Abstract
Background and Purpose
Spontaneous cerebellar intracerebral hemorrhage (ICH) has been been reported to be mainly associated with vascular changes secondary to hypertension. However, a subgroup of cerebellar-ICH, seems related to vascular amyloid deposition (cerebral amyloid angiopathy, CAA). We sought to determine whether location of hematoma in the cerebellum (deep and superficial regions) was suggestive of a particular hemorrhage-prone small vessel disease pathology (CAA or hypertensive vasculopathy).
Methods
Consecutive cerebellar-ICH patients from a single tertiary care medical center were recruited. Based on data from pathologic reports, patients were divided according to the location of the primary cerebellar hematoma (deep vs superficial). Location of cerebral microbleeds (CMB; strictly-lobar, strictly-deep and mixed-CMB) was evaluated on MRI.
Results
One-hundred and eight patients (84%) had a deep cerebellar hematoma and 20 (16%) a superficial cerebellar hematoma. Hypertension was more prevalent in deep than in superficial cerebellar-ICH patients (89 vs 65%, respectively; p<0.05). Among patients who underwent MRI, those with superficial cerebellar-ICH had higher prevalence of strictly lobar-CMB (43%) and lower prevalence of strictly deep or mixed-CMB (0%) compared to those with deep superficial cerebellar-ICH (6%, 17% and 38%, respectively). In a multivariable model, presence of strictly lobar-CMB was associated with superficial cerebellar-ICH (OR: 3.8; 95% confidence interval: 1.5–8.5; p=0.004).
Conclusions
Our study showed that superficial cerebellar-ICH is related to the presence of strictly lobar-CMB, a pathologically proven marker of CAA. Cerebellar hematoma location may thus help to identify those patients likely to have CAA pathology.
Keywords: cerebellar-hemorrhage, cerebral amyloid angiopathy, microbleeds
INTRODUCTION
Spontaneous cerebellar intracerebral hemorrhage (ICH) has been been reported to be mainly associated with vascular changes secondary to hypertension.1 However, a subgroup of cerebellar-ICH, seems related to vascular amyloid deposition.2
In supratentorial ICH patients, the location of the primary bleed in combination with the distribution of small vessel disease (SVD) markers point to the most likely dominant microangiopathy. 3–5 For example, patients with a lobar ICH and strictly lobar-cerebral microbleed (CMB) are likely to harbor CAA according to the pathologically validated Boston criteria.3 Similarly, patients with deep ICH accompained by the presence of MRI markers such as strictly deep-CMB are more likely to harbor vessel changes secondary to hypertension and other vascular risk factors.4,5
In cerebellar-ICH, the hematoma is generally located in or close to one of the dentate nuclei,1,6 which can be referred to as deep location. By contrast, in a subgroup of cases, hematoma location can be restricted to the cerebellar cortex and vermis (eg superficial areas).1,2 In analogy with supratentorial ICH, whether the cerebellar hematoma location (deep vs. superficial) could suggest a dominant microvascular etiology is unknown.
In the present study, we sought to determine whether superficial location of cerebellar-ICH was associated with other neuroimaging markers of CAA, in particular strictly lobar-CMB. Secondly, in order to estimate the proportion of cerebellar-ICH patients who may harbor CAA pathology, we aimed to determine the prevalence of different patterns of primary cerebellar hematoma distribution.
METHODS
We performed a retrospective analysis of data drawn from an ongoing prospective cohort study of ICH performed at Massachusetts General Hospital (MGH; Boston, MA, USA).4,5 Study subjects were consecutive spontaneous cerebellar-ICH patients admitted to MGH (Figure 1). This study was performed with the approval of the institutional review board of MGH and with informed consent of all subjects or authorized family members. The authors declare that all supporting data are available within the article/online supplementary files. Detailed description of study methodology is reported in supplemental material.
