete reperfusion reported in a recent meta-analysis of all available patient cohorts treated solely with IVT (20%; 95%CI:15%–26%).6 This difference could be attributed to potential underreporting of the incidence of tPA-induced SR due to the design of certain RCTs excluding “drip and ship” patients with early reperfusion following IVT pretreatment from enrolment in the trials. Moreover, patient selection in these trials was based on vascular imaging that was predominantly conducted after the beginning of tPA infusion, thus potential missing additional patients with early reperfusion.7
Our results are complimentary to a recent meta-analysis reporting that IVT pretreatment prior to MT is associated with higher successful reperfusion rates (mTICI 2b-3) following MT and a higher likelihood of successful reperfusion with fewer passes compared to direct MT.8 This beneficial effect of IVT pretreatment on SR translated into better three-month functional outcomes with bridging therapy (IVT & MT) compared to direct MT.8 These findings combined with the observations of our meta-analysis further highlight that pretreatment with IVT may avert the need for additional endovascular procedures (reducing costs and preventing potential complications) in a non-negligible portion of LVO patients,2 which could be of paramount importance in LVO patients with unfavorable vessel anatomy (tortuosity, type III aortic arch) complicating endovascular access to intracranial arterial clots. Finally, the beneficial effect of tPA-induced SR in LVO prior to MT may be further accentuated in the settings of mobile stroke units (MSU) given the greater potential for ultra-early treatment within the golden hour (≤60 min from symptom onset).
Our findings also indicate that patients with tandem occlusions have the lowest likelihood to achieve SR following systemic thrombolysis and may benefit the most from direct transfer to comprehensive stroke centers for prompt initiation of MT. Clot burden is the highest among patients with tandem occlusions and this may account for their poor response to IVT.9 Previous studies evaluating AIS patients treated with IVT have shown that tandem occlusions are associated with the lowest rates of complete recanalization and three-month favourable functional outcome.10,11
Certain limitations of the present meta-analysis need to be acknowledged including the moderate sample size and the significant heterogeneity across studies (I2>50%) in overall and subgroup analyses. The per-protocol exclusion of patients with SR occurring before MT in many protocols could have been partially responsible for the observed heterogeneity that we detected across included studies, but also might have biased the results of the present meta-analysis towards an underestimation of SR. In an effort to account for this possible underestimation of SR we reviewed the methods on patient selection and imaging procedures of included studies and performed a post-hoc sensitivity analysis after excluding those protocols not clearly describing the timing of initial vascular imaging in relation to IVT onset (Supplemental Figure II). Another major limitation of the present report and possible source of bias, which could further explain part of the documented heterogeneity across included studies, is the inclusion of patients that were reported to have significant clinical improvement after IVT without angiographic confirmation of SR. Third, we were able to assess in univariable meta-regression analyses the potential association of SR after IVT only with age, sex, OTBT, BTGPT and baseline stroke severity, since other baseline characteristics were unavailable in the majority of included studies. Moreover, it should be highlighted that as the aforementioned meta-regression analyses were conducted at the study-level, and not at the patient level, their results should be interpreted with caution. Additionally, it should be noted that no subgroup analysis according to the site of occlusion could be performed due to unavailable data. This analysis could be of major importance since response to IVT is known to be influenced by the site of occlusion,9 while the association of tandem occlusions with lower SR rates should ideally have been adjusted for the site of intracranial occlusion. Finally, the potential publication bias could not be reliably assessed due to the substantial heterogeneity across trials.
In conclusion, pretreatment with systemic thrombolysis in LVO patients eligible for MT results in SR in one out of ten cases, negating the need to pursue further endovascular procedures. This beneficial effect of bridging therapy should be further evaluated in the prehospital settings of MSU that are associated with the swiftest possible tPA delivery in AIS patients.
Supplementary Material
Acknowledgments
Funding: None
Footnotes
Disclosures: Dr. Schellinger has received significant honoraria from Boehringer Ingelheim as a consultant, member of the advisory and speaker board and modest speaker honoraria from Medtronic. Dr. Schellinger has also received significant honoraria as official and independent expert witness and advisor for German federal courts related to diagnosis and treatment of stroke including intravenous thrombolysis and thrombectomy. Dr. Köhrmann has received travel compensation, lecture fees and honoraria for advisory boards from Boehringer Ingelheim, Bayer, BMS/Pfizer and Daiichi. Dr. Anne W. Alexandrov has been a member in the Genentech and Stryker Neurovascular Speakers’ Bureau. Dr. Gurol is supported by a research grant from the National Institute of Health (NS083711).
References
- 1.Tsivgoulis G, Katsanos AH, Mavridis D, Magoufis G, Arthur A, Alexandrov AV. Mechanical thrombectomy improves functional outcomes independent of pretreatment with intravenous thrombolysis. Stroke. 2016;47:1661–1664. doi: 10.1161/STROKEAHA.116.013097. [DOI] [PubMed] [Google Scholar]
- 2.Tsivgoulis G, Katsanos AH, Mavridis D, Alexandrov AW, Magoufis G, Arthur A, et al. Endovascular thrombectomy with or without systemic thrombolysis? Ther Adv Neurol Disord. 2017;10:151–160. doi: 10.1177/1756285616680549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 4. [Assessed November 7th 2017];Transparency and Openness Promotion (TOP) Guidelines for Authors Publishing in an American Heart Association Journal. http://www.ahajournals.org/content/TOP-guidelines.
- 5.Zaidat OO, Lazzaro MA, Liebeskind DS, Janjua N, Wechsler L, Nogueira RG, et al. Revascularization grading in endovascular acute ischemic stroke therapy. Neurology. 2012;79:S110–166. doi: 10.1212/WNL.0b013e3182695916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seners P, Turc G, Maïer B, Mas JL, Oppenheim C, Baron JC. Incidence and Predictors of Early Recanalization After Intravenous Thrombolysis: A Systematic Review and Meta-Analysis. Stroke. 2016;47:2409–2412. doi: 10.1161/STROKEAHA.116.014181. [DOI] [PubMed] [Google Scholar]
- 7.Seners P, Oppenheim C, Baron JC. Mechanical Thrombectomy After Intravenous Thrombolysis vs Mechanical Thrombectomy Alone in Acute Stroke. JAMA Neurol. 2017;74:1014–1015. doi: 10.1001/jamaneurol.2017.1340. [DOI] [PubMed] [Google Scholar]
- 8.Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ, et al. Mechanical Thrombectomy Outcomes With and Without Intravenous Thrombolysis in Stroke Patients: A Meta-Analysis. Stroke. 2017 Jul 26; doi: 10.1161/STROKEAHA.117.017320. [DOI] [PubMed] [Google Scholar]
- 9.Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38:948–54. doi: 10.1161/01.STR.0000257304.21967.ba. [DOI] [PubMed] [Google Scholar]
- 10.Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006;37:2301–2305. doi: 10.1161/01.STR.0000237070.80133.1d. [DOI] [PubMed] [Google Scholar]
- 11.Nogueira RC, Bor-Seng-Shu E, Saeed NP, Teixeira MJ, Panerai RB, Robinson TG. Meta-analysis of Vascular Imaging Features to Predict Outcome Following Intravenous rtPA for Acute Ischemic Stroke. Front Neurol. 2016;18(7):77. doi: 10.3389/fneur.2016.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.