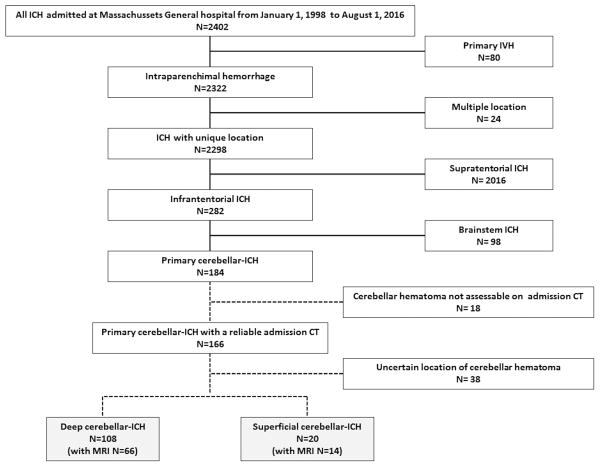
Figure 1.
Flow chart of the study enrollment
Data collection
Baseline data collection was performed as previously described.4,5
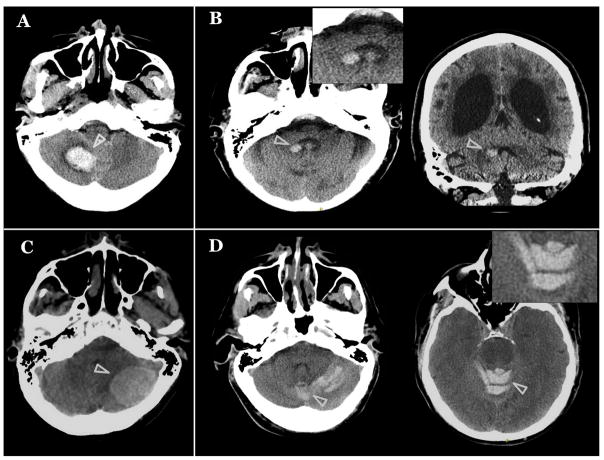
Admission CT scan were evaluated and hematoma location was rated in the cerebellum. According to the hematoma location patients were divided in a) deep cerebellar-ICH (with and without peduncular involvement, Figure 2, Panel A–B); b) superficial cerebellar-ICH (with and without vermian involvement, Figure 2, Panel C–D); For definitions see also Supplemental Table II and Supplemental Figure I.
Figure 2. Examples of different cerebellar hematoma locations.
Axial sections of CT scans (A–D) demonstrating acute cerebellar-hemorrhage (ICH) (white arrowheads). (A) Deep cerebellar-ICH; (B) deep cerebellar-ICH with peduncular involvement, axial and coronal sections; C) superficial cerebellar-ICH; (D) superficial cerebellar-ICH with vermian involvement.
Neuroimaging markers of SVD were rated according to STRIVE consensus criteria.7 We categorized CMB distribution as strictly lobar-CMB, strictly deep-CMB and mixed-CMB.
Statistical analysis
Clinical characteristics were compared between deep cerebellar-ICH and superficial cerebellar-ICH in univariate analyses. Age, sex and variables with a p-value < 0.1 in univariate comparisons were entered in logistic regression models. All analyses were performed using JMP Pro 12 software (SAS Institute Inc).
RESULTS
There were 2402 patients admitted for ICH over 18 years at MGH (Figure 1). In 108 of the 128 (84%) classifiable patients, the hematoma was located in deep areas of the cerebellum (deep cerebellar-ICH). In 20 patients (16%) the hematoma was located in superficial cerebellar areas (superficial cerebellar-ICH; Table 1). Table 1 compares clinical characteristics between deep cerebellar-ICH and superficial cerebellar-ICH. In multivariable analysis, presence of hypertension was associated with deep cerebellar-ICH (OR 2.03; 95% confidence interval [CI] 1.1–3.6; p=0.018) after correction for age and sex.
Table 1.
Comparisons between deep and superficial cerebellar-ICH
| All cohort | MRI cohort | |||
|---|---|---|---|---|
| Variables | Deep cerebellar-ICH N=108 | Superficial cerebellar-ICH N=20 | Deep cerebellar-ICH N=66 | Superficial cerebellar-ICH N=14 |
| Mean age±SD | 72.7±12.1 | 73.3±11.9 | 73.6±11.8 | 73.5±10.8 |
| Sex (female) (%) | 51 (47) | 12 (60) | 34 (51) | 8 (57) |
| Hypertension (%) | 96 (89) | 13 (65)* | 57 (86) | 9 (64)* |
| Diabetes (%) | 24 (22) | 4 (20) | 18 (27) | 2 (14) |
| Hypercholesterolemia (%) | 42 (41) | 10 (50) | 30 (45) | 6 (43) |
| Atrial Fibrillation (%) | 27 (26) | 6 (30) | 16 (26) | 4 (29) |
| Warfarin (%) | 28 (26) | 8 (40) | 16 (24) | 4 (29) |
| Antiplatelets (%) | 45 (42) | 11 (55) | 30 (45) | 7 (50) |
| Statins (%) | 37 (36) | 8 (40) | 22 (33) | 5 (36) |
| Previous IS (%) | 24 (23) | 3 (15) | 24 (20) | 3 (21) |
| Previous ICH (%) | 6 (6) | 1 (5) | 5 (7) | 1 (7) |
| Hematoma evacuation (%) | 23 (21) | 7 (35) | 10 (16) | 5 (35) |
| Strictly-lobar CMB (%) | NA | NA | 4 (6) | 6 (43)* |
| Strictly-deep CMB (%) | NA | NA | 11 (17) | 0 |
| Mixed-CMB (%) | NA | NA | 25 (38) | 0 |
| Lacunes (%) | NA | NA | 35 (53) | 3 (21)* |
| Severe CSO-EPVS (%) | NA | NA | 8 (12) | 2 (14) |
| Severe BG-EPVS (%) | NA | NA | 21 (32) | 2 (14) |
| cSS (%) | NA | NA | 3 (5) | 1 (7) |
| Moderate-severe WMH (%) | NA | NA | 39 (59) | 9 (64) |
| Moderate-severe GBA (%) | NA | NA | 26 (39) | 4 (29) |
ICH: intracerebral hemorrhage, IS: ischemic stroke; CMB: cerebral microbleeds; CSO: centrum semiovale; BG: basal ganglia; EPVS: enlarged perivascular spaces; WMH: white matter hyperintensities; GBA: global brain atrophy;
p<0.05;
In the subgroup of enrolled patients who underwent MRI during hospitalization, 66 (83%) had a deep cerebellar-ICH and 14 (17%) had a cerebellar hematoma located in a superficial location. Supplemental Table III reports differences between patients with and without MRI. Patients with superficial cerebellar-ICH had higher prevalence of strictly lobar-CMB (43%) and no strictly deep or mixed-CMB (0%) compared to deep cerebellar-ICH (6%, 17% and 38%, respectively; Table 1). Presence of lacunes was significantly higher in deep cerebellar-ICH than superficial cerebellar-ICH (53 vs 21%, respectively; p=0.041). In multivariate analyses, presence of strictly lobar-CMB was associated with superficial cerebellar-ICH (OR: 3.8; CI: 1.5–8.5; p=0.004) after correction for age, sex, hypertension and lacunes. We repeated the analysis adding 13 patients with uncertain location but with predominant deep involvement and 1 patient with predominant superficial involvement and the results remain unchanged.
DISCUSSION
Our study showed that superficial cerebellar-ICH was related with the presence of strictly lobar-CMB, a pathologic proven marker of CAA.3,8 The majority of cerebellar-ICH patients showed a primary hematoma located in deep cerebellar areas and were more likely to have hypertension. Finally, our results suggest that the location of the hematoma in cerebellar-ICH may help to identify those patients with likely CAA pathology. This could potentially impact future treatment decisions in these patients.9
Our aim was to evaluate whether superficial cerebellar-ICH is related to CAA, a highly frequent SVD in the elderly. We found that patients with superficially located cerebellar hematomas were not only more likely to have strictly lobar-CMB but also lacked CMB in strictly deep or mixed locations. Previous pathological studies have reported that cerebellar hematomas located in superfical areas represent a minority of cerebellar ICH, but may be more likely to harbor CAA compared to cerebellar-ICH in deep locations.2 Vessels implicated in these cases appear to be distal penetrating pial arteries arising from the major cerebellar arteries.1,2 Conversely, previous pathological observations have suggested that most cerebellar-ICHs related to hypertension arise in or close to one of the dentate nuclei in the deep areas of the cerebellum.1
This study has limitations. Our study lacks pathologic data to allow for a definitive characterization of the type of vessel changes underlying both deep and superficial cerebellar-ICH. However, our results are in line with previous pathologic studies that have suggested that the location of the cerebellar hematoma may be related to different vasculopathies.1,2 Furthermore, a recent meta-analysis taking into account only 8 cerebellar-ICH patients reported presence of pathologically proven CAA in half of the cases.10 Because our study was exploratory and hypothesis-generating, we did not correct for multiple comparisons.
In conclusion, our data suggests that patients with superficial cerebellar-ICH are more likely to harbor CAA pathology, by neuroimaging criteria. If confirmed in other cohorts, it is conceivable that cerebellar hematoma location may help to identify those patients suspected to have CAA pathology.
Supplementary Material
Acknowledgments
Source of funding: NIH grants R01AG047975, R01AG026484, P50AG005134, K23AG02872605
Footnotes
Disclosures: None
References
- 1.Dinsdale HB. Spontaneous hemorrhage in the posterior fossa: a study of primary cerebellar and pontine hemorrhages with observations on their pathogenesis. Arch Neurol. 1964;10:200–217. doi: 10.1001/archneur.1964.00460140086011. [DOI] [PubMed] [Google Scholar]
- 2.Itoh Y, Yamada M, Hayakawa M, et al. Cerebral amyloid angiopathy: a significant cause of cerebellar as well as lobar cerebral hemorrhage in the elderly. J Neurol Sci. 1993;116:135–141. doi: 10.1016/0022-510x(93)90317-r. [DOI] [PubMed] [Google Scholar]
- 3.Knudsen KA, Rosand J, Karluk D, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: Validation of the Boston Criteria. Neurology. 2001;56:537–539. doi: 10.1212/wnl.56.4.537. [DOI] [PubMed] [Google Scholar]
- 4.Charidimou A, Boulouis G, Pasi M, et al. MRI-visible perivascular spaces in cerebral amyloid angiopathy and hypertensive arteriopathy. Neurology. 2017;88:1157–1164. doi: 10.1212/WNL.0000000000003746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pasi M, Boulouis G, Fotiadis P, et al. Distribution of lacunes in cerebral amyloid angiopathy and hypertensive small vessel disease. Neurology. 2017;88:2162–2168. doi: 10.1212/WNL.0000000000004007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher M, Picard EH, Polak A, Dalal P, Pojemann RG. Acute hypertensive cerebellar hemorrhage: diagnosis and surgical treatment. J Nerv Ment Dis. 1965;140:38–57. doi: 10.1097/00005053-196501000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–838. doi: 10.1016/S1474-4422(13)70124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martinez-Ramirez S, Romero J-R, Shoamanesh A, et al. Diagnostic value of lobar microbleeds in individuals without intracerebral hemorrhage. Alzheimers Dement J Alzheimers Assoc. 2015;11:1480–1488. doi: 10.1016/j.jalz.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurol ME, Greenberg SM. Management of intracerebral hemorrhage. Curr Atheroscler Rep. 2008;10:324–331. doi: 10.1007/s11883-008-0050-y. [DOI] [PubMed] [Google Scholar]
- 10.Samarasekera N, Smith C, Salman RA-S. The association between cerebral amyloid angiopathy and intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2012;83:275–281. doi: 10.1136/jnnp-2011-300371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.